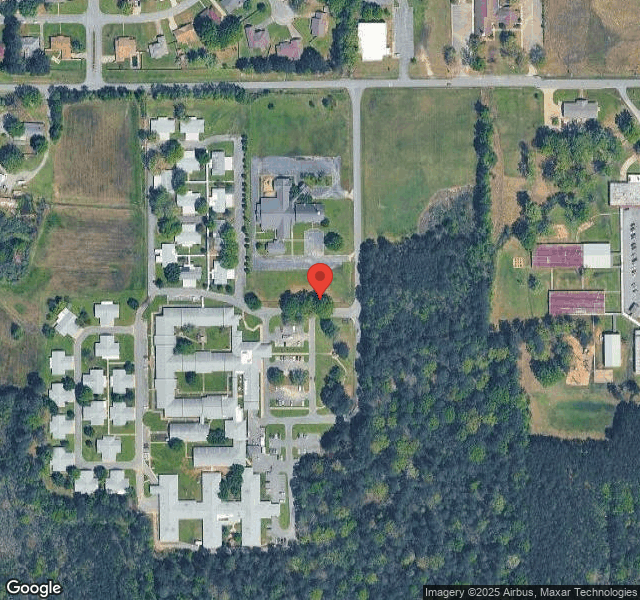
TRINITY VILLAGE MEDICAL CENTER



Inspected within the last 6 months. Data reflects current conditions.
Trinity Village Medical Center in Pine Bluff, Arkansas has received a Trust Grade of F, indicating significant concerns about the facility’s quality of care. It ranks #216 out of 218 nursing homes in the state, placing it in the bottom half, and #4 out of 4 in Jefferson County, meaning there are no better local options. The facility's trend is worsening, with issues increasing from 15 in 2024 to 16 in 2025, and it has reported 37 deficiencies, including critical incidents where residents suffered injuries of unknown origin that were not reported or investigated properly, posing serious risks. While staffing is rated average with a turnover rate of 48%, which is below the state average, the overall health inspection score is a poor 1 out of 5, raising concerns about resident safety and care quality. Although there have been no fines, the serious nature of the deficiencies suggests families should carefully consider other options.
- Trust Score
- F
- In Arkansas
- #216/218
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 48% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Arkansas facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 21 minutes of Registered Nurse (RN) attention daily — below average for Arkansas. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 37 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Arkansas average (3.1)
Significant quality concerns identified by CMS
Near Arkansas avg (46%)
Higher turnover may affect care consistency
The Ugly 37 deficiencies on record
Jul 2025
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on record reviews, interviews, and facility policy review, the facility failed to ensure a smoking assessment was completed for one (Resident #12) of two residents reviewed for smoking safety.
T...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, record review, interview, and facility policy review, the facility failed to ensure Enhanced Barrier Precautions (EBP) were followed during high contact care to prevent the risk ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on interviews, record reviews, and facility policy review, the facility failed to ensure Care Plans were updated for two (Resident #11 and Resident #12) of two residents reviewed for Care Plan a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and facility policy review, the facility failed to ensure food stored in the freezer and dry storage area were covered or sealed, one of one ice scoop holder was maint...
Read full inspector narrative →
Jan 2025
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observations, interviews, record review, and facility policy review the facility failed to ensure the care planned positioning device was in place to prevent further contracture for 1 of 1 sa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review, interview, and facility policy review the facility failed to ensure gradual psychotropic (anti-anxiety) dose reductions (GDR) were attempted in the absence of a physician's doc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure pureed food items were blended to a smooth, lump free consistency to minimize the risk of choking or other complications for those res...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected multiple residents
Based on observations, interviews, record review, and facility policy review the facility failed to ensure the personal and medical information was protected for 3 (Resident #1, #40, #236) of 4 sample...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record review, and facility policy review, it was determined that the facility failed to ensure care plans ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the use of a physical restraint was used to treat a resident's medical symptoms, and was not being used for staff conv...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observations, interviews, record review, and facility policy review, the facility failed to ensure the medication error rate was not greater than 5%. The Medication error occurred with 2 (Res...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
Based on observation, interview, record review, and facility policy review, the facility failed to ensure the facility was free of significant medication errors for 1 (Resident #44) of 1 sampled resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations, interviews, record review, and facility policy review, the facility failed to ensure medications and biologics were securely stored away at all times to prevent unauthorized ind...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure meals were prepared and served according to the planned written menu to meet the nutritional needs of the residents fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, record review, and facility policy review, the facility failed to ensure food items in the refrigerator, freezer and storage room were covered, and sealed; leftovers m...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, record review and facility policy review the facility failed to ensure enhanced barrier precautions (EBP) were being followed to prevent the spread of possible infecti...
