LAKEPORT POST ACUTE




Inspected within the last 6 months. Data reflects current conditions.
Lakeport Post Acute has a Trust Grade of C+, indicating that it is slightly above average but not exceptional. It ranks #382 out of 1,155 facilities in California, placing it in the top half, and is the #1 facility out of 3 in Lake County, meaning it is the best local option. This facility is improving, with a decrease in issues from 24 in 2023 to 10 in 2025, but it still has some concerns. Staffing is rated below average at 2 out of 5 stars, with a turnover rate of 35%, which is better than the state average. However, there is less nursing coverage than 75% of California facilities, which raises concerns about the quality of care. While there have been no fines, which is a positive aspect, recent inspections revealed some significant issues. For example, the facility did not provide enough nursing staff on multiple days, which could delay timely care for residents. Additionally, there were concerns about the visibility of important information for residents, potentially impacting their ability to report issues or seek help. Overall, while there are strengths such as good quality measures and no fines, families should weigh these against the staffing challenges and recent incidents of concern.
- Trust Score
- C+
- In California
- #382/1155
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- 35% turnover. Near California's 48% average. Typical for the industry.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most California facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 16 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 53 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (35%)
13 points below California average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
10pts below California avg (46%)
Typical for the industry
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 53 deficiencies on record
Jun 2025
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to assess one of 18 sampled residents (Resident 12) for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement a comprehensive person centered care plan for one of 18 sampled residents (Residents 222) when Resident 222's care ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, the facility failed to ensure quality of care when physician orders to monitor fasting blood sugar levels of Resident 35, who is on insulin medica...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility had a medication error rate of 10 percent when three identified...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the kitchen food preparation and storage areas were maintained in a safe and sanitary manner when two fans blowing air...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain an effective infection prevention and control program when powder like substance was observed on the surface areas a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to provide pain management services consistent with professional standards of practice for two of 18 sampled residents (Resident ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During a concurrent observation and interview on 6/19/25 at 1:40 PM, with Licensed Vocational Nurse (LVN) 1 at the medication...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record reviews, the facility failed to provide nursing staff based on the 3.5 direct hours...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility nursing staff failed to give acetaminophen (generic for Tylenol, a medication...
Read full inspector narrative →
Dec 2023
19 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0551
(Tag F0551)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to ensure that a resident's, Resident 230's, responsible party, act on behalf of Resident 230 in order to support her in decision-making reg...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0573
(Tag F0573)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to ensure that one resident, Resident 71, was provided her medical records within the accepted timeframes after she made an oral request to t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to coordinate the Medical Doctor's (MD) appointment for Level II Pread...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to ensure staff were aware of the Basic Care Plan (BCP, a plan that ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to ensure residents receive treatment and care in accordance with pr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to help schedule an appointment for evaluation of a heari...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** (2) Resident 52
Resident 52 was initially admitted to the facility on [DATE] with mental conditions of agoraphobia (is afraid to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observation, interviews and record reviews, the facility failed to ensure the development of a plant-based menu. This failure had the potential for vegetarian residents to not meet the recomm...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
Based on observation, interviews and record reviews, the facility failed to ensure the kitchen walls were in good repair when holes on the walls were noted. This failure could result in rodents and pe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure five sampled residents (Resident 1, Resident 14, Resident 35...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on observation, interviews and record reviews, the facility failed to ensure 1. they were adequately staffed for 21 out of 31 days for CNAs and nine out of 31 days for licensed nurses in 10/2023...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility did not ensure training materials, resources, and policies and procedures explained all allegations of abuse must be reported in two hours.
This fai...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0574
(Tag F0574)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to ensure that the list of information such as the name and the correct Department of the State Survey Agency, & the State Licens...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
Based on observations, interviews and record reviews, the facility failed to ensure the food was palatable, was served timely and was served at temperatures in accordance with resident preferences for...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interviews, the facility failed to ensure 1. residents' food items were labeled with name and dated and...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0837
(Tag F0837)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the Governing Body (a group of people that has the authority to exercise governance over an organization) failed to ensure to designate or appoint a ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to ensure the Quality Assurance Committee (QAA) is composed of the required committee members, such as an active licensed Nursing...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observations, interviews and record reviews, the facility failed to 1. ensure staff were offering and performing hand hygiene (HH, a way of cleaning one's hands that substantially reduces pot...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to treat 4 of 6 residents (Resident 1, Resident 2, Reside...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the residents were free from accidents for one ...
Read full inspector narrative →
May 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0551
(Tag F0551)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of four sampled residents ' (Resident 1) rights were uph...
Read full inspector narrative →
Apr 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to develop and implement a care plan to manage and respon...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide annual dementia management training to two of three sampled nurse aides.
This failure decreased the facility ' s potential to ensur...
Read full inspector narrative →
Nov 2022
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to follow and implement their facility standard and trans...
