SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to ensure the resident's environment was free from acci...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to ensure the resident's environment was free from accident hazards for three (#95, #12 and #19) of eight residents reviewed for falls out of 53 sample residents.
Resident #95, who had a previous history of falls at the facility and was identified to be at high risk for falling, experienced a fall on 1/9/24 which resulted in a left hip fracture that required hospitalization and a left partial hip replacement.
The facility failed to ensure effective and timely interventions were in place after 11/27/23 to prevent Resident #95 from sustaining a fall on 1/9/24 which resulted in a left hip fracture. The facility failed to ensure effective interventions to prevent additional falls on 2/6/24 and 3/1/24.
The facility failed to timely assess and notify providers of the fall on 1/9/24 until two hours after Resident #95 began complaining of left lower extremity pain, when pain medication and a hip x-ray was ordered.
The facility failed to notify the provider for further orders when the x-ray was not completed until 12 hours after the - ray was initially ordered and 14 hours after Resident #95 began complaining of left lower extremity pain.
The facility's failures to implement effective and timely fall interventions resulted in Resident #95 sustaining a fall resulting in a left hip fracture. Due to the facility's failure to follow-up timely with the provider after the resident's fall and complaints of pain, Resident #95's left hip fracture was not identified and treated in a timely manner.
Resident #12 was admitted on [DATE] with a known history of repeated falls and fall with major injury. Resident #12 sustained a fall on 11/13/23 which resulted in an abrasion to the resident's back.
The facility implemented a fall intervention for Resident #12's bed to be in the lowest position when she was in bed following the 11/13/23 fall, however, facility staff failed to implement the intervention or report the resident refused to allow her bed to be in the lowest postion.
Resident #12 sustained a second fall on 1/20/24 which resulted in the resident being transferred to the hospital and receiving 12 staples for a laceration to the back of her head.
The facility again failed to update Resident #12's care plan with additional interventions or reassess the resident's fall interventions to determine their effectiveness.
Due to the facility's failure to implement and monitor the effectiveness of fall interventions, Resident #12 sustained a fall resulting in a laceration to the back of her head which required staples.
Additionally, the facility failed to:
-Ensure staff were implementing the fall interventions identified on Resident #19's care plan; and,
-Ensure staff knew what person-centered fall interventions were to be implemented for Resident #19 and where to locate what interventions were to be implemented for the resident.
Findings include:
I. Facility policy and procedure
The Fall Management System policy and procedure, reviewed December 2023, was provided by the nursing home administrator (NHA) on 3/7/24 at 1:20 p.m. It read in pertinent part,
It is also the policy of this facility to provide each resident with appropriate assessment and interventions to prevent falls and to minimize complications if a fall occurs.
Residents with high risk factors identified on the Fall Risk Evaluation will have an individualized care plan developed that includes measurable objectives and timeframes. The care plan intervention will be developed to prevent falls by addressing the risk factors and will consider the particular elements of the evaluation that put the resident at risk.
When a resident sustains a fall, a physical assessment will be completed by a licensed nurse, with results documented in the medical record.
II. Resident #95
A. Resident status
Resident #95, age [AGE], was admitted on [DATE] and readmitted on [DATE]. According to the March 2024 computerized physician orders (CPO), diagnoses included left femur fracture, vulvar cancer and dementia.
The 1/20/24 minimum data set (MDS) assessment revealed the resident was cognitively intact with a brief interview for mental status (BIMS) score of 15 out of 15. She required supervision/touch assistance with transfers and toileting, set up assistance for eating and was independent with personal hygiene and bed mobility.
The assessment documented the resident did not have any falls since the prior assessment or admission.
B. Observations and resident interview
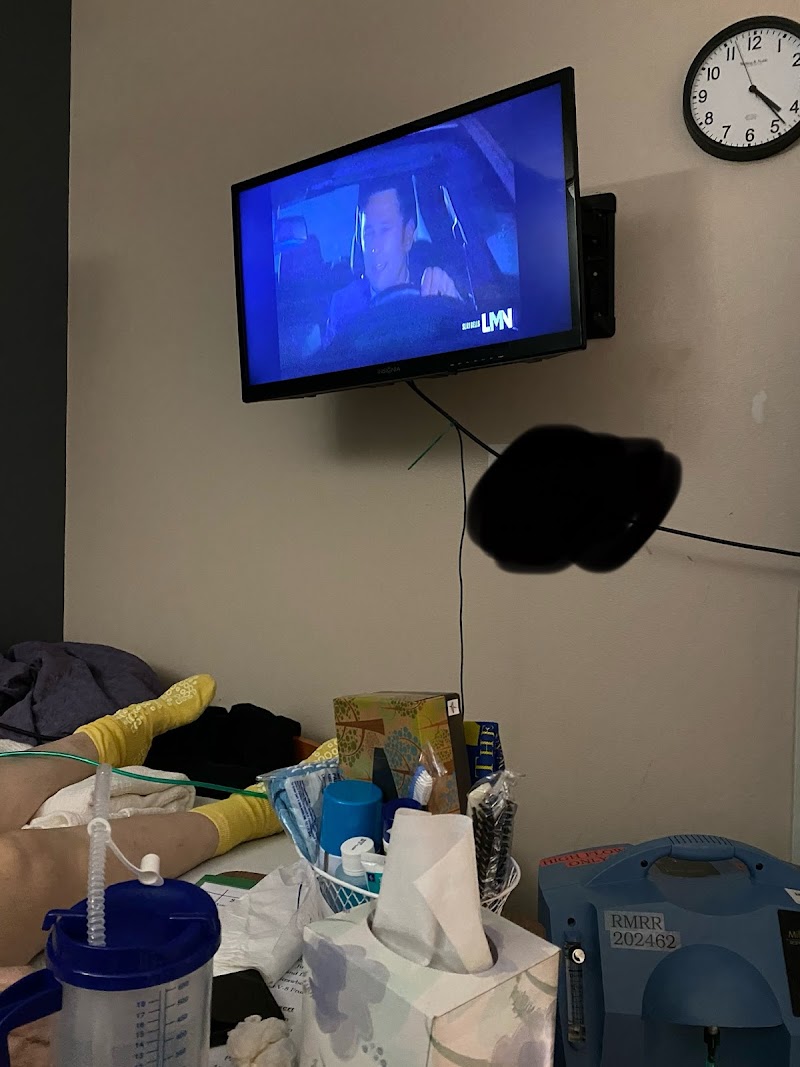
On 3/5/24 at 1:26 p.m., Resident #95 was sitting in a wheelchair wearing non-skid socks. Resident #95's bed mattress was observed to have raised edges.
-There was no bedside floor mat observed in the room and no signage to remind the resident to call for assistance was observed in the room.
On 3/6/24 at 1:00 p.m., Resident #95 was lying in bed on a raised edge mattress. The resident's bed was in a low position.
-There was no floor mat observed on the floor next to the resident's bed and no signage to remind the resident to use her call light for assistance was observed in the room.
On 3/7/24 at 1:00 p.m., signage was observed taped to the wall at the foot of Resident #95's bed underneath the television.
Resident #95 was interviewed on 3/7/24 at 1:00 p.m. She said the night she broke her hip she fell on the floor next to the bathroom. She said when they returned her to bed it hurt a lot. She said it took them a long time to call the doctor and finally call an ambulance to take her to the hospital. She said she did not know what hipsters were and she was not currently wearing them.
C. Record review
The fall care plan, initiated 10/13/21 revised 3/8/23, indicated Resident #95 had experienced a fall. Interventions included signage to remind the resident to call for help, therapy to focus on safety with turning and sitting safely in chairs, bed bolsters in bed, bed in lowest position, non-skid socks, needed items within reach and neurological checks.
The actual fall care plan, initiated on 1/11/24, indicated Resident #95 had experienced an actual fall with a left hip fracture. Interventions included bed in lowest position, encourage resident to share feelings with staff and engage in meaningful activities, evaluate height of chair and assess for super hemi chair versus leg rests, floor mat when resident was in bed, monitor and report to physician for pain, bruises, change in mental status, offer and encourage resident to wear hipsters for protection and therapy consult.
A comprehensive review of the care plan interventions included to ensure staff applied non-skid socks was added after an unwitnessed fall out of her wheelchair on 11/27/23.
A comprehensive review of the care plan interventions revealed bed placed in lowest position on 1/11/24, floor mat when resident was in bed and hipsters on 1/18/24 after the resident experienced a fall with hip fracture on 1/9/24.
-However, observations revealed there was no floor mat next to the resident's bed when she was in bed and the resident said she did not know what hipsters were and was not wearing any (see observations and resident interview above).
