SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure resident comfort is achieved in accordance wit...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure resident comfort is achieved in accordance with comprehensive person-centered care plan when physician's order of No turning on Right Side was not implemented for one of 33 sampled residents (Resident 33).
The deficient practice resulted in Resident 33 having a headache and discomfort, and had the potential to cause further brain tissue injury and increase intracranial pressure (pressure inside the skull).
Findings:
Review of Resident 33's History and Physical Report dated 12/13/21, indicated, Resident 33 was admitted to the facility on [DATE] with the following diagnoses:
i. Right-sided hemorrhagic stroke (a condition in which a blood vessel breaks and bleeds into the brain),
ii. Right hemicraniectomy on 6/26/19 (a surgical procedure where a large flap of the skull is removed to give space for the swollen brain to bulge and reduces the intracranial pressure),
iii. Seizure (a sudden, uncontrolled electrical disturbance in the brain) and
iv. Constantly recurring left-sided pain.
The Minimum Data Set (MDS, a resident assessment tool) comprehensive assessment dated [DATE], indicated Resident 33 was cognitively intact. Under Section J 400, the pain assessment indicated, Resident 33 was frequently in pain and was receiving routine and as needed pain medications for pain management.
During an observation on 2/10/22, at 10:33 AM, a sign posted on the wall by the left side of the bed indicated, NURSING ALERT (PLEASE READ BEFORE GIVING CARE). Another sheet was attached after the nursing alert sign, it indicated, DO NOT TURN PATIENT TO THE RIGHT SIDE. During a concurrent interview, Resident 33 stated she reminded Certified Nursing Assistant (CNA) 4 not to turn her on the right side but continued to do so. Resident 33 stated, It happened during diaper change. I was pushed to the left side and right side. My left side does not work (referring to weakness on left side of the body) and it (left side of the body) hurts all the time. I have something on my head (pointing at the bulging area on the right side of her head).
The History and Physical Report dated 12/13/21, indicated, .Her craniotomy on the right side is without the scalp plate and she is wearing a protective helmet at the movement . At present, the patient's main issue is her chronic pain on the left side of her body, for which she was referred to Pain Clinic. She was also referred to Neurosurgery Specialty Clinic in (Name of facility) and (Name of facility) Neurosurgery Department to cover for her right craniotomy with a scalp plate . Head: Bulging of the right side of the head. Soft, nontender, no erythema, no discharge .
During an interview on 2/10/22, at 10:42 AM, Charge Nurse (CN) 2 stated Resident 33 had a right hemicraniectomy and should not be turned on her right side. CN 2 explained that a Nursing Alert sign of do not turn patient on right side was posted on the wall as a reminder for the staff providing care for Resident 33. CN 2 confirmed during the evening shift on 5/19/21, Resident 33 complained of a headache after CNA 4 turned her on the right side. CN 2 stated, She's not supposed to be turned on her right side. There's no bone in there (referring to the bulging area on the right side of her head).
During an interview on 2/10/22, at 2:35 PM, Resident 33 was asked how she felt after she was turned on her right side on 5/19/21, Resident 33 stated, I was in pain. There's a sign do not turn on right side but she kept going. My right side hurt. My head hurt.
During an interview on 2/14/22, at 4:38 PM, CNA 4 stated she was told by Resident 33 not to turn on her right side during care on 5/19/21. CNA 4 acknowledged she did not know Resident 33 cannot be turned on her right side. CNA 4 stated, I did not see the note posted on the wall. I was told by other CNAs not to turn on her right side after she complained of pain on the head. I was not aware of the care plan. I have not read her care plan.
Review of the Patient Care Notes, dated 5/20/21, indicated, .CNA (referring to CNA 4) pushed her on her R (right) side even when she's telling the CNA (referring to CNA 4) to stop & don't turn on the right side . Pt. c/o (patient complained of) slight pain on her R side, the head & shoulder.
Review of the 5-DAY INVESTIGATION SUMMARY, dated 5/24/21, indicated, .On 5/20/2021 at approximately 0830, (Resident 33) reported to the charge nurse . the CNA (Certified Nursing Assistant) from the night before (5/19/2021), pushed her hard to the right side lying position even if she had just told her that she did not want to be turned . (Resident 33) mentioned to CNA that there are instructions posted that she cannot be turned to the right . after CNA pushed her, she felt pain on the right shoulder and right side of neck .
Review of Resident 33's Physician's Orders, dated May 2021, indicated, No turning on Right Side Q (every) SHIFT ordered on 12/5/19.
Review of Resident 33's care plan indicated the following:
a. The Activities of Daily Living (ADL) care plan, started on 12/5/19 and revised on 6/2/21, indicated, .13. No turning on right side as ordered.
b. The Pain care plan, started on 12/8/19 and revised on 6/2/21, indicated, Potential for pain and discomfort r/t (related to) Right hemorrhagic stroke . right hemi craniotomy with left side hemiplegia (paralysis of one side of the body), chronic left side pain . 1. Check pain level Q (every) shift and medicated per pain scale . Check patient 30-60 minutes after medication if relieved or not. 2. Repositioning/turning for comfort to relieve pressure .
Review of the facility's policy and procedure titled, Plan of Care, dated 9/2019, indicated, . (Name of the facility) must develop and implement a baseline care plan for each resident that includes the instructions needed to provide effective and person-centered care of the resident that meets professional standards of quality care . 1. The comprehensive plan of care shall include: a. The frequency at which care, services, treatments, and interventions will occur b. The IDT member(s) responsible for providing the care, treatment, interventions . d. Current needs, problems, goals, care, treatment and services . 3. The evaluation of the resident's progress is made based upon the care plan goals and the resident's plan of care, treatment and services.
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0688
(Tag F0688)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide preventative treatment, equipment, and servic...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide preventative treatment, equipment, and services to maintain, improve, and prevent further decline in range of motion (ROM) and/or mobility when:
1. The physician's order for hand splint and rolled bath blanket at lumbar spine were not implemented for Resident 33. The deficient practice resulted in pain, further increase in contractures, and decline in ROM for Resident 33.
A contracture is a condition of shortening and hardening of muscles, tendon or other tissue, often leading to deformity and rigidity of joints which limit and interfere with daily functioning.
2. The Physical Therapist (PT) recommendation to ambulate with staff supervision was not implemented for Resident 46. The deficient practice could potentially contributed to Resident 46's decline in range of motion, mobility and pressure injuries on left and right foot.
3. The physician's order for hand splint was not implemented for Resident 44. The deficient practice could potentially worsen the stiffness of Residdent's 44 hands and further decline in ROM.
4. Residents 65 and 127 missing splints were not promptly replaced. The deficient practice could potentially worsen the contractures and decline in ROM for Resident 65 and Resident 127.
5. The physician's order for range of motion exercise was not implemented for Resident 76. The deficient practice could potentially resulted in pain, further increase in contractures, and decline in ROM for Resident 76.
6. There was no evidence Resident 111's private caregivers was given education and training in performing ROM excersice and the use of Active Passive Trainer (APT, a unique exercise rehabilitation trainer for the upper or lower limbs) machine to aid in improving the ROM. In addition, there is no evidence a physician's order was obtained, an assessment and care plan were completed prior to the use of APT machine. The deficient practice could potentially contribute in further pain and increase in contractures of Resident 111.
7. The physician's order for hand roll was not implemented for Resident 66. This deficient practice had the potential for Residents 66's contractures to worsen and cause further decline in ROM.
A hand roll is a rubber device or rolled washcloth used to maintain joint positioning and further prevent joint deformity.
8. PT and Occupational Therapy (OT) initial and/or quarterly evaluation assessment was not completed for Resident 100, 11, and 133. The deficient practice could result residents not receiving the proper services or treatment to address their needs.
9. Resident-centered and individualized ROM exercises was not provided in accordance to facility policy.
The deficient practice prevents the residents from attaining their maximum functional potential and from achieving or maintaining their highest practicable physical, mental, and psychosocial well-being.
Findings:
1A. Resident 33 was admitted on [DATE] with diagnoses including stroke, hemiplegia (paralysis of one side of the body) and chronic pain (persistent pain that lasts weeks to years).
Review of Resident 33's history and physical (H&P) report dated 12/13/21 indicated, . The patient's physical condition has been stable for the last 2 years. The patient was able to participate in her physical therapy and occupational therapy program. She continues to require assistance . Has complaints of chronic left-sided continues pain . EXTREMITIES: Weak left upper extremity and left lower extremity secondary to CVA (cerebrovascular accident, also known as stroke). Good range of motion on the right upper extremity and right lower extremity .
Review of Resident 33's physician's order for May 2022 indicated the following orders:
i. 5/29/21 - Continue OOB (out of bed) daily. PROM LUE/LLE daily if patient allows.
ii. 9/16/21 - OT order: Place rolled bath blanket at lumbar spine when up in wheelchair.
iii. 10/18/21 - OT order: Left hand splint wearing schedule ON during the day when up in wheelchair and PRN (as needed) per pt (patient) preference to decrease loss of ROM.
iv. 4/30/22 - Clarification PT order cont. (continue) 1x1 month for 1 month include there-ex (therapeutic exercise), there-act (therapeutic activity), neuromuscular ex due to generalized weakness.
During an observation on 5/2/22, at 10:06 AM, in the activity room, Resident 33 was sitting in a wheelchair with the left arm resting on the armrest. Resident 33's left hand and fingers were bent and curled inward. Resident 33 did not have a splint on the left hand and did not have a rolled bath blanket to support the lumbar spine During concurrent interview, Resident 33 stated she's been having pain on the left side of her body. Resident 33 was observed tearing up while verbalizing, The pain never goes away. Resident 33 acknowledged she's been given pain medications and stated, It's not helping my pain.
During an interview with Licensed Vocational Nurse (LVN) 6 on 5/2/22 at 2:15 PM, LVN 6 stated Resident 33 has pain on her left side of the body and is on pain management which includes, repositioning and ROM. LVN 6 also stated Resident 33 has a splint on the right leg and left hand PRN (as needed).
During an interview with the Rehab Staff (RS) on 5/3/22, at 11:05 AM, RS stated, Certified Nursing Assistant (CNA) supposed to apply the splint to the resident when she's up on a wheelchair but there are times when Resident 33 does not want to wear the splint. RS also explained that ROM should be done during ADLs (activities of daily living) and stated Usually it's not done.
During an observation on 5/4/22 at 11:10 AM, in the activity room, Resident 33 was sitting in a wheelchair with the left arm/hand resting on the arm rest. Resident 33's left hand and fingers were bent and curled up. During observation, there was no hand splint on Resident 33's left hand and no rolled bath blanket on her lower back.
During an interview with Certified Nursing Assistant (CNA) 5 on 5/4/22 at 11:50 AM, CNA 5 stated, She (Resident 33) has no splint. I'm not sure if she has a splint. CNA 5 also stated he provides 5 to 8 minutes of ROM exercises for both the upper and lower extremities for Resident 33 during ADL care such as dressing. CNA 5 added that the ROM exercises were not fully performed due to Resident 33's constant complaints of pain on the left side arm and hand.
Review of Resident 33's care plan for ADL Functional/Rehabilitation Potential last revised on 2/23/22 did not include the use of hand splint and range of motion exercise.
During an interview on 5/4/22, at 11:56 AM, LVN 6 acknowledged the care plan for ADL Functional/Rehabilitation Potential did not include the use of hand splint and range of motion exercises.
During an interview with Resident 33's Responsible Party (RP) on 5/4/22, at 2:31 PM, the RP stated, She's (Resident 33) not getting enough therapy. She's only doing standing in parallel bars once a week and her toes started to curl up. She needed more assistance than before. She's deteriorating and her quality of life is not improving at all.
During an interview with CNA 13 on 5/4/22, at 2:50 PM, CNA 13 stated, She's (Resident 33) total care. She declined a little. She complained of pain when putting on the splint.
Review of Resident 33's progress notes from the pain clinic dated 3/2/22 indicated, .Patient reports she gets PT 1x/week and states standing up is the only time she feels ok. She mentions she has worsening spasticity throughout the left side . She reports she doesn't sleep well, either, as a result of pain . Assessments . May have chronic intractable pain on left side of her body due to spasticity vs. central pain . Treatment . 1d. Consider increasing tizanidine (used to treat muscle spasm) to 4 mg po BID (milligrams by mouth twice a day) as patient reports worsening spasms . 2. Mobilize with PT as much as possible and HEP (home exercise program) .
Review of Resident 33's Minimum Data Set (MDS, an assessment tool) dated 11/30/21 indicated, Resident 33 required extensive assistance (resident involved in activity, staff provide weight-bearing support) with dressing. The MDS assessment dated [DATE] indicated, total dependence (full staff performance) with dressing, upper extremity (UE) impairment on one side, and lower extremities (LE) impairment on both sides.
2. Resident 46 was admitted to facility on 11/26/19 with diagnoses including schizophrenia (a disorder that affects the ability to think, feel, and behave clearly) and Alzheimer's disease (a progressive disease that destroys memory and other important mental functions).
Review of Resident 46's physician's order for May 2022 indicated, Recommendation from PT 9/15/21: Ambulate with walker by staff supervision and assistance.
During an observation on 5/3/22, at 8:45 AM, Resident 46 was awake in bed wearing foam booties on both feet.
During an interview with the Wound Care Nurse (WCN) 1 on 5/3/22, at 9:03 AM, WCN 1 stated Resident 46 used to get up on the wheelchair and wheel around the unit. WCN 1 further stated, Resident 46 experienced a change in condition on 4/23/22. Resident 46 developed four deep tissue injury (DTI, an injury to a patients underlying tissue below the skin's surface that results from prolonged pressure in an area of the body) on the left and right foot.
During an observation on 5/4/22, at 3:19 PM, CNA 2 was feeding Resident 46 in bed with the head of bed elevated and foam booties on both feet. During concurrent interview, CNA 2 stated Resident 46 was wearing foam booties to protect the wounds on his feet. CNA 2 stated Resident 46 used to wheel himself around and into other resident's room but recently, Resident 46 had been staying in bed. CNA 2 added, Resident 46 had a decline in ADL function, he used to require limited assistance but now requires total assistance.
During an interview with CNA 2 on 5/4/22, at 3:22 PM, CNA 2 stated, He's (Resident 46) not ambulatory. He was evaluated by PT/OT but no recommendation. CNA 2 further stated, he provides ROM exercises (stretching) to Resident 46 during ADL care for a total of two to three minutes on both UE/LE.
During a concurrent interview and record review with LVN 2 on 5/5/22, at 11:35 AM, Resident 46's care plan was reviewed. LVN 2 was unable to find a care plan addressing Resident 46's ROM exercises and PT's recommendation for ambulation. LVN 2 stated he was not aware of Resident 46's recommendation for ambulation. LVN 2 added, He's not ambulatory.
Review of Resident 46's MDS dated [DATE] indicated, Resident 46 was independent with bed mobility and locomotion (how resident moves in and out of the unit) and required limited assistance with transfer. Under ROM, indicated no impairment of upper extremities (UE) and impairment on both sides of lower extremities (LE). Under Restorative Nursing Program indicated 0 on walking.
Review of Resident 46's MDS significant change assessment dated [DATE] indicated, Resident 46 required total assist with bed mobility, transfer, eating, and hygiene while locomotion and walking activity did not occur. Under Section M, Skin Condition indicated Resident 46 has four DTIs.
During an interview with MDS Coordinator (MDSC) 1 on 5/5/22, at 3:15 PM, MDSC 1 acknowledged and stated, a significant change assessment was completed for Resident 46 due to a decline in ADL function and development of DTI. MDSC 1 added, Resident 46 now requires more assistance with ADLs.
Review of Resident 46's Occupational Therapy Initial Evaluation/Discharge Summary dated 5/5/22 indicated, the prior level of function was I (independent) propel w/c (wheelchair), min (minimum) assist with ADL's. Resident 46's current level of function indicated dependent. The Occupational Therapy Initial Evaluation/Discharge Summary indicated, the upper extremity assessment indicated decreased AROM on the shoulder and increased rigidity in tone. The overall assessment indicated, Impaired ADL ability. Impaired functional mobility/transfers. Impaired ADL endurance. Impaired standing/sitting balance. At risk for deconditioning/contractures/skin breakdown. Seating and positioning needs not met.
Review of Resident 46's ADL Function/Rehabilitation Potential care plan dated 5/6/22 indicated, .Pt has increased weakness and requires total assist with ADL's .
Review of facility's policy and procedure titled, Change in Resident Condition, revised on 10/2021, indicated, .2b. A significant change reassessment must be done when a decline or improvement occurs in 2 or more of the following areas: c. Decline: 1) Any decline in ADL/physical functioning where a resident is newly coded as 3 (extensive assistance), 4 (total dependency), or 8 (activity did not occur) . 8) Emergence of a condition/disease in which the resident is judged to be unstable. 9) Emergency of a pressure ulcer at Stage II or higher, when no ulcers were present at Stage II or higher. 10) Overall deterioration of a resident's condition or resident receives more support, e.g., in ADLs or decision-making .
3. Resident 44 was admitted on [DATE] with diagnoses including stroke and hemiplegia.
Review of Resident 44's physician's order dated 3/10/22 indicated, DON (put on) RIGHT HAND SPLINT with foam under wrist 4 hours every day from 10 AM to 2 AM. Check for redness and skin irritation.
During an observation on 5/5/22, at 10:45 AM, Resident 44 was on his wheelchair and did not have a hand splint on the right arm/wrist. The hand splint was observed on top of the bedside drawer. During concurrent interview, Resident 44 stated his hand is very stiff and that he does not wear the splint every day. Resident 44 added, Nobody helps me (referring to splint application).
During an interview with CNA 5 on 5/5/22 at 10:52 AM, CNA 5 stated, I'm not sure when the resident wears the splint. I will ask the OT.
During a follow up interview with CNA 5 on 5/5/22 at 11:14 AM, CNA 5 stated Resident 44 should wear the splint 4 hours a day from 10 AM to 2 PM according to the OT instruction.
During concurrent interview and record review with LVN 2 on 5/5/22 at 2:45 PM, Resident 44's OT's progress notes for March 2022 indicated there was no assessment and documentation regarding the hand splint that was ordered on 3/10/22. LVN 2 acknowledged the OT progress notes dated 3/31/22 did not mention about the hand splint and stated, I don't see any. Resident 44's care plan was also reviewed and LVN 2 was unable to find a care plan addressing use of hand splint and range of motion exercise.
Review of Resident 44's MDS dated [DATE] indicated, one side of upper extremities (UE) was impaired. Under section O, Restorative Nursing Program indicated, 0 on splint or brace assistance which means splint was not applied.
4A. Resident 65 was admitted on [DATE] with diagnoses including stroke and hemiplegia.
Review of Resident 65's MDS dated [DATE] indicated, the staff assessment for mental status indicated Resident 65 was cognitively impaired. The functional limitation in ROM indicated, both sides of upper and lower extremities (UE/LE) were impaired.
Review of Resident 65's physician's order for May 2022 indicated the following orders:
a. 4/2/19 - RUE (right upper extremity) Splints: Wear when in bed. remove when up in chair. Remove splints to perform ADLs .
b. 10/8/20 - RLE (right lower extremity) Splints: Wear in bed. Place towel around upper thigh and lower leg under Velcro attachments to decrease risk of skin breakdown. Remove splint if any skin irritation or redness.
During an interview with CNA 4 on 5/3/22, at 4:14 PM, CNA 4 stated Resident 65 has a splint on the right arm and right thigh to prevent contractures when in bed.
During an observation on 5/3/22 at 4:15 PM, Resident 65 was in bed, asleep and did not have a splint on the right arm thigh. During concurrent interview, CNA 4 acknowledged Resident 65 was not wearing a splint on the right arm and right thigh. CNA 4 went to check Resident 65's bedside drawer and closet but was unable to find the splint. CNA 4 stated, I don't know where it is (referring to the splint). I will look for it.
During an interview with CNA 5 on 5/4/22, at 11:43 AM, CNA 5 stated, [Resident 65] has a splint but not anymore. The splint is missing.
Review of Resident 65's TAR for February 2022 indicated under comments, 2/10/22 8AM CNA reported cannot find pt (patient) R (right) hand splint . CN (Charge Nurse) and physical therapy made aware. The comments dated 2/13/22, 2/14/22, 2/17/22, 2/22/22, 2/24/22, 2/26/22, and 2/27/22 (seven days) indicated RUE and RLE splint were missing. The TAR for March 2022, April 2022, and May 2022 indicated, RUE splint . FYI MISSING 2/10/22 OT AWARE.
