SILOAM HEALTHCARE, LLC




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Siloam Healthcare, LLC has received a Trust Grade of F, indicating significant concerns about the quality of care provided. With a state rank of #164 out of 218 facilities in Arkansas, they are in the bottom half, and #9 out of 12 in Benton County means there are only a few local options that are better. Although the facility is showing improvement, reducing issues from 9 in 2023 to 6 in 2025, it still has a long way to go. Staffing is average with a 3/5 rating, but the turnover rate is concerning at 53%, which is similar to the state average. There have been no fines reported, which is a positive aspect, but the RN coverage is lower than 81% of Arkansas facilities, raising concerns about oversight. Specific incidents include issues with food safety, such as unclean grease traps that could pose fire risks, and inadequate food storage practices that could lead to foodborne illnesses. While there are strengths, such as no fines and a slight improvement trend, families should weigh these against the serious issues the facility has faced.
- Trust Score
- F
- In Arkansas
- #164/218
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 53% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Arkansas facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 15 minutes of Registered Nurse (RN) attention daily — below average for Arkansas. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 36 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Arkansas average (3.1)
Below average - review inspection findings carefully
Near Arkansas avg (46%)
Higher turnover may affect care consistency
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 36 deficiencies on record
Jan 2025
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on interviews and record review, it was determined that the facility failed to ensure the Minimum Data Set (MDS) assessment was accurately completed for 1 (Resident #88) of 22 residents reviewed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to ensure physician order changes were immediately initiated for 1 (Resident #13) of 5 residents reviewed for anti-psychotic medications.
Th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** F689
Based on observations, record review, interviews, document review, and facility policy review, the facility failed to inves...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to assess resident for edema and administer prescribed, as needed medication, according to physician's orders for 1 (Resident #7) ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure a Facility-wide Assessment included pertinent information to determine what resources were allocated to care and to meet the needs o...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and facility document review, the facility failed to ensure that food was prepared in accordance with professional standards for food service safety by not keeping the...
Read full inspector narrative →
Dec 2023
7 deficiencies
1 IJ
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation and interview, the interdisciplinary team (IDT) failed to ensure 1 (Resident #29) of 1 sampl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview, the facility failed to ensure an order was obtained to administer oxygen therapy to 1 (Resident #94) of 1 sampled resident to minimize the potential...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview, the facility failed to ensure medications were stored in accordance with stat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation and interview, the facility failed to ensure resident's personal food and beverage items sto...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview, the facility failed to ensure infection control measures, including hand hygiene, was performed, before entering a resident room on contact isolation...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation and interview, the facility failed to maintain a safe, functional, sanitary, and homelike en...
Read full inspector narrative →
May 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the residents who were dependent on staff for personal hygiene were provided care to promote hygiene and dignity for 1...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure residents' fingernails were cleaned and trimmed to promote good personal hygiene and grooming for 2 (Residents #1 and ...
Read full inspector narrative →
Sept 2022
21 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the admission nursing assessment was documented completely to create a baseline care plan to enable staff to properly care for resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure razors were stored in a manner to prevent accidents or hazards for 1 (Resident #236) sampled resident. This failed prac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0808
(Tag F0808)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure physician ordered nutritional supplements and diet were provided for 1 (Resident #75) sampled resident who was to rece...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on observation and interview, facility failed to ensure all components of the Antibiotic Stewardship Program were completed for all infections and prescribed antibiotics. This failed practice ha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0888
(Tag F0888)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure COVID-19 vaccinations or exemptions were received for all employees working in facility and failed to ensure accurate and up-to-date...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure resident call lights were in reach for residents to be able to notify staff of their needs for 1 of 1 (R#62) sample selected residents...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview the facility failed to ensure a resident had the right to make a significant choice about his life in the facility to promote and facilitate self-det...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to ensure walls were in good repair, the courtyard decking was in good repair, and the facility was maintained a safe, clean, and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop/implement a Comprehensive Care Plan to enable staff to prop...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents were provided nail care for 3 (Resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure oxygen tubing and/or nebulizers were dated and stored in a storage bag when not in use to prevent infections for 2 (Re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected multiple residents
Based on observation, interviews, and record review the facility failed to ensure pain management was provided and pain medication was administered as ordered prior to wound care for 1 of 1 sampled re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure meals were prepared and served according to the planned written menu to meet the nutritional needs of the residents fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure food was prepared by methods that maintained appearance; hot foods were served hot and cold foods were served cold to ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure pureed food items were blended to a smooth, lump free consistency to minimize the risk of choking or other complications for residents...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure residents' meals were consistently served at regularly scheduled times to provide residents with a dependable eating s...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure COVID-19 screening of all person's entering fa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** .Based on interview and record review, the facility failed to ensure COVID-19 vaccinations were provided in a timely manner to r...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, record review, and interview, the facility failed to ensure foods stored in the freezer, refrigerator and dry storage area were covered, sealed and dated to minimize the potentia...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0569
(Tag F0569)
Minor procedural issue · This affected multiple residents
Based on interview and record review, the facility failed to ensure Medicaid recipient residents and/or their responsible parties were notified when their trust balance was within $200 of, or over, th...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0885
(Tag F0885)
Minor procedural issue · This affected most or all residents
Based on observation, interview, and record review, facility failed to inform residents, resident representatives, and families of new suspected or confirmed cases of COVID-19 cases in the facility by...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Arkansas facilities.
