LINWOOD MEADOWS CARE CENTER




Inspected within the last 6 months. Data reflects current conditions.
Linwood Meadows Care Center has a Trust Grade of C+, indicating it is slightly above average but still has room for improvement. It ranks #620 out of 1155 facilities in California, placing it in the bottom half, and #8 out of 16 in Tulare County, meaning only seven local options are better. The facility's trend is concerning as the number of issues has worsened significantly, increasing from 4 in 2024 to 19 in 2025. Staffing is rated average with a 3/5 star rating, but the 47% turnover rate is concerning, as it is higher than the state average. On a positive note, there have been no fines reported, which is a good sign. However, the facility has less RN coverage than 99% of California facilities, which raises concerns about the quality of care. Specific incidents noted by inspectors include failures in infection surveillance that could lead to outbreaks, inadequate food handling practices that may cause foodborne illnesses, and improper garbage disposal that could attract pests. Overall, while there are some strengths, families should be aware of the significant areas needing improvement.
- Trust Score
- C+
- In California
- #620/1155
- Safety Record
- Low Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 47% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most California facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 9 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 57 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near California average (3.1)
Meets federal standards, typical of most facilities
Near California avg (46%)
Higher turnover may affect care consistency
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 57 deficiencies on record
Aug 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the physician was notified when one of three sampled residents (Resident 1) medication was not administered per physician's orders. ...
Read full inspector narrative →
May 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to report allegations of physical abuse to the California Department o...
Read full inspector narrative →
May 2025
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to:
1. Ensure Informed Consent (IC, a process in which a healthcare pr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to assess the effectiveness of the plan of care for the ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to act on a recommendation from the pharmacy consultant (a professiona...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to maintain accurate medical records for two of 38 sampled residents (Resident 3 and Resident 142) when the Nursing Weekly Summary (NWS) did n...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure maintenance staff conducted bed rail risk assessments to inc...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to offer, obtain, and complete advance directives (AD- a written statement of a person's wishes regarding medical treatment when one is unable...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During a review of Resident 14's AR, dated 1/23/23, the AR indicated, Resident 14 was admitted on [DATE] with diagnosis includin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure a Registered Nurse (RN) worked at least eight hours a day, seven days a week on 11 of 21 sampled days. This failure had the potentia...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to have an effective Certified Nurse Assistant (CNA) performance evaluation (PE- a process to give employees feedback on their job performance...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0807
(Tag F0807)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to:
1. Honor two of 25 sampled residents (Resident 31, Resident 73) food preferences.
2. Follow physician diet orders for one o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure:
1. Opened Food items were labeled with an open date.
2. Dented cans were properly discarded.
These failures had th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure infection control practices were implemented when:
1. Three large barrels containing residents' clean personal laundry...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to:
1. Maintain an effective antibiotic stewardship (efforts to ensure that antibiotics are used only when necessary and appropriate) for one ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to provide in-service education on Covid-19 (severe respiratory illness) for 143 of 186 total staff. This failure had the potential for staff ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain an ambient (surrounding air) temperature for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure :
1. Six of Six sampled Certified Nursing Assistants (CNA 3, CNA 1, CNA 2, CNA 5, CNA 6 and CNA 4) attended a minimum of five hours ...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a fall assessment was accurate for one of two sampled residents (Resident 1). This failure had the potential for staff to be unaware...
Read full inspector narrative →
Dec 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0837
(Tag F0837)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow its policy and procedure when staff in-service training records were incomplete. This failure resulted in incomplete training record...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure three of three sampled staff Restorative Nursing Assistant (RNA 1), Registered Nurse (RN 1), and Certified Nursing Assistant (CNA 1)...
Read full inspector narrative →
Nov 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0551
(Tag F0551)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure two of three sampled residents (Resident 1 and Resident 2) R...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop and implement a care plan for two of two sampled residents (Resident 1 and Resident 2). This failure had the potential for Resident...
Read full inspector narrative →
Dec 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
Oct 2023
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow their policy and procedure titled, Dignity, for one of two sampled residents (Resident 299), when a urine collection b...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) titled, Transfer or Discharge Notice, when the facility did not send a notice of transfer to the Om...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
2. During a concurrent interview and record review on 10/25/23 at 2:42 p.m. with Minimum Data Set (MDS) Coordinator, Resident 19's MDS assessment, dated 9/13/23 was reviewed. The MDS Section L labeled...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow its policy and procedure titled, Administering Medications when:
1. The Director of Nursing of Nursing (DON) did not c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of 19 sampled residents (Resident 29) received nail care. This failure had the potential to cause injury to Reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, record review, the facility failed to ensure one of eight sampled residents (Resident 14) physician's order for treatment was followed. This failure had the potential ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow their policy and procedure (P&P) titled, Medic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of two sampled residents (Resident 36)'s diet texture was followed according to the physician's order. This failur...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement an effective antibiotic stewardship program when one of six sampled residents (Resident 86) was reviewed and monitored for the us...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide for three of eight sampled residents (Resident 14, Resident 62, Resident 55) a home-like environment when:
1. Residen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide prompt efforts to act on and resolve grievances for two of seven sampled residents (Resident 54 and Resident 70). Thi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure manufacturers guidelines were followed for use of low air loss (LAL) mattresses (mattress used for prevention of press...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During an interview on 10/25/23 at 9:47 a.m. with Resident 55, Resident 55 stated, I need my teeth cleaned, they [staff] said th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure food items in the storage area were labeled and dated. This failure had the potential to result in foodborne illnesses...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0924
(Tag F0924)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure a handrail was firmly secured and in good repair. This failure had the potential to expose residents and visitors to i...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to follow its policy and procedure on:
1. Surveillance for Infections when the monthly reports did not contain the complete information requir...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policy (P&P) on Verify Leave of Absence for one of thr...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure the glucometer (a medical device used to measure the amount of sugar in the blood) was properly disinfected prior to us...