Review of Resident 65's OT progress notes dated 2/10/22 indicated, RUE splint reported missing by nursing. Nursing to look for splint prior to OT replacing. OT progress notes dated 3/1/22, CNA reports RUE/LE splint missing to OT. OT progress notes dated 5/4/22 indicated, LATE ENTRY FOR 3/16/22 Quarterly Assessment . Severe tone RUE/LE with decreased ROM . RUE/LE splint reordered .
During an inteview with RS on 5/5/22, at 10:02 AM, RS acknowledged Resident 65's RUE and RLE splints were missing and stated she did not have a back up supply of the splint.
Resident 65's care plan was reviewed, LVN 2 was unable to find a care plan addressing the use of splint. LVN 2 stated, The splint should be care planned. There should be an alternative approach for the missing splint.
4B. Resident 127 was admitted on [DATE] with diagnoses that include vegetative state secondary to subarachnoid bleed (bleeding in the space between your brain and the surrounding membrane) from cerebral aneurysm (a bulge or ballooning in a blood vessel in the brain) and chronic extremity contractures. Review of Resident 127's Interim History and Physical, dated 6/12/21 indicated Resident 127 had .no right upper extremity movement .
Review of Resident 127's Physician's orders for May 2022 indicated, Date prescribed .5-22-2018 . Resting splint to right hand . with a Wearing Schedule indicating Resident 127 was to wear the splint from 10 AM to 6 PM, and 10 PM to 8 AM. Review of Resident 127's MDS, dated [DATE], indicated Resident 127 had functional limitations on both upper extremities and was totally dependent on nursing staff for all his activities of daily living; the same MDS also indicated that a splint or brace assistance was not applied to Resident 127.
During a concurrent observation and interview on 5/4/22 at 2:47 PM with CNA 2, Resident 127 was lying in bed and slightly turned to his right side. Resident 127 had a contracture of the right hand with his wrist bent inwards towards his forearm Resident 127 did not have a splint applied to his right hand. CNA 2 stated, He (Resident 127) does not have a splint, only towel roll (referring to hand roll) on the right hand . CNA 2 proceeded to get a washcloth, rolled it, and applied it on Resident 127's right hand. CNA 2 stated he was not sure which hand needed a splint and was not aware of Resident 127's wearing schedule for the splint. CNA 2 stated, I don't know the order. The splint, nobody told me. The wearing schedule of the splint was not posted in Resident 127's room.
During a concurrent observation and interview with RN 6 on 5/5/22 at 11:30 AM, Resident 127 was lying bed with his eyes open he did not have a splint applied to his right hand.
During an interview on 5/5/22 at 11:45 AM, the Registered Nurse (RN 6) stated, Nobody reported that it (splint) has been missing. They (nursing staff) said it's been missing a long time, about a month ago. They (nursing staff) can't tell me specifically when. RN 6 stated that the use of splint for Resident 127 is to prevent further flexion and more contractures.
During an interview on 5/6/22 at 11:32 AM, the RS stated that the use of splint to Resident 127's right hand was to limit him (Resident 127) from going into further decline and to prevent his fingers from going into his skin.
During an interview on 5/6/22 at 11:53 AM, the Director of Nursing (DON) stated that not applying the splint to residents as prescribed could contribute to further contractures.
Review of the facility policy and procedure titled, Splinting, revised on 4/17 indicated, Splinting is used to protect joints and surrounding soft tissue. This can be accomplished by maintaining joints at position of rest, preventing positions that contribute to contracture and/or deformity, protecting the system of arches within the hand and increasing or maintaining ROM in the joint . The Occupational Therapist shall assess patient's need for splints with the following considerations: To protect joints and surrounding soft tissue; To increase hand function; To maintain range of motion . The Occupational Therapists shall then evaluate for type of splint required by patient . A splint handout with precautions and wearing schedule will be posted in resident's room . The Occupational Therapists shall train nursing staff/patient/caregivers/family members on donning/doffing the splint, cleaning of the splint, precautions (reddened areas) and wearing schedule .
5. Resident 76 was admitted on [DATE] with diagnoses including stroke, hemiplegia (paralysis of one side of the body) and chronic pain (persistent pain that lasts weeks to years).
Review of Resident 76's MDS dated [DATE] indicated, Resident 76 has impairment on one side of UE and both sides of LE. Under section O, Restorative Nursing Program indicated 0 on both AROM and PROM, splint or brace assistance.
Review of OT's quarterly assessment dated [DATE] indicated, .R (right) hand contractures [with] limited use of L (left) hand. R feet plantar [check mark symbol] contractures LUE shoulder [check mark symbol] AROM 0-120, RUE PROM 0-90 .
During an observation on 5/2/22, at 11:17 AM, Resident 76 was in bed with a rolled towel on the right hand. Resident 76's right hand and fingers were bent and curled inward.
Review of Resident 76's physician's order for May 2022 indicated, Range of Motion exercise to right upper extremity daily for flexion of contractures was ordered on 12/3/19.
During an interview with CNA 9 on 5/4/22, at 2:53 PM, CNA 9 stated she provide ROM exercises five to eight minutes for both upper and lower extremities to Resident 76 during ADL care. CNA 9 added, Resident 76 has pain on the right arm/hand due to contractures and a rolled towel is applied every day.
Review of Resident 76's care plan for pain revised on 3/13/22 indicated, Potential for pain or discomfort r/t (related to) Disease processes, Limited Mobility . Approach . Moving hands and feet a little .
Review of the TAR for May 2022 indicated, an FYI (for your information) under the treatment order Range of Motion exercise to right upper extremity daily for flexion of contractures.
During interview with LVN 2 and concurrent review Resident 76's care plan on 5/4/22, at 3:05 PM, LVN 2 was unable to find a care plan addressing the application of rolled towel on the right hand and range of motion exercises. LVN 2 acknowledged and stated the care plan should indicate the interventions provided to the resident.
Review of the facility's policy and procedure titled, Range of Motion, revised on 8/2020, indicated, Purpose: 1. To maintain and improve muscle strength and tone . 3. To prevent contractures . Procedure/Responsibilities 1. Licensed personnel are to supervise nursing assistants in ROM. 2. Physical Therapy is to be called for initial evaluation, if necessary. ROM is a nursing measure . 4. ROM exercise doe not take the place of position change and support for dependent parts . 7. Do not bring the joint/limb motion to the point of pain . 9. Each joint is moved through its range 3-5 times per treatment . In-Service Education: 1. All nursing staff are instructed in the techniques of active and passive ROM . 2. All resident will receive ROM every 4 hours between the hours of 0900 and 2100 every day. 3. Passive ROM may be ordered as a nursing order . Documentation: CNA Flowsheet.
Review of facility's policy and procedure titled, Plan of Care, revised on 9/2019, indicated, . 1. The comprehensive plan of care shall include: a. the frequency at which care, services, treatments, and interventions will occur . d. Current needs, problems, goals, care, treatment and services . 3. The evaluation of the resident's progress is made based upon the care plan goals and the resident's plan of care, treatment and services.
6. Resident 111 was admitted on [DATE] with diagnoses including hemorrhagic stroke (an emergency condition in which a ruptured blood vessel causes bleeding inside the brain) and quadriplegia (paralysis of both sides of the body).
Review of Resident 111's MDS dated [DATE] indicated both sides of upper and lower extremities (UE/LE) were impaired. Under Restorative Nursing Program indicated, 0 on both AROM and PROM, splint or brace assistance.
During an observation on 5/4/22, at 3:08 PM, Resident 111's Private Caregiver (PCG) 1 was observed putting on a white rolled towel on resident's right hand. Resident 111's wrist/hand were bent and his fingers were curled inward. During concurrent interview, PCG 1 explained he's putting a hand roll for Resident 111 due to contractures on the hands and fingers. PCG 1 also stated she provide ROM exercises to Resident 111 at night during ADL care.
During an interview with Resident 111's PCG 2 on 5/5/22, at 8:55 AM, PCG 2 stated he used to assist Resident 111 with ROM exercises using the Active Passive Trainer (APT, are electric exercise machines used for the improvement of physical abilities and can be operated in either active or passive mode) machine. PCG 2 pointed at the APT machine behind the privacy curtain. PCG 2 stated the APT machine was last used few months ago. PCG 2 also stated, [Resident 111] contractures became harder. The exercise hurts him. PCG 2 explained that they are waiting for the special shoes for Resident 111 prior to resuming use of APT machine. PCG 2 added, the shoes the resident had was hurting him.
During an interview with LVN 2 on 5/5/22, at 9:01 AM, LVN 2 stated Resident 111 has a private caregiver doing passive ROM and mostly providing care for the resident. LVN 2 added, I don't know about that machine (referring to the APT machine). The family provided it. I will ask the caregiver.
During an interview with RN 6 on 5/5/22, at 9:30 AM, RN 6 stated, [Name of Resident 111] family provided the APT machine. The private caregivers were assisting him (referring to Resident 111) with the exercise. RN 6 also stated the private caregivers reported they stopped using the APT machine due to increased stiffness of the upper and lower extremities.
During an interview with RN 6 on 5/5/22, at 9:32 AM, RN 6 stated the rehab provided PROM training to the caregivers and the use of APT machine. During concurrent record review, RN 6 was unable to find training records on the use of APT machine for Resident 111's private caregivers (PCG 1 and PCG2). RN 6 stated, I don't see their names in chart.
During concurrent interview and further review of Resident 111's record, on 5/5/22, at 9:34 AM, RN 6 was unable to find an order, assessment, and care plan for the use of APT machine. RN 6 stated, I don't see about the machine over here (referring to the OT progress notes). It's not in the order. It's not in the care plan. It's not mentioned in the OT assessment.
During an interview with RS on 5/5/22, at 9:55 AM, RS stated Resident 111 had a decline with ROM on 1/27/22. RS explained Resident 111 has APT machine in the room for home exercise which helps maintain ROM of the resident. RS added, The nursing staff has nothing to do with the home exercise program (referring to APT machine). The caregivers assist him (Resident 111) with it (APT machine). RS further stated, [Name of a caregiver] is using the APT but not PCG 2. RS stated she provides training to the private caregivers on how to perform ROM exercise and the use of APT machine for Resident 111. RS acknowledged the training was not documented in Resident 111's chart.
Review of the Active Passive Trainer user's manual revised on 01/2020, indicated, . 3.1 Indications: The Active Passive Trainers are intended to be operated by persons of most physiques and ages. In case the user has limited strength in the arm or cognitive impairment, it is required to have an attendant present during exercise . 3.3 Contraindications . In case of any disease or physical complaints, a healthcare provider should be consulted before participating in any exercise program . In case of recurring discomforts, consult with a health care provider .
Review of facility's policy and procedure titled, Education for Patient and Caregiver, revised on 4/2017, indicated, The Therapist and Therapist Assistant will instruct patient, family, and caregiver regarding home exercise programs and safe assistance techniques for functional mobility . The Therapist and Therapist Assistant will complete the following: 1. Provide on-going patient education during treatment sessions regarding safe techniques for home exercise and functional mobility . 3. Provide written instructions with pictures for patient and family when appropriate. The handout will be signed by the therapist/assistant and a contact number will be provided . 5. Document all patient/family education and training in progress notes. include the name and relationship of the family member/caregiver that was instructed. 6. Monitor and document the patient's or caregiver's ability to understand and follow through accurately. Request return demonstration of patient's/caregiver's when appropriate .
7. Resident 66 was admitted on [DATE] with diagnoses that include ischemic stroke (occurs when a vessel supplying blood to the brain is obstructed) with left hemiplegia (paralysis on side of the body).
Review of Resident 66's MDS, dated [DATE], indicated Resident 66 had functional limitations on one side of the upper extremities and on both lower extremities and was totally dependent on nursing staff for all his activities of daily living.
Review of Resident 66's Physician's orders for May 2022 indicated, 01-16-2018 . Apply hand roll to: Left hand contracture to prevent further limitations .Q (every) shift .
During an observation and interview with CNA 2 on 5/4/22 at 11 AM, Resident 66 was in bed, awake, and turned to his left side. Resident 66 had a contracture of the left hand with his fingers bent inwards towards his palm. CNA 2 stated Resident 66 is unable to stretch his left fingers and use his left hand. There was no hand roll applied to the left hand or fingers of Resident 66. CNA 2 stated, He (Resident 66) does not have it. We don't have a hand roll.
During a concurrent review of clinical records of Resident 66 and interview on 5/4/22 at 11:16 AM, RN 6 reviewed Resident 66's ADL Functional/Rehabilitation Potential care plan (CP), dated 3/12/22. The CP did not include interventions addres[TRUNCATED]
SERIOUS
(H)
Actual Harm - a resident was hurt due to facility failures
Safe Environment
(Tag F0584)
A resident was harmed · This affected multiple residents
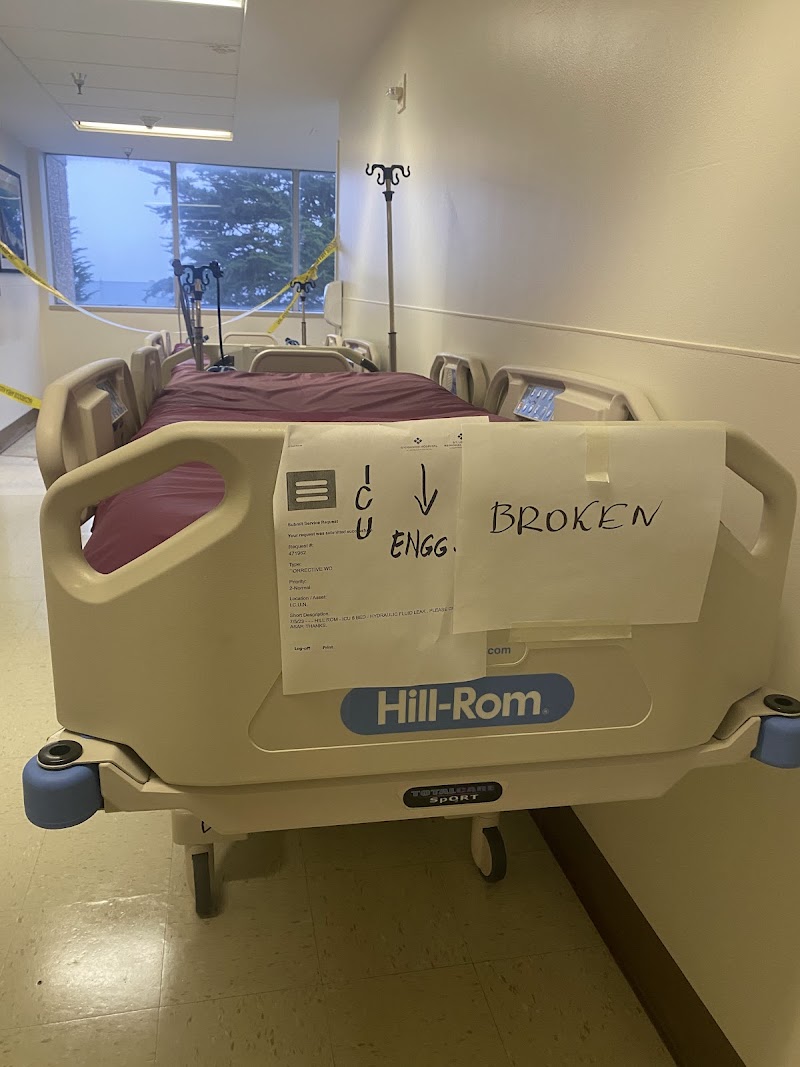
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2c. During a concurrent observation and interview, on 2/14/22, at 10:47 AM, observed a sign at the door of room [ROOM NUMBER] in...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2c. During a concurrent observation and interview, on 2/14/22, at 10:47 AM, observed a sign at the door of room [ROOM NUMBER] indicated room out of order: don't use. CNA 1 stated room [ROOM NUMBER]'s bathroom is out of order, and they moved the resident to another room yesterday (2/13/22). There were two holes on the wall near the shower head exposing the pipes. Also observed the bathroom floor linoleum with bubble like raised areas.
During an interview with the EVSS, on 2/14/22, at 11:42 AM, the EVSS stated there was a leakage which started around mid January (1/17/22). He stated, the engineer came the same day, had to cut through the wall to find the source of the leakage and had done the repair, but they are waiting for the engineer to come patch the holes. The EVSS stated he had no documentation regarding the repairs as it was more of a verbal thing.
During an observation on 2/14/22, at 11:25 AM, in the room [ROOM NUMBER] bathroom, observed a blackish substance around the base of the toilet bowl. Also observed the linoleum flooring with greyish stains.
During an observation on 2/14/22, at 11:45 AM, in the room [ROOM NUMBER] bathroom, observed a defined blackish substance around the base of the toilet bowl. Also observed a dark colored raised area on the floor linoleum, under the sink pipe. Also observed that the Formica covering the bathroom's sink cabinet was chipped at the edges.
Based on observation, interview, and record review, the facility failed to maintain a sanitary, comfortable and homelike environment when:
1. The linoleum flooring in room [ROOM NUMBER]'s bathroom were torn, cracked, and peeling off around the base of the toilet exposing the subfloor and had a pungent musty odor.
2. 20 of 41 resident bathroom flooring (Rooms 101, 105, 111, 201, 206, 208, 301, 302, 305, 306, 308, 309, 310, 311, 401, 403, 406, 407, 408 and 410) were damaged and discolored.
3. There was an evidence of stagnant, dark colored liquid in the shower room (number) 3 with pungent musty odor on the missing tiles.
The pungent musty odor had caused Resident 91 to feel sick and want to throw up. In addition, exposure to unpleasant odor, unsanitary, unkempt, and uncomfortable environment could affect mood, anxiety and stress level of other residents, staff, families, and visitors in the facility.
Findings:
1. During the initial tour, on 2/7/22, at 9:58 AM, in room [ROOM NUMBER], Resident 91 was sitting on his wheelchair by the bed watching television. Resident 91 expressed his concerns regarding the damaged linoleum flooring and the pungent odor coming from the bathroom. Resident 91 stated, The linoleum is broken. It was not fixed. They cover it with the rug and it smells.
Review of Resident 91's clinical record indicated, he was admitted in the facility on 10/25/13. The Minimum Data Set (MDS, a resident assessment tool) dated 1/4/22 indicated Resident 91 was cognitively intact.
During an observation, on 2/7/22, at 10:05 AM, in room [ROOM NUMBER]'s bathroom, the linoleum flooring was torn and ripped around the base of the toilet, exposing the subfloor. A black, rectangular scraper mat was placed over the areas with torn and ripped linoleum. The mat appeared wet with a pungent musty odor. The linoleum behind the base of the toilet was bulging and tearing apart. Portion of the caulking (a material used to seal joints or seams against leakage in various structures and piping) at the base of the toilet was missing and had a build-up of red-orange, dark brown, and black colored matter.
During an interview, on 2/7/22, at 10:08 AM, Resident 91 stated, It's been like that for a long time. They never fixed it (refering to the damaged bathroom floor).
During an interview, with Certified Nursing Assistant (CNA) 2 on 2/7/22, at 10:10 AM, CNA 2 acknowledged the damaged linoleum flooring in room [ROOM NUMBER]'s bathroom and stated, The toilet bowl is leaking and the floor is rotten. It's been like that for years. No action.
During an interview, on 2/8/22, at 9:46 AM, Resident 91 stated, It smells like pee and poop. It makes me feel sick. I want to throw up. Resident 91 added, the pee and poop smell is more notable in the afternoon and at night. Resident 91 further stated, the smell of the bathroom and the torn linoleum flooring in his bathroom (room [ROOM NUMBER]) and other resident bathrooms were discussed in the previous resident council meetings. Resident 91 added, the nurses, Environmental Services Supervisor (EVSS), engineering, maintenance, previous Director of Nursing (DON) and Executive Director for Continuum Care (EDCC) were all aware of the issue.
During an interview, on 2/8/22, at 9:54 AM, CNA 5 stated, It's been like that since I started working here (referring to the broken linoleum flooring in room [ROOM NUMBER]'s bathroom). CNA 5 also stated he's been working at the facility for more than two months now and has not seen someone fixed the flooring.
