OCEAN VIEW POST ACUTE




Inspected within the last 6 months. Data reflects current conditions.
Ocean View Post Acute in Escondido, California, has a Trust Grade of B+, indicating it is above average and recommended for consideration. It ranks #151 out of 1,155 facilities in California, placing it in the top half, and #20 out of 81 in San Diego County, meaning only 19 local facilities are better. However, the facility is currently facing a worsening trend, with issues increasing from 5 in 2024 to 14 in 2025. Staffing is a moderate strength, rated 3 out of 5 stars, with a turnover rate of 39%, which is close to the state average. Notably, the facility has not incurred any fines, which is a positive sign. On the downside, the facility has several concerning incidents, such as failing to follow proper infection control procedures for residents requiring enhanced barrier precautions, potentially leading to cross-contamination and health risks. Additionally, there were failures to provide necessary documentation to residents being discharged, which could hinder their access to advocacy. While the facility offers good RN coverage, which is better than 76% of California facilities, the increase in deficiencies suggests families should weigh these concerns carefully against the positives.
- Trust Score
- B+
- In California
- #151/1155
- Safety Record
- Low Risk
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 39% turnover. Near California's 48% average. Typical for the industry.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most California facilities.
- Skilled Nurses ○ Average
- Each resident gets 40 minutes of Registered Nurse (RN) attention daily — about average for California. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 41 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (39%)
9 points below California average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Near California avg (46%)
Typical for the industry
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 41 deficiencies on record
Jun 2025
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record review, the facility failed to implement a care plan (detailed plan with informatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow nursing standards of practice when:
1) A Licen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure two persons assist when safely transferring a r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure oxygen was administered per physician's order f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure dialysis (a process to remove waste from the b...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure monitoring of medication management was conduct...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the medication error rate was less than five pe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure menus and recipes were followed for pureed foods.
This failure negatively affected the nutritional value of foods prepa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure kitchen staff utilized recipes when preparing foods.
This failure had the potential to place residents at risk for poor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide alternate menu options of similar nutritional value to residents.
This failure had the potential to result in meals no...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to dispose of an expired food product in a nursing unit refrigerator.
This failure had the potential to place residents at risk f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the flu vaccine (a vaccine which provides immunity to a vari...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interview, and record review the facility failed to ensure infection control procedures were followed whe...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0573
(Tag F0573)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to respond to a medical records request for one of two sampled patient...
Read full inspector narrative →
Sept 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to prevent a hazardous situation when supervision was not provided for...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to appropriately discharge on e of one resident (Resident 3) with elop...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide a plan of care and adequate supervision to pre...
Read full inspector narrative →
Feb 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify the responsible party when sodium valproate (a medication th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to apply a skin protective cream as ordered for one of two sampled res...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure current infection control practices were follo...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to:
1. Perform and document neurological checks (assessing mental stat...
Read full inspector narrative →
Mar 2023
2 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to label the oxygen (O2) tubing and humidification water ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a medication error rate of less than 5%. The facility's medication error rate was 8%. Two medication errors were observ...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of three residents (Resident 1) received pressure ulcer ...
Read full inspector narrative →
Aug 2019
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to maintain a tile floor in good repair when tiles were chipped and missing, in 1 of 2 shower rooms.
As a result, there was a po...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to code the MDS correctly, for one of 19 sampled residents (81).
As a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to consistently provide a method of communication, in a r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility did not provide person-centered, in-room activities that met the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure appropriate urinary catheter (a tube placed in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a CNA acted within their scope of practice whe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to comprehensively assess the needs of one of three resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 7 was admitted to the facility on [DATE], with diagnoses including cognitive communication deficit (difficulty commu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility failed to ensure appropriate urinary catheter (a tube placed in the bladder to drain urine) care was provided to on...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to send a copy of the Notice of Transfer or Discharge form to the Ombu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide a written notice of bed- hold, upon transfer to the GACH, f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident 62 was admitted to the facility on [DATE], with diagnoses which included heart failure per the facility's admission ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to revise care plans that reflected resident preferences ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to:
1. Label and date glasses of liquids, soup bowls of liquids, remove a watermelon with fuzzy brown spots, and cover cut celer...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected multiple residents
Based on oberservation, interview, and record review, the facility failed to label and date resident food stored in one of two nursing station refrigerators.
