SAN RAFAEL HEALTHCARE & WELLNESS CENTER, LP
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
San Rafael Healthcare & Wellness Center has received a Trust Grade of F, indicating significant concerns and a poor overall rating. They rank #900 out of 1155 facilities in California, placing them in the bottom half of state nursing homes, and #8 out of 11 in Marin County, meaning only a few local options are worse. The facility is experiencing a worsening trend, with issues increasing from 2 in 2024 to a staggering 32 in 2025. Staffing is a concern as well, with a turnover rate of 51%, which is above the California average of 38%, and overall staffing is rated at 2 out of 5 stars, indicating below-average performance. Specific incidents of concern include a resident who suffered severe falls due to inadequate monitoring and a lack of physical therapy, and unsafe food preparation practices that could expose residents to foodborne illnesses. While the facility does have average RN coverage, the high number of issues and critical deficiencies suggest families should carefully consider their options before choosing this nursing home.
- Trust Score
- F
- In California
- #900/1155
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 51% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $8,278 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 29 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 56 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below California average (3.1)
Below average - review inspection findings carefully
Near California avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Minor penalties assessed
The Ugly 56 deficiencies on record
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to protect one resident (Resident 1) of four sampled res...
Read full inspector narrative →
Jun 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record reviews, the facility failed to ensure two out of five sampled residents (Resident ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, the facility failed to provide service aligned with professional standards for one out of five sampled residents (Resident 1) when medication was ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interviews and record reviews, the facility failed to a safe and sanitary environment for three out of five sampled residents when:
1. Toothbrushes found in a shared bathroom wer...
Read full inspector narrative →
May 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to ensure:
1. An alleged sexual abuse incident on 4/28/25 was reported to the local ombudsman (an advocate for residents of nursing homes, b...
Read full inspector narrative →
Apr 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure pain management was provided to 1 of 3 sampled residents (Resident 1), when Resident 1 ' s pain intensity level was no...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure four of five sampled residents (Resident 1, Resident 3, Resident 4 and Resident 5) could call for staff assistance thr...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to honor the residents' right to be informed of the plan...
Read full inspector narrative →
Mar 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement and monitor the effectiveness of interventions of a care ...
Read full inspector narrative →
Mar 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to ensure a copy of the notice of transfer was sent to the representative of the Office of the State Long-Term Care (LTC) Ombudsman (an advo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to ensure one out of two sampled residents (Resident 1) was free from unnecessary psychotropic medications (drugs that affect the brain and ...
Read full inspector narrative →
Mar 2025
18 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the call light for one of 26 sampled residents...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of 26 sampled residents (Resident 1) was notified of a room/roommate change with a written notice that included the reason befor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the shower's water temperature was comfortable for one of 26 sampled residents (Resident 1). This failure resulted in ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a copy of notice of transfer/discharge was sent to the Ombud...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to assess and submit accurate data for one of 26 sampled residents (Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During a review of Resident 9's admission Record, dated 3/18/2025, the admission Record indicated Resident 9 was admitted to ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to assist one of 26 sampled residents (Resident 50) with...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide the necessary services to attain the highest practicable ph...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to label an enteral feeding (a method to provide food th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a Licensed Vocational Nurse (LVN) appropriatel...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the medication error rate was not greater than...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide physical therapy treatment (PT, the treatment of disease, i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow and implement infection control practices for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide a sanitary environment when one of 26 sampled ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure services provided met professional standards of practice when:
1. Resident 54 did not receive scheduled medications in ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure insulin (medication used to reduce blood sugar...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure medications, supplements, and supplies were app...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure that food was stored in safe and sanitary conditions in the food service department when:
1. The kitchen refrigerator ...
Read full inspector narrative →
Feb 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to provide a written notice to a resident's Responsible Party (RP) for one resident (Resident 2) of three sampled residents when Resident 2 w...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to develop and implement a person-centered care plan for one resident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to provide adequate supervision to one resident (Resident 1) of three sampled residents when Resident 1 eloped from the facility. This failur...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to manage the dialysis (use of a machine to clean the blood when the kidneys are no longer able to do this) care of one of two sampled residen...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to develop a system for validating the competencies of registry nurses. This failure had the potential to result in residents being cared for b...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to protect one of three sampled residents (Resident 1's) right to be f...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0912
(Tag F0912)
Could have caused harm · This affected multiple residents
Based on observation and concurrent interview with the Administrator on 8/2/23, the facility failed to provide bedrooms measuring at least 80 square feet per resident in 4 of 27 resident rooms (rooms ...