During an interview, on 2/8/22, at 10:13 AM, the Environmental Services Technician (EVST) 1 stated he was aware of the damaged linoleum flooring in room [ROOM NUMBER] and was instructed to clean and mop the bathroom floor with Clorox bleach (a brand of disinfecting solution) every morning. EVST 1 further stated, I don't know about the mat. I did not put it there.
During an observation, on 2/8/22, at 10:18 AM, in room [ROOM NUMBER]'s bathroom, the EVSS lifted the black mat covering the exposed subfloor showing a build-up of white, gray, green, and black colored matter underneath. During concurrent interview, the EVSS stated, This (referring to the torn linoleum flooring) started about a year ago when the toilet was leaking on and off. That area (pointing at the subfloor and surrounding base of the toilet) is rotten. That's from the leak. The EVSS explained, there were missing caulking around the base of the toilet. The water started to leak and seeped through the cracks causing the bubble and moisture under the linoleum flooring. In addition, the EVSS acknowledged that he personally placed the black mat on the torn linoleum flooring to prevent the urine from dripping on the subfloor which will further the rot. The EVSS acknowledged Resident 91 has verbalized about the pungent odor coming from the bathroom and stated, the EVS staff cleaned the bathroom daily and changed the mat two to three times a week.
According to an article titled, Odors and health, retrieved from https://www.health.ny.gov/publications/6500/index.htm, dated October 2019, indicated, . In some cases, odors can be used to tell whether there is a problem that needs to be fixed. For instance, mold problems, sewage backups and gas leaks in the home can all be detected by their odor, even if they can't be seen . Exposure to odors could result in health effects ranging from none, to mild discomfort, to more serious symptoms. Some chemicals with strong odors may cause eye, nose, throat or lung irritation. Strong odors may cause some people to feel a burning sensation that leads to coughing, wheezing or other breathing problems. People who smell strong odors may get headaches or feel dizzy or nauseous. If an odor lasts a long time or keeps occurring, it also could affect mood, anxiety and stress level . Try to find the source if you have unpleasant indoor odors . If you have a musty smell, check for moisture problems that could lead to mold growth. The way to control indoor odors is to find the source and remove it, or contain it in some way so that it doesn't release odors .
2a. During an observation, on 2/7/22, at 10:28 AM, in room [ROOM NUMBER]'s bathroom, the caulking and linoleum around the base of the toilet were chipped, cracked, peeling off, bulging with a buildup of dark brown, black and dark red-orange colored matter. The linoleum surrounding the base of the toilet had a grayish-black and brown colored markings.
During an observation, on 2/8/22, at 10:38 AM, in room [ROOM NUMBER]'s bathroom, the caulking and linoleum around the base of the toilet were torn, cracked, bulging and pulling away from the floor exposing the subfloor. The linoleum close by the baseboard and the wall was bulging and had a light brown stains or markings. There was a buildup of dark brown and black colored matter around the base of the toilet and in between cracks and tears of the linoleum.
During an observation, on 2/8/22, at 10:40 AM, in room [ROOM NUMBER] and 410's shared bathroom, the caulking around the base of the toilet were missing and had a buildup of dark brown and black colored matter. The linoleum surrounding the base of the toilet had a white, yellowish-brown markings and gray discoloration.
During an observation, on 2/8/22, at 10:43 AM, in room [ROOM NUMBER]'s bathroom, there was a buildup of dark brown, black, and dark orange colored matter on the caulking and around the base of the toilet. The linoleum around the toilet and close to the baseboard were cracked and bulging. The bolts anchoring the base of the toilet had a crusty orange and brown colored matter.
During a concurrent interview, and record review, on 2/8/22, at 11:01 AM, the undated Service Requester form indicated, Submit Service Request . Priority: 2-Normal . Short Description: remove and replace broken floor in r/r rms 403, and 406. The EVSS stated there were two bathrooms that needed new floor and that includes room [ROOM NUMBER]. When asked for the date of the service request was submitted, the EVSS stated, I just sent it out today (2/8/22). The EVSS then wrote 2/8/22 at the bottom right of the Service Requester form to indicate the date it was submitted. When asked for the maintenance log, the EVSS was unable to provide one. He acknowledged he did not have a log for the work order or service request submitted through the Service Requester.
During an interview, on 2/8/22, at 11:48 AM, the EDCC stated the Director of Facilities has the access to the work order log in the main hospital and should be responsible in following up the work orders. The EDCC acknowledged she was aware of the bathroom floor issues and stated a ticket was sent to the corporate to get a quote for the new floor.
Review of the letter document dated and signed on 2/8/22 by the EDCC, indicated, Plan for fixing 403 and 406: Director of Facilities (and team) will get a new quote for fixing both bathroom floors by 2/15. Submit for local and corporate approval 2/17. Start work as soon as materials arrive.
During an interview, on 2/14/22, at 10:42 AM, the Maintenance Supervisor (MS) stated he was verbally made aware of the leak and broken floor in room [ROOM NUMBER] by the EVSS. The work order don't go to me. Nursing will report verbally. The MS further explained, all staff have access to the work order email through Maintenance Connection online system in case there is something that needed to be fixed or replaced. When asked if a work order was submitted for room [ROOM NUMBER], MS stated he cannot remember when it was submitted. The MS acknowledged he does not have a log nor access of the pending work orders until he get a notification from the Director of Facilities or engineering department that a service request had been fixed and/or completed.
During an interview, on 2/14/22, at 11:44 AM, the EDCC stated the EVS, Director of Facilities, Chief/Assistant Chief of Engineering, and Nursing conduct the environmental rounds every quarter. The EDCC further stated, the identified list of things needed to be fixed and will be prioritized accordingly.
During an interview, on 2/14/22, at 12:09 PM, the Medical Director (MD) stated, I am not aware of the floor issues before. I just knew it now. We don't talk about it in QAPI (Quality Assurance and Performance Improvement) but will do it now. I'm embarrassed.
Review of the facility document titled, Work Order Status, dated 8/1/21 to 2/9/22, indicated, .Work order # - SMCCS-438255 - remove and replace broken floor tile in r/r/rms 403, and 406 . The document did not indicate the status and date the work order was submitted.
Review of the facility's policy and procedure titled, Maintenance Strategies and Frequencies, dated 6/5/17, indicated, .A work order system is used to manage planned maintenance activities. Work orders are issued for maintenance performed by the Facilities Department in-house staff and by contractors. The Facilities Director manages the worker order generation and completion process. 1. A Facilities Engineer performs assigned activities and return completed documentation to managers. Activities completed by contractors are tracked to assure the activities are completed in accordance with the terms of a contract . 4. The Facilities Director provides weekly assignments for all tasks schedule dint he system. Components maintained by corrective maintenance will be repaired on request, by work orders. 5. The Facilities Director will provide regular reports to determine percentage of activities completed, and identify problems associated with the individual work assignments and departmental and equipment trends . 7. All documentation of the maintenance activity will be completed by the Facilities Engineer, reviewed by the appropriate supervisor, and filed or the information entered into the work order system. Work orders for maintenance activities not completed will remain open until finalized.
2b. During an observation, on 2/10/22, at 10:42 AM, in room [ROOM NUMBER]'s bathroom, observed black and brownish liquid substance surrounding the base of the toilet bowl. The black and brownish substance was seeping out from the base of the toilet bowl. The bolts anchoring the base of the toilet had a crusty orange and brown colored matter.
During an observation, on 2/10/22, at 10:44 AM, the base of the toilet in room [ROOM NUMBER]'s bathroom, had a flaking white grout. Observed brownish liquid substance seeping out from the base of the toilet bowl.
During an observation on 2/10/22, at 10:47 AM, the base of the toilet in room [ROOM NUMBER]'s bathroom, had a flaking white grout. Observed brownish liquid substance seeping out from the base of the toilet bowl.
2d. During observations on 2/14/22, at 10:15 AM, in room [ROOM NUMBER], 302, 305, 306, 308, 310, and 311 bathrooms, the linoleum flooring at the junction of the base of the toilet bowl and the flooring, had gaps around the base of the toilet bowl. The gaps contained a buildup of dark brown colored substance.
During an interview with EVST 4, on 2/14/22, at 10:20 AM, EVST 4 acknowledged that rooms 301, 302, 305, 306, 308, 310, and 311 bathrooms had a dark colored substance at the junction of the base of the toilet bowl and the linoleum flooring. He stated that the Skilled Nursing Facility (SNF) trained staff to use bleach to clean the flooring gaps at the junction of the base of the toilet bowl and the flooring in the bathrooms. He said, afternoon environmental services staff are required to terminally clean shower rooms every afternoon.
3. During observations on 2/14/22, at 9:30 AM, in the company of EVSS, the SNF placed a sign outside the door of Shower room [ROOM NUMBER] indicating that staff not use the shower room to shower residents. EVSS used a tape measure to measure the size of the missing tiles on the floor. He counted 21 missing tiles each measuring 1/2 x 1/2 inches (in) size. The missing tiles were located next to each other in the form of a square and next to the drainage plate and were visible upon entering Shower room [ROOM NUMBER]. The floor space missing tiles contained sheer stagnant liquid with pungent smell. A black substance was visible through the sheer liquid, at the bottom of the floor spaces missing the tiles.
During concurrent interview on with EVSS on 2/14/22, at 9:45 AM, EVSS acknowledged that the floor of Shower room [ROOM NUMBER] had 21 ceramic tiles, 1/2 x 1/2 in size missing from the floor. He agreed that the space where the tiles were missing contained sheer stagnant liquid with a black substance visible at the bottom of the space missing the tiles. He stated that the SNF contracted with few bidders for the opportunity to work in replacing the missing tiles. He said the facility was aware that the tiles were missing, was trying to replace the missing tiles, and was waiting for contract bidders to give the SNF requested bids. He stated, the main SNF has documentation of the requested contractor bids.
During an interview with CNA 3, on 2/14/22 at 4:30 PM, in Shower room [ROOM NUMBER], CNA 3 stated, I would not shower my residents in the moldy shower room. She said CNAs working during the day shift showered resident in the shower room with the tiles missing on the floor of the shower room.
During an interview with Registered Nurse (RN) 4, on 2/14/22, at 4:35 p. m, in Shower room [ROOM NUMBER], RN 4 acknowledged that CNAs showered residents in Shower room [ROOM NUMBER] while the tiles were missing from the floor. She stated that the SNF trained staff to submit a work order to replace the missing floor tiles, and to continue to use the shower room to shower residents while waiting for the SNF to replace the missing tiles.
During a review of undated facility document titled, Work-order Status. SMCC Open Work Order List, the Work Order Status. SMCC Open Work Order List indicated that the SNF documented (1) on 9/16/21, at 12:01 PM, Third request to replace missing floor tile in Shower #3 in 300 hall, (2) on 12/7/21, at 9:01 AM, Leaking water from the shower cap on Shower 3 at 300 hall. Please check out, (3) on 1/13/22, at 8:04 AM, 300 shower drain plugged. and (4) on 1/18/22, at 10:45 AM, Shower drain clogged in 300 hallway.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the call light was within reach for one of 33 sampled residents (Resident 37) who was at risk for fall.
This deficient...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to ensure the call light was within reach for one of 33 sampled residents (Resident 37) who was at risk for fall.
This deficient practice had the potential to result in falls, injury, and harm to the resident and not meeting Resident's needs.
Findings:
During a concurrent observation and interview on 2/8/22, at 8:15 AM, Resident 37 was awake, banging the table with the empty water pitcher and yelling, I need water, I don't have a call light. Observed Resident 37's call light with its cord, hanging over the overhead light adjacent to Resident 37's bed.
During a concurrent observation and interview on 2/8/22, at 8:35 AM, Licensed Vocational Nurse (LVN) 1 looked for Resident 37's call light, then found it hanging on the overhead light above, adjacent to Resident's bed. LVN 1 stated, the call light was supposed to be within the reach of Resident at all times and gave the call light button to the Resident.
During an interview on 2/8/22, at 9:25 AM, Certified Nursing Assistant (CNA) 1 stated, Resident's call light was supposed to be within reach.
During an interview on 2/8/22, at 10:35 AM, Charge Nurse (CN) 1 stated call light should at all times be within the reach of the resident.
During an interview on 2/9/22, at 11:20 AM, CNA 2 stated the call light should be within reach of the Resident at all times.
During an interview on 2/8/22, at 2:55 PM, with the Executive director of Continuum of Care (EDCC) stated they do not have a call light policy.
Review of care plan for Resident 37, dated 9/22/21, the care plan indicated, Resident 37 was .at risk for fall related to dementia, stroke with left sided hemiparesis [paralysis on the left side of the body], and recent fall; with interventions to move items such as call light, water .by the patient within easy reach, and to respond to call light .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure their abuse prevention policy and procedure was implemented when there was no evidence of background screening for two nursing staff...
Read full inspector narrative →
Based on interview and record review, the facility failed to ensure their abuse prevention policy and procedure was implemented when there was no evidence of background screening for two nursing staff (CNA 4 and LVN 8).
Failure to implement abuse prevention policy had the potential to compromise the resident's health, safety, and well-being.
Findings:
1. Review of the 5-DAY INVESTIGATION SUMMARY, dated 5/24/21, indicated, .On 5/20/2021 at approximately 0830, (Resident 33) reported to the charge nurse . the CNA (Certified Nursing Assistant) from the night before (5/19/2021), pushed her hard to the right side lying position even if she had just told her that she did not want to be turned . (Resident 33) mentioned to CNA that there are instructions posted that she cannot be turned to the right .after CNA pushed her, she felt pain on the right shoulder and right side of neck .
During an interview on 2/11/22, at 2:35 PM, the Director of Staff Development (DSD) stated CNA 4 is the alleged staff. CNA 4 was placed on administrative leave for a week and provided with abuse prevention in-service training. During concurrent record review, the DSD was unable to find the background screening for CNA 4 in the employee file. The DSD acknowledged there was no evidence a background check/screening for CNA 4 was completed. The DSD stated, It's not here. It should be available in her (employee) file.
Review of the facility's policy and procedure titled, Background Screening, dated 3/17, indicated, . A. The Human Resources Department is responsible for screening: 1) All candidates for employment . B. Screening shall determine whether the individual has: 1) A conviction of any sort that may be inconsistent with the duties of the position, or 2) been listed by a federal agency as debarred, excluded or otherwise ineligible for federally funded healthcare program participation .
Review of the facility's policy and procedure titled, Abuse, Elder and Dependent Adult, dated 8/20, indicated, . II. Procedure: A. Pre-employment Screening - 1. Prospective employees will be screened to detect a history of abuse, neglect, exploitation, misappropriation of property, or mistreatment of residents. 2. Such screening shall include previous and current employers as sell as applicable state licensing boards and registries.
2. During an interview and concurrent review of personnel file of Licensed Vocational Nurse (LVN ) 8, on 2/9/22, at 2:45 PM, the Executive Director of Continuum of Care (EDCC) concurred evidence that background screening was missing.
Review of the facility's policy and procedure titled, Background Screening, dated 3/17, indicated, . A. The Human Resources Department is responsible for screening: 1) All candidates for employment . B. Screening shall determine whether the individual has: 1) A conviction of any sort that may be inconsistent with the duties of the position, or 2) been listed by a federal agency as debarred, excluded or otherwise ineligible for federally funded healthcare program participation .
Review of the facility's policy and procedure titled, Abuse, Elder and Dependent Adult, dated 8/20, indicated, . II. Procedure: A. Pre0employment Screening - 1. Prospective employees will be screened to detect a history of abuse, neglect, exploitation, misappropriation of property, or mistreatment of residents. 2. Such screening shall include previous and current employers as sell as applicable state licensing boards and registries.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to report an alleged abuse incident in a timely manner for one of six sampled residents (Resident 132) with abuse allegation incidents when Cer...
Read full inspector narrative →
Based on interview and record review the facility failed to report an alleged abuse incident in a timely manner for one of six sampled residents (Resident 132) with abuse allegation incidents when Certified Nursing Assistant (CNA) 7 reported the alleged verbal abuse two days after the incident.
The facility failure to report abuse according to the required timeframe had the potential to delay the identification and implementation of appropriate corrective action that may place the residents at risk of abuse.
Findings:
A review of the facility Report of Adverse Event letter dated 4/23/21 sent to the California Department of Public Health (CDPH) via fax (transmission of data) on 4/23/21 at 5:34 PM, under descrption of events indicated, It was reported today (4/23/21) at 3:40 pm that a CNA witnessed the following event on 04/20/21 at approximately 9:30 pm: .The LVN (Licensed Vocational Nurse) began suction (removal of plegm using a machine) the patient and stated I don't care if the patient is to going to die [sic].
During an interview on 2/9/22 at 3:47 PM, CNA 7 stated, on 4/20/21 at about 9:30 PM, she over heard the LVN 8 saying I don't care if he dies (referring to Resident 132). This was stated while LVN 8 was providing care for Resident 132. CNA 7 reported the incident on 4/21/21 because she did not want to disturb the Charge Nurse on duty the day of the incident and stated she was very busy.
A review of the facility policy dated 8/2020 and titled Abuse, Elder and Dependent Adult indicated: .Reporting/Response - 1. The person hearing or observing the allegation of abuse will immediately, but no longer than 2 hours, complete and fax the Report of Suspected Dependent Adult/Elder Abuse (SOC 341) to the Ombudsman and the CDPH and submit the form to the Charge Nurse/designee.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 65 was admitted on [DATE] with diagnoses including stroke and hemiplegia (paralysis of one side of the body).
During...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 65 was admitted on [DATE] with diagnoses including stroke and hemiplegia (paralysis of one side of the body).
During an interview with CNA 4 on 5/3/22 at 4:15 PM, CNA 4 stated, Resident 65 wears a splint on the right arm and right thigh to prevent contractures when in bed. CNA 4 added that she provides ROM exercises to Resident 65 during ADL care.
Review of Resident 65's TAR for March 2022 indicated, right lower extremity splint was applied on 3/1/22 to 3/15/22.
Review of Resident 65's MDS dated [DATE] indicated, under restorative nursing program indicated, 0 (zero) minutes on splint or brace assistance. Zero minutes means none or the activity did not happen.
During an interview on 5/6/22, at 2:55 PM, MDSC 1 acknowledged she was not coding Resident 66 and Resident 65's ROM and splints in the MDS assessment. MDSC 1 stated, We don't have an RNA program. There is no section in the MDS for splint.
During an interview with the DON on 5/6/22, at 3:10 PM, the DON stated the number of minutes for ROM and splint application should be documented in the resident's flow sheets as well as the number of feet for ambulation. The DON added, for residents with PT/OT (Physical Therapy/ Occupational Therapy) recommendations and physician's order for ROM, splints, and ambulation should also be coded in the MDS assessment to reflect the resident's current status.
Review of the facility's policy and procedure titled, ASSESSMENT - MDS and CAA, revised on 9/2011, indicated, POLICY: There should be a process in place for resident assessment on admission and ongoing re-assessment which includes the completion of the Minimum Data Set and Care Area Assessment (CAA) . PROCEDURE: . 2. The Interdisciplinary Team (IDT) performs and documents a complete assessment during the next fourteen days utilizing departmental assessment forms, the MDS, and the CAA . 5. Residents are reassessed following a significant change in condition and/or as needed, and at regularly scheduled times . At all of these times the plan of care is updated as appropriate .
Based on observations, interviews, and record reviews, the facility failed to ensure the Minimum Data Set (MDS) accurately reflect the functional status of two of 13 sampled residents (Residents 66 and 65).
MDS is an assessment tool that serves as the clinical basis for care planning and delivery of care and services
Failure to complete accurate assessment could potentialy result in inappropriate care planning, ineffective interventions and/or delay in provision of needed care and services to maintain residents highest level of functioning.
Findings:
1. Resident 66 was admitted on [DATE] with diagnoses that include ischemic stroke (occurs when a vessel supplying blood to the brain is obstructed) with left hemiplegia (paralysis on side of the body).
Review of the MDS dated [DATE] and 3/15/22, indicated Resident 66 had functional limitations on one side of the upper extremities and on both lower extremities and was totally dependent on nursing staff for all his activities of daily living.
During an observation on 5/4/22 at 10:44 AM, Resident 66 was in his room, lying in bed, and awake. Resident 66 was observed extending and bending his right leg while lying in bed.
During a concurrent observation and interview on 5/4/22 at 11 AM, Certified Nursing Assistant (CNA) 15 stated, I have known him (referring to Resident 66) since he got here. He cannot move his left leg. He is weak on the left side but this one (pointing to the right leg), he can move, no problem here. The other one (left leg) he cannot. With the instructions of CNA 15, Resident 66 extended his right leg from a bent position, lifted it slightly off the bed, and lowered it back on the bed.