As a result, there was a potential for fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure resident medical records were stored in a secured location.
This failure had the potential for residents' private medi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to implement an Antibiotic Stewardship Program (a system to monitor antibiotic use).
This failure had the potential to increase the risk of ad...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Grade B+ (80/100). Above average facility, better than most options in California.
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most California facilities.
- • 39% turnover. Below California's 48% average. Good staff retention means consistent care.
- • 41 deficiencies on record. Higher than average. Multiple issues found across inspections.
About This Facility
What is Ocean View Post Acute's CMS Rating?
CMS assigns OCEAN VIEW POST ACUTE an overall rating of 5 out of 5 stars, which is considered much above average nationally. Within California, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Ocean View Post Acute Staffed?
CMS rates OCEAN VIEW POST ACUTE's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 39%, compared to the California average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Ocean View Post Acute?
State health inspectors documented 41 deficiencies at OCEAN VIEW POST ACUTE during 2019 to 2025. These included: 41 with potential for harm.
Who Owns and Operates Ocean View Post Acute?
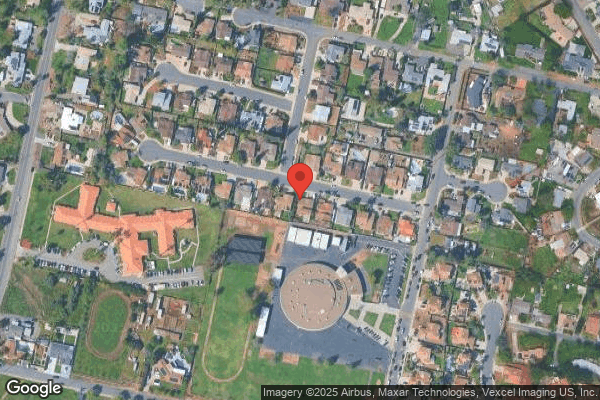
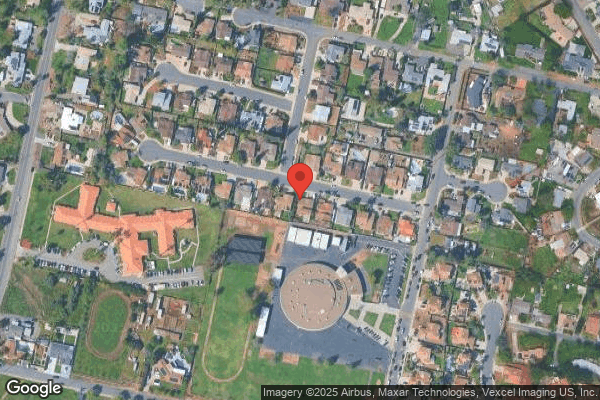
OCEAN VIEW POST ACUTE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by DAVID & FRANK JOHNSON, a chain that manages multiple nursing homes. With 120 certified beds and approximately 105 residents (about 88% occupancy), it is a mid-sized facility located in ESCONDIDO, California.
How Does Ocean View Post Acute Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, OCEAN VIEW POST ACUTE's overall rating (5 stars) is above the state average of 3.2, staff turnover (39%) is near the state average of 46%, and health inspection rating (4 stars) is above the national benchmark.
What Should Families Ask When Visiting Ocean View Post Acute?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Ocean View Post Acute Safe?
Based on CMS inspection data, OCEAN VIEW POST ACUTE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 5-star overall rating and ranks #1 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Ocean View Post Acute Stick Around?
OCEAN VIEW POST ACUTE has a staff turnover rate of 39%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Ocean View Post Acute Ever Fined?
OCEAN VIEW POST ACUTE has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Ocean View Post Acute on Any Federal Watch List?
OCEAN VIEW POST ACUTE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.