A comprehensive review of the care plan interventions revealed bed bolsters applied on 2/6/24 after the resident experienced a fall rolling out of bed on 2/6/24.
A comprehensive review of the care plan intervention revealed evaluation of wheelchair height and assess for hemi chair versus leg rests on 3/4/24 after the resident experienced a fall transferring from her wheelchair to the bed.
The 11/27/23 nursing progress note revealed Resident #95 had an unwitnessed fall out of her wheelchair. The resident was combative and had an elevated blood pressure and pulse during the assessment. The resident was observed wearing fuzzy non gripping socks. The resident was sent to the emergency department for further evaluation for a change in behaviors.
The 11/28/23 fall committee interdisciplinary team (IDT) progress notes documented interventions initiated ensuring staff encouraged the use of non-slip socks at all times and occupational therapy upon the resident's return from the hospital.
The 12/14/23 fall risk assessment indicated Resident #95 was at high risk for falls.
The 1/9/24 at 9:30 p.m. nursing progress notes documented a fall, witnessed by a certified nurse aide (CNA), while the resident was ambulating in the room. There was no visible injury upon assessment by the registered nurse (RN) and the staff assisted the resident into a wheelchair.
-A comprehensive review of Resident #95's electronic medical record (EMR) failed to reveal documentation of a pain assessment before the resident was moved to the wheelchair.
-There was no documentation of notification of the provider, director of nursing (DON) or family members immediately after the fall.
The 1/9/24 at 10:30 p.m. nursing progress notes documented the resident was complaining of left lower extremity pain. The RN assessment indicated there was no swelling or bruising. The RN explained to the resident she did not have pain medication ordered.
-There was no documentation to indicate the RN notified the provider or the fall at the time the resident was complaining of left lower extremity pain to obtain orders for pain medication or an x-ray.
The 1/10/24 at 12:22 a.m. physician's order revealed Ibuprofen 400 milligrams (mg) one time only for pain.
-The physician's order for pain medication was not obtained until two hours after Resident #95 began complaining of left lower extremity pain.
The 1/10/24 at 12:23 a.m. nursing progress notes documented the resident was complaining of left lower extremity pain and was moving the leg minimally. No injury was noted. A left hip x-ray was ordered.
-The order for the x-ray was not obtained until two hours after Resident #95 began complaining of left lower extremity pain.
The 1/10/24 at 1:49 p.m. nursing progress notes documented an x-ray of the resident's left hip was obtained at 12:30 p.m. and results of a fractured hip was reported to the facility. Resident #95 was sent to the hospital via ambulance at 1:40 p.m.
-The left hip x-ray was not obtained until 12 hours after it was ordered (14 hours after Resident #95 began complaining of left lower extremity pain).
-The EMR failed to reveal documentation that the facility had notified the provider for further orders when the left hip x-ray was not completed in a timely manner.
The 1/10/24 fall investigation documented a witnessed fall. The resident was ambulating in her room on 1/9/24 at 9:30 p.m. and fell on the floor onto her left side and did not hit her head. She had initially complained of right hip pain but later complained of left hip pain. She was assessed by two RN's. Orders were received for pain medication and a left hip x-ray. Resident #95 was sent to the hospital on 1/10/24 at 1:30 p.m. It documented the physician was notified at 1:25 pm. Family member was notified on 1/10/24 at 3:40 p.m. (Two hours after the resident was sent to the hospital).
The 1/16/24 hospital records documented the resident was admitted on [DATE] with a closed fracture of the left hip. The resident underwent surgery for a partial left hip replacement.
-A comprehensive review of Resident #95's EMR failed to reveal an IDT note post fall on 1/10/24.
The 1/16/24 fall risk assessment indicated Resident #95 was at high risk for falls.
The 2/6/24 nursing progress notes documented a witnessed fall when the resident rolled out of bed and fell onto her right side but did not hit her head. A physical assessment was performed and the resident had no obvious injuries and denied pain. She was assisted back to bed.
The 2/6/24 fall IDT progress notes documented a fall with no injuries. Interventions added were bolsters to the bed.
The 2/6/24 fall investigation documented a witnessed fall of the resident rolling out of bed and landing on her right side. It documented there was no physical injury on assessment and the resident denied pain. The resident was assisted back to bed and the bed was left in lowest position with call light in reach.
-A review of the EMR did not reveal if the bed mat was in place during the 2/6/24 fall.
The 3/1/24 nursing progress notes documented an unwitnessed fall when the resident was self transferring to the bed from the wheelchair. Resident was assisted to bed, bed lowered to the floor, bed mat in place and educated to use call light. Resident had no injuries, no pain, vital signs and neurological assessments were stable. Provider, DON and family were notified.
The 3/1/24 fall risk assessment indicated Resident #95 was at medium risk for falls.
The 3/4/24 IDT progress notes documented an unwitnessed fall with no injuries. Interventions added were occupational therapy to assess wheelchair.
The 3/4/24 occupational therapy (OT) notes documented the resident had low safety awareness. Interventions included were increasing functional ability to use walker, education to lock brakes on wheelchair before standing. Resident required verbal and tactile cues.
The CNA documentation for fall prevention devices (low bed, mats on floor, hipsters, visual checks, bolster pillow/concave mattress) in place from 2/7/24 to 3/6/24 revealed:
-On 2/7/24 there was no documentation of bed mats on the floor or bolster pillow/concave mattress in place;
-On 2/8/24 there was no documentation of hipsters in place;
-On 2/9/24 there was no documentation of bed mats on the floor or hipsters;
-On 2/10/24 there was no documentation of bed mats on the floor or hipsters;
-On 2/11/24 there was no documentation of bed mats on the floor, hipsters or non-skid socks;
-On 2/13/24 there was no documentation of bed mats on the floor;
-On 2/14/24 there was no documentation of bed mats on the floor;
-On 2/15/24 there was no documentation of bed mats on the floor;
-On 2/16/24 there was no documentation of bed mats or non-skid socks;
-On 2/17/24 there was no documentation of bed mats, hipsters or non-skid socks;
-On 2/18/24 there was no documentation of low bed;
-On 2/19/24 there was no documentation of bed mats on the floor or hipsters;
-On 2/21/24 there was no documentation of bed mats on the floor;
-On 2/22/24 there was no documentation of bed mats on the floor or non-skid socks;
-On 2/23/24 there was no documentation of bed mats on the floor, non-skid socks, and visual checks by staff;
-On 2/24/24 there was no documentation of bed mats on the floor or non-skid socks;
-On 2/25/24 there was no documentation of bed mats on the floor or non-skid socks;
-On 2/26/24 there was no documentation of bed mats on the floor or non-skid socks;
-On 2/27/24 there was no documentation of bed mats on the floor or non-skid socks;
-On 2/29/24 there was no documentation of bed mats on the floor or non-skid socks;
-On 3/1/24 there was no documentation of bed mats on the floor or non-skid socks;
-On 3/2/24 there was no documentation of bed mats on the floor or non-skid socks;
-On 3/3/24 there was no documentation of bed mats on the floor;
-On 3/4/24 there was no documentation of non-skid socks;
-On 3/5/24 there was no documentation of bed mats on the floor or non-skid socks; and,
-On 3/6/24 there was no documentation of bed mats on the floor.
The visual bedside kardex report (a tool utilized by CNAs to provide consistent care) indicated safety interventions included signage to remind the resident to call for help, added 10/22/21, bed bolsters, bed in lowest position, monitor for increased fall risk with position changes, needed items within reach, hipsters applied daily as tolerated and resident was independent with transfers.
D. Staff interviews
CNA #4 was interviewed on 3/7/24 at 12:45 p.m. CNA #4 said residents at high risk for falls should have a low bed and call light in reach. She said CNAs accessed the point of care (POC) task section to find out what fall interventions were in place for the resident. She said Resident #95 required a low bed and a call light in reach and one person assistance to transfer from wheelchair to the bed but she was getting to the point where she could transfer herself. She said she did not know of any other interventions. She said she did not know the frequency to check on Resident #95 but they would check on her every so often.
Licensed practical nurse (LPN) #1 was interviewed on 3/7/24 at 12:50 p.m. LPN #1 said fall interventions were populated in the treatment administration record (TAR). She said residents at high risk for falls should have interventions to include a call light in reach and a specialty bed. She said she did not know the specific fall interventions for Resident #95 but she said the resident should not be transferring herself from the wheelchair to the bed.
After consulting with the DON on how to access the care planned interventions, LPN #1 said Resident #95's interventions included a low bed, call light in reach, fall risk assessments, signage in room to call for help, a walker to ambulate, therapy to work with resident and bed mats in place while in bed.