During an interview on 5/6/22 at 11:23 AM, the Rehab Staff (RS) stated Resident 66 had no impairment on his right lower extremity.
Review of the MDS dated [DATE] and 3/15/22, indicated Resident 66 had functional limitations on one side of the upper extremities and on both (left and right) lower extremities.
During a concurrent interview, in the presence of the DON, and review of Resident 66's MDS dated [DATE] and 3/15/22 on 5/6/22 at 1:47 PM, the Minimum Data Set Coordinator (MDSC) 1 stated, I was not able to assess him because he was not cooperating. MDSC 1 stated, I should tell the nurse that I was not able to assess the patient. MDSC 1 also stated that she did not communicate with the Rehabilitation Services staff during the assessment period.
The DON acknowledged that if assessments do not reflect the actual condition of the residents, there is a potential provision for the facility to provide inaccurate and ineffective care and services to the residents.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure the baseline care plan (BCP) summary was provided to one of 3...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure the baseline care plan (BCP) summary was provided to one of 33 sampled residents (Residents 241) when there was no evidence a summary of there BCP was provided to the resident and/or the responsible party.
This deficient practice had the potential to place the resident at risk to not receive the quality of care and the appropriate interventions and goals to maintain the resident's quality of life.
Findings:
Review of the Face Sheet and the Hospice Physician's Order (HPO), dated 1/28/22, the Face Sheet indicated, Resident 241 was admitted to the facility on [DATE] and the HPO indicated a terminal diagnosis of hepatic failure (liver damaged).
In an interview on 2/10/22, at 10:24 AM, with the Registered Nurse (RN) 1, RN 1 explained, the facility would develop a Comprehensive Care Plan, used it as the Baseline Care plan (BCP) and would provide the BCP Summary to the resident and/or Responsible Party.
During a concurrent interview and record review, on 2/10/22, at 10:30 AM, with the RN 1 and the Nurse Manager (NM) 1, the BCP Summary was reviewed. The section on the BCP Summary indicated, Discussed with and copy given to Resident in a manner /language understood: Resident signature of receipt:, it was blank, undated and no signature of the resident. RN 1 stated, staff would usually document verbal consent by patient on the form, signed and date it, but that did not happened. RN 1 and NM 1 acknowledged BCP Summary form did not have evidence the resident was provided summary of the BCP.
Review of the facility's Policy and Procedure titled, Plan of Care, with the last revised date of 9/19 indicated, Policy: xxx (name of the facility) must develop and implement a baseline care plan for each resident Procedure: 1. 2. Provide a summary of the Baseline care Plan to the resident and their representative and place a copy in the medical record.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement their wound care policy for two of 33 sampled residents (...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement their wound care policy for two of 33 sampled residents (Resident 44 and 77), when:
1. Staff did not develop a non-pressure skin report and the nursing weekly summary did not indicate Resident 44's new skin condition.
2. Staff did not develop a non-pressure skin report and did not complete a nursing weekly assessment to address Resident 77's abdominal folds rash.
This failure could potentially result in a negative outcome for Resident 44 and 77.
Findings:
1. Resident 44 was admitted on [DATE], with diagnoses that includes hemorrhagic stroke (an emergency condition in which a ruptured blood vessel causes bleeding inside the brain) with left hemiplegia (partial paralysis on one side of the body that can affect the arms, legs, and facial muscles).
Review of Resident 44's progress notes, dated 1/28/21, indicated Resident 44 noted with left abdominal fold abrasion and right upper buttock abrasion.
Review of Resident 44's clinical records and concurrent interview with Wound Care Nurse (WCN)1, on 2/10/22, at 11:31 AM, WCN1 stated nurses must complete a skin report for any new skin condition found on residents. WCN 1 acknowledged there was no skin report completed for Resident 44's left abdominal fold abrasion and right upper buttock abrasion. WCN1 stated the skin report is the form she use to track, measure and monitor progress of skin conditions.
Review of Resident 44's clinical record, titled Resident Weekly Summary, dated 1/28/21 and 2/4/22, and concurrent interview with WCN1, 2/10/22, at 11:45 AM, did not indicate presence of the left abdominal fold abrasion and right upper buttock abrasion. WCN1 acknowledged the findings and stated the left abdominal fold abrasion and right upper buttock abrasion should have been included in the Resident 44's weekly summary.
2. Resident 77 was admitted on [DATE] with diagnoses including schizophrenia (a serious mental illness that affects how a person thinks, feels, and behaves)
Review of Resident 77's physician orders, dated 2/2/22, indicated nystatin powder to abdominal folds rashes BID [twice a day] x 14 days then re-eval [re-evaluate].
Review of Resident 77's clinical record and concurrent staff interview with Registered Nurse (RN) 5, on 2/10/22, at 2:45 PM, there was no evidence a care plan, a skin assessment, and a weekly summary, due on 2/7/22, was completed to address Resident 77's abdominal folds rashes. RN 5 acknowledged the findings and stated licensed staff who assessed the new skin condition should complete a skin care plan and an updated skin condition report. RN5 also stated the nursing weekly summary should have been completed to reflect the Resident 77's abdominal folds rashes.
During an interview with Director of Staff Development (DSD) on 02/11/22, at 1:57 PM, DSD stated the licensed nurse who found the new skin condition should call the doctor, complete a skin care plan, complete a non-pressure/pressure skin form and indicate in the nursing weekly summary the new skin condition.
Review of facility policy and procedure titled Wound Care Management, revised 8/2019, indicated Policy: Nursing, in collaboration with the health care team, assesses and manages resident's skin integrity throughout their stay at the skilled nursing facility II. Skin Inspection . 3. Findings are documented in the medical record . III Interventions B. The care and intervention for skin breakdown/wounds is intended to prevent wound advancement and/or additional skin breakdown . D. Evaluation of the Plan of Care Includes: 1. Changes to the plan of care if expected outcomes are not achieved . E. Documentation. 1. Skin Integrity and/or conditions affecting the patient's skin must be documented according to established procedures. 2. The presence of skin breakdown/abnormal skin appearance, i.e. abrasion . skin tear or wounds is documented upon admission and weekly. 3. Upon identification of a wound, a full wound assessment, including its location, size, description of the tissue involved is completed. 4. Interventions and progress towards outcome focused goals need regular documentation according to established procedures.
Review of facility policy and procedure, titled Weekly Summary, revised 10/2004, indicated Policy and Procedure: It is the responsibility of each RN [Registered Nurse] to determine which resident's Weekly Summaries are assigned to him/her and complete the form for each resident. The weekly summary must represent a total picture of the current status of the resident, as wells as address any issues which have been raised during the previous week.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the resident environment remains free of hazar...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the resident environment remains free of hazards when sharp objects were observed in plain sight in the room of one of 25 sampled residents (Resident 30).
This failure had the potential to cause accident and harm when accessed by other residents.
Findings:
Resident 30 was admitted on [DATE] with diagnoses that include quadriplegia (paralysis from the neck down, including the trunk, legs, and arms).
Review of Resident 30's Minimum Data Set (MDS, an assessment tool), dated 2/22/22, indicated Resident 30 is cognitively intact and has functional limitations in ROM on both upper extremities, and was totally dependent on nursing staff for all his activities of daily living.
During an observation on 5/3/22 at 8:38 AM, four pairs of straight scissors and one screwdriver inside an open container were observed on the Resident 30's nightstand. In a concurrent interview, Resident 30 stated, Yesterday, I asked the staff to fix the armrest of my wheelchair. He (staff) used the screwdriver to fix it. Resident 30 also stated a family member, and sometimes the staff, use the scissors to assist him with cutting pictures as a project.
During a concurrent observation and interview on 5/3/22 at 8:53 AM, Licensed Vocational Nurse (LVN) 1 verified the surveyor's observation and stated, Not sure if they're supposed to be on the nightstand.
During an interview on 5/3/22 at 9:04 AM, Registered Nurse (RN) 6 stated, They (scissors) are sharp objects. For items like sharp objects, should be kept in the drawer, somewhere not visible, so others like residents won't get it (sharp objects). It could harm us (staff and residents). It's for safety.
During an interview on 5/3/22 at 9:52 AM, the Director of Nursing (DON) stated, They (residents) are not allowed to have it (scissors). It's in the policy. It's for patient safety.
A review of the facility policy and procedure titled, Resident's Living Space and Possessions, dated 7/19, indicated Policy .Procedure: A.residents are provided with a nightstand and closet to store personal items . II. Prohibited Items . E. Weapons of any kind. (including, but not limited to, .scissors) .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to evaluate and implement interventions that are consistent with the n...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to evaluate and implement interventions that are consistent with the nutritional status for one of four sampled residents (Resident 111) when:
1. Staff rely on the caregivers verbal report of Resident 111 meal intake percentage with no verification.
2. There was no Registered Dietitian (RD, a health professional with special training in diet and nutrition) nutritional assessment and progress notes addressing Resident 111's nutritional status for the month of February, March, and April 2022 and weight loss on March and April 2022.
3. The nursing staff did not document and communicate to the Medical Doctor (MD) and RD to address Resident 111's significant weight loss.
These deficient practices resulted in a severe weight loss and had the potential to result in progressive decline in nutrition that compromised the health of Resident 111.
Findings:
Review of Resident 111's clinical record indicated, was admitted on [DATE] with diagnoses including hemorrhagic stroke (an emergency condition in which a ruptured blood vessel causes bleeding inside the brain), quadriplegia (paralysis of both sides of the body), dysphagia (difficulty swallowing), and aphasia (loss of ability to understand or express speech, caused by brain damage).
Review of Resident 111's Minimum Data Set (MDS an assessment tool) dated 4/19/22 indicated, Resident 111's cognition was severely impaired. The functional status assessment indicated Resident 111 was dependent in activities of daily living (ADL) including, eating.
Review of Resident 111's physician's order for May 2022 indicated the following orders on 1/18/22: Diet Order: .Texture: Chopped Mechanical Soft (any foods that can be blended, mashed, pureed, or chopped using a kitchen tool such as a knife, a grinder, a blender, or a food processor), Extra Gravy, with Thin liquids. No straw and Dietary supplement: PO (by mouth) BID (two times a day) ENSURE ENLIVE PLUS (a brand of dietary supplement) to be given with meals (Lunch and Dinner). Document % (percentage) intake.
During an observation on 5/6/22, at 9:13 AM, Private Caregiver (PCG) 2 was feeding Resident 111 in his room. During concurrent interview, PCG 2 stated, [Resident 111's] diet used to be pureed plus (a paste or thick liquid suspension usually made from cooked food ground finely) but lately it's not really puree. It is small pieces of food. PCG 2 added, the CNA's would usually ask for Resident 111's intake after meals but do not visually check the meal tray. PCG 2 also stated Resident 111 is offered with snacks brought by family and is given a dietary supplement every lunch and dinner.
During an interview with Certified Nursing Assistant (CNA) 5 on 5/6/22, at 2:40 PM, CNA 5 stated the caregiver reports to him Resident 111's meal intake and he will then document it in the ADL flowsheet (a documentation of resident's ADLs). CNA 5 further stated, he relies on the caregiver's report of Resident 111's intake and did not verify the actual percentage of the resident's intake.
Review of Resident 111's meal intake indicated, on 3/1/22 to 3/31/22, Resident 111's meal intake ranges from 75 percent (%) to 100 %. On 4/1/22 to 4/30/22, Resident 111's meal intake ranges from 50 % to 100%.
Review of Resident 111's weight record with Registered Nurse (RN) 4 on 5/5/22, at 4:17 PM, indicated the following:
On March 2022: 172 pounds (lbs),
On April 2022: 164 lbs, an 8 lbs dropped in a month.
During concurrent interview, RN 4 acknowledged Resident 111's weight loss of 8 lbs from March to April 2022. RN 4 stated, I don't have his weight for May. I will ask the CNA (Certified Nursing Assistant) to weigh him now. At 4:41 PM, RN 4 stated Resident 111's weight was taken and the current weight is 157.9 lbs. RN 4 further stated, an additional 6.1 lbs weight loss from April to May and a total of 14.1 lbs weight loss from March to May (two month period).
On 5/5/22 at 4:20 PM, Resident 111's nutritional assessment and progress notes from January to April 2022 were reviewed with RN 4. RN 4 confirmed there was no RD nutritional assessment and/or progress notes for the month of February, March, and April 2022. RN 4 stated, I don't see any RD assessment (referring to nutrition assessment). No notes or change of condition (COC) in the chart. RN 4 acknowledged there was no documentation addressing Resident 111's 8 lbs weight loss from March to April 2022. RN 4 verified, the last nutrition assessment in Resident 111's chart was dated 1/17/22. RN 4 added, the RD should have completed a nutrition assessment when Resident 111 had a weight loss of 8 lbs in April 2022.
During an interview with RD 2 on 5/5/22, at 4:50 PM, RD 2 acknowledged Resident 111's weight loss of 14.1 lbs. from February to May 2022 and stated, That is 8.1% in the last 3 months. It is considered a significant weight loss.
During concurrent interview and record review with RD 2 on 5/5/22, at 4:43 PM, Resident 111's weight record and nutrition assessment from February 2022 to April 2022 were reviewed. RD 2 acknowledged Resident 111 had a weight loss of 8 lbs from March 2022 to April 2022. RD 2 added, Resident 111's reported weight on 5/5/22 was 157.9 lbs. and stated, It's another weight loss. RD 2 also acknowledged there was no nutrition assessment in February, March, and April 2022. RD 2 stated there should be a nutrition assessment in April 2022 when Resident 111 experienced weight loss. RD 2 also explained, the RD in charge of doing the nutritional assessment and follow up for the residents at Coastside resigned and most likely the reason why nutritional assessment and follow up was not completed.
During a concurrent interview and record review on 5/6/22, at 9:18 AM, Resident 111's progress notes, COC documentation, nutrition notes and assessments were reviewed. RN 5 acknowledged there was no progress note, COC documentation, nutrition note and assessment addressing Resident 111's weight loss and communication to MD and RD. RN 5 stated, I don't see any COC, notes and RD assessment (referring to nutrition assessment). There should be one.
Review of Resident 111's nutrition care plan revised on 1/18/22 indicated, .Goal: No significant weigh changes (> [more than] 5 % [percent] in 1 month, > 7.5 % in 3 months, > 10 % in 6 months) . Approach .Weigh monthly and notify MD and RD of any significant weight changes.
Review of facility's policy and procedure titled, Weight Monitoring and Weight Variance, dated 5/2018, indicated, Purpose: Residents are weighed regularly to monitor for significant changes and/or changes in condition. Procedure/Responsibilities . 5. Significant weight changes are defined as the following: A. 3 pounds in one month for residents weighing less than 100 pounds; 5 pounds in one month for residents weighing >100 pounds . 6. Significant weight changes initiate the following actions: A. Weekly weights for four weeks. B. Weight change is reported to the MD and the registered dietitian. C. Licensed nurses initiate a Change of Condition (COC) . 9. Residents on weight variance are reviewed weekly until weight stabilizes .
Review of facility's policy and procedure titled, Change in Resident Condition, revised on 10/2021, indicated, Policy: The attending physician or his/her alternate, other disciplines, the resident, and/or resident's family will be notified by the nurse of any change in a resident's condition. The attending physician or his designee will be notified promptly of . 2. Any sudden and/or marked adverse change in signs, symptoms and behavior exhibited by a resident . c. Decline: . 6) Emergence of unplanned weight loss problem . 4. A change in weight of five percent or more within a thirty (30) day period unless a different stipulation has been stated in writing by the resident's physician . 8. All attempts to notify physicians shall be noted in the resident's health record. The information to be recorded is the time and method of communication and the name of the person acknowledging contact, if any .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide pharmaceutical services to meet the needs of one of eight sampled residents (Resident 123) when Licensed Vocational N...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to provide pharmaceutical services to meet the needs of one of eight sampled residents (Resident 123) when Licensed Vocational Nurse (LVN) did not rotate injection sites of Copaxone (glatiramer acetate, a medicine that is used to treat multiple sclerosis, a disease that impacts the brain and nerves) as per manufacturer's instructions.
This failure may result to skin and fatty tissue irritation.
Findings:
During an observation on 2/8/22, at 9:00 AM, in Resident 123's room, LVN 3 administered (gave) Copaxone injection (a way of giving a liquid medicine by using a needle and syringe) to Resident 123's right abdomen.
During review of Resident 123's Medication Administration Record (MAR), dated 1/25/22 to 2/8/22, indicated Copaxone was administered on the following dates:
On 1/25/22 at 9:00 AM, given in the left arm
On 1/26/22 at 9:00 AM, given in the right arm
On 1/27/22 at 9:00 AM, given in the left arm
On 1/28/22 at 9:00 AM, given in the right arm
On 1/29/22 at 9:00 AM, given in the left arm
On 1/30/22 at 9:00 AM, given in the right arm
On 1/31/22 at 9:00 AM, given in the left arm
On 2/1/22 at 9:00 AM, given in the right arm
On 2/2/22 at 9:00 AM, given in the left arm
On 2/3/22 at 9:00 AM, given in the right arm
On 2/4/22 at 9:00 AM, given in the left arm
On 2/5/22 at 9:00 AM, given in the right arm
On 2/6/22 at 9:00 AM, given in the left arm
On 2/7/22 at 9:00 AM, given in the right arm
On 2/8/22 at 9:00 AM, given in the right abdomen
During a concurrent interview and record review on 2/8/22, at 11:51 AM, with Charge Nurse (CN) 2, Resident 123's MAR, dated from 1/1/22 to 2/8/22 was reviewed. CN 2 acknowledged, the left arm and right arm were rotated every other day instead of weekly for Copaxone.
During an interview with Pharmacist 1, and review of Resident 123's MAR on 2/8/22, at 11:54 AM, Pharmacist 1 acknowledged, the left arm and right arm were used every other day instead of weekly from 1/25/22 to 2/7/22 for Copaxone.
During an interview on 2/8/22, at 12:01 PM, LVN 4 acknowledged, she did not rotate the injection sites as per manufacturer's instructions by using the same site more than 1 time a week.
During an interview on 2/8/22, at 12:15 PM, Pharmacist 1 stated, the nurses did not follow the manufacturer's instructions to rotate the same injection site every week for administration of Copaxone.
During an interview on 2/8/22, at 12:18 PM, LVN 5 acknowledged, she did not rotate the injection sites as per manufacturer's instructions by using the same site more than 1 time a week.
Review of manufacturer's instructions of Glatopa (also known as Copaxone), dated July 2019, indicated, . Do not stick the needle in the same place(site) more than 1 time each week . Avoid injecting in the same site over and over again .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
On 7/20/22, at 11:20 AM, with the DS 9, the Menu Arrival and Post Retherm (MAPR) Temperature logs dated 7/20/22 was reviewed with DS 9. The MAPR log indicated the following:
For Breakfast: Cart D: oa...
Read full inspector narrative →
On 7/20/22, at 11:20 AM, with the DS 9, the Menu Arrival and Post Retherm (MAPR) Temperature logs dated 7/20/22 was reviewed with DS 9. The MAPR log indicated the following:
For Breakfast: Cart D: oatmeal was 171 degrees, the sausage was 170 degrees, pancake was 170 degrees and scrambled egg was 173 degrees.
For Lunch: chicken soup was 192 degrees, meat was 180 degrees, mashed potato was 195 degees and spinach 185 degrees. During concurrent interview, DS 9 acknowledged the food temperature was high.
Review of the US (United States) Food and Drug Administration (FDA) website, dated 9/27/18 indicated: Cook to Proper Temperatures. Heating foods to the right temperature for the proper . Meat and Poultry: [NAME] ground beef, veal, lamb, and pork to at least 160° F (71° C). [NAME] all poultry to a minimum of 165° F (74° C). [NAME] beef, pork, veal, and lamb roasts and chops to at least 145° F (63° C), with a 3 minute rest time. Take Special Care with Ground Meat and Poultry: When meat and poultry are ground up, bacteria that might have been on the surface of the meat or poultry can end up inside. Always use a food thermometer to check. Tips to even out the cooking: . When done cooking, make sure the food is hot and steaming. Using a food thermometer, test the food in two or three different areas to check that it has reached a safe internal temperature.
Based on observation, interview and record review the facility failed to provide food at required temperature for residents.
This failure had the potential to place residents at risk for poor food intake which could compromise their nutritional and health status.