Read full inspector narrative →
Jul 2021
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to accurately code the Minimum Data Set (MDS- a standardized screening...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop and implement comprehensive care plans for th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Surveyor: [NAME], [NAME]
Based on observation, interview, and record review, the facility failed to ensure two of 24 sampled res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of 24 sampled residents (Resident 32) rece...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on interview and record review, the consultant pharmacist failed to identify and make recommendations to attempt a gradual dose reduction of an antipsychotic drug (classification of drugs used t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to attempt a gradual dose reduction of an antipsychotic drug (classifi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure medication error rate was five percent or less when four medication errors were observed out of 42 medication administ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure Minimum Data Set (MDS- standardized screening assessment too...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to follow their policy and procedure (P&P) for the reconciliation of controlled substances (a drug subject to special handling, storage, and d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to:
1. Lock controlled substances in one of five medication carts.
This failure had the potential to result in medication loss....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure two of five sampled residents (Resident 24 and Resident 50) ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the dietary staff failed to follow proper sanitation and safe food handling practices when:
1. Ensuring the inside of two clean plate covers were no...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure garbage and refuse were properly collected and disposed in a safe and efficient manner. This failure had the potential...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to:
1. Handle, store, process linens in a safe and sanitary method to prevent the spread of infection.
2. Store clean briefs ap...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review, the facility failed to provide an effective pest control program. This failure h...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most California facilities.
- • 57 deficiencies on record. Higher than average. Multiple issues found across inspections.
About This Facility
What is Linwood Meadows's CMS Rating?
CMS assigns LINWOOD MEADOWS CARE CENTER an overall rating of 3 out of 5 stars, which is considered average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Linwood Meadows Staffed?
CMS rates LINWOOD MEADOWS CARE CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 47%, compared to the California average of 46%.
What Have Inspectors Found at Linwood Meadows?
State health inspectors documented 57 deficiencies at LINWOOD MEADOWS CARE CENTER during 2021 to 2025. These included: 57 with potential for harm. While no single deficiency reached the most serious levels, the total volume warrants attention from prospective families.
Who Owns and Operates Linwood Meadows?
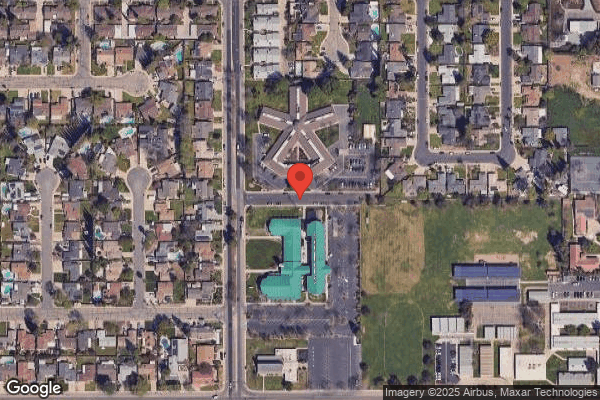
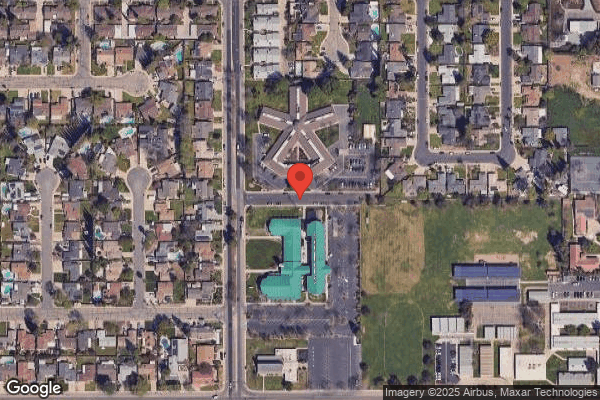
LINWOOD MEADOWS CARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PACS GROUP, a chain that manages multiple nursing homes. With 98 certified beds and approximately 92 residents (about 94% occupancy), it is a smaller facility located in VISALIA, California.
How Does Linwood Meadows Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, LINWOOD MEADOWS CARE CENTER's overall rating (3 stars) is below the state average of 3.1, staff turnover (47%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Linwood Meadows?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Linwood Meadows Safe?
Based on CMS inspection data, LINWOOD MEADOWS CARE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Linwood Meadows Stick Around?
LINWOOD MEADOWS CARE CENTER has a staff turnover rate of 47%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Linwood Meadows Ever Fined?
LINWOOD MEADOWS CARE CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Linwood Meadows on Any Federal Watch List?
LINWOOD MEADOWS CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.