The DON was interviewed on 3/11/24 at 9:32 a.m. The DON said when a fall occurred the fall was reported to the RN and the RN would conduct an assessment before the resident was removed from the floor. She said the provider, family and DON would be notified. She said risk management would be notified and a post fall IDT committee would meet the following day. She said the IDT committee did a root cause analysis with staff input for what interventions to put into place to help prevent further falls and minimize injury.
The DON said interventions were care planned and placed on the Kardex for CNAs. She said CNAs did a shift end report to discuss what fall interventions were in place for residents at high risk for falls. She said CNAs accessed the Kardex for the current fall interventions and the POC task tab was for documentation.
The DON said nurses accessed the care plan, progress notes and reviewed IDT post fall notes to get the most current information on fall interventions. She said nurses did not access fall interventions on the TAR.
The DON said standard fall interventions included call light in reach, bed in low position, floor mats, reminder signs, work around preferences to avoid self transfers, medication reviews, and frequent rounding every two hours. Increased rounding occurred with staff input for frequently falling residents. Frequent rounding was care planned and documented. She said frequent round documentation was on a separate form that was carried with the nurses.
The DON said Resident #95 had bed mats after returning from her hospitalization in January 2024, however, she said the floor mats had been removed as an intervention on 3/7/24 (during the survey) because it was a tripping hazard. She said when an intervention was removed it would be documented on the care plan.
The DON said Resident #95 would remove the signage to call for assistance. She said Resident #95 had not been cleared by therapy to self transfer. She said failure to implement or monitor fall interventions could result in additional falls or injury.
III. Resident #12
A. Resident status
Resident #12, age [AGE], was admitted on [DATE]. According to the March 2024 CPO, diagnoses included chronic respiratory failure, cognitive communication deficit, lack of coordination, compression fracture of the first lumbar (lower back) vertebrae and repeated falls.
The 1/27/24 MDS assessment revealed the resident had moderate cognitive impairment with a BIMS score of 12 out of 15. The resident required substantial assistance for bathing and transferring in and out of the shower; moderate assistance with dressing and personal hygiene, and bed/chair to chair transfers; and supervision or touching assistance with mobility and moving from a sit to stand position.
The MDS assessment revealed the resident had a history of a fall with a major injury.
B. Resident observations
On 3/7/24 at 7:59 a.m., Resident #12 was lying in bed in her room with the lights off.
Resident #12's bed was not in a low position and a wheelchair, walker and bedside table were next to the bed.
On 3/7/24 at 8:54 a.m., Resident #12 was lying in bed awake and reading.
-Resident #12's bed was not in a low position and a wheelchair, walker and bedside table were next to the bed.
-A review of the Fall Prevention Devices task response history revealed the low bed task was marked completed at 8:51 a.m. on 3/7/24 (see below).
On 3/10/24 at 7:50 a.m., Resident #12 was in her bed with the lights off.
-Resident #12's bed was not in a low position.
C. Record review
Resident #12's electronic medical record (EMR) documented Resident #12 had two falls at the facility on 11/13/23 and 1/22/24.
The 11/13/23 nursing progress notes documented at 6:20 p.m. a staff member heard Resident #12 yelling for help from her room. Upon entering the resident's room, Resident #12 was lying on her back with her walker standing upright at her feet. Her feet were facing the window and her head was facing the door.
Resident #12 said she was at her sink and when she turned to walk back to her chair, her right knee gave out. A RN was called to assess the resident.
The RN assessment indicated Resident #12 told the nurse that her arthritic right knee gave way and she fell on the floor, landing on her back. Resident #12 said she bumped her head.
The 11/13/23 fall committee interdisciplinary team (IDT) note documented Resident #12 had an unwitnessed fall in her room resulting in a small abrasion to her back.
-The IDT note did not include any interventions put into place except for placing the bed in the low position, which was initiated on 7/25/23, and a therapy evaluation, which was not new to the resident's comprehensive care plan.
The 1/20/24 nursing progress note documented at 7:30 a.m. a nurse heard a loud sound and someone yell for help while administering medications. The nurse ran to Resident #12's room and found Resident #12 on the floor in a supine position (on her back) in front of the bathroom.
Resident #12 said she was trying to go to the bathroom while using her walker and fell. Resident #12 denied pain and dizziness. A physical assessment was conducted on Resident #12 which revealed the resident was bleeding from the back of her head, with blood observed on the floor.
The nurse applied compression at the site of bleeding and shouted for help. Vital signs were taken and neurological observations began. Resident #12 appeared disoriented with time. Facility staff called 911 and and Resident #12 was transferred to a local hospital at 8:00 a.m. The physician, DON and Resident #12's family were notified.
The 1/22/24 fall committee IDT note documented Resident #12 had an unwitnessed fall in her room that resulted in a posterior (back of) scalp laceration. Resident #12 was subsequently sent to the emergency room where she received staples for a head laceration.
-The IDT note did not include any additional interventions put into place besides putting the bed in the low position, which had already been in place since 7/25/23, therapy evaluation (put into place since the previous fall) and a pharmacy consult.
-The facility continued to fail to put effective interventions into place to prevent further falls with injuries after the knowledge of the resident's history falls and actual recent falls.
A 3/2/24 nurse practitioner (NP) note documented Resident #12 had a past medical history of recurrent falls, and was at high risk for falls due to her poor safety awareness and generalized weakness.
Resident #12's Fall Prevention Devices task response history was reviewed from 2/11/24 to 3/10/24. A low bed was listed as a fall prevention device, however a clear pathway was not listed. The low bed was marked completed at least once per day during the review period, and there were no documented refusals by Resident #12 recorded by facility staff during the dates reviewed.
Resident #12's kardex (electronic care summary) was reviewed. Resident #12's kardex did not list the intervention of a clear pathway on her kardex, which was used by the CNAs to ensure fall interventions were in place (see interview below).
Resident #12's fall care plan, initiated on 7/25/23, documented Resident #12 was at risk for further falls related to medication side effects, a wedge compression fracture of lumbar (lower back region) and multiple falls. Resident #12 had additional post fall care plans initiated 11/13/23 and 1/22/24. The 1/22/24 fall care plan revealed she had a fall with injury requiring staples to her head.
Pertinent fall care plan interventions included:
-Be sure the call light was within reach and encourage the resident to use it to call for assistance as needed, initiated 7/25/23;
-Maintain a clear pathway free of obstacles, initiated 7/25/23;
-Resident needed a safe environment: floors free from spills and/or clutter; adequate, glare-free light; a working and reachable call light, the bed in a low position at night; side rails as ordered, handrails on walls, and personal items within reach, initiated 7/25/23;
-Bed in lowest position, initiated 11/13/23; and
-Bed in low position, initiated 1/22/24.
-However, observations on 3/7/24 and 3/10/24 revealed interventions, such as the bed in the lowest position and an uncluttered pathway, were not being implemented (see below) and the investigation revealed Resident #12's refusal of interventions was not documented nor her care plan updated.
D. Staff Interviews
The DON was interviewed on 3/11/24 at 10:19 a.m. The DON said a clear pathway meant Resident #12's room should be cleared of items so the resident was able to ambulate safely in her room. The DON said the resident should have a clear space next to her bed so the resident could safely get to her wheelchair and walker to use them if needed. The DON said the bed in low position meant the bed should be in the lowest position while the resident was in the bed.
CNA #1 and CNA #2 were interviewed on 3/11/24 at 1:20 p.m. CNA #1 said she used the kardex to see a resident's fall interventions. CNA #1 said Resident #12 should have a low bed when the resident was in bed, but Resident #12 did not like her bed low or her wheelchair and walker moved out of her reach. CNA #1 said Resident #12 was able to use the remote control for her bed and move her bed higher herself. CNA #1 said she had not reported Resident #12 refused to have her bed low to the nurse. CNA #1 said she was unsure if she was able to document in the resident's medical record her refusal of a fall intervention.
CNA #2 said when Resident #12 refused to have her bed put in a low position, she would provide education to the resident on the importance of her bed being in a low position. CNA #2 said Resident #12 did not like her bed in a low position and Resident #12 used the remote to move her bed higher herself. CNA #2 said she was unsure if she was able to document Resident #12's refusal of fall interventions in the resident's electronic medical record.
-However, there was no documentation in Resident #12's medical record that she did not like or refused to have her bed in a low position or assessments completed of the effectiveness of the fall interventions on Resident #12's comprehensive care plan.