Findings:
In an interview on 7/20/22, at 9:20 AM, Resident 91 stated, the food was served too hot, the hamburger was burned, and the food issue was brought up in the Resident Council meeting.
Review of the April, May, and June 2022, Coastside Resident Council Minutes (RCM), indicated the following:
On 4/28/22, it indicated, the hamburger patty was crispy and burned and the food was served too hot.
On 5/26/22 indicated, the cold food is served hot and hot food is served cold.
On 6/23/22 indicated, food is served too hot.
In an interview, on 7/20/22, at 9:32 AM, the Dietary Staff (DS) 9 stated, the facility used a high heat disposable plates and dinex coffee mugs.
In a group interview, on 7/20/22 at 12:18 PM, with the Physician 1, Chief Nursing Officer (CNO), Director of Nursing (DON), Infection Preventionist (IP) 2, Director of Food and Nutrition Services (DFNS), and Director of Quality (DOQ), the DFNS stated, this was the first time she heard of the hot food complaint by the residents and would make sure it would be addressed. The other QAPI members did not have anything to say about the facility's actions on the hot food issue raised by the Resident council.
On line review of the US (United States) Food and Drug Administration (FDA) website, dated 9/27/18 indicated: Cook to Proper Temperatures. Heating foods to the right temperature for the proper . Meat and Poultry: [NAME] ground beef, veal, lamb, and pork to at least 160° F (71° C). [NAME] all poultry to a minimum of 165° F (74° C). [NAME] beef, pork, veal, and lamb roasts and chops to at least 145° F (63° C), with a 3 minute rest time. Take Special Care with Ground Meat and Poultry: When meat and poultry are ground up, bacteria that might have been on the surface of the meat or poultry can end up inside. Always use a food thermometer to check. Tips to even out the cooking: . When done cooking, make sure the food is hot and steaming. Using a food thermometer, test the food in two or three different areas to check that it has reached a safe internal temperature.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the Skilled Nursing Facility (SNF) failed to ensure that staff educated and documented i...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the Skilled Nursing Facility (SNF) failed to ensure that staff educated and documented in residents medical records education regarding the risk and benefits of vaccinations, for one out of 33 sampled residents, Resident 35.
This failure had a potential to expose Resident 35 to lack of information needed to make informed choices regarding immunization, increasing Resident 35 to the likelihood of suffering from adverse events (unanticipated injuries, harm, death or risk of infectious diseases) related to infectious diseases, and compromising her health and safety.
Findings:
During a review of Resident 35's record titled Inpatient Record dated 2/4/22, the Inpatient Record indicated that Resident 35 was a [AGE] years old female admitted to the SNF on 4/10/2. The SNF admitted Resident 35 with diagnoses that included hypertension, depression and anxiety.
During a review of Resident 35's document titled Consultation Report dated 12/21/20, the Consultation Report indicated that in May 2020, Resident 35 was admitted to long-term setting since an episode of sepsis due to left lower aspiration pneumonia .
During a review of Resident 35's comprehensive (significant change in status) Minimum Data Set (MDS an assessment tool) dated 8/31/21, and Quarterly MDS assessment dated [DATE], indicated that the SNF documented that Resident 13 had a Brief Interview of Mental Status (BIMS - ability to understand and recall information) Summary Score of 13 (Cognitively intact - able to understand and recall information). The SNF documented that Resident 35 declined influenza (flu) and pneumococcal (pneumonia) vaccinations.
During a review of Resident 35's document titled Pneumococcal/Influenza Adult Vaccination Orders - Long Term Care, undated, the document indicated that the SNF required registered nurses to complete residents' immunization history- resident history form) and risk assessment below. The SNF documented that on 9/25/20, at 15:30 PM, Resident 35 was unable to sign, refused all vaccinations of flu and pneumonia vaccination.
During a review of Resident 35's document titled Pneumococcal/Influenza Adult Vaccination Orders - Long Term Care, undated, the document indicated that the SNF required registered nurses to complete residents' immunization history- resident history form and risk assessment below. On 10/2/21, at 11:00 AM, the SNF documented verbal refusal of flu vaccination on the form.
Resident 35's medical record did not contain documentation that the SNF informed Resident 35 specific risks and benefits of influenza and Pneumococcal immunization and alternative options available to the resident upon refusal of vaccination.
During an interview with Resident 35 on 2/9/22, at 10:15 AM, in the company of Charge Nurse (CN) 2, Resident 35 stated she could not remember any conversations regarding influenza and pneumococcal vaccinations.
During a concurrent interview with CN 2 on 2/9/22, at 10:25 AM, CN 2 stated that When they decline we update and offer explanation of benefits, but do not document explanation in the medical record.
During an interview with Director of Quality/Infection Preventionist (DoQ/IP) on 2/9/22, at 1:00 PM, DoQ/IP stated that the SNF designated the responsibility of explaining risks and benefits of immunization to medical providers. He stated that nursing staff handed over the vaccination form to residents' and requested residents to sign the forms. He repeated that nursing staff, and physician providers, were not educated to document patient education regarding the risk and benefits ofinfluenza and pneumonia vaccines in the medical record. He said, If it was not documented in the medical record it was not done.
During a review of the facility policy and procedure titled TITLE: IC 5_H: PNEUMOCOCCAL AND SEASONAL INFLUENZA VACCINATION PROTOCOL undated, the policy and procedure did not have documentation that staff educate residenst about the risks and benefits of flu and pneumococcal vaccination. The policy and procedure did not address how the facility required staff to document in residents' medical records that they provided education regarding the risks and benefits of flu and pneumococcal vaccination.
During a review of the Center for Disease and Prevention (CDC) document titled Best Practices Guidance of the Advisory Committee on Immunization Practices (ACIP- national organization that advices healthcare facility on immunization practices), updated 2/15/22, the Best Practice Guidance of the ACIP recommended that healthcare facilities inform patients about the benefits and risks of vaccines in languages that are culturally sensitive and at appropriate educational level. It stated that healthcare providers can be a pivotal source of science-based credible information by discussing with patients the risks and the benefits of vaccines which helps patients make informed decisions. The guidance stated that discussions of risks and benefits from vaccination 'is a sound medical practice and is required by law.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0888
(Tag F0888)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement its policy and procedure to ensure all staff were fully v...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement its policy and procedure to ensure all staff were fully vaccinated for COVID-19 (a new infectious viral disease that can cause respiratory illness) when:
1. There was no evidence proof of vaccination were obtained for four (4) facility staff (Staff 1, Staff 2, Staff 3 and Staff 4).
2. Staff vaccination rate was less than 100%.
Failure to track and document COVID-19 vaccination status of all staff could potentially increase risk of spreading infection in the facility.
Findings:
1. Review of facility document, titled COVID-19 Staff Vaccination Status, dated 2/7/22, and concurrent interview with Infection Preventionist (IP), on 2/09/22 , at 2 PM, indicated four staff was not vaccinated without exemption/delay. IP acknowledged the findings. IP was not able to provide evidence/proof vaccination for the four staff.
Review of facility policy and procedure, titled Policy Concerning Required COVID-19 Vaccinations, no date, indicated I. Policy AHMC (Advanced Healthcare Management Corporation) [NAME] Medical Center and AHMC [NAME] Coastside (Facilities) requires that by September 30, 2021, all covered persons who provide services or perform work onsite at the Facility must be vaccinated against COVID-19, and provide proof of vaccination, subject to limited exemptions for qualifying medical reasons and religious beliefs . C. Proof of Vaccination . Proof of vaccination must include the name of the person vaccinated, the type of vaccine provided and the date of the last dose administered
2. Review of facility document, titled COVID-19 Staff Vaccination Status, dated 2/7/22, received by survey team on 2/9/22, at 1:45 PM, and concurrent staff interview with Infection Preventionist (IP), indicated as follows:
i. Completely vaccinated - 189
ii. Pending or granted non-medical exemption - 2
iii. Not vaccinated without exemption without exemption/delay - 3
iv. Total Staff: 194
IP acknowledged the staff vaccination line list did not include all staff as indicated in the facility policy. IP acknowledged the Executive Director for Continuum of Care (EDCC) was not included in the facility staff vaccination list.
Review of facility policy and procedure, titled Policy Concerning Required COVID-19 Vaccinations, no date, indicated II. Covered Person: Any person who provides services or performs work onsite at the Facility, including but not limited to employees, contract workers (i.e. persons not employed by the Facility), physicians, and students/trainees.
Review of facility document, titled COVID-19 Staff Vaccination Status, dated 2/7/22, received by survey team on 2/14/22, at 3:48 PM, indicated as follows:
i. Vaccinated - 296
ii. Exemption approved - 3
iii. Unknown (Not Vaccinated without exemption delay) - 4
iv. Total Staff - 303
Percentage (%) of Vaccinated Staff = (299/303) x 100% = 98.67%
During an interview with Data Analyst (DA) on 2/14/22, at 3:50 PM, DA stated she was responsible for submitting facility vaccination rates data to CDC website. DA stated they updated the staff list, from staff total of 194 to 303, to include all staff per facility policy. DA acknowledged the staff vaccination rate was less than 100%.
Review of facility policy and procedure, titled Policy Concerning Required COVID-19 Vaccinations, no date, indicated III. Procedures . B. Deadline for Compliance . A covered person must have either their first dose of a one-dose regimen or their second-dose of a two-dose regime of a COVID-19 vaccine by September 30, 2021.
According to QSO-22-07-All, dated 12/28/21, indicated Facility must demonstrate that: Policies and procedures are developed and implemented for ensuring all facility staff, regardless of clinical responsibility or patient or resident contact are vaccinated for COVID-19; and 100% of staff have received at least one dose of COVID-19 vaccine, or have been granted qualifying exemption, or identified as having a temporary delay as recommended by the CDC (Centers for Disease Control and Prevention), the facility is compliant under the rule; or Less than 100% of all staff have received at least one dose of COVID-19 vaccine, or have been granted qualifying exemption, or identified as having a temporary delay as recommended by the CDC, the facility is non-compliant under the rule.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to maintain resident's visual privacy for one out of 33 sampled residents (Resident 238) when the privacy curtain was not pulled...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to maintain resident's visual privacy for one out of 33 sampled residents (Resident 238) when the privacy curtain was not pulled and the door to the resident's room was left wide opened, exposing his diaper and legs.
This deficient practice had the potential to negatively affect resident's dignity and could potentially cause feeling of being shameful.
Findings:
During an observation, on 2/8/22, at 1:05 PM, Resident 238 was curled up in bed asleep, turned on his right side, facing the window, with his diapers and legs exposed, visibly seen from the hallway.
In an interview on 2/8/22 at 1:06 PM, the Registered Nurse (RN) 1 was called to attend to the resident and described resident as tilted on his right side with his legs and diaper exposed. RN 1 stated, the resident was inadequately covered and curtain should be pulled to provide privacy. When asked the reason for providing privacy, RN 1 stated, it's for dignity and it can be shameful.
Review of the facility policy and procedure titled, Patient Rights and Responsibilities, with the last revised date of 5/2019 indicated, Policy: . to recognize and respect the individuality Each patient/ resident is entitled to . respect for individual dignity. Procedure: . 11. Privacy curtains will be used in .
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 44 was admitted on [DATE], with diagnoses that includes hemorrhagic stroke (ruptured blood vessel causes bleeding in...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 44 was admitted on [DATE], with diagnoses that includes hemorrhagic stroke (ruptured blood vessel causes bleeding inside the brain) with left hemiplegia (partial paralysis on one side of the body).
Review of Resident 44's progress notes, dated 1/28/21, indicated Resident 44 noted with left abdominal fold abrasion and right upper buttock abrasion.
Review of Resident 44's care plan, and concurrent interview with Wound Care Nurse (WCN) 1, 2/10/22, at 11:50 AM, there was no care plan found addressing the left abdominal fold abrasion and right upper buttock abrasion. WCN 1 acknowledged the findings and stated nurses who found the new skin condition should also complete a new skin care plan.
3. Resident 77 was admitted on [DATE] with diagnoses including schizophrenia (a mental illness that affects how a person thinks, feels, and behaves)
Review of Resident 77's physician orders, dated 2/2/22, indicated nystatin powder to abdominal folds rashes BID [twice a day] x 14 days then re-eval [re-evaluate].
Review of Resident 77's clinical record and concurrent staff interview with RN 5, on 2/10/22, at 2:45 PM, there was no evidence a care plan was completed to address Resident 77's abdominal folds rashes. RN 5 acknowledged the findings and stated licensed staff who assessed the new skin condition should complete a skin care plan.
During an interview with Director of Staff Development (DSD) on 02/11/22, at 1:57 PM, DSD stated the licensed nurse who found the new skin condition should call the doctor, complete a skin care plan.
Review of facility policy and procedure titled Wound Care Management, revised 8/2019, indicated D. Evaluation of the Plan of Care Includes: 1. Changes to the plan of care if expected outcomes are not achieved .
4. During a review of Resident 35's record titled Inpatient Record dated 2/4/22, the Inpatient Record indicated that Resident 35 was admitted on [DATE] with diagnoses that included hypertension, depression and anxiety
During a review of Resident 35's Comprehensive MDS dated [DATE], and Quarterly MDS assessment dated [DATE], indicated that the SNF documented that Resident 13 is cognitively intact. Resident 35 had a bed alarm and a wheelchair alarm placed on her wheelchair. The assessment did not trigger (requiring in-depth review for care planning) for the use of bed and chair alarm restraints.
During an observation on 2/7/22, at 10:30 AM, Resident 35's bed had three one half side rails up; two placed on the upper left and right side of the bed and one placed on the lower right side of the bed. Her wheelchair had a yellow wheelchair alarm, measured 3 inches by 4 inches in size attached to the wheelchair with a wire looped around the wheelchair.
During observations on 2/8/22, at 11:05 AM, in Resident 35's room, Resident 35's wheelchair alarm was observed missing.
During an interview with Resident 35, on 2/8/22, at 11:15 AM in the company of Charge Nurse (CN) 2, Resident 35 stated she did not know what happened to her wheelchair alarm. She stated that she suspected that staff took her wheelchair alarm when they replaced her old wheelchair with the new wheelchair. She said, The wheelchair alarm is missing and I do not know what happened to it.
During concurrent interview with CN 2, on 2/8/22, at 11:20 AM, CN 2 confirmed that Resident 35 had a yellow colored wheelchair alarm attached to her wheelchair.
During concurrent interview on 2/8/22, at 11:23 AM, CN 2 acknowledged that Resident 35's medical record did not contain a care plan for the use of physical restraints. She confirmed that the MDS did not trigger CAA for restraint use. She stated that the facility did not consider bed alarm a restraint and did not develop and implement a restraint care plan with interventions for the use of physical restraints.
Review of Resident 35's Physician's Orders dated 2/2022, indicated that on 4/8/21, .bed side rails up while in bed (upper and lower) as a safety precaution related to involuntary tremors . and staff check placement every shift On 9/25/20, and 9/28/20, the physician order indicated, fall risk: Tab magnetic alarm when in bed. Check placement and function QSHIFT.
5. Review of the Face Sheet and the History and Physical (H & P), dated 1/21/22, the Face sheet indicated Resident 137 was admitted to the facility on [DATE]. The Assessment and Plan section of the H & P included the diagnoses of chronic systolic heart failure (the left ventricle of the heart, which pumps most of the blood, has become weak), chronic pain syndrome and chronic anasarca (general swelling of the whole body), and is being admitted to the skilled nursing facility under hospice.
Review of the Minimum Data Set (MDS, an assessment tool) dated 1/31/22, the Section O, Special Treatment, Procedure and Program of the MDS indicated, K. Hospice Care, was marked.
In a concurrent interview and record review on 2/8/22, at 2:07 PM, with the RN 1 and the Nurse Manager (NM) 1, the lists of CPs were reviewed. The lists of CPs did not have Hospice Care Plans developed either by the facility or the Hospice Agency (HA). RN 1 stated, she did not find the Hospice CP. NM 1 acknowledged there was no CP developed for Hospice Care, there should be a care plan for hospice.
In an interview on 2/10/22 10:19 AM, with the NM 1, NM 1 stated, if there was no CP, there was no way or any documentation that would reflect the care the resident received, where else can we get the information?
In an interview on 2/10/22, at 3:15 PM, it the HA DON and the HA Case Manager (CM), HA DON searched the Medical Record and acknowledged there was no CP developed by the HA for Hospice care. DON explained, there was a big shift in their office, but we can produce it.
Record review of the facility's Policy and Procedure titled, Hospice Policy, with the last revised date of 7/10 indicated, Procedure: 1. 7. The RN (Registered Nurse) from the hospice agency and the Team Leader caring for the resident will jointly develop an interim plan of care to meet the current needs of the resident.
Review of the Hospice Agreement, dated 7/7/20, the Hospice Agreement indicated, III. Responsibilities of the Parties: 3.1 Hospice Responsibilities: . 3.1.5: Provisions of Hospice Services: . Hospice shall provide . to Resident in accordance with the Plan of Care for Resident .
Based on observation, interview, record review the facility failed to develop a comprehensive care plan (CCP) that included measurable objectives and timeframe for five (5) out of 33 sampled residents (Residents 135, 44, 77, 35 and 137) when:
1. For Resident 135, there was no evidence a comprehensive care plan for Dialysis (a procedure to remove waste products and excess fluid from the blood when the kidneys stop working properly) was developed.
2. For Resident 44, there was no evidence skin care plan was developed to address left abdominal fold abrasion and right upper buttock abrasion.
3. For Resident 77, there was no evidence skin care plan was developed to address abdominal folds rash.
4. For Resident 35, there was no evidence a CCP was developed to address the use of restraint (is any physical or chemical means or device that restricts resident's freedom).
5. For Resident 137, there was no evidence the facility and the Hospice Agency developed a CCP to address resident's Hospice care and needs.
Failure to care plan residents goals, needs and preferences had the potential to negatively affect the care and services rendered to residents and had the potential to negatively impact their quality of life.
Definitions:
Comprehensive Care Plan is a person-centered care plan for each resident, consistent with the resident's rights that includes measurable objectives and timeframes to meet a resident's medical, nursing, and mental and psychosocial needs that are identified in the comprehensive assessment. The comprehensive care plan describes the resident's goals for admission and desired outcomes, resident's preference and potential for future discharge, services that are to be furnished to attain or maintain the resident's highest practicable physical, mental, and psychosocial well-being.
Person-centered care means to focus on the resident as the focus of control, and support the resident in making their own choices, and having control over their daily lives.
According to the facility definition, Hospice is a philosophy of care which allows the terminally ill to experience a meaningful, comfortable, and dignified death.
According to the Hospice Agreement, Plan of Care means a coordinated plan of care for individual Patient for the palliation or management of the Patient's terminal illness and related conditions that (a) clearly delineates the services to be provided by Hospice and Facility; (b) is consistent with Hospice philosophy; (c) is based on an assessment of the Patient's current medical, physical, psychological and social needs, and unique living situation: (d) reflects the participation of Hospice, Facility, the Patient and the Patient's family, as appropriate: and (e) complies with applicable federal and state laws and regulations and Accreditation Standards.
Findings:
1. During a review of the Face Sheet and the Progress Notes dated 2/5/22, the Face sheet indicated Resident 135 was admitted to the facility on [DATE]. The section on the Assessment/Plan section of the PN indicated, new onset of end stage renal disease (kidney failure), on hemodialysis (a machine that filters wastes, salts and fluid from the blood when the kidneys are no longer healthy enough to do this work).
In an interview 2/7/22, at 12:58 PM, Registered Nurse (RN) 2 stated, Resident 135 left for dialysis earleir today, has a shunt (a connection, made by a vascular surgeon, of an artery to a vein) on the right arm, and was not back yet at this time.
Review of the Minimum Data Sheet (MDS, an assessment tool) dated 1/23/22, the section O, Special Treatments, Procedures, and Programs section of the MDS indicated, Other: Dialysis, was marked.
During an observation on 2/8/22, at 1:16 PM, there was a sign posted on the outside of resident's room, Contact Precaution. Resident was awake sitting in a chair, with the overbed table in front of her. Resident 135 stated, her shunt was on the right upper arm, and she had dialysis yesterday.
