DIAMOND RIDGE HEALTHCARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Diamond Ridge Healthcare Center in Pittsburg, California has a Trust Grade of D, indicating below-average performance with some concerns. It ranks #569 out of 1155 facilities in California, placing it in the top half, but is #24 out of 30 in Contra Costa County, meaning there are only a few local options that are better. The facility's trend is stable, with 10 issues reported consistently in both 2023 and 2024. Staffing is a strength, rated at 4 out of 5 stars with a 29% turnover rate, which is below the state average, suggesting that staff are familiar with the residents. However, the facility has accumulated $42,033 in fines, which is concerning as it is higher than 76% of California facilities, pointing to ongoing compliance issues. There are notable weaknesses, including a critical finding where the cooling system failed, leading to unsafe temperatures for several residents, which posed serious health risks. Additionally, food safety practices have been called into question with incidents of improperly stored and outdated food items, creating potential exposure to foodborne illnesses. Furthermore, a resident's care plan was not developed within the required 48 hours of admission, which is a procedural oversight that could affect their care. Overall, while there are some strengths in staffing, the facility faces significant challenges that families should consider carefully.
- Trust Score
- D
- In California
- #569/1155
- Safety Record
- High Risk
- Inspections
- Holding Steady
- Staff Stability ✓ Good
- 29% annual turnover. Excellent stability, 19 points below California's 48% average. Staff who stay learn residents' needs.
- Penalties ○ Average
- $42,033 in fines. Higher than 68% of California facilities. Some compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 31 minutes of Registered Nurse (RN) attention daily — about average for California. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 50 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Low Staff Turnover (29%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (29%)
19 points below California average of 48%
Facility shows strength in staffing levels, quality measures, staff retention, fire safety.
The Bad
Near California average (3.1)
Meets federal standards, typical of most facilities
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 50 deficiencies on record
Aug 2024
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of three closed resident records sampled (Resident 112) ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop new interventions to address behavioral care and treatment for one of 32 sampled residents (Resident 264) with dementia (a disorder...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure one of one sampled resident (Resident 364) received Cromolyn Sodium Ophthalmic Solution (a prescription eye drop medica...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of five sampled residents (Resident 52) was free from unnecessary medication, when Resident 52 was prescribed and ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure safe medication storage and labeling practices with census of 110, when:
1. Resident 5's inhalation medication with li...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During a review of Resident 363's AR, dated 8/14/24, the AR indicated Resident 363 had a diagnosis of right femur fracture (brok...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure four of four sampled residents (Residents 28, 21, 63 and 84) received necessary care to maintain good grooming and per...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
3. During a concurrent observation and interview on 8/13/24, at 11:10 a.m. LVN 3, a glucometer stored inside the medication cart # 2B had dark red stains on the insertion port, on the side, and back o...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to store and prepare foods in a sanitary manner that prevented foodborne illness for the facility when:
1. Eleven unlabeled and u...
Read full inspector narrative →
Apr 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to protect one of three sampled residents (Resident 1) f...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, for one of three sampled residents (Resident 1), the facility failed to noti...
Read full inspector narrative →
Oct 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, for one of two sampled residents (Resident 1), the facility failed to ensure...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, for one of two sampled residents (Resident 2), the facility failed to ensure Resident 2 wa...
Read full inspector narrative →
Aug 2023
2 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Safe Environment
(Tag F0584)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to maintain the facility cooling system to provide eight ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to maintain a safely operating toilet for two of 12 sampled residents (Resident 9 and 10).
This failure resulted in toilet water ...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0675
(Tag F0675)
Could have caused harm · This affected 1 resident
Based on interview and record review, for one of three sampled residents (Resident 1), the facility failed to provide care and services to attain and maintain highest practicable physical and mental w...
Read full inspector narrative →
Apr 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to ensure the Minimum Data Set (MDS-Resident Assessment and Care Screening tool used to guide care), was accurate for one ( Resident 1) of th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to provide services to promote wound healing for one (Resident 1) of three sampled residents. The facility did not consistently provide wound...
Read full inspector narrative →
Apr 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure Resident 1 was free from abuse when Resident 1...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one (Resident 1) of three sampled residents received treatment and care services in accordance to professional standards of practice...
Read full inspector narrative →
Apr 2022
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure the Minimum Data Set (MDS-Resident Assessment and Care Scre...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to develop a comprehensive, person-centered care plan with measurable o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide podiatry services
(foot care including cutting of toenails) for one of two sampled residents (Resident 33).
This fai...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to obtain respiratory care orders or follow orders for t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the skilled nursing facility did not effectively manage the pain for one of 20 residents (Resident 155). Resident 155 did not receive pain medication...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to consistently supply a medication prescribed by a physician for one (Resident 9) of five sampled residents.
This failure resulted in Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to ensure two sampled residents (Resident 60 and 84) were free from unnecessary drugs as follows:
1. Resident 60 was administered buspirone (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to ensure the skills competency evaluations were completed for dietary staff. The dietary Aide (DA) and one [NAME] (CK) competency skills eva...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain one (Resident 59) sampled resident's wheelchair in good working condition when Resident 59's wheelchair was squeaky ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to have a baseline care plan for four of five sampled residents when R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on observation, interviews, and record review, the facility failed to maintain sufficient staffing to provide care for five of five sampled residents, Resident 13, Resident 38, Resident 58, Resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
Based on interview and record review , the facility failed to follow the policy and procedure for Medication Regimen Review to act upon the Consultant Pharmacist's (CP) report of medication irregulari...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to serve palatable food when meatballs were served for lunch that lacked flavor.
