THE ORCHARDS POST-ACUTE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
The Orchards Post-Acute in Bakersfield, California, has a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #1134 out of 1155 facilities in California places it in the bottom half, and at #15 out of 17 in Kern County, only one local option is better. While the facility’s overall issues have decreased from 35 in 2024 to 22 in 2025, the trend is improving but still indicates ongoing problems. Staffing is rated at 3 out of 5 stars, with a turnover rate of 35%, which is better than the state average, suggesting that some staff remain for a longer period. However, there are serious concerns, including incidents where a resident's feeding tube was improperly managed, leading to hospitalization for aspiration pneumonia, and inadequate wound care that caused infections and increased pain for other residents.
- Trust Score
- F
- In California
- #1134/1155
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- 35% turnover. Near California's 48% average. Typical for the industry.
- Penalties ⚠ Watch
- $21,635 in fines. Higher than 85% of California facilities, suggesting repeated compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 30 minutes of Registered Nurse (RN) attention daily — about average for California. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 97 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (35%)
13 points below California average of 48%
Facility shows strength in fire safety.
The Bad
Below California average (3.1)
Significant quality concerns identified by CMS
11pts below California avg (46%)
Typical for the industry
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 97 deficiencies on record
Apr 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of five residents' restrooms (room [ROOM N...
Read full inspector narrative →
Mar 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to follow their policy and procedure on Abuse, Neglect, Exploitation or Misappropriation- Reporting and Investigating to immediately protect a...
Read full inspector narrative →
Mar 2025
19 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure one of 24 sampled resident's bathrooms (Resident 72) was clean and sanitary. This failure had the potential to spread infections and/o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to have completed quarterly smoking assessments for two of two sampled ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement the plan of care for one of eight sampled residents (Resident 91) fall precaution. This failure had the potential f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to check blood pressure prior to administration of blood pressure medication for one of one sampled resident (Resident 8). This failure had the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide catheter (a thin, flexible tube inserted into the bladder to drain urine) care for one of two sampled residents (Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow their policy and procedures (P&P) titled, Oxyg...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the Social Services Department documented and followed up on one of three sampled residents' (Resident 93) eyeglasses. This failure ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure medications were available to administer when Licensed Nurse did not reorder medications timely, notify physician of unavailable med...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to have a functional call light system for one of 52 sampled residents (Resident 99). This failure had the potential for Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of 58 residents' rooms (room [ROOM NUMBER]...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure staff were communicating in a language three of three sampled residents (Resident 74, Resident 88, and Resident 110) w...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to obtain and complete informed consents for psychotropic (drugs that affect a person's mental state) medication for three of 29 sampled resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
During a review of Resident 128's Physician's Discharge Summary (PDS), dated 12/10/24, the PDS indicated Resident 128 was discharged on 12/10/24 to home.
During a concurrent interview and record revi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to have daily completed Direct Care Service Hours Per Patient Day (DHPPD) for the month of January 2025 to February 21, 2025. This failure had...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to complete annual performance evaluations for two of five sampled Certified Nurse Assistants (CNA 1 and CNA 2). This failure had the potentia...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the monthly Medication Regimen Review (MRR- a review of all ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
During an observation on 3/10/25 at 11:23 a.m. in Resident 4's room, Resident 4's bedside table had a Calmoseptine (treatment for skin irritation) cream and a bottle of antifungal powder.
During an i...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to:
1) Ensure three of three sampled clean linen carts were in good repair.
2) Follow the manufacturer's guidelines on how to di...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) on Surveillance for Infections when:
1) There were no documented signs/symptoms of the infections a...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to readmit one of three sampled residents (Resident 1) after hospitali...
Read full inspector narrative →
Dec 2024
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Tube Feeding
(Tag F0693)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed follow their policy and procedure (P&P) titled, Enteral Feedings (a me...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure professional standards were followed when:
1. Medications were not administered according to physician's order for one of three samp...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure two of three sampled staff members (Licensed Vocational Nurse [LVN] 2 and Certified Nursing Assistant [CNA] 2) were competent in car...