In a concurrent interview and record review on 2/8/22, at 1:04 PM, with the RN 2, the Care Plans (CPs) were reviewed. There were other CPs developed but nothing to address the Dialysis needs and care for the resident. The RN 2 searched the entire Medical Record and verified there was no Dialysis Care Plan in the chart. RN 2 stated, she would initiate a Care Plan for Dialysis, pulled a template document titled Chronic Renal Failure CP and placed the date 2/8/22. When asked why there should be a CP, RN 2 stated, CPs would helped the staff to assess the resident needs with her dialysis and provide the needed care.
Review of the facility's Policy and Procedure titled, Plan of Care, with the last revised date of 9/19, indicated, Purpose: To develop, review, and update the resident's care plan . Comprehensive Plan of Care: 1. 3. The evaluation of the resident's progress is made upon the care plan goals and the resident's plan of care, treatment and services.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure residents were free from a medication error rate of 5 percent or greater for six of 8 sampled residents (Resident 538,...
Read full inspector narrative →
Based on observation, interview, and record review, the facility failed to ensure residents were free from a medication error rate of 5 percent or greater for six of 8 sampled residents (Resident 538, 123, 539, 540, 541, and 115) during medication pass observation when:
1. For Resident 538, Registered Nurse (RN) 3 did not give Fluticasone nasal spray (a medicine used to treat allergy or non-allergy nasal symptoms such as runny nose, and sneezing) as per the manufacturer's instructions,
2. For Resident 123, Licensed Vocational Nurse (LVN) did not rotate injection sites of Copaxone (glatiramer acetate, a medicine that is used to treat multiple sclerosis, a disease that impacts the brain and nerves) as per manufacturer's instructions (Refer to F755),
3. For Resident 539, 540, 541, and 115, RN 2 prepared medications for four Residents at the same time.
These failures resulted in three medication errors out of 31 opportunities with the facility's medication error rate of 9.68 percent.
Findings:
1. Review of manufacturer's instructions of Fluticasone nasal spray (a medicine used to treat allergy or non-allergy nasal symptoms such as runny nose, and sneezing), dated December 2019, the instructions indicated, . Step 2: Close 1 nostril (openings in the nose). Tilt your head forward slightly . Step 3: Start to breathe in through your nose . Step 4: Breathe out through your mouth .
During a medication pass observation on 2/9/22, at 8:40 AM, in Resident 538's room, RN 3, administered Fluticasone nasal sprays to Resident 538. RN 3 did not tilt Resident 538's head. Resident 538 did not breathe out through mouth after inhaling (breathing in) the nasal spray. RN 3 did not instruct Resident 538 to tilt the head, and to breathe out through mouth after inhaling the nasal spray
During an interview on 2/9/22, at 1:50PM, RN 3 acknowledged not following the manufacturer's instructions of Fluticasone spray.
2. During an observation on 2/8/22, at 9:00 AM, in Resident 123's room, LVN 3 administered (gave) Copaxone injection (a way of giving a liquid medicine by using a needle and syringe) to Resident 123's right abdomen.
Review of Resident 123's Medication Administration Record (MAR), dated 1/25/22 to 2/8/22, indicated Copaxone was administered on the following dates:
On 1/25/22 at 9:00 AM, given in the left arm
On 1/26/22 at 9:00 AM, given in the right arm
On 1/27/22 at 9:00 AM, given in the left arm
On 1/28/22 at 9:00 AM, given in the right arm
On 1/29/22 at 9:00 AM, given in the left arm
On 1/30/22 at 9:00 AM, given in the right arm
On 1/31/22 at 9:00 AM, given in the left arm
On 2/1/22 at 9:00 AM, given in the right arm
On 2/2/22 at 9:00 AM, given in the left arm
On 2/3/22 at 9:00 AM, given in the right arm
On 2/4/22 at 9:00 AM, given in the left arm
On 2/5/22 at 9:00 AM, given in the right arm
On 2/6/22 at 9:00 AM, given in the left arm
On 2/7/22 at 9:00 AM, given in the right arm
On 2/8/22 at 9:00 AM, given in the right abdomen
During a concurrent interview and record review on 2/8/22, at 11:51 AM, with Charge Nurse (CN) 2, Resident 123's MAR, dated from 1/1/22 to 2/8/22 was reviewed. CN 2 acknowledged, the left arm and right arm were rotated every other day instead of weekly for Copaxone.
During an interview with Pharmacist 1, and review of Resident 123's MAR on 2/8/22, at 11:54 AM, Pharmacist 1 acknowledged, the left arm and right arm were used every other day instead of weekly from 1/25/22 to 2/7/22 for Copaxone.
During an interview on 2/8/22, at 12:01 PM, LVN 4 acknowledged, she did not rotate the injection sites as per manufacturer's instructions by using the same site more than 1 time a week.
During an interview on 2/8/22, at 12:15 PM, Pharmacist 1 stated, the nurses did not follow the manufacturer's instructions to rotate the same injection site every week for administration of Copaxone.
During an interview on 2/8/22, at 12:18 PM, LVN 5 acknowledged, she did not rotate the injection sites as per manufacturer's instructions by using the same site more than 1 time a week.
Review of manufacturer's instructions of Glatopa (also known as Copaxone), dated July 2019, indicated, . Do not stick the needle in the same place(site) more than 1 time each week . Avoid injecting in the same site over and over again .
3. During a medication pass observation on 2/9/22, at 9:08 AM, RN 2, prepared the following medications for Resident 539, 540, 541, and 115 all at the same time. RN 2 placed each resident's medications into four different plastic bags as follows:
(a) For Resident 539, RN 2 prepared 200 mg (milligrams) of Docusate Sodium (Stool softener) oral liquid,
(b) For Resident 540, RN 2 prepared Celecoxib (Nonsteroidal anti-inflammatory drug) 200 mg 1 capsule,
(c) For Resident 541, RN 2 prepared, Synthroid (same as Levothyroxine, a medicine to treat hypothyroidism - a condition in which thyroid gland doesn't produce enough hormones) 100 mcg (micrograms) 1 tablet; Ferrous Sulfate (an iron supplement) 325mg 1 tablet; Amlodipine (a medicine to treat high blood pressure) 2.5mg 1 Tablet; Pantoprazole (medicine to help relieve heartburn) 40 mg 1 Tablet; Memantine (a medicine to treat dementia) 10 mg 1 tablet,
(d) For Resident 115, RN 2 prepared, Amlodipine 10mg 1 tablet and Benazepril (a medicine to treat high blood pressure) 40 mg 1 tablet.
During an interview on 2/9/22, at 12:17 PM, RN 2 stated, she was instructed that it is acceptable to prepare multiple residents' medications at the same time.
During an interview on 2/9/22, at 12:55 PM, LVN 7 verified, One at a time when preparing medications for residents.
During an interview on 2/9/22, at 1:50 PM, RN 3 stated, One at a time is safer, when preparing medications for residents.
Review of the facility's policy and procedure (P&P) titled, Medication: Administration, dated July 2011, indicated, . 4. Medications will be prepared and administered to one patient at a time .
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interview and record review the hospital failed to ensure a Registered Dietitian (RD) provided frequent o...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interview and record review the hospital failed to ensure a Registered Dietitian (RD) provided frequent oversight of food and nutrition services and consultation to the Kitchen Supervisor which resulted in deficient practices related to the competency of foodservice staff for the following:
a. Cooldown monitoring of foods capable of supporting bacterial growth associated with foodborne illness;
b. Safe storage of refrigerated foods;
c. Provision of timely and relevant dietary staff training related to the scope and nature of foodservice operations and
d. Consistent use of standardized recipes
These failures had the potential to lead to foodborne illness in a highly susceptible population for greater than 50 residents at the [NAME] and Coastside campuses who received food from the kitchen.
Findings:
1. The intent of the Federal regulation as it pertains to the RD, is the RD is responsible for the functions of food and nutrition services including developing and implementing person centered education for facility staff, and overseeing food preparation, service and storage. The RD can delegate activities but is still responsible for the overall functions of food and nutrition services. If a Registered Dietitian does not provide full-time supervision of Food and Nutrition Services, the RD continues to responsible for the overall oversight and is to provide frequent consultation to the person designated as the Director of Food and Nutrition Services.
During the federal recertification survey from 2/7-2/9/22 there multiple lapses in safe foodservice operations, staff training, and equipment maintenance (Cross Reference F802, F812 and F908).
In an interview with the Kitchen Supervisor (KS) on 2/7/22 beginning at 2 PM, at the [NAME] Campus, the KS stated he was hired 2 months ago. He described his duties as responsibility for all administrative functions as well as daily foodservice staff supervision. KS also indicated multiple staff have permanently left their position, including the Director of Food and Nutrition Services as well as multiple support staff positions such as a café manager and departmental secretary. KS also stated he was not hired as the Director of Food and Nutrition, rather was hired as a kitchen supervisor. KS stated he was unsure if staff received training or guidance from a RD. KS indicated a RD has not provided any guidance or oversight to food and nutrition services. KS described his professional training and education background as hotel and restaurant kitchens.
In an interview on 2/8/22 at 9:50 AM, the Director of Business Development (DOB) stated considering the resignation of the previous Clinical Nutrition Manager and long-term vacancy of the Director of Food and Nutrition Services the hospital discussed the possibility of contracting with a staffing agency to hire a qualified director to oversee food and nutrition services, however no action was taken.
In a telephone interview on 2/08/22 1:30 PM, the RD confirmed she did not provide foodservice oversight or guidance. She said the previous Clinical Nutrition Manager did provide some foodservice oversight. The RD indicted involvement in foodservice operations is limited to the supervision of the diet clerks. She also stated a RD has not provided training or in-service to foodservice staff. The surveyor asked whether a RD completed any trayline (the process of patient meal plating) accuracy audits. The RD replied there have been none during the past 2 years.
2. During review of foodservice operations at the [NAME] and Coastside campuses from 2/7-9/22 between the hours of 9:00 AM and 3 PM there were lapses related to food safety (Cross Reference F812, Findings 1-4). In an interview Dietary Staff 1 indicted kitchen staff have not received in-services in the past year, related to food production activities.
3. During review of food production activities at the [NAME] campus on 2/8/22 it was noted dietary staff were not following standardized recipes in accordance with departmental policies (Cross Reference F802).
4. During review of foodservice operations at both the [NAME] and Coastside campus from 2/7-2/9/21 between the hours of 7:00 AM and 3:00 PM, it was noted there were multiple pieces of equipment that were broken or not maintained in accordance with manufacturers' guidance (Cross Reference F908).
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on food production operations the facility failed to employ sufficient and competent support personnel to implement foodse...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on food production operations the facility failed to employ sufficient and competent support personnel to implement foodservice operations as evidenced by 1) lapses in food production standards and 2) departmental position vacancies.
Failure to ensure sufficient and competent dietetic services staff may result in unsafe food production practices putting residents at risk for foodborne illness and decreased meal intake further compromising medical status.
Findings:
1. Recipe standardization is a key element in the efficient running of a food service institution. It plays an important role in ensuring the nutritional needs of patients are met, supporting a successful recovery. In addition, the use of standardized recipes ensures the quantity and quality of meals is consistent irrespective of who is preparing the meal.
During general food production observation on 2/8/22 beginning at 11:00 AM, it was noted DS 3 was preparing zucchini for the noon meal. DS 3 was observed placing the sliced zucchini from the boiling water in the steam kettle into a steam table pan then placing it on the steam table. No other ingredients were added.
During meal plating observation on 2/8/22 beginning at 11:00 AM, the noon meal entrée included chicken [NAME]. It was noted in place of the [NAME] sauce the meals were plated with a pale, yellow-colored gravy. In an interview on 2/8/22 at 12:10 PM, DS 4, stated the [NAME] sauce did not come in resulting in a substitution of chicken gravy. The zucchini was also noted to be plain, there was no visible seasoning. Additionally, it was noted residents with physician ordered renal diets should have received sponge cake, rather received diet gelatin instead. The surveyor inquired whether the facility had a recipe for the sauce. Concurrent review of the recipe with DS 4, the position responsible for resident meal production, revealed the ingredients for the [NAME] sauce included items such as beef broth, onions, mushrooms, salt and pepper all of which were available. DS 4 indicted the substitution was cleared with the Registered Dietitians. Concurrent review of the recipe with DS 4 for zucchini indicated the finished product should have included a blend of herbs and spices.
In a telephone interview RD 1 stated the RD's were not called to review a menu substitute, however the diet clerks may have been made aware of a substitute. In an interview on 2/9/22 beginning at 2:15 PM, Diet Clerk 1 stated the substitutes come from the Registered Dietitians, who supervised the diet clerks. DC 1 further stated if a substitute was requested, a phone call would be placed to a RD. DC 1 confirmed foodservice staff did not request evaluation of a substitution for either the [NAME] sauce or the sponge cake. DC 1 also indicated the kitchen did not have a substitute log for the RDs to review and sign.
Untitled departmental policy dated 3/17 indicated that standardize recipes shall be maintained and used in food preparation.
Dietary staff training documentation provided by the facility was limited on one training dated 8/5 and 8/6/21, titled [NAME] Geriatric Behavioral Health Unit whose focus was managing a safe environment in the specialized unit. The facility was unable to provide any training related to the operational procedures of a foodservice department.
2. In an interview with the Kitchen Supervisor (KS) on 2/7/22 beginning at 2 PM, at the [NAME] Campus, the KS stated he was hired 2 months ago. He described his duties as responsibility for all administrative functions as well as daily foodservice staff supervision. KS also indicated multiple staff have permanently left their position, including the Director of Food and Nutrition Services as well as multiple support staff positions such as a café manager and departmental secretary and most recently the store keeper whose position was to order and receive all departmental food and ancillary supplies. KS also stated he was not hired as the Director of Food and Nutrition, rather was hired as a kitchen supervisor.
Review of dietetic services departmental schedule from 2/6 through 2/19/22 revealed there were 2 open shifts, each day, for cooks on 2/6-2/9. Similarly, there were between 8 and 10 open shifts each day for food service workers from 2/7 through 2/19. The KS indicated that staffing has become a significant challenge as many of the staff work multiple jobs and may not be readily available to work extra shifts. The KS also indicated there were several new hires completing general hospital orientation on 2/7/22, however he indicated some of the recent new hires leave the position shortly after starting.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on meal distribution observations the facility failed to follow the menu when the portion sizes for 6 residents (Residents...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on meal distribution observations the facility failed to follow the menu when the portion sizes for 6 residents (Residents 38, 72, 97, 115, 242 and 243) at the [NAME] campus with physician ordered mechanically altered diets were not correct. Failure to follow the facility approved menu may result in decreased nutritional intake further compromising medical status.
Findings:
During meal plating observations on 2/8/22 beginning at 11:45 AM, the portions for all items on the steam table were ½ cup except for the mechanically altered zucchini. The serving size for the zucchini was plated as a 1/3 cup serving.
In an interview on 2/8/22 at 2:15 PM, Dietary Staff (DS) 5 indicated the portion sizes for all items was listed as 4 ounces. The surveyor asked how she determined the portion size for the mechanically altered zucchini. DS 5 indicated she had to use a smaller portion as there were not enough 4-ounce scoops. DS 5 further stated in the past when she needed additional items, such as scoops, she would tell the stock person since this was the position that completed food vendor orders. DS 5 indicated she mentioned the need for additional scoops to the supervisor, however, doesn't know what happened.
Review of the facility diet list dated 2/9/22 revealed there were 6 residents on physician ordered mechanically altered diets.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on dietetic services operations, dietary staff interview and departmental document review the facility failed to ensure fo...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on dietetic services operations, dietary staff interview and departmental document review the facility failed to ensure food safety standards when there was lack of 1) effective cooldown monitoring of potentially hazardous foods 2) lack of date receiving of foods capable of foodborne illness as well as shelf stable foods; 3) food storage practices that may promote cross contamination; 4) lapses in handwashing procedures; 5) lack of adequate air gaps in food production equipment at both the [NAME] and Coastside campus; and 6) retention of damaged products.
Failure to provide a food production environment that is safe and sanitary may result in foodborne illness, cross contamination of food and equipment and use of expired ingredients that may affect flavor and/or texture of food. Foodborne illness and cross contamination may result in gastrointestinal distress and in severe instances may result in death. The use of expired ingredients may result in a food product that is unpalatable, resulting in decreased meal intake. This had the potential to affect 108 residents who received meals from the facility.
Findings:
1. Potentially Hazardous Foods (PHFs) are those capable of supporting bacterial growth associated with foodborne illness. PHFs include items such as cooked meat and eggs as well as cooked grains such as rice, pasta and oatmeal as well as cooked vegetables. These items, once cooked, require time/temperature monitoring during the cooling process. The standard of practice is to ensure cooked items cool down from 135 degrees F (Fahrenheit) within 2 hours and to 41 degrees F or below within an additional 4 hours, for a timeframe not to exceed 6 hours (USDA Food Code, 2019).
During initial tour of the [NAME] kitchen on 2/7/22 beginning at 9:00 AM, it was noted there were 2 hotel pans of cooked oatmeal dated 2/5 and 2/6/22 respectively as well as 3 sheet pans containing 8-ounce Styrofoam containers of a soup type product. In a concurrent interview and document review Dietary Staff (DS) 1 identified the items in the containers as rice and noodle soup. DS1 stated the item was prepared on 2/6/22 in preparation for service on 2/7/22. There was also a full hotel pan of cooked, scrambled eggs, prepared on 2/6 with an internal temperature of 42 degrees F. It was also noted the hospital continued to utilize a cook/chill method for meal service, daily. The cook/chill method is a food production technique where foods are cooked in bulk ahead of time. The food is cooled then reheated prior to service.
Concurrent review of departmental documents titled Cooking and Cooling Log for the month of February revealed there were 6 days where cooling was documented. There were no documented cooling temperatures for the items prepared on 2/5 or 2/6/22. DS 1 was unsure where the remaining logs were located. It was also noted that on 2/7/22 there was a documented entry for frozen meatloaf. DS 1 confirmed the item was received frozen, fully cooked and sliced. DS 1 was unable to explain the purpose of placing a fully cooked, frozen item on the cooldown log. The surveyor inquired whether staff received training on the purpose and use of the cooldown log. DS 1 stated there was some in-service approximately 12 months ago, however there were no recent staff trainings that he could recall.
In an interview on 2/7/22 at 2 PM, the Kitchen Supervisor provided cooling logs for January 2022. It was noted cooldown monitoring was limited to 24 of 31 days. It was also noted of the 24, January 2022 logs presented four of them (1/6, 1/9, 1/17 and 1/22) did not contain any cooldown monitoring for lunch or dinner entrees, rather was limited to breakfast items such as eggs and hot cereal.
Facility policy titled Nutrition and Food Service dated 8/16 indicated it was the responsibility of the cooks to maintain chilling logs that documented adherence to food handling standards.
Review of facility document titled Statement of Deficiencies and Plan or Correction-[NAME] Medical Center D/P SNF (Distinct Part Skilled Nursing Facility) dated 1/22/21 indicated the Director of Food and Nutrition Services would randomly choose items daily for the purpose of monitoring cooldown with an implementation date of 1/4/21. There was no indication this process was implemented.
2. During the initial tour of the [NAME] kitchen on 2/7/22 beginning at 9:00 AM, there was a sheet pan containing three packages, each weighing greater than 5 pounds, of unlabeled and undated raw meat cubes. There was also a small pool of red tinged meat juices on the sheet pan.
In a concurrent interview DS 1 indicated the item was cubed pork, intended for dinner on 2/7/22. DS 1 acknowledged, without a label and date it would be difficult to determine the type of meat or how long it was in the refrigerator. It was also noted there was a cardboard box of fully thawed beef shoulder clod, delivered to the facility on 1/28/22 (10 days earlier). There was no indication on the box if the item was shipped frozen then thawed upon receipt or if it was placed in the freezer prior to refrigeration.
In an interview on 2/7/22 beginning at 2:00 PM, the Kitchen Supervisor indicated the ordering/receiving clerk left one week ago and as a result he is responsible for ordering and maintaining food supplies in addition to all other supervisory duties, as currently there is no replacement. The KS acknowledged the items should have been labeled and dated.
Departmental policy titled Nutrition and Food Service dated 8/16 indicated beef roasts were to be held no longer than 3-5 days. It was also noted this policy did not include guidance of labeling and/or dating items. Review of shipping invoices dated 1/28/22 revealed a shipment was received, however the invoice listed only fresh fruits, there was no meat listed.
Untitled departmental policy dated 8/16 guided staff when any box with perishable contents is opened a permanent pen or label will be used to indicate the date the box was initially opened and expiration date of the product.
