PARKVIEW JULIAN HEALTHCARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Parkview Julian Healthcare Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranked #1086 out of 1155 facilities in California, it falls within the bottom half, and at #13 out of 17 in Kern County, it is among the least favorable options in the area. While the facility's trend shows improvement, going from 27 issues in 2024 to 9 in 2025, the overall situation remains troubling. Staffing is a notable weakness, with a 53% turnover rate that exceeds the California average, contributing to a low staffing rating of 1 out of 5 stars. The facility has incurred $121,934 in fines, which is a concerning amount higher than 93% of California facilities, indicating ongoing compliance issues. Specific incidents of care failures include a resident who fell due to the facility's failure to follow their care plan, leading to serious injuries, and multiple residents not receiving trauma-informed care, causing distress. Although there is average RN coverage, the incidents reflect significant gaps in care that families should carefully consider.
- Trust Score
- F
- In California
- #1086/1155
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 53% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $121,934 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 20 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 94 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below California average (3.1)
Significant quality concerns identified by CMS
Near California avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
The Ugly 94 deficiencies on record
Aug 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Grievance and Complaints for one of three sampled residents (Resident 1) when the facility ...
Read full inspector narrative →
Jun 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to accommodate residents needs when call lights were not answering timely for one of three sampled residents (Resident 1). These failures had ...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow their policy and procedure (P&P) titled, Abuse Prevention and Prohibition Program, when the facility failed to:
1. Rep...
Read full inspector narrative →
Mar 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Comprehensive Care Plan
(Tag F0656)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow one of three sampled residents (Resident 1) care plan (perso...
Read full inspector narrative →
Mar 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Abuse Prevention and Prohibition Program, when the facility failed to:
1. Submit the SOC 34...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure an antibiotic (medication used to treat infections) order was given as ordered by the Medical Doctor (MD) for one of five sampled re...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow its policy and procedure (P&P) on assessment and management of resident weights for one of three sampled residents (Resident 1) when...
Read full inspector narrative →
Jan 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0553
(Tag F0553)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of three sampled residents (Resident 1) was involved in the comprehensive person-centered care planning process. This failure re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of three sampled resident (Resident 1) transportation was scheduled for doctor's appointment. This failure resulted in Resident ...
Read full inspector narrative →
Dec 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement a care plan for one of three sampled residents (Resident 1) when the facility did not monitor Resident 1 after a fire. This failu...
Read full inspector narrative →
Dec 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0573
(Tag F0573)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to:
1. Follow their policy and procedure (P&P) titled, Resident Access to PHI (protected health information), when three of four sampled resid...
Read full inspector narrative →
Dec 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure two of three sampled residents (Resident 1 and Resident 2) personal items were inventoried upon admission. This failur...
Read full inspector narrative →
Nov 2024
15 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Informed Consent, for one of two sampled residents (Resident 42) when his informed consent ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
2. During a concurrent observation and interview on 11/20/24 at 8:53 a.m. with Maintenance Technician (MT) 2 in Resident 62's room, a large patch of white drywall was seen between resident's bed and t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Dialysis Care for two of two sampled residents (Resident 67 and Resident 69) when:
1. One o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Pre-admission Screening and Resident Review (PASRR [federal requirement to help ensure that...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure adequate numbers of staff with certain skill set were available to meet one of two sampled resident (Resident 82) care plan needs. T...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow their policy and procedure (P&P) titled, Food Preference, when two of six sampled residents (Resident 24 and Resident ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0807
(Tag F0807)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide reasonable accommodations and follow the care plan for one of one sampled resident (Resident 48) to prevent symptoms ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Transfer and Discha...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed follow their policy and procedure (P&P) titled, Food Preparation when one of one sampled cooks (Cook 1) did not follow the facil...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to store, prepare, and maintain food in a sanitary manner when:
1. Food items were expired in one of one dry storage room.
2. O...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
2a. During a concurrent observation and interview on 11/20/24 at 8:40 a.m. with Maintenance Technician (MT) 2, in Resident 17's room, a space heater was at the Resident 17's bedside. MT stated, I don'...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure:
1. Six of 20 sampled residents (Resident 58, Resident 87, Resident 193, Resident 22, Resident 17, Resident 70) had a signed and dat...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled Smoking, for ten of ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During a concurrent interview and record review on [DATE] at 4:25 p.m. with DSD, RN 1's personnel file was reviewed. DSD stat...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to maintain an environment free of accident hazards for 12 of 22 sampled residents when:
1. One of one sampled resident (Residen...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected most or all residents
Based on interview and record review, facility failed to ensure the Director of Staff Development (DSD) had a minimum of two years of experience as a Licensed Nurse to qualify for the DSD position. Th...