The assistant director of nursing (ADON) #1 was interviewed on 3/11/24 at 1:30 p.m. The ADON #1 said if a staff member marked the low bed task complete, her expectation was that the bed was in a low position. ADON #1 said Resident #12 was able to adjust the height of her bed herself, however that was not included in the comprehensive care plan and had not been evaluated during the IDT fall reviews for effectiveness.
The DON was interviewed again on 3/11/24 at 1:54 p.m. The DON said she was not aware Resident #12 refused to have her bed in the low position and she expected the staff to mark the refusal in the fall prevention devices task history. The DON said Resident #12's comprehensive care plan should have been updated to include her refusals of fall interventions. The DON acknowledged that the resident's comprehensive care plan and medical record lacked the documentation to show the facility had evaluated the effectiveness of the current interventions to prevent further falls with injuries.
E. Facility follow up
The facility provided additional information regarding Resident #12 on 3/12/24 at 5:21 p.m.
The facility provided a general statement regarding fall interventions. The statement documented, At the time of the fall or incident the nurse is to put an intervention in place and document that intervention they determine may keep the resident safe: the next business morning when the IDT reviews the risk management they may determine the intervention one nurse put in place with limited information was not appropriate, and discontinue, change or add to that intervention.
-However, Resident #12's comprehensive care plan documented three separate fall care plans that included fall interventions with the intervention of a low bed initiated on 7/25/23 at the time of her admission to the facility, and added after Resident #12's falls on 11/12/23 and 1/20/24.
-The facility failed to provide documentation the fall interventions, specifically that of a low bed and clear pathway, were implemented and the effectiveness of these interventions were monitored to modify the care plan as necessary and discontinue or change the intervention.
Further documentation provided by the facility revealed in a note signed by the director of rehabilitation (DOR), Resident #12 was interviewed on 3/12/14 after the survey exit. The note documented Resident #12 reported she wanted the bed at mid height and did not want the bed in a low position.
-There was no documentation provided that the fall intervention of a low bed implemented on 7/25/23, and added on 11/12/23 and 1/20/24 was effective, or that the facility staff followed up with Resident #12 on her refusals of the fall intervention prior to 3/12/24, after the survey exit.
The facility also provided physical therapy progress notes for Resident #12. The physical therapy progress notes documented dates of service as 12/29/23 to 1/22/24.
-The physical therapy notes did not provide documentation regarding the implementation or effectiveness of the fall intervention for Resident #12's low bed.
The facility provided an undated care plan document that revealed no changes had been made to the care plan since the last care plan review (1/22/24).
-The documentation failed to provide updated information to Resident #12's refusals, the effectiveness of her low bed fall intervention, or effectiveness of maintaining a clear pathway in Resident #12's room.IV. Resident #19
A. Resident status
Resident #19, age [AGE], was admitted on [DATE]. According to the March 2024 CPO, diagnoses included stroke with paralysis of the left side, mild cognitive impairment and cognitive communication deficit.
The 1/11/24 MDS assessment documented the resident had a moderate cognitive impairment with a BIMS score of twelve out of 15. She required a wheelchair for mobility and had functional impairments to her upper extremities on one side. The resident was unable to walk and required one-person limited assistance with locomotion. She required maximal assistance with showering, dressing, toileting, transfers and bed mobility.
The assessment documented the resident had not had a history of falls and had not fallen in the six months prior to admission.
B. Observations
On 3/5/24 at 2:48 p.m., Resident #19 was sleeping in her bed.
-The call light was hanging on the floor out of the resident's reach and no fall mat was[TRUNCATED]
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0691
(Tag F0691)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interviews, the facility failed to ensure that residents who require colostomy services ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interviews, the facility failed to ensure that residents who require colostomy services receive such care consistent with professional standards of practice, the comprehensive person-centered care plan, and the resident's goals and preferences for one (#130) of three residents reviewed for colostomy care out of 53 sample residents.
Resident #130 was admitted to the facility on [DATE] with diagnoses of cognitive-communication deficit, anxiety disorder and with toxic megacolon (swelling and inflammation of the colon) that required a colostomy (a surgical operation in which a piece of the colon was diverted to an artificial opening in the abdominal wall to bypass a damaged part of the colon). Resident #130 required extensive assistance from staff for toileting and had a severe cognitive impairment according to the brief interview for mental status assessment.
The facility failed to consistently assist Resident #130 with the care of the colostomy. The facility failed to ensure she was provided with proper education to continue to independently care for the colostomy based on her assistance and cognitive functioning. The facility failed to have a personalized care plan for Resident #130 ' s colostomy to include education to be provided or the goal of becoming independent with the care of her colostomy.
Due to the facility's failures, Resident #130 was not provided with consistent care for her colostomy, which resulted in her bag often being full and smelling bad which embarrassed her and made her feel subhuman. The colostomy site was not consistently cleaned by staff and Resident #130 was not shown how to properly care for the site which caused it to be inflamed (red).
Findings include:
I. Professional reference
The National Library of Medicine Colostomy Care, updated on 5/28/23 and retrieved on 3/13/24 from: https://www.ncbi.nlm.nih.gov/books/NBK560503/ revealed in pertinent part,
The purpose of colostomy care was for skin protection and care for patient acceptance and to prevent stoma related complications. This activity outlines colostomy creation and care and highlights the role of the interprofessional team in evaluating and treating patients with this condition.
Managing a colostomy is generally done by a nurse or an entero-stomal therapist, but providers should be aware of the stoma's condition in case intervention may be required.
The 2-piece system consists of a base-plate with a removable ostomy bag attached to the skin. Although it is very durable and long-lasting, it requires an amount of skill to use, has a weaker adhesive, and does not fit very well.
Before starting the procedure, all supplies should be arranged, and handwashing and donning of gloves should be done. The used stoma bag should be first emptied of all content, and then the flange removed by gentle traction on the bag or flange towards the stoma with counter-traction on the skin. An adhesive remover may also be used. The stoma and parastomal area should be gently cleaned with water and dabbed rather than scrubbed without using soap. The stoma should be assessed and must be moist, above skin level, and pink to red in color, and the peristomal skin should be normal. The surgeon should be notified of any deviation from this. The stoma should be measured, or the previous measurement remembered, and the size should not be more than 1/16-1/8.
The peristomal skin should be dried appropriately to allow good seal formation. Adhesive pastes or powders may also be applied peristomally. The paper cover on the back of the flange is then removed with the border tape in place. It is then placed around the stoma and held for 1 to 2 minutes to create an adequate seal. If it is a 2-piece bag, it is clipped onto the flange. A belt may be applied around the abdomen and clipped to the sides of the flange to hold it in place. After this, safe disposal of the stoma bag, handwashing, and procedure documentation must be done.
II. Resident #130
A. Resident status
Resident #130, age [AGE], was admitted on [DATE]. According to the March 2024 computerized physician orders (CPO), diagnoses included toxic megacolon (swelling and inflammation of the colon), cognitive-communication deficit and anxiety disorder.
According to the 12/14/23 minimum data set (MDS) assessment, the resident was severely cognitively impaired with a brief interview for mental status (BIMS) score of six out of 15. She required extensive assistance from staff for toileting and supervision/touching assistance for personal hygiene. The resident had an ostomy.
B. Observations and resident interview
Resident #130 was interviewed on 3/7/24 at 9:28 a.m. The resident said she was required to change her colostomy bag. The resident said she did not always have the supplies to do the task. The resident said she would go days with her colostomy bag full and it would smell bad and was embarrassing. The resident said it made her feel subhuman. The resident said the nurses would not let her change the bag until it tore. The resident said she had cleaning supplies but was never shown how to use them. The resident said she would clean the site with a wet wipe or toilet paper. The resident said the staff showed her once but had never looked at the site after that. The resident said her skin around the stoma site was cherry red. The resident said she had been asking to change her bag since 10:30 p.m. the night before and they did not provide her with a bag until 9:20 a.m.
The resident's clothing, which she wore to bed, had leakage from the stoma site on them. The trash can in the bathroom had the used colostomy bag with fecal matter, toilet paper and wet wipes.
C. Record review
According to a 12/8/23 surgical discharge summary documented the resident had a total abdominal colectomy and ostomy.
According to the cognitive care plan dated 12/8/23 documented the resident had short-term memory loss. Interventions included the following: Use simple directive sentences. Give step-by-step instructions one at a time as needed to support cognitive function. The resident required supervision/assistance with all decision-making.
According to the colostomy care plan dated 12/11/23 documented the resident had a colostomy. Interventions included the following: staff should encourage good nutrition and hydration to promote healthier skin. Follow facility protocols for injury treatment. Keep the resident ' s skin clean and dry. Use a pressure-relieving/reducing mattress to protect the skin while in bed. The resident should avoid scratching and keep hands and body parts from excessive moisture. Keep
fingernails short.
