MISSION DE LA CASA




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Mission de la Casa has a Trust Grade of B, indicating it is a good choice for families considering long-term care options, though there may be some areas for improvement. The facility ranks #131 out of 1,155 in California, placing it in the top half of nursing homes statewide, and #7 out of 50 in Santa Clara County, meaning only six local facilities are rated higher. The trend is improving, with issues decreasing from 14 in 2021 to 5 in 2024. Staffing is a strong point, earning a 5-star rating with a low turnover rate of 22%, which is significantly better than the state average. However, the facility has incurred $79,620 in fines, which is higher than 81% of California facilities, suggesting some ongoing compliance issues. There are serious concerns regarding resident safety, as one resident fell and sustained a fatal injury due to a lack of supervision, despite being assessed as high risk for falls. Additionally, there were incidents of improper infection control practices, such as staff not wearing masks correctly and failing to sanitize equipment, which could potentially affect all residents. While the facility shows strengths in staffing and overall quality ratings, the concerning fines and specific incidents highlight areas that need attention.
- Trust Score
- B
- In California
- #131/1155
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ✓ Good
- 22% annual turnover. Excellent stability, 26 points below California's 48% average. Staff who stay learn residents' needs.
- Penalties ⚠ Watch
- $79,620 in fines. Higher than 78% of California facilities, suggesting repeated compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 41 minutes of Registered Nurse (RN) attention daily — about average for California. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 36 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Staffing Rating · Excellent nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Low Staff Turnover (22%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (22%)
26 points below California average of 48%
Facility shows strength in staffing levels, quality measures, staff retention, fire safety.
The Bad
Well above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 36 deficiencies on record
Jun 2024
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
2. An admission Record revealed the facility admitted Resident #67 on 03/31/2023. According to the admission Record, the resident had a medical history that included diagnoses of major depressive diso...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, record review, interview, and facility policy review, the facility failed to ensure the medication error rate was five percent (%) or less. Medication administration observations...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and facility policy review, the facility failed to sanitize the food thermometer between measuring the temperatures of different food items. This had the potential to ...
Read full inspector narrative →
Apr 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure supervision was provided to one of three residents (Resident...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement their policies and procedures for ensuring ...
Read full inspector narrative →
Jul 2021
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
3. During observation and concurrent interview with licensed vocational nurse J (LVN J), on 7/7/21 at 4:02 p.m., LVN J administered medications in Resident 99's gastrostomy tube (g-tube, surgically pl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure needs were accommodated for five of 24 sampled ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on an observation, interview and record review, the facility failed to complete a significant change in status assessment ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Review of Resident 47's clinical record indicated she was admitted on [DATE] with diagnosis including schizoaffective disorder (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. During observation and concurrent interview with RN G, on 7/6/21 at 8:15 a.m., RN G was observed preparing medications for Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide showers for one of 24 sampled residents (Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of Resident 61's clinical record indicated Resident 61 was admitted to the facility on [DATE] with diagnosis including...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement the policy and procedure for continence management for on...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide dialysis services consistently with profession...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to properly store medication when:
1. One of two medicati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the kitchen staff are aware of the process to measure the sanitizer level of the dishwasher, when cook E (KC E) did no...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to properly store food for one of 24 sampled residents (Resident 74) when a family member brought food from home and the residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Additional review of Resident 66's surveillance data collection form indicated on 7/7/21 Resident 66's culture and sensitivity (...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure infection control practices were implemented w...