3. Pathogens can contaminate and/or grow in food that is not stored properly. Original unprotected packaging can be sources of microbial contamination for stored food. The possibility of product contamination increases whenever food is exposed. Pathogens could be present on the exterior of the original packaging. The standard of practice would be to remove products from unprotected packaging once opened (USDA Food Code, 2019).
During the initial tour of the [NAME] kitchen on 2/7/22 beginning at 9:00 AM, it was noted there was a box of long grain rice, opened in the original packaging. Review of facility policy titled Food Safety Standards dated 8/16 provided guidance on the length of time rice could be stored, however did not provide guidance on how it would be stored to protect from potential contamination.
4. During general food production observations in the [NAME] Kitchen on 2/7/22 at 10:15 AM, DS 1 was preparing food with his gloved hand. DS 1 then proceeded to open the door to an adjacent room. DS 1 proceeded to return to his worktable with the same gloves on his hand continuing food production activities. DS 1 then went to the walk-in refrigerator, opened the door, pulled out the tray cart with pre-prepared foods. DS 1 was observed touching his face mask to adjust it. No hand hygiene was performed prior to resuming food production activities.
Departmental policy titled Uniform Dress Code (HACCP)/Personal Hygiene dated 5/17 indicated gloves should be worn during food preparation and service and shall be changed or replaced as often as handwashing is required.
5. During periods of extraordinary demand, drinking water systems may develop negative pressure in portions of the system. If a connection exists between the system and a source of contaminated water contaminated water may be drawn into and foul the entire system.
The water outlet of a drinking water system must not be installed so that it contacts water in sinks, equipment, or other fixtures that use water. Providing an air gap between the water supply outlet and the flood level rim of a plumbing fixture or equipment prevents contamination that may be caused by backflow. It would be the standard of practice to ensure the air gap is not less than 1 inch from the flood level rim (USDA Food Code, 2019).
During general food production observations, in the [NAME] kitchen, on 2/8/22 beginning at 11:30 AM, it was noted there were multiple pieces of equipment such as steam kettles that discharged water into a trough imbedded in the flooring. It was noted the discharge pipes were all located below the flood level of the drainage system.
In an interview on 2/8/22 beginning at 3:00 PM, the Director of Facilities (DOF) acknowledged the lack of adequate air gaps in the identified equipment.
In an observation on 2/9/22 beginning at 7 AM, in the Coastside kitchen there was no air gap in the 3- compartment sink adjacent to the walk-in refrigerator.
6. Wet nesting occurs when wet dishes or pots and pans are stacked, preventing them from drying and creating conditions that are ripe for microorganisms to grow. Food and Drug Administration (2019) mandates that all wares should be air dried prior to storage.
During review of the warewashing process at the [NAME] campus on 2/7/22 at 1:30 PM, it was noted there were multiple rows of ¼ hotel steam pans measuring roughly 6 x 10 inches. In a single row three of four stacked pans were wet inside.
In an interview DS 2 indicated the dishwasher has been broken for at least 6 months and perhaps longer. He stated the racks surrounding the non-functional dishwasher are intended as spaces for air drying. DS 2 indicated the hotel pans should have been fully dried prior to storage.
Review of facility policy titled Food Safety Standards dated 8/16, section titled Dishwashing/Warewashing revealed there was no guidance to staff on the process of manual warewashing with respect air drying. While there was one statement guiding staff to air dry utensils it was limited to flatware. There was no mention of other cooking related equipment.
7. Food and Drug Administration considers food in hermetically sealed containers that are compromised, swelled or leaking to be adulterated. Depending on the circumstances, rusted and pitted or dented cans may also present a serious potential hazard
During initial tour of the [NAME] kitchen on 2/7/22 beginning at 9:00 AM, of the dry storage area it was noted there were two #10 cans of prunes with an expiration date of 6/21; one can of cranberry juice cocktail, pinto beans and baby corn all with severe V-shaped dents. It was also noted there were greater than three bins of cookies, crackers and vanilla wafers with no receipt date.
In an interview on 2/7/22 beginning at 2:00 PM, the Kitchen Supervisor indicated the ordering/receiving clerk left one week ago and as a result he is responsible for ordering and maintaining food supplies in addition to all other supervisory duties, as currently there is no replacement and shipments were no longer stocked by a single employee, rather were stocked using multiple staff members.
Untitled departmental policy dated 8/16 guided staff when any box with perishable contents is opened a permanent pen or label will be used to indicate the date the box was initially opened and expiration date of the product. Facility policy titled Food Safety Standards dated 8/16 indicated cookies and crackers could be stored for 1 to 6 months from delivery.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure the Quality Assurance and Performance Improvement (QAPI) iden...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure the Quality Assurance and Performance Improvement (QAPI) identified on-going systemic issues, develop and implement appropriate plans of action to correct the identified quality deficiencies when:
1. Resident's bathrooms at [NAME] Coastside were identified to have pungent odor, peeling, cracking of vinyl flooring, and water leak were not addressed. (Refer to F 584)
2. Failed to maintain functional call light system at [NAME] Coastside since 9/30/21. (Refer to F 919)
3. The performance improvement plan did not fully reflect actions to address
identification of lapses in safe food handling practices and maintenance of the dietary physical environment. (Refer to F 803, 812 and 908)
4. Evaluation of residents population and identification of the resources needed to provide the necessary care and services was not conducted. (Refer to F 838)
Failure to identify and act upon systemic concerns had the potential to negatively affect the care and services rendered to the residents including their quality of life and could potentially cause harm.
Definition:
A QAPI plan is the written plan containing the process that will guide the nursing home's efforts in assuring care and services are maintained at acceptable levels of performance and continually improved.
A facility assessment may be similar to common business practices for strategic and capital budget planning. Strategic planning is an organization's process of defining its strategy, or direction, and making decisions on allocating its resources to pursue this strategy. However, while a facility may include input from its corporate organization, the facility assessment must be conducted at the facility level. The facility assessment will enable each nursing home to thoroughly assess the needs of its resident population and the required resources to provide the care and services the residents need. It should serve as a record for staff and management to understand the reasoning for decisions made regarding staffing and other resources, and may include the operating budget necessary to carry out facility functions.
Findings:
During a group interview on 2/11/22, at 2:05 PM, with the QAPI members, which include the Administrator, Executive Director, Continuum of Care (EDCC), Chief Nurse Officer (CNO, also the acting Director of Nursing for the Skilled Nursing Facility), MDS (Minimum Data Set) Coordinator 2, Quality Staff 1, Director of Quality also Infection Control Preventionist, Nurse Manager (NM) 1 and NM 2, the EDCC stated, the QAPI meets on a monthly basis and the last QAPI meeting was held in December, 2021. The EDCC stated, the indicators identified in the last QAPI meeting were: Fall incidents, as the highest indicator, followed by the use of restraints, hand hygiene and Antibiotic Stewardship.
Review of the Monthly QAPI Minutes from January, 2021 to December, 2021 (No record of QAPI minutes for September, 2021) indicated, the identified indicators, as mentioned on 2/11/22 meeting with the QAPI members, were discussed. The Nutrition Report included the result of the resident satisfaction survey on quality of food, food temperature, sanitation checklist, and overall quality of food services. A work order was mentioned in the December, 2021 minutes, for the non-functioning audible sound of the call light system (3 months after the issue was identified). However, there was no evidence that all the components of the call light system was followed up, and the on-going systemic issues in the residents rooms, Dietary concerns/issues identified during the survey, and lack of Facility Assessment, were not addressed.
In a group interview on 2/15/22, at 9: 30 AM, with the EDCC, NM 1 and NM 2, QS 1 and MDS Coordinator 2, the EDCC acknowledged the Dietary issues identified during the survey were not addressed and the broken tiles in the residents room and water leak with pungent odor in the Shower Room were not also identified in the QAPI meetings. The NM 1 stated, the QAPI meetings were focused mostly on the clinical aspects of residents care and the environmental issues went to the Environment of Care Committee (ECC). EDCC stated, the environment issues did not escalate to the QAPI and acknowledged environment issues identified at the ECC level should be part of the QAPI and moving forward, it would be integrated in the QAPI's Standing Agenda items. EDCC stated, she was not aware of the non-functioning audible call light issue in the Nursing Central Station at the [NAME] Coastside prior to Friday (2/11/22) and Dietary issues /concerns would also be included, we will take a look, to make it better and expand our clinical rounds. QS 1 acknowledged the facility did not develop a Facility Assessment. EDCC acknowledged the need to develop FA was not discussed in the QAPI meeting.
Review of the facility document titled, Quality Assessment and Performance Improvement, 2021, indicated, The purpose of xxx (name of the facility) Quality Assurance /Performance Improvement (QAPI) plan is to . continually assess the quality of care provided to the residents . The QAPI is a facility wide plan which applies to all department, services . QAPI committee: Maintain leadership oversight of continual progress of all departments . Ensures accountability for adherence to action items and plans .
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. During a concurrent observation and interview on 2/9/22, at 8:40 AM, with Licensed Vocational Nurse (LVN) 1 in Resident 488's...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. During a concurrent observation and interview on 2/9/22, at 8:40 AM, with Licensed Vocational Nurse (LVN) 1 in Resident 488's room, Resident 488 was sitting in a wheelchair. Resident 488 had a nasal cannula (NC), with a handwritten date label (1/17/22) which was fading and hardly legible, inserted in her nostrils. The tip of the cannula looked hazy and old. The NC was connected to the big green oxygen tank (oxygen storage vessel, held under pressure in gas cylinders), set at two Liters per minute (LPM). Resident stated she does not use the oxygen all the time but had needed to use it more the past few days stating, I'm having a ., I don't know what it is. LVN 1 acknowledged the NC needed changing. LVN 2 stated she did not know how often the NC should be changed and she would find out.
During an interview on 2/9/22, at 11:30 AM, with charge nurse (CN) 1, CN 1 stated Resident 488 was readmitted on [DATE] and was in a different room until she was moved yesterday. CN 1 stated the NC should have been changed to a new one and she thinks NC should be changed every five days. Later, CN 1 stated she could not find the policy and procedure (P & P) and might have been changed.
During a review of Resident 488's face sheet for Resident, dated 1/4/22, the face sheet indicated Resident 488 was initially admitted on [DATE].
During a review of the facility's policy and procedure titled, Changing Resident's Disposable Respiratory Supplies, dated 4/2017, the P & P indicated Disposable respiratory supplies shall be kept clean and protected from contamination and changed at regular intervals.
5. During an observation on 2/8/22, at 11AM, Licensed Vocational Nurse (LVN) 2 entered Resident 43's room with the prepared treatment cart. LVN 2 had a face mask (N 95 mask) on, but with no face shield. LVN 2 donned new gloves and was about to start the dressing change, then stated he forgot the chucks, went out of the room, came back and placed chucks on the cart. LVN 2 removed the old/soiled dressing from the left hip of Resident 43, removed his gloves but did not perform hand hygiene. LVN 2 donned new gloves, opened the clean dressings, got the wound cleanser, and sprayed Resident's wound and changed his gloves. LVN 2 then packed the wound with wet to moist dressing, then covered the wound with a foam dressing. LVN changed his gloves and repositioned Resident, took the treatment cart out of the room, and washed his hands.
During an interview on 2/8/22, at 11:25 AM with LVN 2, LVN 2 stated they do not have to perform hand hygiene during the dressing change as long as they are frequently changing their gloves. LVN 2 stated he would check their policy to confirm this. Later, LVN 2 acknowledged he was supposed to perform hand hygiene especially after removing his glove. LVN 2 also acknowledged he was supposed to wear a face shield during the dressing change to protect against splashes and stated sorry, I forgot.
During an interview on 2/9/22, at 1PM, with the Infection preventionist/Director of Quality(IP/DoQ), IP/DoQ stated staff should be performing hand hygiene in between change of gloves, after touching and removing soiled dressings, and do not have to be in the policy as this is CDC guideline. IP/DoQ stated when staff anticipate splashes, they should be wearing face shield to protect against pathogen exposure. IP/DoQ stated staff should also be wearing gown to protect against pathogen exposure. IP/DoQ stated staff should have more personal protective equipment when performing wound treatment.
During a review of the facility's policy and procedure (P & P) titled, IC 2-1: Hand Hygiene, dated 5/2019, the P & P, indicated, . 1. Gloves are not a substitute for handwashing or hand sanitizing. 2. Gloves shall be for hand contaminating activities such as having contact with blood or body fluids etc., and removed and hands washed or sanitized as soon as the activity is completed .
During a review of the facility's P & P titled, Standard and Transmission Based Precautions, dated, 9/2018, the P & P indicated, 2.a. Perform hand hygiene after contact with blood, body fluids .non intact skin . After removing gloves .3. PERSONAL PROTECTIVE EQUIPMENT (PPE), PPE should be worn when contact with blood or body fluids may occur during patient care .
Based on observation, interview and record review, the facility failed to implement and maintain its infection control program according to standard of practice and facility's policy and procedures when:
1. Certified Nurse Assistant (CNA) 8 was not wearing appropriate eye protection (face shield). CNA 8 was designated to both areas with residents with active COVID-19 infection and without, within the same shift.
2. Facility COVID-19 Outbreak was not reported to California Department of Public Health (CDPH).
3. Visitor Screening for COVID was not performed per policy.
4. Oxygen nasal cannula for Resident 488 appeared hazy and was outdated
5. Licensed Vocational Nurse (LVN) 2 was not wearing face shield and did not perform hand hygiene during wound dressing change with Resident 43.
Failure to implement infection prevention practices had the potential for cross contamination of infection that can compromise the health and safety of the residents, staff, and visitors.
Definition:
COVID-19 - a respiratory disease caused by SARS-CoV-2, a coronavirus discovered in 2019. The virus spreads mainly from person to person through respiratory droplets produced when an infected person coughs, sneezes, or talks.
Isolation Rooms/ Red zone- areas where residents with COVID-19 infection are placed.
Green zone- areas where residents who recovered or are free of COVID-19 are placed.
Findings:
1. During an interview with Executive Director for Continuum of Care (EDCC), on 2/8/22, at 2 PM, EDCC stated [NAME] Coastside has an ongoing COVID-19 outbreak of three residents located in red zone. EDCC stated the red zones were rooms 104,106 and 108.
During an observation on 2/8/22, at 2:41 PM, and concurrent interview with Certified Nurse Assistant (CNA) 8, near the red zone entrance, CNA 8 was not wearing a faceshield or eye protection. CNA 8 stated she was designated to work with three residents on the red zone and two residents in the green zone. CNA 8 stated she forgot her faceshield in the staff break room where she had lunch.
During an interview on 2/9/22, at 1:44 PM, the Infection Preventionist (IP) stated, all staff should wear eye protection or faceshield within the facility to prevent spread of infection because of the ongoing COVID-19 outbreak. IP acknowledged CNA 8 was designated to work for both red zone and green zone and safe to do so as long as CNA 8 wear appropriate Personal Protective Equipment (PPE) between resident care. IP acknowledged there was no designated break room for staff assigned to the red zone and all staff can share the common break room as long as they keep six feet social distancing. IP stated the facility dedicated the [NAME] Coastside rooms 104, 106 and 108 for resident with active COVID-19 infection.
During a review of facility's COVID-19 Mitigation Plan, dated 7/7/20, indicated 1. Testing and Cohorting . PUIs (Person Under Investigation) and Positive Residents: [NAME] Coastside Hospital utilizes Transition and Isolation Rooms (Rooms 104, 106 and 108) to segregate those with possible symptoms, potential exposure and for those under investigation pending test outcomes Staffing Plan: To limit transmission of COVID-19, staffing who work with COVID-19 Residents are dedicated and consistent to that unit. Clinical and other staff with direct resident contact . do not rotate between floors during the period they are working each day .
Review of facility's policy and procedure, titled Management of Influx of Infectious Patients, revised 3/2017, indicated . e. Employee shall use the appropriate personal protective equipment based on SMC's ([NAME] Medical Center) Infection Control policies and the CDC's (Center for Disease Control and Prevention) disease specific guidelines found in the Infection Control Manual.
2. During a review of facility's COVID-19 line list, indicated as follows: (a) on 1/10/22: two Residents tested positive for COVID-19. (b) on 1/17/22: two Residents tested positive for COVID-19 (c) on 1/20/22: five Residents tested positive for COVID-19. (d) on 1/24/22: six Residents tested positive for COVID-19 (e) on 1/27/22: five Residents tested positive for COVID-19
During an interview on 2/9/22, at 1:55 PM with IP, IP stated he reported the COVID-19 outbreak to the California Department of Public Health (CDPH) but was not able to provide evidence IP notified CDPH about the facility outbreak on any dates indicated in the facility COVID-19 line list.
Review of facility's policy and procedure, titled Outbreak Investigation and Management, revised 3/2017, indicated . Process . A. Confirm an outbreak exists . 15. Notify public health department especially if the case involves a reportable disease 16. Notify public and Department of Health Services .
Review of facility's policy and procedure, titled Management of Influx of Infectious Patients, revised 3/2017, indicated . Definition: An influx of patients is an emergency situation involving an outbreak, an epidemic or pandemic . Responsibilities: . 2. Infection Control sahll stay abreast of potential influx occurences via communication with: . b. California Department of Health Services (State Level) .
Review of facility's policy and procedure, titled Unusual Occurrence Reporting Requirements, revised 1/2015, indicated Policy: The Director/designee will report all unusual occurrences and sentinel events to the Director of Quality and Risk Management and the California Department of Public Health, Licensing and Certification Program . Procedure 1. All unusual occurrences will be thoroughly investigated and documented. 2. If the occurrence is considered unusual according to Title 22 section 724541, or a sentinel event . or is reportable to the Ombudsman and/or California Department of Public Health (CDPH), notification will be made within 24 hours by telephone by the Director/designee. 3. The following list contains examples of the above Title 22 reference . b. An epidemic outbreak of any disease, prevalence of communicable disease . 4. The Director will provide a written description of the occurrence including the facts known at the time. The written notification shall include the information outlined on the attached Unusual Occurrence Reporting Form for Facilities and Licensing and Certification Review Form for Supervisors. The letter can be mailed or faxed to the CDPH. The Director will keep a copy of the letter .
According to AFL 20-75.1, dated July 22, 2021, indicated SUBJECT: Coronavirus Disease 2019 (COVID-19) Outbreak Investigation and Reporting Thresholds . All Facilities Letter (AFL) Summary . This AFL reminds licensed health facilities of requirements to report outbreaks and unusual infectious disease occurrences to their local health department (LHD) and Licensing and Certification District Office and provides investigation and reporting thresholds for reporting for COVID-19 . Long-Term Care Facilities and Long-Term Acute Care Hospitals: Outbreak Definition =1 facility-acquired COVID-19 case in a resident .
3.The facility failed to follow COVID screening in accordance with their mitigation plan for all visitors and staff.
During an observation on 2/7/22 at 8:30 AM, the Security Officer (SO) responsible for screening, did not screen three CDPH Surveyors, visitors, and hospital personnel.
During an interview with SO on 2/8/22 at 8:40 AM, stated he was not instructed on screening for COVID.
During an interview on 2/8/22 at 11:00 AM, the Infection Preventionist (IP) stated he had provided a complete packet with screening instructions to the Security Manager. He indicated the Security Manager was responsible for distributing the information to all Security Officers working at the Main Entrance to the facility.
A record review of a document titled Coronavirus Disease 2019 (COVID-19) Mitigation Plan for Skilled Nursing Facilities indicated HCP (health care personnel) Screening: all those who enter the Acute and Post Acute settings are screened for COVID 19 symptoms via screening stations at entrances of [NAME] Medical Center .screening logs document the name of each person, their temperature, and answer to associated screening questions .
A record review the document Daily Symptom Check and Screening Upon Entering Facility, indicated .we will no longer require completion of an attestation (proof) form. Instead, staff and physicians will perform the following: 1. Show identification badge to screener, 2. Self-check for symptoms, 3. Perform hand hygiene, 4. Assure that you are wearing a well-fitting mask and 5. Affix a sticker to your badge.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on dietetic services observations, dietary and administrative staff interview and departmental document review the facilit...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on dietetic services observations, dietary and administrative staff interview and departmental document review the facility failed to ensure essential dietetic services equipment was functional at both the [NAME] and Coastside locations when there were multiple pieces of equipment that have been non-functional from 2 months to greater than 12 months. Failure to maintain equipment in a safe and functional manner may affect the ability for the department to operate in a safe and effective manner which may result in nutritional risk to residents. This has the potential to affect the efficient delivery of meal services to 108 residents.