-However, the care plan did not include the education procedure for the resident or the goal of becoming independent with the care of her colostomy.
According to the medication administration note dated 1/20/24 documented the resident was not available for education and assistance with learning to care for colostomy.
According to social services dated 1/23/24 documented if the resident moved in with her husband, she would need to be educated on emptying and placing back the colostomy bag.
III Staff interviews
Certified nurse aide (CNA) #3 was interviewed on 3/12/24 at 9:00 a.m. CNA #3 said the resident needed help with colostomy care. CNA #3 said the resident was not discharged due to her inability to perform colostomy care independently.
Licensed practical nurse (LPN) #1 was interviewed on 3/11/24 at 10:37 a.m. She said the resident performed her colostomy care by herself. LPN #1 said the nursing staff educated the resident on proper colostomy care. LPN #1 said the nursing staff did not have a standard way to perform education or return demonstration. LPN #1 said the tasks in the treatment administration record were reminders for staff to ask the resident if she had performed the tasks.
The director of nursing (DON) was interviewed on 3/11/24 at 3:14 p.m. The DON said individuals who perform colostomy care should be assessed to ensure the resident performed the task safely. The DON said nurses performed the colostomy care because the certified nurse aides (CNAs) were not qualified to accomplish the task. The DON said the nurse staff should continue to oversee the colostomy care. The DON said the nursing staff did not have a standard education plan for educating residents about colostomy care. The DON said the resident needed to be able to perform colostomy care to be discharged safely. The DON said the resident should not use toilet paper to clean her stoma site. The DON said the resident was able to communicate her needs clearly and accurately. The DON said the colostomy bag should be emptied when it was full. The DON said the staff should bring the resident supplies when the resident asked for them. The DON said there would be no leakage if the bag was placed properly.
IV. Facility follow-up
The NHA provided the following information post survey on 3/12/24 at 5:29 p.m.
It read in pertinent part,
According to the interdisciplinary team (IDT) care plan review team meeting, dated 3/8/24, the resident said she could perform colostomy care; however the IDT team said the resident continued to require oversight from staff.
-The IDT meeting confirmed that the resident continued to require oversight from staff. In addition, according to the MDS assessment (see above) she required extensive assistance from staff.
According to the BIMS assessment dated [DATE], the resident scored 15 out of 15.
-The facility changed the residents BIMS score from a six (severe cognitive impairment) out of 15 to a score of 15 (cognitively intact) out of 15 after the survey.
A signed document dated 3/12/24 from Resident #131 outlining the steps required to perform colostomy care and the resident acknowledged that she understood and could perform these steps.
-However, this had not been completed prior to the survey and the document did not include a demonstration back from the resident.
A progress note dated 3/12/24 documented the resident was able to complete the return demonstration of colostomy care.
-However, there was no documentation during or prior to the survey that the resident was able to complete colostomy care with return demonstration.
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to ensure one (#26) of three out of 53 sample residents...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to ensure one (#26) of three out of 53 sample residents received the care and services necessary to meet their nutrition needs and to maintain their highest level of physical well-being.
Resident #26 displayed slurred speech, confusion, and left sided weakness resulting in an admission to the hospital on 1/17/24. It was concluded he had suffered from a stroke and was readmitted to the facility on [DATE].
On 1/21/24, the resident weighed 161.9 pounds (lbs). On 2/19/24, a month later, Resident #26 weighed 143.3 lbs. which was a 11.49% weight loss and a difference of 18.6 lbs.
On his next weight on 3/7/24 (during the survey), the resident weighed 137.6 lbs. which was a 3.98% loss and a difference of an additional 5.7 lbs with a total of 18.6 lbs and 15.02% weight loss.
According to the change of condition minimum data set (MDS) assessment dated [DATE], the resident required maximum assistance with eating. The MDS revealed the resident relied on the staff for more than 50% of the task of eating. The resident was participating in speech and occupational therapy to improve his oral intake and functional ability to eat. Education was provided to the staff caring for him on techniques and risks for the resident to improve his oral intake.
Based on observations and interviews, it was determined the staff were not consistently providing the resident the level of assistance required according to his functional limitations and this contributed to his significant weight loss.
Findings include:
I. Resident #26
A. Resident status
Resident #26, age [AGE], was admitted to the facility on [DATE]. According to the March 2024 computerized physician's orders (CPO), diagnoses included diabetes mellitus type II, dementia, and heart disease.
The 1/24/24 MDS assessment showed the resident had moderate cognitive impairments with a brief interview for mental status (BIMS) score of twelve out of 15. The resident required maximum assistance with personal hygiene and eating. The resident required total assistance with bed mobility, toileting, dressing, showering, and transfers.
The resident had an impairment to one side of his body causing functional limitations.
The resident had a swallowing disorder with loss of liquids/solids from his mouth when eating, coughing and choking during meals, and complaints of pain or difficulty with swallowing.
B. Resident observations
The resident was observed on 3/5/24 at 12:25 p.m. in the dining room of the secured unit. Certified nurse aide (CNA) #11 provided the resident with a mechanically altered meal. The plate was placed in front of the resident but no staff members sat down with the resident. The resident was able to lift a regular cup of fluids and drink after a lot of effort with his right hand.
The occupational therapist (OT) sat down with the resident at 12:33 p.m. and adjusted his clothing protector. She left the table at 12:34 p.m. to locate a cup of ice cream for Resident #26.
The resident kept trying to get the attention of the staff by saying excuse me several times. CNA #8 sat down with the resident at 12:36 p.m. and assisted him one spoon of his lunch.
The OT returned at 12:37 p.m. and provided the resident with a cup of ice cream. The resident displayed left sided weakness when trying to lift the ice cream cup in front of him. He was able to feed himself ice cream with his right hand and hold the cup with his left hand while OT provided encouragement and cues to the resident. The OT left the table at 12:38 p.m.
CNA #11 sat down at the resident's table at 12:38 p.m. and assisted the other resident sitting at the table with his meal.
The speech therapist (ST) came at 12:41 p.m. and was providing instruction to the staff to remind the resident to clear his throat when eating and take sips of fluids in between bites of food. ST left at 12:46 p.m.
During the continuous observations, the resident coughed three times while eating his ice cream. The staff did not respond when the resident coughed.
CNA #8 came at 12:28 p.m. and asked the resident if he was done with his lunch. The CNA took the plate away and scrapped it in the trash. He was then taken to the common area at 12:49 p.m.
During the meal, the resident was observed to have drank three cups of fluids, ate one bite of his lunch plate, and completed one cup of ice cream.
Resident #26 was observed on 3/6/24 at 12:33 p.m. in the dining room of the secured unit. The meal was placed in front of the resident at 12:40 p.m. The resident attempted to lift his right arm to the plate and struggled when he got his arm caught under the table. The resident called out to CNA #5 stating I need help at 12:40 p.m. The CNA walked past the resident and did not acknowledge him.
At 12:43 p.m. Resident #26 called out to CNA #5 again for assistance and CNA #5 sat down with the resident. The resident was able to get his arm from under the table and the CNA provided the resident with a cup of ice cream. Once the resident began eating the ice cream independently, CNA #5 left the table at 12:44 p.m.
At 12:49 p.m the resident was able to get one spoon of food from his meal plate into his mouth after several attempts. The resident still had fluids in his mouth he had not swallowed when he put the food into his mouth.
At 12:53 p.m., the resident saw CNA #5 and requested assistance. CNA #5 sat down and assisted the resident. The resident was cooperative and when he wanted another bite, he opened his mouth freely. Twice CNA #5 tried to put food into the resident's mouth while he was still chewing and CNA #5 was looking away. Both times, the resident put his hand up to prevent the CNA from putting food into his mouth. The CNA did not speak to the resident, provide encouragement or cueing during the meal. The CNA assisted the resident three spoons of food between 12:53 p.m. and 12:58 p.m.
After the resident put his hand up the second time, the CNA stopped feeding him. The CNA left the table at 12:58 p.m. At 1:00 p.m., CNA #8 took the resident's plate and scraped it in the trash.
C. Record review
The ADL comprehensive care plan revised on 9/16/19 revealed the resident had self care deficits related to a history of falls, dementia, and physical limitations. Interventions initiated on 3/7/24 (during survey) included cueing and one-on-one assistance for eating.
The nutrition care plan initiated 1/21/24 revealed the resident had a nutrition problem related to a new stroke and dysphagia (difficulty swallowing). The resident had triggered a significant weight loss and required a mechanically altered diet related to chewing/swallowing difficulties. The resident had difficulty feeding himself at times related to a stroke affecting his non-dominant left side. Interventions initiated 3/7/24 (during survey) included to provide vanilla ice cream and mildly thick liquids during meals and occasionally assist/cue with eating.