Read full inspector narrative →
Sept 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their Five-Day Investigation Report to implement a follow-up monitoring for one of seven sampled residents (Resident 1). This failur...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide wound treatment as ordered by the physician for one of three sampled residents (Resident 1). This failure had the potential to resu...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide foley catheter (a device that drains urine (pee) from the urinary bladder into a collection bag outside of your body ...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow their policy and procedure titled, Abuse, Neglect, Exploitation, or Misappropriation-Reporting Investigating for one o...
Read full inspector narrative →
Jun 2024
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to ensure the kitchen was maintained clean and sanitary. This failure ha...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement an effective pest control program for three...
Read full inspector narrative →
Jun 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, record review, the facility failed to provide nail care and hand hygiene for one of the five sampled residents (Resident 1). This failure had the potential for Residen...
Read full inspector narrative →
May 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the Physician was notified timely when one of three sampled residents (Resident 1) fell. This failure resulted in a delay of Physici...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure medications were administered as ordered by the physician for one of three residents (Resident 2). This failure resulted in Resident...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide showers to one of three sampled residents (Resident 1). Thi...
Read full inspector narrative →
Feb 2024
20 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
2. During an interview on 2/15/24 at 4:39 p.m. with Assistant Director of Nursing (ADON), ADON stated a Level I PASRR needed to be resubmitted to obtain a Level II PASRR.
During a review of Resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a neurological assessment (checking motor and sensory function following possible head trauma) was not completed after an unwitnesse...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure nail care was provided for one of 30 sampled residents (Resident 61). This failure had the potential to result in skin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
2. During an interview on 2/12/24 at 9:59 a.m. with Resident 88, Resident 88 stated he had lost weight, more than 10 pounds (Lbs-unit of measurement of mass).
During a review of Resident 88's Brief In...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure behavior monitoring was accurately completed according to physicians' orders for one of three sampled residents (Resident 605). This...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to communicate to social services when the resident lost his ability to make medical decisions and did not have effective family representatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled Adverse Consequences and Medication Errors for one of one sampled resident (Resident 604). T...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure:
1. Multi dose medication was labeled after being opened.
2. An unlabeled medication was properly discarded.
These fa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure dishware was stored safely, and food was stored and prepared safely when:
1.
The clean plate holder area was observed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the medical record accurately reflected the behavioral health concerns for two of two sampled residents (Resident 29 and Resident 60...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to assess, evaluate, and provide a call system appropria...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure call lights were within reach for three of 78 sampled residents (Resident 37, Resident 15, and Resident 64). This fail...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
During an observation, interview, and record review, the facility failed to maintain a clean and sanitary environment for six of six sampled residents (Resident 42, Resident 52 Resident 88, Resident 9...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to complete and submit comprehensive Annual Minimum Data Set (MDS- standardized assessment tool) assessments annually for six of six sampled r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
Based on interview, and record review, the facility failed to ensure MDS (Minimum Data Set - assessment tool) quarterly (every three months) assessments were completed for four of four sampled residen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Care Plans, Compreh...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure one of four sampled residents (Resident 58) dialysis (procedure to mechanically remove waste products and excess fluid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure an effective Quality Assessment and Assurance program was in place, when deficient practices still occurred after bein...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain a hazard-free environment when:
1. The over...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to implement infection control practices when:
1. Hand hygiene was not provided to residents prior to eating in the dining room...
Read full inspector narrative →
Feb 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to provide warm water for showers/bathing and adequate water pressure for four of four sampled residents (Resident 1, Resident 2,...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0914
(Tag F0914)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of three sampled residents (Resident 2) had a completely covered window blinds for privacy. This failure had the p...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure three of four sampled residents (Resident 1, Resident 2, and...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement its policy and procedure (P&P) titled Administering Medications for one of three sampled residents (Resident 1). This failure had...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to administer pain medication according to physician's order for one of three sampled residents (Resident 1) for two days. This failure result...