This deficient practice had the potential to decrease meal enjo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interviews and record review, the facility failed to follow proper sanitation and food storage practices when:
a. Kitchen floor tiles had brownish black residual discoloration,
...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow infection control practices during storage and...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0888
(Tag F0888)
Minor procedural issue · This affected most or all residents
Based on interview and record review, the facility failed to follow the policy and procedure (P&P) for staff requesting COVID-19 (a contagious respiratory infection mainly affecting the lungs) vaccine...
Read full inspector narrative →
Jul 2019
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement the Advance Directive (legal document with written instructions for the provision of health care) policy at the time of admission...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide fingernail care and nail hygiene for two (Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record review, the facility failed to ensure one (Resident 79) of 30 sampled residents received restorative care services (assists patient to gain strength and mo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide assistance and arrange services to restore the hearing aids for one (Resident 7) of 30 sampled residents to maintain hearing abilit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, for one (Resident 66) of 30 sampled residents, the facility failed to elevat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure controlled medications were reconciled (count verification) to prevent potential diversion or tampering when one of fi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow the policy for Medication Regimen Reviews (MRR) for one (Resident 46) of thirty sampled residents when the antidepress...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide an environment free from unnecessary drugs fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure drugs and biologicals were labeled, stored, an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide safe storage of laboratory test supplies when...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to provide residents with a nourishing, well balanced diet that meets their daily nutritional intake and special dietary need...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed follow the policy and procedure to store, clean floors, and keep equipment under sanitary conditions when:
- The Kitchen floor t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews for three (Residents 160, 93, and 161) of 30 sampled residents, the facility failed to ensure the clinical records contained accurate health statu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure the infection control program was implemented and to use the proper sanitary technique when:
1. Registered Nurse/Nursin...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 29% annual turnover. Excellent stability, 19 points below California's 48% average. Staff who stay learn residents' needs.
- • Multiple safety concerns identified: 1 life-threatening violation(s), $42,033 in fines. Review inspection reports carefully.
- • 50 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $42,033 in fines. Higher than 94% of California facilities, suggesting repeated compliance issues.
- • Grade D (46/100). Below average facility with significant concerns.
About This Facility
What is Diamond Ridge Healthcare Center's CMS Rating?
CMS assigns DIAMOND RIDGE HEALTHCARE CENTER an overall rating of 3 out of 5 stars, which is considered average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Diamond Ridge Healthcare Center Staffed?
CMS rates DIAMOND RIDGE HEALTHCARE CENTER's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 29%, compared to the California average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Diamond Ridge Healthcare Center?
State health inspectors documented 50 deficiencies at DIAMOND RIDGE HEALTHCARE CENTER during 2019 to 2024. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 48 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Diamond Ridge Healthcare Center?
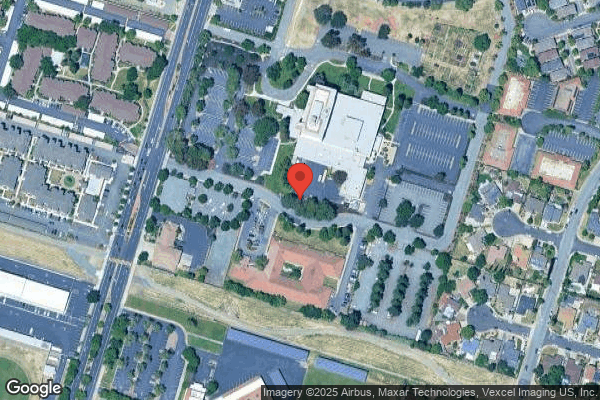
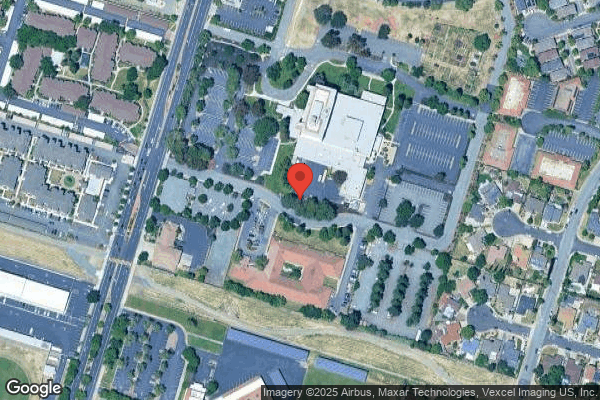
DIAMOND RIDGE HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by DAVID & FRANK JOHNSON, a chain that manages multiple nursing homes. With 120 certified beds and approximately 106 residents (about 88% occupancy), it is a mid-sized facility located in PITTSBURG, California.
How Does Diamond Ridge Healthcare Center Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, DIAMOND RIDGE HEALTHCARE CENTER's overall rating (3 stars) is below the state average of 3.1, staff turnover (29%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Diamond Ridge Healthcare Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Diamond Ridge Healthcare Center Safe?
Based on CMS inspection data, DIAMOND RIDGE HEALTHCARE CENTER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in California. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Diamond Ridge Healthcare Center Stick Around?
Staff at DIAMOND RIDGE HEALTHCARE CENTER tend to stick around. With a turnover rate of 29%, the facility is 17 percentage points below the California average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly.
Was Diamond Ridge Healthcare Center Ever Fined?
DIAMOND RIDGE HEALTHCARE CENTER has been fined $42,033 across 1 penalty action. The California average is $33,499. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Diamond Ridge Healthcare Center on Any Federal Watch List?
DIAMOND RIDGE HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.