Read full inspector narrative →
Jun 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure two of five sampled residents (Resident 1 and Resident 2) physician's orders were followed. This failure had the potential for Resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure behaviors were monitored for one of five sampled residents (Resident 1). This failure had the potential for Resident 1 to receive un...
Read full inspector narrative →
Apr 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents care planning meetings were completed timely for o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to administer ordered medications for one of three sampled residents (Resident1). This failure had the potential for adverse outcomes for Resi...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of three sampled residents (Resident 1) was provided safety to prevent injuries. This failure resulted in Resident...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of four sampled resident (Resident 1) attending physician (AP) and resident ' s representative (RR) were notified of alleged abu...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0675
(Tag F0675)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure two of three sampled residents (Resident 1 and Resident 2) received scheduled showers. This failure had the potential to result in u...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure suspected abuse was reported timely for one of two sampled residents (Resident 1). This failure had the potential for Resident 1 ' s...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow their policy and procedure titled, Privacy and Dignity and Catheter-Indwelling, Insertion of , when a urine collection...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow its policy and procedure on change of conditio...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to notify the responsible party (RP) when one of three sampled residents (Resident 1) had a change of condition. This failure had the potentia...
Read full inspector narrative →
Jul 2023
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0555
(Tag F0555)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to protect the resident's rights for four of 36 sampled residents (Resident 1, Resident 2, Resident 4, and Resident 6). These failures resulte...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to fully informed in advance for 29 of 36 sampled residents (Resident 3, Resident 4, Resident 5, Resident 6, Resident 7, Resident 8, Resident ...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure its residents were able to receive calls from outside sources. This failure resulted in violation of residents' rights...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of four sampled residents (Resident 1) personal belongings were safeguarded. This failure resulted in Resident 1 to have missing...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to maintain the dish machine (a dishwasher for commercial use that has high temperature water capabilities for thorough sanitati...
Read full inspector narrative →
May 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of three sampled resident (Resident 1) was assisted with toileting. This failure had the potential to result in Resident 1 not b...
Read full inspector narrative →
Apr 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the outside patio areas were safe for the residents. This failure had the potential for accidents and injuries.
Findin...
Read full inspector narrative →
Apr 2023
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a notice of transfer or discharge was sent to the State Long...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed ensure the discharge process was thoroughly followed for five of ten s...
Read full inspector narrative →
Apr 2023
19 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0699
(Tag F0699)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow their policy and procedure (P&P), titled Traum...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed follow their policy and procedure titled Catheter-Indwelling, Insertion of, when a urine collection bag (drains urine from the b...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure titled Change of Condition Notification [COC], when the physician was not notified of a COC for one of fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Abuse Prevention and Prohibition Program, to report resident to resident abuse to the State...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the risks, benefits, and alternatives (RBAs) of leaving the facility Against Medical Advice (AMA) were explained by the physician fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Transfer and Discharge, when the facility did not send a notice of transfer to the ombudsma...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to complete and submit comprehensive Annual Minimum Data Set (MDS- standardized assessment tool) assessments in a timely manner for five of th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to accurately complete the Minimum Data Set (MDS-a standardized assessment tool) for two of 5 sampled residents (Resident 85 and Resident 41)....