Read full inspector narrative →
Oct 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based interview and record review, the facility failed to ensure one of three sampled residents (Resident 2) received medications as ordered by the attending physician (AP). This failure resulted in R...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide sufficient staffing to accommodate residents needs by not answering call lights timely for two of three sampled resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to accommodate two of three sampled residents (Resident 1 and Resident 2) food allergies and preferences. This failure had the p...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to provide adequate needed supplies for two of three sampled residents (Resident 1 and Resident 2). This failure had the potential to result i...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow its policy titled Abuse Investigation and Reporting for one of three sampled residents (Resident 1). This failure had the potential ...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide adequate supervision for two of three sampled residents (Resident 1 and Resident 2) to prevent a resident to resident altercation. ...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow its policy and procedure on Administering Medications for one of three sampled residents (Resident 1) when a cup of medication was n...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement their planned intervention to provide one of three sampled residents (Resident 1) a call bell to minimize the chanc...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement their policy on Abuse Investigation and Reporting when th...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to report an allegation of abuse within 24 hours to the California Dep...
Read full inspector narrative →
May 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure wound treatment was completed and documented for one of four sampled residents (Resident 1). This failure had the potential for wors...
Read full inspector narrative →
May 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of three sampled residents (Resident 1) diet order was followed when Resident 1 was not provided a double protein ...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure two of three sampled residents (Resident 1 and Resident 2) received the enteral feedings [way of delivering nutrition directly to yo...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to carry out a physician ' s order in a timely manner for one of three sampled residents (Resident 1). This failure had the potential to affec...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to perform assessments per their stated policy, on 1 of 1 sampled resident (Resident 1), for a full 72 hours after Resident 1 fell and experie...
Read full inspector narrative →
Jan 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure two of three sampled residents (Resident 1 and Resident 2) received their scheduled showers. This failure resulted in unmet care nee...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure wound care was consistently administered for one of three sampled residents (Resident 3). This failure had the potential for infecti...
Read full inspector narrative →
Dec 2022
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure:
1. Wound (pressure injury) care was provided and weekly wo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure 40 of 40 Licensed Nurses (Registered Nurse [RN], RN 1, RN 2, RN 3, RN 4, RN 5, Director of Nursing [DON], Assistant Director of Nurs...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure wound care was provided for 10 of 33 sampled residents (Resident 5, Resident 6, Resident 13, Resident 16, Resident 17,...
Read full inspector narrative →
Nov 2022
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to:
1. Provide a clean environment for four of four samp...
Read full inspector narrative →
Apr 2022
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to maintain the dignity of one of 53 sampled residents (Resident 116) when Resident 116 was not provided timely incontinence (inability to sen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to promote self-determination for one of 53 sampled residents (Resident 116) when choices were not honored for shower times. This failure resu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
3. During a review of Resident 30's Medical Record (MR), the MR contained no documentation the facility provided written information showing whether Resident 30 had formulated an advance directive, wh...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the physician and responsible party (RP) were notified of an unplanned significant weight loss for one of four sampled residents (Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the accuracy of an oral assessment for one of 53 sampled residents (Resident 50). This failure had the potential for R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop and implement a coordinated plan of care with the hospice provider for one of five sampled residents (Resident 122). This failure h...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide care and services to ensure one of 37 sampled...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure:
1. Nutrition orders and consumption of therapeutic (to cure or restore to health) nutritional supplements were accura...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure narcotics (highly regulated, highly addictive drugs) were reconciled (inventoried) each shift for two of five medicati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0810
(Tag F0810)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of 10 sampled residents (Resident 110) was provided special adaptive equipment as ordered for liquids with meals. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to maintain an accurate antibiotic stewardship program
(coordinated program that promotes the appropriate use of drugs used to treat infectio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain a wheelchair in safe operating condition for one of 14 sampled residents (Resident 100). This failure had the potent...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain a safe environment for one of 53 sampled residents (Resident 10) when the flooring at the entrance of the Resident 1...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During a concurrent observation and interview on 4/14/22, at 9:06 AM, with Resident 2, Resident 2's bathroom was observed not...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure food brought in from outside sources was stored in a safe and sanitary manner. This failure had the potential to place...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure safe food handling and sanitation when:
1. There were general unsanitary conditions in the kitchen including the dry f...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 35% turnover. Below California's 48% average. Good staff retention means consistent care.