-The care plan did not indicate the resident refused meals or had unavoidable weight loss.
The March 2024 CPO revealed the following physician orders:
Speech therapy (ST) evaluate and treat- ordered on 1/20/24;
Occupational therapy (OT) evaluate and treat- ordered on 1/20/24;
Physical therapy (PT) evaluate and treat- ordered on 1/20/24;
Regular diet, minced and moist, mildly thick with vanilla ice cream at all meals- ordered 3/7/24 (during survey); and
Boost (supplement drink) high calorie- three times a day- ordered 3/8/24 (during survey) - this was the only nutritional supplement ordered for the resident while he was experiencing significant weight loss since his readmission back to the facility.
A review of progress notes dated 2/12/24 to 3/11/24 revealed:
NP progress note dated 2/12/24 revealed the resident had a recent stroke 1/17/24. The resident was at weight loss/malnutrition risk. He was being followed by the registered dietitian (RD) for nutritional supplement recommendations. The resident had a diagnosis of dysphagia and staff were to monitor for difficulty swallowing and signs of aspiration.
NP progress note dated 2/19/24 revealed the resident was on a diabetic diet, minced and moist with mildly thick liquids. The NP documented weight loss was likely expected and unavoidable due to the disease progression, multiple comorbidities, and sporadic intakes (eating). If weight loss continued, it was suggested to consider a hospice evaluation and referral.
-However, according to the NP interview (see below), the NP was not aware the nutritional interventions for his weight loss were being consistently provided.
NP progress note dated 2/28/24 revealed the resident had failed to thrive since the stroke. Oral intakes were less than 25% and to consider hospice if weight loss continued.
NP progress note dated 3/4/24 revealed the resident continued with poor oral intakes and nutritional guidance was provided by the RD. It was suggested to consider hospice for the resident.
-NP notes failed to reveal the NP was aware the level of assistance required for intakes was not being consistently provided to mitigate weight loss and failure to thrive.
Resident weights reviewed from 1/21/24 to 3/7/24 revealed:
1/21/24 161.9 lbs. was the resident's weight immediately after the stroke.
1/29/24 156.2 lbs. which was a 3.52 % loss.
2/7/24 150.0 lbs. which was a 3.97 % loss.
2/12/24 143.8 lbs. which was a 4.13 % loss.
2/19/24 143.3 lbs. which was a 0.35 % loss.
3/7/24 137.2 lbs. which was a 3.98 % loss.
From Resident #26's readmission to the facility on 1/21/24 to 3/7/34 (during the survey process), the resident lost a total of 18.6 lbs and 15.02% weight loss.
Nutrition assessment dated [DATE] revealed the resident would be trialed on a scoop plate. Intake was 0-50% and the resident required assistance with meals.
-It did not include any other nutritional interventions to prevent further loss of weight.
A review of the resident's medical record did not reveal any additional nutritional assessments since his continued significant weight loss.
Daily skilled progress notes dated 3/6/24 revealed the resident had active symptoms of dysphagia and complaints of difficulty or pain with swallowing. He held food in his mouth/cheeks or residual food in mouth after meals. He coughed or choked during meals or when swallowing medication. Nutritional approaches include mechanically altered diet and thickened liquids.
-Condition follow up progress note dated 3/6/23 revealed current conditions: resident not eating 50% of meal, or not drinking 50%.
Physical therapy notes dated 1/22/24 revealed the resident had been referred post stroke. His prior level of ADL functioning was independent and currently was maximum assistance for ADLs.
A review of occupational therapy notes dated 1/23/24 to 3/11/24 revealed:
Occupational therapy notes dated 1/22/24 revealed the occupational therapist (OT) provided the resident with assistance for self-eating tasks. The RN was provided education by OT to provide the resident with one-on-one staff assistance with eating tasks at all times.
Occupational therapy notes dated 1/23/24 revealed the resident required one-on-one staff assistance for self feeding.
Occupational therapy notes dated 1/24/24 revealed the resident required moderate assistance to complete self-eating and drinking tasks. Education was provided to the RN on techniques to promote the use of the left upper extremities (arm/hand) as able with increased cues.
Occupational therapy notes dated 1/25/24 revealed the resident completed the self feeding task with OT assistance with initiation of positioning of left upper extremity and hand over hand to initiate grasp on the cup while using utensils in right upper extremity. The resident required verbal, visual, and tactile cues. Education was provided to the RN and CNA staff via a visual demonstration on techniques. The staff verbalized understanding of the education.
Occupational therapy notes dated 1/31/24 revealed the resident completed the self feeding and drinking task with verbal, visual, and tactile cues for continuum of task. RN and CNA staff were educated to incorporate left upper extremity throughout tasks via facilitating grasp onto plates and cups as well as having left upper extremity positioned into immediate midline (chest area) positioning with tasks.
Occupational therapy notes dated 2/1/24 revealed the resident completed the self feeding and drinking task with overall moderate assistance. Education was provided to staff on proper wheelchair positioning and set up of bilateral upper extremities with a focus on grasping cups, plates, and bowls with his left hand.
Occupational therapy notes dated 2/12/24 revealed the resident was noted with increased oral intake of food and completed the self feeding and drinking task with minimal assistance. Education was provided to the RN and CNA staff on positioning modifications and setup for self feeding and drinking throughout the meal.
Occupational therapy notes dated 2/13/24 revealed the resident required minimal assistance with maximum verbal cues for self pacing during eating and drinking tasks. The resident tended to eat and drink with increased speed and overall decreased safety awareness. The RN was present and aware of intermediate coughing and recommendations for one-on-one staff assistance with alternating the residents food and liquid intake at a slower pace.
Occupational therapy notes dated 2/15/24 revealed the resident completed self feeding and drinking tasks with minimal assistance and maximum assistance for verbal, visual, and tactile cues for sequencing and self safe pacing throughout.
Occupational therapy notes dated 2/29/24 revealed the resident was able to complete the self feeding tasks while sitting in his wheelchair at the tabletop. The resident was able to scoop and transport food to his mouth with verbal and visual cueing to initiate the task and the resident was able to attend self feeding task following cueing to improve self eating and nutrition.
Occupational therapy notes dated 3/5/24 (during survey) revealed the resident completed the self feeding and drinking task with multiple trials. Overall minimal assistance provided with hand over hand to initiate grasp onto bowl with hand left hand to complete task with right upper extremity for feeding. Increase time required for cueing for attention to task and safe sequencing.
Occupational therapy notes dated 3/7/24 (during survey) revealed education was completed with RN, CNA, and memory care staff with training on recommendations for one-on-one staff assistance with meals for cueing. The staff were educated on the resident's ability to physically complete self feeding tasks with use of his right upper extremity with recommendations to incorporate/facilitate grasp of left upper extremity onto plates and bowls throughout the meal. It was recommended by OT for staff to encourage the resident to complete eating independently as he is able to. However, if the resident is fatigued and not able to complete the task on his own, staff are to provide assistance. The staff are to encourage the resident to eat at a slower pace with smaller bites while checking occasionally for pocketing (storing food inside mouth and not swallowing.) The staff verbalized understanding of education with visual demonstration provided.
A review of speech therapy notes dated 1/23/24 to 3/11/24 revealed:
Speech therapy notes dated 1/23/24 revealed the resident had been started on minced and most texture food with mildly thick liquids. For meal tasks, the resident successfully responded 55% of the time with therapeutic attempts and 75% of the time if given tactile cues and visual aides during meal.
Speech therapy notes dated 1/26/24 revealed the resident required moderate to maximum cueing to remain attentive to meal tasks. The resident ate rapidly using large bites and talked with food in his mouth. Exhibited coughing after swallowing 50%-60% of the time.
Speech therapy notes dated 2/13/24 revealed the resident would leave his drinking cup tipped at his mouth for several seconds and required maximum cueing to complete follow through of the drinking task. There had been a positive impact on drinking when a spouted cup (a cup with a lid and a spout to drink out of to decrease fluid flow) was presented.
Speech therapy notes dated 2/14/24 revealed the resident completed more efficient swallowing of mildly thick liquid drinking tasks when intake was provided by on-one-on staff in a quiet environment.
Speech therapy notes dated 2/21/24 revealed the nurse had reported to the ST the resident had episodes of choking on his own saliva when taking medications.
Speech therapy notes dated 2/26/24 revealed ST was to begin trialing a spouted cup.