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During an observation on 4/3/23, at 12:07 PM, in the dining room, Resident 57 was being aggressive towards staff and other re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of 5 sampled residents (Resident 42) was placed on a bowel and bladder (B&B) training program to maintain or improve her urinary...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure:
1. An order for a therapeutic (to cure or restore to health) nutritional supplement (used to increase calories and p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Behavior-Management, for completing a gradual dose reduction (GDR) for one of three sampled...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During a concurrent observation and interview on 4/3/23, at 10:17 AM, with Resident 76, in Resident 76's shared room, water was ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to submit Quarterly Minimum Data Set (MDS- a standardized assessment tool) in a timely manner for four of 13 sampled residents (Resident 83, R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow its Policy and Procedure (P&P) titled, Medication Storage and Labeling, for monitoring the receipt discontinued contro...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
2. During an observation on 4/3/23, at 6:24 AM, empty IV bag with tubing still attached was noted to be hanging from an IV pole inside Resident 417's room. The bag indicated it was 100 milliliters (ml...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow the menu as planned for therapeutic diets when:
1. The planned menu for a mechanical soft diet order was not followed...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure safe food handling and a sanitary kitchen envi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to follow their policy and procedure (P&P) titled, Infection Prevention and Control Program, when the facility did not:
1. Have ...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide a clean bed for one of three sampled residents (Resident 1). This failure resulted in Resident 1 sleeping in a blood-...
Read full inspector narrative →
Feb 2023
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Comprehensive Care Plan
(Tag F0656)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop and implement a care plan for one of three sampled resident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain a safe environment and follow its plan of correction for residents at risk for falls and/or elopement when three of ...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure new interventions were implemented for one of three sampled residents (Resident 1) after each subsequent fall. This had the potentia...
Read full inspector narrative →
Feb 2020
23 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
Based on observation, interview, record review, the facility failed to address the needs of one of one sampled resident (Resident 25), with unplanned weight loss, when:
1. Physician orders (PO) were n...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure one of 52 sampled residents (Resident 75) was provided a call light in order to summon staff. This failure had the potential to result...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the Minimum Data Set (MDS-resident assessment tool) assessme...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. During an interview on 2/12/20, at 2:39 PM, with Resident 52, Resident 52 stated, she was not using her continuous positive a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the Activity Department maintained activity programs for two of two sampled residents (Resident 76 and Resident 104). ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow its policy and procedure (P&P) on prn (as needed) pain medication for one of 52 sampled residents (Resident 97) when prn pain medica...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow its' policy and procedure (P&P) for nine of nine residents (Resident 6, Resident 25, Resident 34, Resident 42, Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop, maintain and implement a procedure to ensure Gradual Dose Reduction (GDR) recommendations were acted upon in a timely manner for t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of 52 sampled residents (Resident 25) was free from unnecessary medications. This failure had the potential to result in Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a Gradual Dose Reduction (GDR) for a psychoactive medication (drug that affects brain activities associated with mental processes an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure an intravenous (IV) medication administered was labeled for one of one sampled resident (Resident 91). This failure ha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0924
(Tag F0924)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to ensure corridor handrails were in good condition and secured to the w...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure the quarterly Minimum Data Set (MDS, resident assessment tool) Assessments for 12 of 12 sampled residents (Resident 6, Resident 1, R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to develop, maintain, and implement a person-centered care plan (CP) for one of 52 residents (Resident 25). This failure had the potential to ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure medications administered were documented for three of three sampled residents (Resident 38, Resident 76, and Resident 79). This fail...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow their policy and procedure (P&P) on smoking for two of two sampled residents (Resident 52 and Resident 59). This failu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to provide competency skill assessments for licensed staff nurses. This failure had the potential of not having a competent staff to provide a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to:
1. Complete a performance review of each Certified Nurses' Assistant (CNA) every 12 months.
2. Provide 12 hours of inservice education for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow manufacturers' recommendations and the facility's policies and procedures (P&P) regarding storage of perishable food i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
2. During a concurrent observation and interview on 2/10/20, at 2:20 PM, in C wing, with DSD, in C wing, DSD confirmed the clean resident laundry on the bottom shelf of the laundry cart was not covere...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure regular inspections of bed frames, mattresses, and side rails for four of 4 residents' (Resident 80, Resident 83, Resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to:
1. Provide functioning oxygen regulators (equipment r...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure the QAPI (Quality Assurance and Performance Improvement) quarterly meetings were attended by the Medical Director (MD), the Administ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 4 harm violation(s), $121,934 in fines, Payment denial on record. Review inspection reports carefully.
- • 94 deficiencies on record, including 4 serious (caused harm) violations. Ask about corrective actions taken.
- • $121,934 in fines. Extremely high, among the most fined facilities in California. Major compliance failures.