- • 97 deficiencies on record, including 2 serious (caused harm) violations. Ask about corrective actions taken.
- • $21,635 in fines. Higher than 94% of California facilities, suggesting repeated compliance issues.
- • Grade F (28/100). Below average facility with significant concerns.
About This Facility
What is The Orchards Post-Acute's CMS Rating?
CMS assigns THE ORCHARDS POST-ACUTE an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is The Orchards Post-Acute Staffed?
CMS rates THE ORCHARDS POST-ACUTE's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 35%, compared to the California average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at The Orchards Post-Acute?
State health inspectors documented 97 deficiencies at THE ORCHARDS POST-ACUTE during 2022 to 2025. These included: 2 that caused actual resident harm and 95 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates The Orchards Post-Acute?
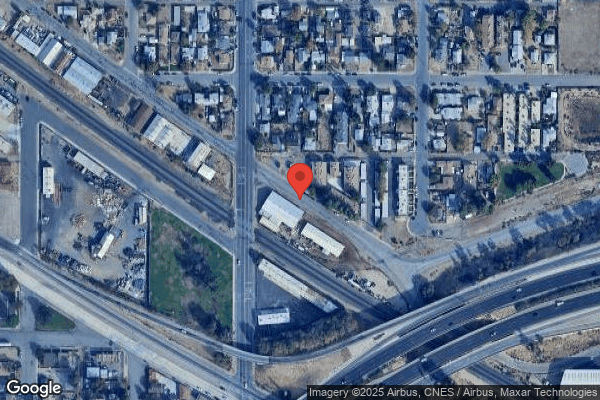
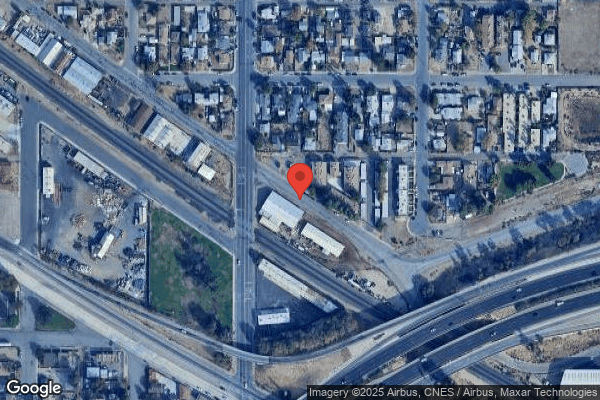
THE ORCHARDS POST-ACUTE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by LINKS HEALTHCARE GROUP, a chain that manages multiple nursing homes. With 150 certified beds and approximately 139 residents (about 93% occupancy), it is a mid-sized facility located in BAKERSFIELD, California.
How Does The Orchards Post-Acute Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, THE ORCHARDS POST-ACUTE's overall rating (1 stars) is below the state average of 3.1, staff turnover (35%) is significantly lower than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting The Orchards Post-Acute?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is The Orchards Post-Acute Safe?
Based on CMS inspection data, THE ORCHARDS POST-ACUTE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at The Orchards Post-Acute Stick Around?
THE ORCHARDS POST-ACUTE has a staff turnover rate of 35%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was The Orchards Post-Acute Ever Fined?
THE ORCHARDS POST-ACUTE has been fined $21,635 across 2 penalty actions. This is below the California average of $33,295. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is The Orchards Post-Acute on Any Federal Watch List?
THE ORCHARDS POST-ACUTE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.