Speech therapy notes dated 3/4/24 revealed the resident benefited when an adaptive cup with straw was used to assist with drinking
Speech therapy notes dated 3/11/24 revealed ST was working with the resident on identifying food items to add to the resident's diet to promote adequate nutrition.
III. Staff interviews
CNA #10 was interviewed on 3/6/24 at 9:16 a.m. She said Resident #26 needed staff to sit with him, prompt him and assist him to eat.
CNA #8 was interviewed on 3/6/24 at 9:36 a.m. She said Resident #26 needed staff to sit with him and prompt him to eat meals. He would feed himself independently sometimes but staff had to sit with him, cue, and prompt him. She said if the staff put a plate of food in front of him and walked away, he would not eat.
CNA #11 was interviewed on 3/6/24 at 9:51 a.m. She said Resident #26 required total assistance to include assistance from staff to eat his meals. She said he was not able to eat independently.
The registered dietitian (RD) was interviewed on 3/6/24 at 9:57 a.m. She said Resident #26 had a stroke recently and had swallowing difficulties. He required thickened liquids and had decreased intakes. The resident required a lot of help with eating to include cueing, prompting and assistance at times. The OT had tried a scoop plate and a cup and a lid to assist the resident with eating.
She said in order to monitor the effectiveness of feeding interventions, staff needed to weigh the resident weekly. The RD said she did not know why weekly weights were stopped 2/19/24. The RD said she put a boost supplement into place, however did not have any other documented nutritional interventions.
The ST and OT were interviewed on 3/6/24 at 10:10 a.m. The ST said she had been working with the resident to advance his diet from the current texture for resident preference. The resident had swallowing difficulties, was at risk for aspiration and weight loss.
The OT said she had instructed staff to put items in the resident's left hand for stability and to encourage him to use his right hand to utilize the utensils to feed himself. He currently needed one-on-one supervision for meals to include at minimum prompting to eat. The resident did not eat independently. She had provided education to the CNAs several times on how to provide the resident adequate eating assistance. Based on her assessment of the resident, he could benefit from therapy. Hospice was intended for residents who could not benefit or participate in therapy. The OT said to determine if a resident could no longer benefit from therapy, the facility needed to exhaust all interventions. To exhaust all interventions, the interventions needed to be tried as intended and on a consistent basis.
The director of nursing (DON) was interviewed on 3/7/24 at 10:52 a.m. She said Resident #26 had decreased oral intake since his stroke in January 2024. The DON had considered referring the resident for hospice but wanted to exhaust all possible interventions before referring them. The CNAs provided assistance to the resident during meals by encouraging, cueing or physically assisting him with a spoon. The DON said according to the staff, sometimes the resident would feed himself if the staff put his meal plate in front of him. The DON had not observed the resident during meals. The resident was weighed weekly and the DON was not aware the resident had not been weighed since 2/19/24. Speech therapy had been working with the resident on intake and swallowing difficulty but the DON did not know the interventions therapy had recommended for eating assistance. She did not know what interventions therapy had instructed the CNAs to use with the resident and if the CNAs had been consistently using the interventions. The physician had recommended hospice for the resident but the DON said she did not know if the physician knew the eating assistance interventions were not being followed consistently.
The NP was interviewed on 3/11/24 at 11:18 a.m. He said resident #26 recently had a stroke and had begun losing weight related to a failure to thrive. He said he was not aware there were eating assistance interventions that were not being used with the resident consistently. The NP said he had never observed the resident eating or drinking but had just assumed the staff were doing all available interventions.
He said he thought the resident was receiving the care and services required and still losing weight, however that was not the case based on the observations throughout the survey.
IV. Facility follow-up
On 3/13/24 at 3:32 p.m. an updated care plan was provided by the NHA. The documents were as follows:
The nutrition care plan revised 3/13/24 (after survey) revealed the resident had a nutrition problem related to a new stroke and dysphagia. The resident meet criteria for significant weight loss. Unavoidable noted due to comorbidities. Multiple interventions will still be attempted and in place.
-The facility identified the resident's significant weight loss as unavoidable, however based on the observations during the survey process, Resident #26 did not receive the care and services required to meet his nutritional needs. The facility failed to identify that the resident was not receiving the eating assistance he required while he continued to lose a significant amount of weight. The facility failed to put significant nutritional interventions into place, failed to conduct regular nutritional assessments and observations of the resident during meals and address his continued significant weight loss.
-No new interventions were put into place in the care plan.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to ensure residents retained the rights to their personal belongings f...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to ensure residents retained the rights to their personal belongings for two (#11 and #51) of five out of 53 sample residents.
Specifically, the facility failed to obtain Resident #11 and Resident #51's permission prior to searching and confiscating items from their rooms.
Findings include:
I. Facility policy and procedure
The Resident Rights policy and procedure, reviewed April 2023, was received from the nursing home administrator (NHA) on 3/11/24 at 4:21 p.m. It read in pertinent part, The resident has the right to be treated with consideration, respect, and full recognition of his or her dignity and individuality.
II. Resident #51
A. Resident status
Resident #51, age [AGE], was admitted on [DATE]. According to the March 2024 computerized physician orders (CPO), the diagnoses included heart disease, morbid obesity and chronic kidney disease.
The 11/24/23 minimum data set (MDS) assessment revealed the resident was cognitively intact with a brief interview for mental status score of 15 out of 15. She required partial/moderate assistance with personal hygiene, toileting, supervision with transfers and was independent with eating and bed mobility.
B. Observations and resident interview
On 3/5/24 at 11:30 a.m. registered nurse (RN) #3, who was wearing street clothes, was observed entering and exiting multiple resident rooms.
Resident #51 was interviewed on 3/5/24 at 2:09 p.m. She said a nursing staff member went through her drawers that morning without asking her permission. She said she did not know the nurse.
She said she had mentholatum cream (cream used to soothe sore muscles and joints) at her bedside that she self administered. She said the nursing staff member made her feel like a criminal because she had the mentholatum cream at her bedside.
She said the nurse did not ask her permission before removing the cream from her room.
III. Resident #11
A. Resident status
Resident #11, age [AGE] , was admitted on [DATE]. According to the March 2024 CPOs, the diagnoses included heart disease, type 2 diabetes mellitus (DM) and major depressive disorder.
The 1/16/24 MDS assessment revealed the resident was cognitively intact with a brief interview for mental status score of 15 out of 15. He required supervision with toileting, personal hygiene, transfers, set up assistance with eating and was independent with bed mobility.
B. Resident interview
Resident #11 was interviewed on 3/5/24 at 2:46 p.m. He said a nurse with blonde hair came into his room that morning and removed two tubes of athlete's fungal foot cream and a laxative pill that was lying on the counter. He said she went through his drawers without his permission.
He said he knew his rights and she should have asked for permission before opening and going through his drawers.
He said she removed the cream and pill without asking his permission.
IV. Staff interviews
Licensed practical nurse (LPN) #1 was interviewed on 3/11/24 at 10:14 a.m. She said all staff needed to obtain a resident's permission before searching a resident's belongings or drawers.
The director of nursing (DON) was interviewed on 3/11/24 at 3:10 p.m. She said RN #3 was the staff member who was going in and out of the resident's rooms on 3/5/24. She said consent should be obtained from the resident before any staff member was able to search resident belongings and drawers. She said resident's with medications at the bedside needed an order and an evaluation.
She said she would provide education with RN #3 regarding her interactions with the residents and not going through resident belongings without permission.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to ensure two (#6 and #56) of two residents reviewed for abuse out of ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to ensure two (#6 and #56) of two residents reviewed for abuse out of 53 sample residents were free from abuse.
Specially, the facility failed to prevent a resident to resident altercation between Resident #6 and Resident #56.
Findings include:
I. Facility policy
The Abuse Prevention policy, dated 7/11/21, was received from the nursing home administrator (NHA) on 10/12/23. It read in pertinent part:
The employees of the facility will take action to protect and prevent abuse and neglect from occurring within the facility by: Assess, care plan, and monitor residents with history of aggressive behaviors, behaviors such as entering other residents' rooms, self-injurious behavior, communication disorders, totally dependent on staff.
II. Resident to resident physical altercation between Residents #6 and #56.
A. Observations of a resident to resident altercation on 3/5/24 between Resident #6 and Resident #56
Resident #6 was observed on 3/5/24 at 3:00 p.m. approaching Resident #56 who was coming out of a resident room. Resident #6 pushed Resident #56 in the shoulder and Resident #56 reached out and grabbed the wrist of Resident #6. The two residents yelled at each other but the words were unintelligible. Two unidentified staff members approached the residents and got in between them.
