ALHAMBRA POST ACUTE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Alhambra Post Acute has a Trust Grade of C+, indicating it is decent and slightly above average among nursing homes. It ranks #521 out of 1155 facilities in California, placing it in the top half, but #23 out of 30 in Contra Costa County suggests there are better local options available. The facility is improving overall, having reduced issues from 21 in 2023 to 13 in 2024. Staffing is rated 3 out of 5 stars, with a concerning turnover rate of 53%, significantly higher than the state average of 38%. While there have been no fines reported, which is a positive indicator, there were several incidents noted during inspections, such as failing to properly label and store medications, not allowing residents to heat personal food items, and not following proper infection control practices, which could lead to safety concerns.
- Trust Score
- C+
- In California
- #521/1155
- Safety Record
- Low Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 53% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most California facilities.
- Skilled Nurses ✓ Good
- Each resident gets 68 minutes of Registered Nurse (RN) attention daily — more than 97% of California nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 51 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near California average (3.1)
Meets federal standards, typical of most facilities
Near California avg (46%)
Higher turnover may affect care consistency
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 51 deficiencies on record
Nov 2024
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete the Level I Preadmission Screening and Resident Review (PA...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure adequate supervision was provided to prevent falls and implement resident-centered care interventions for one (Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, for one of two sampled residents (Resident 31), the facility failed to develo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to label medications and properly dispose of a medication...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to maintain an effective infection control program when t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to act promptly upon the grievances and recommendations from the residents' group meetings concerning residents care and life in the facility....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Findings:
4. During a review of Resident 145's admission record, the admission record indicated the resident was admitted on [DA...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interviews and record review, the facility failed to ensure storage of food under sanitary conditions when the following food items in the refrigerator were not dated and labeled...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure garbage and refuse storage area was maintained in a sanitary condition when the dumpster was overflowed with bags of tr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0920
(Tag F0920)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to provide a dining/activity room with adequate space for 42 residents.
This failure resulted in limiting the independent functioning and task ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0912
(Tag F0912)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility had sixteen resident rooms (Rooms 1, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 14, 15, 1...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a follow up call and /or assessment was done to verify durab...
Read full inspector narrative →
Apr 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide bathing assistance for one of two sampled residents (Resident 1) for two extended intervals: a five-day interval from ...
Read full inspector narrative →
Dec 2023
20 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to perform a medication self-administration assessment p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure that missing property for one of one sampled resident (Resident 24) was accounted for and addressed.
This failure placed Resident 2...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to conduct a comprehensive Minimum Data Set assessment (MDS, an assess...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, the facility failed to follow federal requirements to submit Quarterly Minimum Data Set (MDS,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2.During a review of Resident 6's admission Record printed on 11/28/23, the record indicated Resident 6 was admitted to the faci...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to develop and implement a person-centered care plan for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to review and revise one of one sampled resident (Reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide a shower for two of two sampled Residents (Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure residents were served palatable food when,
1. The lunch for Resident 17 was not fortified as ordered by the physician...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure privacy and right to send secure mail when a stack of residents' mail was left unattended on top of an unlocked mail box located outsi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. During a record review of the admission Record dated 11/29/2023, the record indicated Resident 38 was admitted to the facilit...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to make information on how to file a grievance or complaint available to six (3, 19, 22, 24, 26 and 38) of seven sampled residents...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow safe pharmacy services when the following were noted:
1. Facility did not have morning medications readily available f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2.
During a record review of the admission Record dated 11/29/2023, the record indicated Resident 38 was admitted to the facili...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure three of six sampled residents for medication administration observation (Residents 200, 11, and 5) received medicatio...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement the pneumococcal immunization (a vaccine to protect again...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to store medications appropriately when the following were noted:
1. Resident 5's Lotemax eye drops bottle was not labeled with ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected most or all residents
2. During a concurrent observation and interview on 11/27/23 at 09:41 a.m., with Resident 298, Resident 298 stated the facility did not warm the lobster brought from home on her birthday 11/22/23. Res...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow infection prevention and control practices whe...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0912
(Tag F0912)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility had sixteen residents (Rt) rooms (room [ROOM NUMBER], 3, 4, 5, 6, 7, 8, 9, 10, ...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0573
(Tag F0573)
Could have caused harm · This affected 1 resident
Based on interview and record review, for one of one sampled resident (Resident 1), the facility failed to allow Resident 1's Representative (RR) to obtain a copy of the medical records within the req...
Read full inspector narrative →
Mar 2022
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to immediately notify one (Resident 39) sampled residents' physician and representative or family member of the significant weight loss of sev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to conduct an annual comprehensive Minimum Data Set assessment (MDS, an assessment tool used to direct resident care) for one sampled resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one (Resident 39) sampled resident's Pre-admission Screening Resident Review (PASRR) was referred to the appropriate state mental au...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to provide one (Resident 26) sampled resident restorative nursing care (RNA) for Resident 26's contracture (shortening of the musc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of two sampled residents (Resident 191) received supplemental oxygen according to the physician's order.