- • Multiple safety concerns identified: 1 life-threatening violation(s). Review inspection reports carefully.
- • 36 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • Grade F (38/100). Below average facility with significant concerns.
About This Facility
What is Siloam Healthcare, Llc's CMS Rating?
CMS assigns SILOAM HEALTHCARE, LLC an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Arkansas, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Siloam Healthcare, Llc Staffed?
CMS rates SILOAM HEALTHCARE, LLC's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 53%, compared to the Arkansas average of 46%.
What Have Inspectors Found at Siloam Healthcare, Llc?
State health inspectors documented 36 deficiencies at SILOAM HEALTHCARE, LLC during 2022 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 33 with potential for harm, and 2 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Siloam Healthcare, Llc?
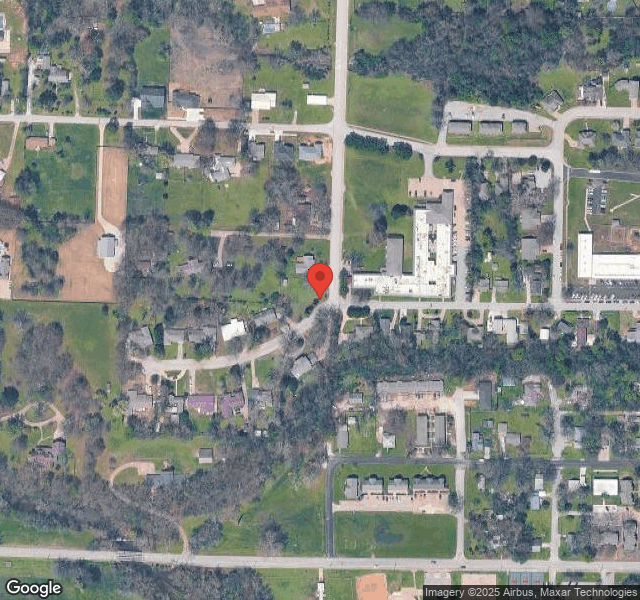
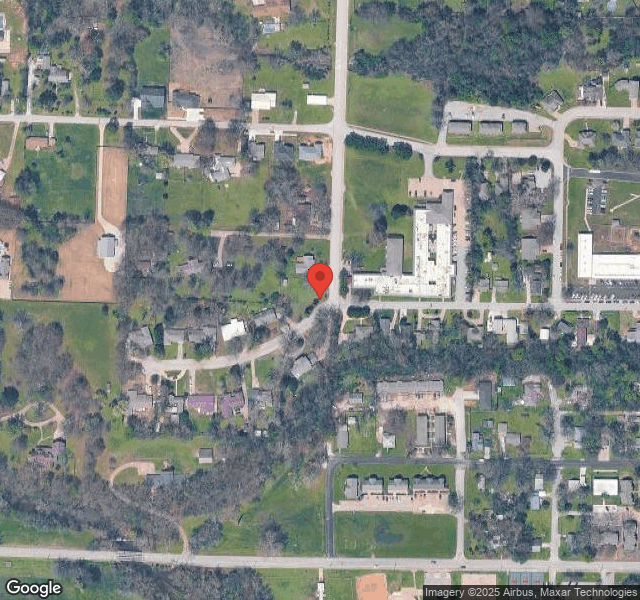
SILOAM HEALTHCARE, LLC is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by THE SPRINGS ARKANSAS, a chain that manages multiple nursing homes. With 120 certified beds and approximately 83 residents (about 69% occupancy), it is a mid-sized facility located in SILOAM SPRINGS, Arkansas.
How Does Siloam Healthcare, Llc Compare to Other Arkansas Nursing Homes?
Compared to the 100 nursing homes in Arkansas, SILOAM HEALTHCARE, LLC's overall rating (2 stars) is below the state average of 3.1, staff turnover (53%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Siloam Healthcare, Llc?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Siloam Healthcare, Llc Safe?
Based on CMS inspection data, SILOAM HEALTHCARE, LLC has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Arkansas. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Siloam Healthcare, Llc Stick Around?
SILOAM HEALTHCARE, LLC has a staff turnover rate of 53%, which is 7 percentage points above the Arkansas average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Siloam Healthcare, Llc Ever Fined?
SILOAM HEALTHCARE, LLC has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Siloam Healthcare, Llc on Any Federal Watch List?
SILOAM HEALTHCARE, LLC is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.