- • Grade F (5/100). Below average facility with significant concerns.
About This Facility
What is Parkview Julian Healthcare Center's CMS Rating?
CMS assigns PARKVIEW JULIAN HEALTHCARE CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Parkview Julian Healthcare Center Staffed?
CMS rates PARKVIEW JULIAN HEALTHCARE CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 53%, compared to the California average of 46%. RN turnover specifically is 64%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Parkview Julian Healthcare Center?
State health inspectors documented 94 deficiencies at PARKVIEW JULIAN HEALTHCARE CENTER during 2020 to 2025. These included: 4 that caused actual resident harm and 90 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
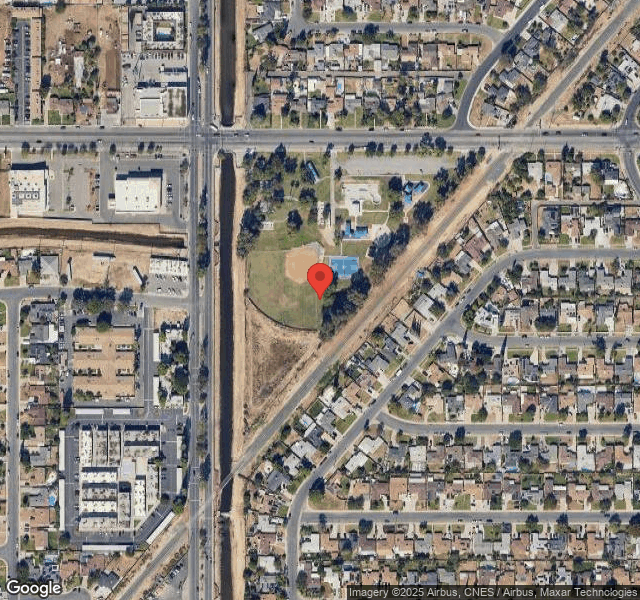
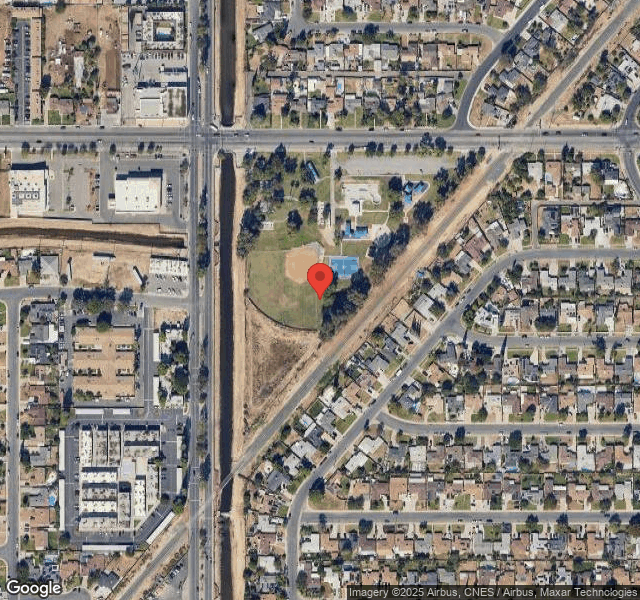
Who Owns and Operates Parkview Julian Healthcare Center?
PARKVIEW JULIAN HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 99 certified beds and approximately 85 residents (about 86% occupancy), it is a smaller facility located in BAKERSFIELD, California.
How Does Parkview Julian Healthcare Center Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, PARKVIEW JULIAN HEALTHCARE CENTER's overall rating (1 stars) is below the state average of 3.1, staff turnover (53%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Parkview Julian Healthcare Center?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Parkview Julian Healthcare Center Safe?
Based on CMS inspection data, PARKVIEW JULIAN HEALTHCARE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Parkview Julian Healthcare Center Stick Around?
PARKVIEW JULIAN HEALTHCARE CENTER has a staff turnover rate of 53%, which is 7 percentage points above the California average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Parkview Julian Healthcare Center Ever Fined?
PARKVIEW JULIAN HEALTHCARE CENTER has been fined $121,934 across 3 penalty actions. This is 3.6x the California average of $34,298. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Parkview Julian Healthcare Center on Any Federal Watch List?
PARKVIEW JULIAN HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.