RIDGECREST REGIONAL TRANSITIONAL CARE AND REHABILI
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Ridgecrest Regional Transitional Care and Rehabili has a Trust Grade of D, indicating below-average performance with some concerns. They rank #889 out of 1155 facilities in California, placing them in the bottom half, and #5 out of 17 in Kern County, meaning only a few local options are better. The facility is worsening, with issues increasing from 15 in 2024 to 17 in 2025. Staffing is average with a 3 out of 5 rating and a turnover rate of 42%, which is on par with the state average. However, they have concerning fines totaling $42,640, higher than 75% of California facilities, and less RN coverage than 76% of state facilities, which is a potential risk for residents. Specific incidents include a failure to protect a resident from abuse, where another resident with a history of inappropriate behavior was not adequately supervised, leading to an abusive situation. Additionally, there were issues with food safety protocols, such as raw eggs stored improperly above raw meat, which violates health standards and could lead to contamination. Lastly, essential kitchen equipment was not maintained safely, posing potential health hazards. Overall, while the staffing situation is somewhat stable, there are significant safety and care concerns that families should consider.
- Trust Score
- D
- In California
- #889/1155
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 42% turnover. Near California's 48% average. Typical for the industry.
- Penalties ⚠ Watch
- $42,640 in fines. Higher than 96% of California facilities. Major compliance failures.
- Skilled Nurses ⚠ Watch
- Each resident gets only 23 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 50 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (42%)
6 points below California average of 48%
Facility shows strength in fire safety.
The Bad
Below California average (3.1)
Below average - review inspection findings carefully
Near California avg (46%)
Typical for the industry
Above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 50 deficiencies on record
Mar 2025
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide a home-like environment for one of six sampled residents (Resident 72) when the bathroom had an odor. This failure ha...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow its Policy and Procedure, Care Plans [CP], Comprehensive Person-Centered, when care plans were not developed and implemented for two...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to ensure one of one sampled residents (Resident 31) diet order was clarified per Resident 31's preference for lacto-vegetarian (which includ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure two of two sampled residents (Resident 32 and ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to monitor the effectiveness of pain medications for two of two sampled residents (Resident 35 and Resident 55). This failure had the potentia...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure insulin (a medication to control blood sugar levels) vials were labeled with the resident's name for one of one sample...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure:
1. The planned menu for a therapeutic renal diet (for kidney disease) was followed for one of one sampled resident (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the Infection Preventionist (IP) failed to demonstrate competency to carry o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to enusre call lights were withing reach for four of 36 sampled residents (Resident 47, Resident 61, Resident 16, Resident 15). ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure three of seven sampled residents (Resident 14,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed follow their Policy and Procedure (P&P) titled, Staffing, Sufficient and Competent Nursing, for all residents (73) when direct care service hou...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility's Quality Assurance and Performance Improvement (QAPI) committee failed to identify, develop, and implement infection prevention and co...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. During a concurrent observation and interview on 3/5/25 at 11:20 a.m. with LVN 1, LVN 1 checked the blood sugar level of Resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0945
(Tag F0945)
Could have caused harm · This affected multiple residents
Based on interview, and record review, the facility failed to follow its Policy and Procedure titled, Employee Training on Infection Control, for 11 of 25 sampled Licensed Vocational Nurses (LVN) (LVN...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
2. During a concurrent observation and interview on 03/04/25 at 8:53 a.m. with Dietary Manager (DM) in a walk-in refrigerator, a crate of raw pasteurized shell eggs located on a food storage tray on a...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure essential equipment was maintained in safe operating condition when:
1. A food preparation sink located in the kitchen...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide pharmaceutical services to meet the needs of one of four re...
Read full inspector narrative →
Dec 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow its policy and procedure (P&P) on recording and investigating grievances or complaints for one of three sampled residents (Resident ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow its policy and procedure (P&P) on administering medications for one of three sampled residents (Resident 1) when Resident 1's two in...
Read full inspector narrative →
Oct 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide reasonable accommodations for two of three sampled resident (Resident 1 and Resident 2). This failure had the potential for delay i...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based interview and record review, the facility failed to ensure medication were administered as ordered for one of three sampled residents (Resident 1). This failure had the potential for Resident 1 ...
Read full inspector narrative →
May 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of three sampled residents (Resident 1), mail was delivered unopened. This failure resulted in violation of Resident 1's residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of three sampled residents (Resident 1) grievances were resolved. This failure had the potential for negative psychosocial outco...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure adequate supplies were available for two of three sampled residents (Resident 1 and Resident 2). This failure had the potential for ...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure care plan was implemented for one of three sampled residents (Resident 1) when the behaviors were not monitored hourly. This failure...
Read full inspector narrative →
Apr 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to monitor efficacy of the bed alarm to ensure it (bed alarm) was functioning for one of four sampled residents (Resident 1). Th...
Read full inspector narrative →
Apr 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to protect one of two sampled residents from abuse (Resi...
Read full inspector narrative →
Mar 2024
5 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of 49 sampled residents (Resident 37) reported loss of personal belongings was investigated. This failure resulted in not recove...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During a review of Resident 309's Record of admission (ROA), dated 3/6/24, the ROA indicated, Admitting .Diagnoses . Strain o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
2. During an observation on 3/14/24 at 9:53 a.m. in Resident 32's room, Licensed Vocational Nurse (LVN) was changing Resident 32's dressing of the wound to coccyx area. LVN removed the wound dressing,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0620
(Tag F0620)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure five of 49 sampled residents (Resident 15, Resident 32, Resi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to develop and implement an action plan in the facility's Quality Assessment and Performance Improvement (QAPI), when the Pharmacist had ident...