Read full inspector narrative →
Jun 2022
18 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0553
(Tag F0553)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide 1 of 6 sampled residents (Resident 179), the opportunity to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to notify the Ombudsman for one discharged resident to the Community, Resident 80. This failure had the potential to result in unsafe discharg...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow the recommendations by the State of California when they did...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record reviews, the facility failed to provide care in accordance with professional standards of practice to one out of three sampled residents, Resident # 66, wh...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop and implement an effective discharge planning process plan for one sampled Resident (Resident 80) when Resident 80 was discharged h...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure one of six sampled residents (Resident 178) rec...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0710
(Tag F0710)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 48
Based on interview and record review, the facility failed to ensure resident's medical supervision such as weight lo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to follow its policy and procedure in ordering and re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to monitor 1 of 6 sampled residents (Resident 32) for episodes of anxi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure grievance forms and complaints information were visually accessible and attainable by residents in the Facility without retaliation ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 48
Record review indicated Resident 48 had a diagnoses of Parkinson's disease, Dementia without behavioral disturbance,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 48
Record review indicated Resident 48 had a diagnoses of Parkinson's disease, Dementia without behavioral disturbance,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to:
1. Adequately supervise one of four sampled resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During an interview on 6/23/2022 at 2:33 p.m. Administrator stated he tried to ask for more staff to help but had no success.
Ba...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to offer a palatable meal to the residents of the facility on regular and pureed consistencies. This had the potential to cause a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to store and prepare meals in a sanitary manner, when:
1. Expired dairy was found in one of the facility's refrigerators,
2. Flie...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure documentation for 2 of 6 sampled residents (Res...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During an observation on 6/20/2022 at 3 p.m., in Hallway 400, most resident's door had yellow signage indicating staff must wear...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most California facilities.
- • 35% turnover. Below California's 48% average. Good staff retention means consistent care.
- • 53 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
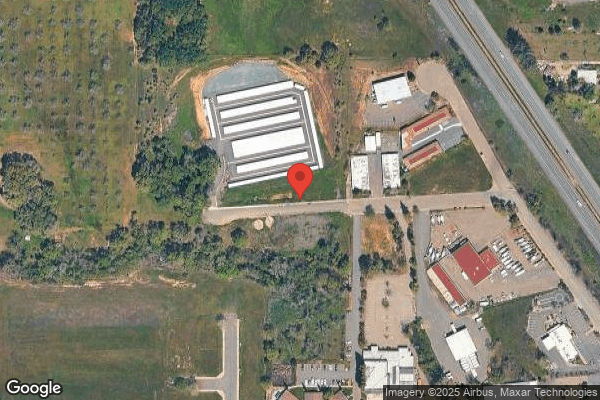
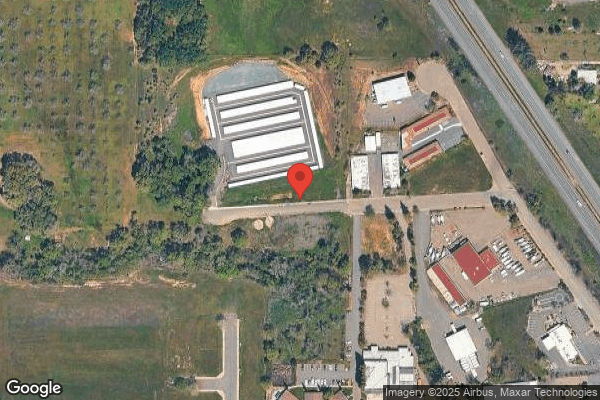
About This Facility
What is Lakeport Post Acute's CMS Rating?
CMS assigns LAKEPORT POST ACUTE an overall rating of 4 out of 5 stars, which is considered above average nationally. Within California, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Lakeport Post Acute Staffed?
CMS rates LAKEPORT POST ACUTE's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 35%, compared to the California average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Lakeport Post Acute?
State health inspectors documented 53 deficiencies at LAKEPORT POST ACUTE during 2022 to 2025. These included: 1 that caused actual resident harm and 52 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Lakeport Post Acute?
LAKEPORT POST ACUTE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PACS GROUP, a chain that manages multiple nursing homes. With 81 certified beds and approximately 73 residents (about 90% occupancy), it is a smaller facility located in LAKEPORT, California.
How Does Lakeport Post Acute Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, LAKEPORT POST ACUTE's overall rating (4 stars) is above the state average of 3.2, staff turnover (35%) is significantly lower than the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Lakeport Post Acute?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Lakeport Post Acute Safe?
Based on CMS inspection data, LAKEPORT POST ACUTE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 4-star overall rating and ranks #1 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Lakeport Post Acute Stick Around?
LAKEPORT POST ACUTE has a staff turnover rate of 35%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Lakeport Post Acute Ever Fined?
LAKEPORT POST ACUTE has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Lakeport Post Acute on Any Federal Watch List?
LAKEPORT POST ACUTE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.