Read full inspector narrative →
Mar 2019
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide written notification to the Long-Term Care Ombudsman (person who routinely visits the facility and advocates for the residents) for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a baseline care plan was developed within 48 hours of admiss...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to:
1. Implement fall care plan for Resident 447.
2. Implement pressure ulcer care plan for Resident 62.
These failures had th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a picture communication system for ADL (activities of daily living; basic self-care tasks) needs/requests was availabl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide adequate nail care for one of 31 sampled resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure quality of care was provided for two of 31 sam...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2a. During a review of the clinical record for Resident 150, the Order Summary Report indicated he was admitted to the facility ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to ensure two of 31 sampled residents (Residents 74 and 71) received treatments to maintain range of motion (ROM, exercises to maintain or in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to implement their fall management policy and procedure for one of 31...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to timely receive medications from the provider pharmacy...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of 31 residents (Resident 447) has the correct indication for medication when clopidogrel bisulfate (an antiplatelet used to pre...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of 31 sampled residents (Resident 14) was free from unnecessary psychotropic medications (drugs that affects brain...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility had a 6.9% medication error rate when two medication errors out...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure medication was stored appropriately when a bottle of travoprost eye drops (medication for glaucoma, a condition of inc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
3. During a wound treatment observation for Resident 150's right foot pressure injuries with RN A on 3/19/19 at 9:59 a.m., RN A did not perform hand hygiene in between changing gloves.
During an inter...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to ensure a safe environment when several puddles of water were found on...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure sanitary conditions were maintained in the food services area when:
1. An open air vent and fan had dust particles and...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 22% annual turnover. Excellent stability, 26 points below California's 48% average. Staff who stay learn residents' needs.
- • 36 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $79,620 in fines. Extremely high, among the most fined facilities in California. Major compliance failures.
About This Facility
What is Mission De La Casa's CMS Rating?
CMS assigns MISSION DE LA CASA an overall rating of 5 out of 5 stars, which is considered much above average nationally. Within California, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Mission De La Casa Staffed?
CMS rates MISSION DE LA CASA's staffing level at 5 out of 5 stars, which is much above average compared to other nursing homes. Staff turnover is 22%, compared to the California average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Mission De La Casa?
State health inspectors documented 36 deficiencies at MISSION DE LA CASA during 2019 to 2024. These included: 1 that caused actual resident harm and 35 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
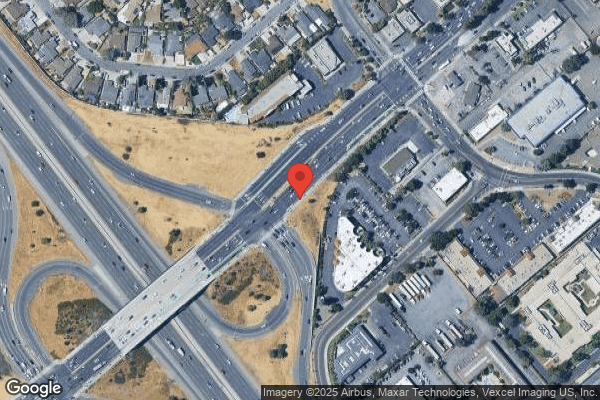
Who Owns and Operates Mission De La Casa?
MISSION DE LA CASA is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 163 certified beds and approximately 150 residents (about 92% occupancy), it is a mid-sized facility located in SAN JOSE, California.
How Does Mission De La Casa Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, MISSION DE LA CASA's overall rating (5 stars) is above the state average of 3.2, staff turnover (22%) is significantly lower than the state average of 46%, and health inspection rating (4 stars) is above the national benchmark.
What Should Families Ask When Visiting Mission De La Casa?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Mission De La Casa Safe?
Based on CMS inspection data, MISSION DE LA CASA has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 5-star overall rating and ranks #1 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Mission De La Casa Stick Around?
Staff at MISSION DE LA CASA tend to stick around. With a turnover rate of 22%, the facility is 24 percentage points below the California average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly. Registered Nurse turnover is also low at 21%, meaning experienced RNs are available to handle complex medical needs.
Was Mission De La Casa Ever Fined?
MISSION DE LA CASA has been fined $79,620 across 1 penalty action. This is above the California average of $33,875. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Mission De La Casa on Any Federal Watch List?
MISSION DE LA CASA is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.