Read full inspector narrative →
Jul 2024
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure interventions for a hand device was consistently used for 1 (Resident #39) of 1 sampled resident who had a hand contra...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure dental care was provided for 1 (Resident #71) of 1 sampled (Resident #71) to promote good oral hygiene.
The findings a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure all bodily areas were cleansed during incontinent care to promote cleanliness and good personal hygiene to prevent the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure a refund was received by the resident or respo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
On 07/16/2024 at 1:03 PM, this surveyor observed Dakin's solution, oxy cleaner and wound cleanser in an open closet and antimicrobial soap on the floor in an open unattended office.
On 07/16/2024 at ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
2. Review of the Order Summary Report indicated Resident #25 had diagnoses of Chronic Obstructive Pulmonary Disease (COPD) with acute exacerbation (worsening), acute respiratory failure with hypercapn...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview, the facility failed to ensure staff were trained on how to monitor residents on a high-risk medication (anticoagulants), Apixaban (Eliquis), for 1 (R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
On 07/17/2024 at 11:30 AM, the Director of Nursing (DON) provided the Medication Regime Reviews forms that were provided to the facility by the pharmacist. The DON confirmed the only medication regime...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
On 07/16/2024 at 10:32 AM, the Surveyor inspected the medication room (1of 3) with Registered Nurse (RN) #1 and observed a locked box containing refrigerated controlled medications was not permanently...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure meals were prepared and served according to the planned written menu to meet the nutritional needs of the residents fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure pureed food items were blended to a smooth, lump free consistency to minimize the risk of choking or other complications for those res...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure the physician's plan of care for chopped meat was followed for 8 residents who had a physician's order for chopped mea...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0847
(Tag F0847)
Could have caused harm · This affected multiple residents
Based on interview, and record review, the facility failed to ensure the Binding Arbitration Agreement stated the resident or resident representative were not required to sign the binding arbitration ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
5. Review of medical diagnosis noted Resident #277 had hemiplegia and hemiparesis following cerebral infarction affecting left non-dominant side and dementia.
The admission Minimum Data Set (MDS) with...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to ensure dirty trash cans were stored away from the food storage racks; kitchen sink was free of leaks; the walk-in freezer floor was free of i...
Read full inspector narrative →
Nov 2022
4 deficiencies
3 IJ (3 affecting multiple)
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Report Alleged Abuse
(Tag F0609)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure injuries of unknown origin were reported to the Office of Lo...
Read full inspector narrative →
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Investigate Abuse
(Tag F0610)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure injuries of unknown origin were properly investigated for 2 ...
Read full inspector narrative →
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure professional standards of practice for fall protocols were f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to review and revise the care plan to meet the residents' needs for 1 (Resident #2) of 3 (Residents #1, #2 and #3) sampled residents who had a...
Read full inspector narrative →
Nov 2022
2 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** w. On 11/3/2022 at 2:09 p.m., the Surveyor asked the Social Director (SD), If a resident elopes, what are you supposed to do? Th...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. On 11/3/2022 at 12:55 p.m., the Surveyor asked Certified Nursing Assistant (CNA) #1, Who do you report any allegations of abu...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Arkansas facilities.
- • Multiple safety concerns identified: 4 life-threatening violation(s). Review inspection reports carefully.
- • 37 deficiencies on record, including 4 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Trinity Village Medical Center's CMS Rating?
CMS assigns TRINITY VILLAGE MEDICAL CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Arkansas, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Trinity Village Medical Center Staffed?
CMS rates TRINITY VILLAGE MEDICAL CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 48%, compared to the Arkansas average of 46%. RN turnover specifically is 70%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Trinity Village Medical Center?
State health inspectors documented 37 deficiencies at TRINITY VILLAGE MEDICAL CENTER during 2022 to 2025. These included: 4 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 33 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Trinity Village Medical Center?
TRINITY VILLAGE MEDICAL CENTER is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 94 certified beds and approximately 77 residents (about 82% occupancy), it is a smaller facility located in PINE BLUFF, Arkansas.
How Does Trinity Village Medical Center Compare to Other Arkansas Nursing Homes?
Compared to the 100 nursing homes in Arkansas, TRINITY VILLAGE MEDICAL CENTER's overall rating (1 stars) is below the state average of 3.1, staff turnover (48%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Trinity Village Medical Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Trinity Village Medical Center Safe?
Based on CMS inspection data, TRINITY VILLAGE MEDICAL CENTER has documented safety concerns. Inspectors have issued 4 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Arkansas. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Trinity Village Medical Center Stick Around?
TRINITY VILLAGE MEDICAL CENTER has a staff turnover rate of 48%, which is about average for Arkansas nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Trinity Village Medical Center Ever Fined?
TRINITY VILLAGE MEDICAL CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Trinity Village Medical Center on Any Federal Watch List?
TRINITY VILLAGE MEDICAL CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.