Findings:
1a. During evaluation of warewashing procedures at the [NAME] kitchen, and concurrent interview with Dietary Staff (DS) 2 on 2/7/21 beginning at 1:30 PM, he indicted the dishwasher was currently non-functional. DS 2 stated the equipment has been broken for at least 6 months and perhaps for closer to one year. He stated there was intermittent work conducted on the machine, however he was unsure of the status.
During observation of patient meal plating on 2/8/21 beginning at 11:45 AM, revealed the conveyor on the trayline was non-functional. This resulted in staff having to manually push each individual tray around the circular centralized piece of equipment, measuring greater than 25 feet in circumference.
In an interview on 2/08/22 at 3:00 PM, the Director of Facilities (DOF), explained the Engineering department have rebuilt plumbing and electrical components after which they discovered there was an issue with the conveyor belt, and are currently waiting for parts. With respect to the trayline the Facility Director stated he has been working on replacement options as the equipment is too old to get parts. The surveyor asked if the Engineering department completed any risk assessment of current equipment. He stared there was not. The surveyor also inquired if the Engineering department had a method of evaluating the timeliness of assessments and/or repair of non-functional dietary equipment or a preventive maintenance program. He stated there was not. The surveyor also requested a timeline of actions taken on the both the dishwasher and the trayline.
Review of undated document titled Trayline Repair Timeline noted the conveyor and cold plates have been non-functional since 3/2021. The timeline indicated the facility spent from 3/21 until 4/21 attempting to repair at which time it determined all repair options were exhausted. It was also noted there was a lapse of 4 months while searching for a vendor. A vendor was identified in 8/21, however the parts were not ordered until 2/8/22 (6 months later), during the recertification survey. As of 2/15/21 the facility did not submit documentation demonstrating a timely and effective process for repairing the dish machine.
b. Materials that are used in the construction equipment shall be durable, corrosion resistant, and nonabsorbent and be finished to have an easily cleanable surface, resistant to decomposition (USDA Food Code, 2017).
During a general physical environment observation, in the dish room at the [NAME] kitchen, on 2/7/22 at 1:30 PM, there was a black unidentified substance, resembling mold, on top of clear silicone caulking in the area where the stainless-steel backsplash connected with the wall tiles. The surveyor ran a white clean paper towel along the caulking, wiping the black substance onto the paper towel. It was also noted there was an area measuring approximately 4 inches along the backsplash where there was no caulking, allowing moisture to seep between the backsplash and the wall.
In an interview, on 2/08/22 at 9:50 AM, the Director of Business Development stated there have not been any environment of care rounds, assessing the physical environment of dietetic services, during the past 2 years.
2a. During general dietetic services observations at the Coastside kitchen on 2/9/22 beginning at 7:00 AM, it was noted the patient meal rethermalization cart was held closed using Velcro straps affixed to the side of the cart. In a concurrent interview DS [NAME] indicated the cart door lock has been broken for a long time, however, was unable to recall a specific timeframe.
Materials that are used in the construction of equipment shall be nonabsorbent and finished to have a smooth and easily cleanable surface (USDA Food Code, 2017).
b. It would be the standard of practice to ensure equipment for cooling food shall be sufficient in number and capacity to provide food temperatures as specified under Chapter 3 of the USDA Food Code, 2017. The 2017 USDA Food Code, Chapter 3 specifies that stored frozen foods shall be maintained frozen.
In the dry storeroom it was noted the internal temperature of Freezer A was recorded as 29 degrees Fahrenheit (a metric unit of measure). Additionally, the external temperature reading of Freezer C recorded 0 degrees Fahrenheit, however two internal thermometers indicated the temperature was +6 and +8 degrees Fahrenheit respectively. It was also noted the Freezer B was listed as out of service on 12/17/21 with a notation that parts were ordered. Both Freezer B and Freezer C were completely full with cardboard food boxes, with limited space for effective air circulation.
A follow up observation in the dry storage room, on 2/9/22 at 11:20 AM, the nutritional supplements in Freezer A were not frozen solid, rather were soft to touch, indicating the item was in the process of thawing. The internal temperature of a 4-ounce carton was recorded as 14 degrees Fahrenheit.
Departmental policy titled Food Safety Standards dated 8/16 indicated frozen foods must be stored at 0 degrees Fahrenheit or less.
c. During general kitchen observation on 2/9/22 at 10:50 AM, at the Coastside kitchen Docking station A was not functioning. In a concurrent interview stated DS 6 stated this piece of equipment has not functioned for several years. The docking station is a necessary piece of equipment for reheating patient meals. When meals are reheated, a specialized cart is plugged into the docking station. An average reheating cycle can require 45-60 minutes depending on the types of foods being reheated. It was also noted that each docking station had the capacity to reheat 24 meals and the facility was currently limited to 3 docking stations.
Review of the current facility license, dated 1/1/22 listed 111 distinct part skilled nursing beds. Based on the licensed bed capacity the facility did not have enough dietetic services equipment to serve meals to the licensed bed count.
d. During observation of the dishwashing process on 2/9/22 at 11:00 AM, it was noted the temperature gauge on the dishwasher was not functioning. In a concurrent interview DC 1 stated the dishwasher used to be a high temperature machine for sanitation and was converted to a low temperature machine because the water booster was broken. The final rinse temperature on the water gauge was consistently 108 degrees Fahrenheit. The surveyor placed a waterproof holding thermometer through greater than 3 dishwashing cycles. The maximum water temperatures ranged from 74 -81 degrees Fahrenheit. A holding thermometer records both the maximum and minimum temperatures or a specified period of time, in this case a dishwashing cycle (DeltaTrak, 2022). Concurrent observation of the manufacturers' data plate operating specifications listed a minimum temperature of 110 degrees Fahrenheit.
e. It would be the standard of practice to ensure multiuse food contact surfaces are free of breaks, open seams, cracks, chips, inclusions, pits, and similar imperfections. The surface shall also be smooth and easily cleanable (USDA Food Code, 2017).
During general dietetic services observations at the Coastside campus on 2/9/22 beginning at 11:00 AM, there were multiple holes in the stainless steel food production counter adjacent to the reach in refrigerator. In a concurrent interview DS 6 indicated there used to be a different coffee machine and the holes were intended for the water line as well as electrical cords for the machine.
f. During general dietetic services observations on 2/9/22 beginning at 11:00 AM, the surveyor asked DS 6 if the oven and stove were utilized. DS 6 indicated only one side of the oven was used to heat resident alternate meals. DC 6 indicated the other side was not fully operational.
In an interview on 2/9/22 beginning at 11:35 AM, the Maintenance Supervisor (MS) acknowledged there were multiple pieces of equipment that was non-functional. MS stated the oven was purchased new several years ago, was under warranty and required a new ignitor assembly. MS indicated he had no documentation to validate the parts were ordered, rather only had a picture of an appliance repair van that came to the facility. Similarly, MS staff indicated a transformer for the dishwashing machine was ordered and a freezer defrost heater was also received on 2/7/22. MS also acknowledged the docking station was broken and unrepairable, however the facility has not taken steps to order a replacement. During the concurrent interview the surveyor requested validation of purchase orders and/or invoices for the repair and replacement parts for the identified equipment. The surveyor also inquired if the facility completed an assessment of the functionality or viability of dietetic services equipment. MS indicated no assessment has been completed. As of 2/15/22 the facility failed to provide any additional information with respect to equipment repairs.
Review of facility document titled Facility Wide Self Assessment dated 7/12/21 revealed while the facility completed an assessment, which included resident and workforce profiles along with the building and physical environment, the equipment assessment was limited to patient care equipment such as medical and physical therapy equipment as well as fire alarms. The assessment did not include an evaluation of dietetic services food production/storage equipment.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide training to all nursing staff how to perform r...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide training to all nursing staff how to perform range of motion (ROM) exercises to residents in accordance with the facility policy. (Refer to F 688)
This failure could potentially delay the identification of issues and provision of care to prevent further decline of resident's functional status.
Findings:
Resident 98 was admitted on [DATE] with diagnosis including history of cerebral vascular attack (CVA or stroke include symptoms like trouble walking, speaking, and understanding, as well as paralysis or numbness of the face, arm, or leg).
During an observation on 5/2/22, at 10:09 AM in Resident 98's room, Resident 98 was in bed alert and was waving her left arm. Resident was not able to move her right arm.
Review of Resident 98's care plan, dated 4/8/22, indicated CNA (Certified Nurse Assistant) to provide ROM during adls (Activities of Daily Living) to UE (upper extremities) and LE (lower extremities).
During an interview with CNA 22, on 5/4/22, at 11:11 AM, CNA 22 stated he was responsible for assisting Resident 98 range of motion exercises. CNA 22 considered ROM exercise when she assisted Resident 98 to raise her arms, put on a gown and arms down. CNA 22 was not able to verbalize the frequency and duration of the exercise.
Resident 38 was admitted on [DATE], with diagnoses including CVA and hemiplegia (paralysis of one side of the body).
Review of Resident 38's care plan, dated 2/18/22, indicated CNA to provide ROM during adls to UE and LE.
During an observation on 5/5/22, at 11:51 AM, in Resident 38's room, Resident 38 was in bed alert. Resident 38 was unable to move his right arm.
During an interview on 5/5/22, at 11:52 AM, CNA 19 stated, Resident 38's right arm was contracted. CNA 19 stated she provide range of motion to Resident 38's right upper extremity by moving the right lower arm from his right side and put the lower arm to his chest.
CNA 19 was not able to verbalize the frequency and duration of the exercise.
During an interview on 5/5/22, at 1:35 PM, Physical Therapist (PT) 1 stated, Rehab Department conducts quarterly assessment of all residents in the facility. PT1 stated range of motion exercises for upper extremities should include shoulders, elbow, wrist and hands and fingers.
During an interview on 5/6/22, at 12:16 PM, Director of Staff Development (DSD) stated there used to be a specific annual training for CNAs on how to assist residents to perform range of motion exercises two years ago, but it was removed when facility renew the CNA training calendar.
Review of facility policy and procedures, titled Range of Motion, revised 8/20, indicated Purpose: 1. To maintain and improve muscle strength and tone . 3. To prevent contractures . 6. To prevent complications and disability attendant upon other physical/emotional dysfunctions and adverse states of well-being . Procedure/Responsibilities: 1. Licensed personnel are to supervised nursing assistants in ROM (range of motion) .8. The join area is left free. Limbs are supported and directed through exercises. See protocol. 9. Each joint is moved through its range 3-5 times per treatment . In-Service Education: 1. All nursing staff are instructed in the techniques of active and passive ROM, during orientation and ongoing (classroom and on the unit, all shifts). 2. All resident will receive ROM every 4 hours between the hours of 0900 and 2100 every day .
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop and document an individualized (own) facility-wide assessme...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop and document an individualized (own) facility-wide assessment (assessment of resident care needs) to determine resources needed to care for its resident population.
The lack of development and documentation of a facility-wide assessment had potential to affect the care and safety of all residents.
Findings:
During a review of a facility document titled Facility-Wide Self Assessment dated 7/12/21, the Facility-Wide Self Assessment indicated that the document was a template developed by the State of Missouri's [NAME] School of Nursing. The document had the State of Missouri's regulations were documented on it.
During an interview with Quality Officer (QS 1), on 2/15/22, at 9:30 AM, QS 1 acknowledged that the SNF (Skilled Nursing Facility) used a template downloaded from the internet. She said that she found the template in a binder placed in her office, and did not know where the template came from. She confirmed that the SNF designated Director of Facilities (DoF) and Minimum Data Set (MDS-assessment tool) Coordinator 2 responsibility to conduct and document a facility-wide assessment to determine resources the SNF needed to care for its resident population. She agreed that the facility wide-assessment was developed by the University of Missouri's [NAME] School of Nursing and had the University of Missouri's [NAME] School of Nursing insignia and the State of Missouri regulations documented on it. She confirmed that documentation on the template did not reflect the status of the SNF's required resources needed to take care of its residents' needs based on the acuity of its resident population. She said that she did not know what and how to explain the numbers and the information documented on the template. She confirmed that DoF and MDS Coordinator 2 were the only two people who participated in completing the information documented on the facility-wide assessment template and DoF was not available for interview because he resigned.
During an interview with MDS Coordinator 2 on 2/14/22, at 10:15 AM in the presence of QS 1, Executive Director of Continuum Care (EDCC), MDS Coordinator 2 stated that he completed the MDS portion of the template, and did not know who completed the rest of the facility wide-assessment template. He stated, DoF probably completed most portions of the template.
During concurrent interview QS 1 on 2/14/22, 10:20 AM, in the presence Executive EDCC and MDS Coordinator 2, QS 1 stated. We did not understand what was needed in conducting a facility wide-assessment. She said, We did not have a facility wide-assessment. We have a new template and we will use the new template to conduct and document our facility- wide assessment. EDCC stated that, We now have an understanding of what a Facility-wide assessment is. It sounds like a plan of care.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to ensure all portions of the residents' call light s...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to ensure all portions of the residents' call light system was functioning to communicate resident calls from all residents' rooms and all bathrooms to the call system's computer placed at the nursing station.
This failure had a potential to delay all resident call communications between residents and staff, delaying staffs' response to residents' urgent needs, with the potential to expose all residents to adverse events (unexpected injury, harm, death or risk thereof), and compromising their health and safety.
Findings:
During an observation on 2/8/22, at 10:45 AM, in Resident 3's room, Resident 3's room contained three resident beds, bed A, B, and C. Resident 3 was observed sitting on her wheelchair between the footboard of bed B and the wall, facing the door. She attempted to push her wheelchair backwards to move back to her bed, bed C to use the call light to call for assistance.
During an interview with Resident 3, on 2/8/22, at 10:47 AM, Resident 3 stated that she had been stuck between the footboard of bed B and the wall for a long time after pressing the call light to call facility staff to help her to get out of the room. She said she was not able to move her wheelchair back to her bed, bed C or move the wheelchair forward to get out of the room. She stated that she wanted to get out of the room, and needed help in moving her wheelchair pass bed B.
During observation on 2/8/22, at 10:56 AM, in resident 3's room, LVN 6 tried to push Resident 3's wheelchair backwards to release Resident 3's wheelchair stuck between the wall and the footboard of bed B. LVN 6 was unable to release the wheelchair. LVN 6 moved bed B towards the wall by pushing the footboard of the bed towards the headboard wall, and released Resident 3's wheelchair. He pressed Resident 3's call light, and the call light did not trigger the audio portion of the call light system. No sound signal was heard coming out of Resident 3's room after LVN 6 pressed Resident 3's call light.
During concurrent interview with LVN 6, on 2/8/22, at 11:04 AM, LVN 6 acknowledged that Resident 3's wheelchair was stuck between the wall and the footboard of bed B, while Resident 3 was sitting on the wheelchair. He confirmed that Resident 3 was unable to move her wheelchair to pass bed B to get out of the room. He agreed that Resident 3's call light did not trigger the audio portion of the call light system. He said no sound signal was heard coming out of Resident 3's room after LVN 6 pressed Resident 3's call light. He stated, The call did not relay a message to the computer located at the nursing station because the computer was switched off.
During an observation on 2/8/22, at 11:10 AM, Charge Nurse (CN) 1, prepared to check the call light system in each room located in Hallway 3. Each room in Hallway 3, room [ROOM NUMBER], 302, 303, 304, 305, 306, 307, 308, 309, 310 and 311 contained three resident beds, bed A, B, and C.
The facility used an electronic call light system, Composer Communication System, manufactured by Hill-Rom Company. The Composer Communication system had five components, the Master Station computer, resident room call light station, the emergency bathroom call light, the resident bed call light, and the hallway call light. The Master Station computer was placed at the nurse's station. The resident room call light station, an electronic device, 3 x 4 inches in size, was mounted on a wall in each room, at eye level to the right upon entering each room. The emergency call light was placed in each room bathroom. The resident bed call light for each bed, bed A, B, and C, was placed next to the headboard of each bed. The hallway call light was mounted on top of each door, outside each room along the hallway.
CN 1 tested emergency call lights in each resident bathroom, and call lights for bed A, B, C in rooms 301, 302, 304, 306, 308, 310, and 311. The emergency call did not trigger the audio portion of the call light system. No sound signal was heard coming out of each bathrooms when CN 1 pressed each bathroom call light. Each bathroom call light did relay a message to the Master Station computer placed at the nursing station. Each resident bed call light, bed A, B, and C in rooms 301, 302, 304, 306, 308, 310, and 311 did not trigger the audio portion of the call light system when CN 1 pressed call light. No sound signal was heard coming out of the room when CN 1 pressed each resident bed call light.
Each resident bed call light did not relay a message to the Master Station computer placed at the nurses' station. The screen of the Master Station computer placed at the nurses' station was dark, and the computer was switched off.
During interview with CN 1 on 2/8/22, at 11:20 AM, CN 1 acknowledged that the audio portions of the call light system did not function when she pressed the call lights for bed A, B, and C in rooms 301, 302, 304, 306, 308, 310, and 311 and the emergency call lights in the bathrooms. She confirmed that the call lights for bed A, B, and C, in rooms 301, 302, 304, 306, 308, 310, and 311and residents' bathrooms did not relay messages to the computer placed at the nurses' station because the computer was switched off. She said that the computer at the nurses' station was switched off because the computer was not functioning.
During observation on 2/8/22, at 11:30 AM, Resident 129 was sitting on his wheelchair and his call light was not accessible to him. His call light hang high on top of the headboard, on the left side of the bed.
During an interview with Resident 129, on 2/8/22, at 11:35 a. m., Resisent 129 requested his roommate observed sitting on bed B to reach his call light for him, and stated that he was not able to reach the call light. He said that staff placed the call light too high for him to reach the call light. He stated that staff took 15 minutes to 30 minutes to respond to residents' call for assistance. He said, The time dependent on how busy nurses are.
During an interview on EMS on 2/8/22, at 12:30 p. m., in the company of Executive Director of Continuum Care (EDDC), EMS acknowledged that the audio portion of the call light system, and the Master Station computer placed at the nurses' station was not functional.
He confirmed that the computerized call light system's audio and the Master Station computer placed at the nurses' station has not been functioning for more than a month. He stated that the manufacturer, Hill-Rom, stated that the electronic computerized call light system was not repairable. He said, The Hill-Rom computerized call light system's audio was not functional in all the rooms.
During concurrent interview with EDDC on 2/8/22, at 12:35 p, m., EDDC acknowledged that the audio portions of the call light system and the Master Station computer placed at the nurses' station was not functional in all resident rooms.
During a review of the SNF document titled Work-order Status. SMCC Open Work Order List undated, the Work Order Status. SMCC Open Work Order List indicated that during physical plant rounds the SNF documented that (1), on 9/30/21, at 08:46 a. m., Hill-Rom computer not functioning, (2), on 10/14/21, at 12:33 p. m., Nurse call down. Ringing sound at the nurses' station call light. I turned it off, (3), on 10/29/21, at 9:53 a. m., Hill-Rom computer down, (4), on 12/13/21, at 2:09 p. m., . Nurse call down (5), on 12/20/21, at 11:11 a. m., Hill-Rom computer. They are down. Bad computer (6), on 12/23/21, at 12:51 p. m., Call light monitor is not working. Please check, on (6), on 12/28/21, at . Call light in room [ROOM NUMBER]B . turn off, (7) on 12/28/21, at 9:57 a. m., All call lights not working, and (8), on 1/18/21, at 10:44 a. m., Hill-Rom computer down.
During the recertification survey conducted on 2/8/22, at 12:25 p. m., four months and eight days after the SNF initiated the first worker order to repair the call light system on 9/30/21, not all portions of the call light system were functional. The audio portions of the call light system and the Master Station computer placed at the nurses' station were not functional in all resident rooms.
During a review of the Association for Advancement of Medical Instrumentation (AAMI - an organization for advancing the development, safe, and effective use of medical technology) document titled Clinical Alarm Effectiveness: Recognizing and Mitigating Risks to Patient Care, dated June 2013, the document indicated that the AAMI included nurse call systems and bed alarms in list of devices with alarms. The document indicated that factors contributing to alarm-related sentinel events (patient safety event that results in death, permanent harm, or severe temporary harm) included absent or inadequate alarm systems, alarm systems not audible, alarm systems inappropriately turned off, inadequate staff training on proper use of equipment, inadequate staffing, and equipment failures and malfunction.