Read full inspector narrative →
Nov 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to prevent abuse for one of three sampled residents (Resident 1). This failure had the potential for negative consequences including physical h...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to implement its policy and procedure (P&P) regarding employee abuse tr...
Read full inspector narrative →
Oct 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to notify one of three sampled residents (Resident 2) resident's representative (RR) regarding a change of condition. This failure resulted in...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement the plan of care for one of three sampled residents (Resident 1). This failure had the potential for accidents and ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to:
1. Complete a Neurological Record (NR) for one of three sampled re...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure an allegation of verbal abuse was reported in a timely manner for one of 5 sampled residents (Resident 1). This failure resulted in ...
Read full inspector narrative →
Jul 2022
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to:
1. Ensure a call light was placed within reach for one of 29 sampled residents (Resident 11).
2. Facilitate provision of he...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the advance directive (documentation indicating a person's wishes for end-of-life care) was prepared for one of four sampled residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure nursing assessments were completed for one of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop/update care plans for two of 29 sampled residents (Resident 26 and Resident 28) when they were tested positive for COVID-19 (highly...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide appropriate services to maintain hygiene for one of 29 sampled residents (Resident 3) when showers were not given as ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure vision care and devices were provided for one of one sampled resident (Resident 35). This failure resulted in Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide restorative services to prevent a decline in range of motion for one of one sampled resident (Resident 10). This fail...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
4. During a concurrent observation, interview, and record review, on 7/13/22, at 12:14 PM, with Registered Nurse (RN), in Nurses' Station 1's medication room, the E-Kit was observed with a red plastic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
2. During a concurrent interview and record review on 7/13/22, at 11:34 AM, with Registered Nurse (RN) 1, in nurses' station 1, at medication cart 1, Resident 3's package of unit dose vials containing...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure a thermometer was placed inside the kitchen dry food storage room to monitor the temperature. This failure had the pot...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0840
(Tag F0840)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to follow its policy and procedure (P&P) when audiology (assess and diagnose hearing issues) services were provided to 3 of 3 sampled resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure complete and accurate medical records for three of 29 sampled residents (Resident 2, Resident 18, Resident 33). This f...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 42% turnover. Below California's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 1 harm violation(s), $42,640 in fines, Payment denial on record. Review inspection reports carefully.
- • 50 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $42,640 in fines. Higher than 94% of California facilities, suggesting repeated compliance issues.
- • Grade D (40/100). Below average facility with significant concerns.
About This Facility
What is Ridgecrest Regional Transitional Care And Rehabili's CMS Rating?
CMS assigns RIDGECREST REGIONAL TRANSITIONAL CARE AND REHABILI an overall rating of 2 out of 5 stars, which is considered below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Ridgecrest Regional Transitional Care And Rehabili Staffed?
CMS rates RIDGECREST REGIONAL TRANSITIONAL CARE AND REHABILI's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 42%, compared to the California average of 46%. This relatively stable workforce can support continuity of care. RN turnover specifically is 62%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Ridgecrest Regional Transitional Care And Rehabili?
State health inspectors documented 50 deficiencies at RIDGECREST REGIONAL TRANSITIONAL CARE AND REHABILI during 2022 to 2025. These included: 1 that caused actual resident harm and 49 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Ridgecrest Regional Transitional Care And Rehabili?
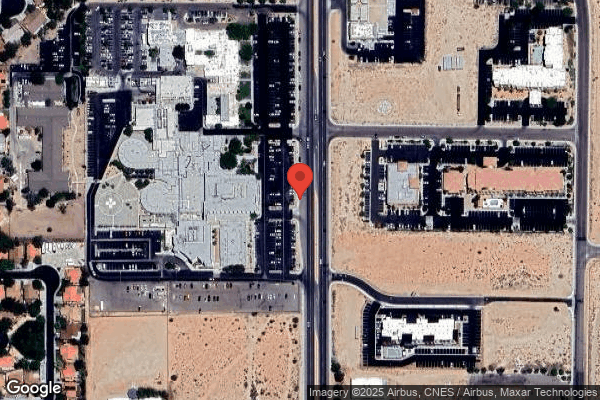
RIDGECREST REGIONAL TRANSITIONAL CARE AND REHABILI is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 124 certified beds and approximately 69 residents (about 56% occupancy), it is a mid-sized facility located in RIDGECREST, California.
How Does Ridgecrest Regional Transitional Care And Rehabili Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, RIDGECREST REGIONAL TRANSITIONAL CARE AND REHABILI's overall rating (2 stars) is below the state average of 3.1, staff turnover (42%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Ridgecrest Regional Transitional Care And Rehabili?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Ridgecrest Regional Transitional Care And Rehabili Safe?
Based on CMS inspection data, RIDGECREST REGIONAL TRANSITIONAL CARE AND REHABILI has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Ridgecrest Regional Transitional Care And Rehabili Stick Around?
RIDGECREST REGIONAL TRANSITIONAL CARE AND REHABILI has a staff turnover rate of 42%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Ridgecrest Regional Transitional Care And Rehabili Ever Fined?
RIDGECREST REGIONAL TRANSITIONAL CARE AND REHABILI has been fined $42,640 across 1 penalty action. The California average is $33,505. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Ridgecrest Regional Transitional Care And Rehabili on Any Federal Watch List?
RIDGECREST REGIONAL TRANSITIONAL CARE AND REHABILI is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.