Read full inspector narrative →
May 2023
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete and obtain informed consents (a consent that provides the ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the call light and the phone were within reach...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of 21 sampled residents (Resident 37) had a Physician Or...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a physician's order for a floor pad next to th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that one of three sampled residents (Resident 301) received ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure two of 21 sampled residents (Resident 5 and Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure:
1. The Residents' Refrigerator was free of ice buildup.
2. The Residents' food that was brought into the facility was ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure the garbage was disposed of properly when one of the garbage dumpster lids was not closed, and the surrounding area had trash on the g...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the Medication Administration Records (MAR) fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain a safe environment for one resident, with an intellectual disability (Resident 101), out of 21 sampled residents, wh...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility did not record accurate diagnoses on the Minimum Data Set Reports (MDS- an as...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure safe and sanitary food preparation and storage practices requirement were met in the kitchen when:
1. The Ansul System...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. During an interview on 5/23/23, at 10:27 a.m., with Maintenance Director 1 (MD 1), when asked about the facility's water mana...
Read full inspector narrative →
Apr 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure prompt notification of a change in condition of one of three sampled residents (Resident 2), when Resident 2 ' s Responsible Party (...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on interview and record review, facility failed to ensure dialysis services were provided as ordered, when it failed to arrange for necessary transportation services for one of one sampled resid...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility did not implement its infection control policies, when it failed to maintain an Infection Preventionist. This failure had the potential for ineffecti...
Read full inspector narrative →
Jan 2020
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure one sampled resident (Resident 38) received oxygen therapy per physician's order and facility policy. This failure had ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to provide oversight and supervision, by a Registered Dietician, to kitchen staff (Cook C). This failure resulted in the Register...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview and review of documents, the facility failed to ensure food was prepared, stored, served or distributed in accordance with professional standards of food service safety...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
During an observation and interview on 1/13/20 at 12:45 p.m. in Resident 23's room, Resident 23 was not offered hand hygiene before his meal. Resident 23 stated, When I cannot get up, I have to put my...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 1 harm violation(s), Payment denial on record. Review inspection reports carefully.
- • 56 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade F (28/100). Below average facility with significant concerns.
About This Facility
What is San Rafael Healthcare & Wellness Center, Lp's CMS Rating?
CMS assigns SAN RAFAEL HEALTHCARE & WELLNESS CENTER, LP an overall rating of 2 out of 5 stars, which is considered below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is San Rafael Healthcare & Wellness Center, Lp Staffed?
CMS rates SAN RAFAEL HEALTHCARE & WELLNESS CENTER, LP's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 51%, compared to the California average of 46%. RN turnover specifically is 69%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at San Rafael Healthcare & Wellness Center, Lp?
State health inspectors documented 56 deficiencies at SAN RAFAEL HEALTHCARE & WELLNESS CENTER, LP during 2020 to 2025. These included: 1 that caused actual resident harm and 55 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates San Rafael Healthcare & Wellness Center, Lp?
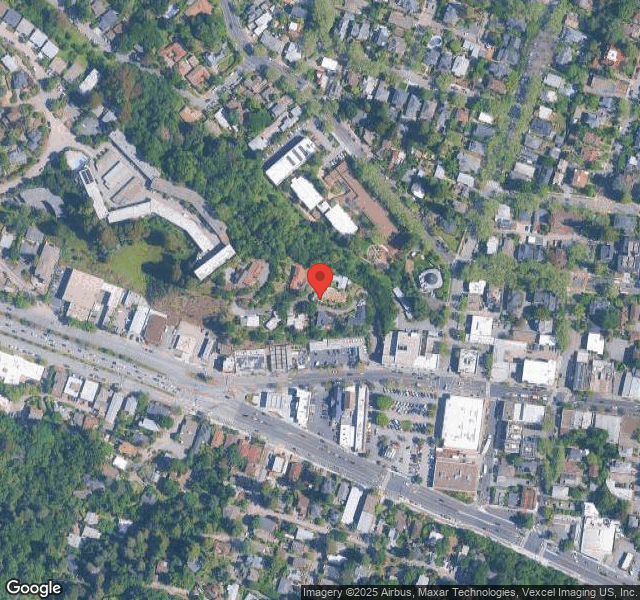
SAN RAFAEL HEALTHCARE & WELLNESS CENTER, LP is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 54 certified beds and approximately 58 residents (about 107% occupancy), it is a smaller facility located in SAN RAFAEL, California.
How Does San Rafael Healthcare & Wellness Center, Lp Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, SAN RAFAEL HEALTHCARE & WELLNESS CENTER, LP's overall rating (2 stars) is below the state average of 3.1, staff turnover (51%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting San Rafael Healthcare & Wellness Center, Lp?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the below-average staffing rating.
Is San Rafael Healthcare & Wellness Center, Lp Safe?
Based on CMS inspection data, SAN RAFAEL HEALTHCARE & WELLNESS CENTER, LP has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in California. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at San Rafael Healthcare & Wellness Center, Lp Stick Around?
SAN RAFAEL HEALTHCARE & WELLNESS CENTER, LP has a staff turnover rate of 51%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was San Rafael Healthcare & Wellness Center, Lp Ever Fined?
SAN RAFAEL HEALTHCARE & WELLNESS CENTER, LP has been fined $8,278 across 1 penalty action. This is below the California average of $33,162. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is San Rafael Healthcare & Wellness Center, Lp on Any Federal Watch List?
SAN RAFAEL HEALTHCARE & WELLNESS CENTER, LP is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.