This fail...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure proper labeling of medications for two of six sampled residents (Residents 18 and 23) when nasal spray and inhaler (med...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to educate and offer COVID-19 (a new coronavirus that causes a respira...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, for five of six residents (Resident 3, 4, 5, 6, and 7) that were reviewed for resident ass...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on interviews and record review, the facility failed to develop and implement comprehensive care plans for five sampled residents (Resident 6, 12, 32, 34 and 39) when;
1 The care plan was not d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on interviews and record review, the facility failed to ensure that one Certified Nursing Assistant (CNA 3) had the skilled competency evaluation completed, and for three CNAs (CNA 4. 5 and 6 ) ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
Based on interviews and record review, the facility failed to ensure three sampled residents (Resident 6, 32, 34 and 39) with diagnosed Alzheimer's Dementia (an irreversible, progressive brain disorde...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interviews and record review, the facility failed to follow proper sanitation and food storage practices and ensure staff maintained competencies for kitchen service as follows.
...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to implement their infection prevention and control progr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure three of five sampled Residents (Residents 37, 90 and 191) w...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure the designated Infection Preventionist (infection control nurse) completed the specialized training in infection prevention and cont...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0888
(Tag F0888)
Minor procedural issue · This affected most or all residents
Based on interview and record review, the facility failed to develop and implement a comprehensive staff COVID-19 (a new coronavirus causing a respiratory infection that is easily spread) vaccination ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0912
(Tag F0912)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide the required 80 square feet (sq ft) of living...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most California facilities.
- • 51 deficiencies on record. Higher than average. Multiple issues found across inspections.
About This Facility
What is Alhambra Post Acute's CMS Rating?
CMS assigns ALHAMBRA POST ACUTE an overall rating of 3 out of 5 stars, which is considered average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Alhambra Post Acute Staffed?
CMS rates ALHAMBRA POST ACUTE's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 53%, compared to the California average of 46%.
What Have Inspectors Found at Alhambra Post Acute?
State health inspectors documented 51 deficiencies at ALHAMBRA POST ACUTE during 2022 to 2024. These included: 47 with potential for harm and 4 minor or isolated issues. While no single deficiency reached the most serious levels, the total volume warrants attention from prospective families.
Who Owns and Operates Alhambra Post Acute?
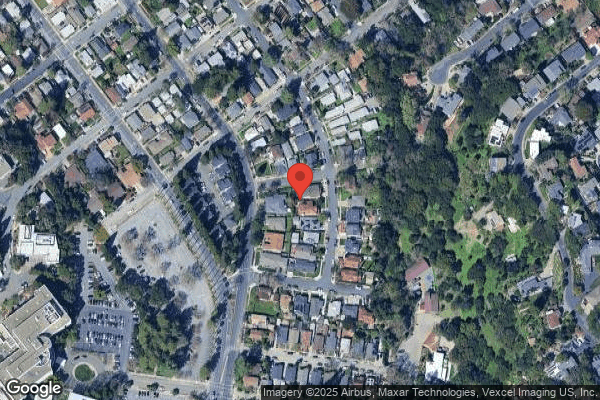
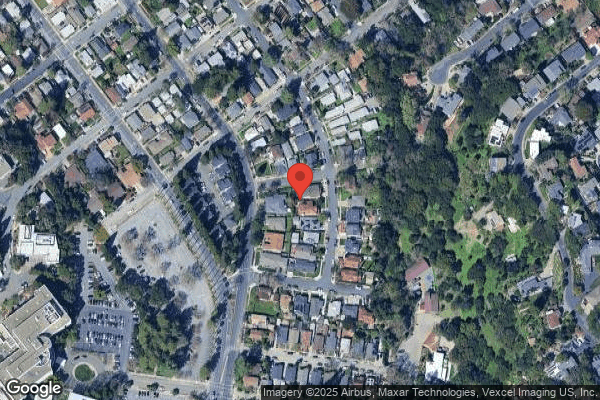
ALHAMBRA POST ACUTE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PACS GROUP, a chain that manages multiple nursing homes. With 44 certified beds and approximately 38 residents (about 86% occupancy), it is a smaller facility located in MARTINEZ, California.
How Does Alhambra Post Acute Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, ALHAMBRA POST ACUTE's overall rating (3 stars) is below the state average of 3.1, staff turnover (53%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Alhambra Post Acute?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Alhambra Post Acute Safe?
Based on CMS inspection data, ALHAMBRA POST ACUTE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Alhambra Post Acute Stick Around?
ALHAMBRA POST ACUTE has a staff turnover rate of 53%, which is 7 percentage points above the California average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Alhambra Post Acute Ever Fined?
ALHAMBRA POST ACUTE has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Alhambra Post Acute on Any Federal Watch List?
ALHAMBRA POST ACUTE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.