The staff member (later identified as CNA #9) stood in front of Resident #6. While still looking at Resident #56, Resident #6 balled up his fists and held his hands up in a boxing pose. Another unidentified staff member (later identified as the activity assistant) redirected Resident #6 to another part of the unit and Resident #56 back to his room.
B. Facility investigation
Staff interviews provided by the facility on 3/6/24 at 10:45 a.m., revealed the activities assistant (AA) and certified nursing aide (CNA) #9 had been involved.
In the AA's statement, she wrote she was providing a hand massage and then heard loud voices. She got up and saw Resident #6 and Resident #56 getting into it and she separated the two residents. She denied seeing contact made between the two residents.
-The investigation failed to have the AA define what getting into it entailed.
CNA #9's statement documented she did not witness any incident between Resident #56 and Resident #6, despite the observations of CNA #9 being involved and separating both residents.
III. Resident #56 (victim)
A. Resident status
Resident #56, age [AGE], was admitted on [DATE]. According to the March 2024 computerized physician orders (CPO), diagnoses included stroke, vascular dementia, alcohol dependence in remission, and macular degeneration.
The 2/2/24 minimum data set (MDS) assessment documented the resident was moderately cognitively impaired with a brief interview of mental status (BIMS) score of ten out of 15.The resident used a wheelchair for mobility. He required maximum assistance from staff with personal hygiene, toileting, dressing, and showering. He required supervision with transfers.
It indicated the resident did not exhibit any behaviors during the assessment period.
B. Record review
The cognitive care plan, revised 2/10/23, revealed the resident had impaired cognitive functioning, decision making, and thought processes related to dementia. Interventions included identifying self at every interaction, keeping the resident's routine consistent, and providing psychosocial support by social services.
The behavior care plan, initiated on 3/6/24 (during the survey process), revealed the resident had the potential to demonstrate behaviors related to anger. Triggers for the resident were other residents expressing behaviors and getting too close to his personal space. Interventions included analyzing the circumstances for triggers and de-escalating, documenting behaviors and attempting interventions, and engaging the resident calmly when agitated.
A social service progress note dated 3/5/24 revealed the social services director (SSD) followed up with Resident #56 post altercation. The resident said he had a bad day, Resident #6 had entered his personal space and he did not like that.
A social services progress note dated 3/6/24 revealed Resident #56's roommate, Resident #6, had been moved to another room. Resident #56 told SSD he was sorry for the incident and he was only playing around.
IV. Resident #6 (assailant)
A. Resident status
Resident #6, age [AGE], was admitted on [DATE]. According to the March 2024 CPO, diagnoses included dementia, anxiety, and major depressive disorder.
The 1/22/24 MDS assessment documented that the resident had short and long term memory deficits, severe impairment in decision making, and was only orientated to people and places. The resident used a wheelchair for mobility. He required maximum assistance from staff with toileting, dressing, and showering. He required supervision with transfers, personal hygiene, and eating.
It indicated that the resident did not exhibit behaviors during the assessment period.
B. Record review
The cognitive care plan, revised 5/18/23, revealed the resident had episodes of delirium and confusion related to dementia. Interventions included identifying self at every interaction; observing environmental factors; and providing gentle redirection.
The behavioral care plan, initiated 8/18/23, revealed the resident had the potential to demonstrate behaviors such as agitation, physical aggression, and delusions related to major depression disorder. Interventions included monitoring the resident for increased anger, labile mood, agitation, feeling threatened by others, thoughts of harming someone else, and possession of objects that could be used as weapons. Staff to document behaviors and interventions.
The March 2024 CPO revealed the following physician orders:
Behavior monitoring of episodes of agitation and delusions- ordered on 6/16/23.
Behavior monitoring for episodes of self-isolation and irritability- ordered on 6/16/23.
-The March 2024 medication administration record (MAR) indicated that the resident did not exhibit any behaviors, however staff indicated that Resident #6 had behavioral concerns (see interviews below).
V. Staff interviews
CNA #7 was interviewed on 3/5/24 at 3:45 p.m. She said Resident #6 and Resident #56 had a history of verbal altercations, however she was unaware of any physical altercations.
CNA #9 was interviewed on 3/5/24 at 3:50 p.m. She said Resident #6 and Resident #56 always verbally fought with each other. Resident #56 did not like it when other residents got too close to him.
CNA #9 said Resident #6 had a history of going around the secured unit pushing other residents and getting close to other residents' personal space. She said Resident #6's behavior caused issues for other residents.
CNA #9 said she responded to the altercation on 3/5/24. She said did not witness Resident #6 push Resident #56 but did witness Resident #56 release Resident #6's wrist when she approached. She said she witnessed Resident #6 put his fists up. She said she re-directed both residents and prevented further escalation of the incident between the two residents.
CNA #9 said she did not report to the nurse or the abuse coordinator regarding the incident because she had not witnessed either resident hit the other resident.
Licensed practical nurse (LPN) #4 was interviewed on 3/5/24 at 3:54 p.m. She said she had not been notified by staff of an altercation between Resident #6 and Resident #56. She said Resident #6 had problematic behaviors toward other residents on the secured unit and said she was not surprised he had pushed Resident #56.
The nursing home administrator (NHA) was interviewed on 3/5/24 at 4:20 p.m. He confirmed he had received a report from LPN #4 regarding a resident to resident altercation between Resident #6 and Resident #56. He said CNA #9 should have made the report immediately.
The NHA was interviewed again on 3/6/24 at 10:30 a.m. He said the facility had started an investigation regarding the altercation between Resident #6 and Resident #56. Resident #6 had been moved to another room and the two residents were on frequent checks during the investigation. The NHA provided the occurrence number for the report made to the State Agency.
During the survey, the AA was unavailable for interview.
VI. Facility follow up
On 3/12/24 at 4:45 p.m. documents were provided by the nursing home administrator (NHA) via email. The documents were as follows:
Facility findings of physical abuse investigation. The facility concluded there was no abuse and unsubstantiated the incident. Through the internal investigation, staff interviewed denied witnessing physical contact between the two residents.
-The facility unsubstantiated the incident between Resident #56 and Resident #6, even though it was witnessed and reported to the NHA (during the survey process) that Resident #6 pushed Resident #56, Resident #56 grabbed Resident #6's wrist, and the residents continued to verbally attack one another.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0603
(Tag F0603)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observations and interviews, the facility failed to ensure that one (#19) of six residents out of 53 sam...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observations and interviews, the facility failed to ensure that one (#19) of six residents out of 53 sample residents were free from involuntary seclusion and were receiving the least restrictive approach for their needs.
Specifically, the facility failed to ensure Residents #19, residing on the secure locked unit, had the required documentation to justify such restrictions including documentation such as doctor orders, documentation reflecting secure/locked placement was the least restrictive approach possible and documentation the impact or reaction to the resident was assessed.
Findings include:
I. Facility policy
The Secure Unit policy, revised March 2024, was provided by the nursing home administrator (NHA) on 3/8/24 at 10:37 a.m. It read in pertinent part:
In order to place a resident into a secure environment, the facility shall ensure that all of the following requirements are met:
An evaluation team finds, based on available evidence, that:
a. The resident is a serious danger to self or others, or
b. The resident habitually wanders or would wander out of buildings and is unable to find the way back, or
c. The resident has a significant behavioral health issue that seriously disrupts the rights of other residents; and in all cases
d. Less restrictive alternatives have been unsuccessful in preventing harm to self or others.
A practitioner has authenticated the placement. Written findings and the factual basis for the placement are documented in the health information record. There shall be a designated team to evaluate placement of a resident in a secure environment. The team shall include, at a minimum, the director of nursing or designee, a social services staff member, the administrator or designee and an individual (with mental health or social work training as appropriate to the needs of the residents) who is not a facility staff member (independent reviewer).
II. Resident #19
A. Resident status
Resident #19, age [AGE], was admitted on [DATE]. According to the March 2024 computerized physician orders (CPO), diagnoses included stroke with paralysis of the left side, mild cognitive impairment, cognitive communication deficit and anxiety.
The 1/11/24 minimum data set (MDS) assessment documented the resident had a moderate cognitive impairment with a brief interview of mental status (BIMS) score of 12 out of 15. She had behaviors of verbal and physical aggression towards others. She did not have behaviors of wandering. She required a wheelchair for mobility and had functional impairments to her upper extremities on one side. The resident was unable to walk and required one-person limited assistance with locomotion. She required maximal assistance with showering, dressing, toileting, transfers and bed mobility.
B. Resident interview
Resident #19 was interviewed on 3/5/24 at 2:37 p.m. She said she did not like the unit she had been moved to because the staff did not allow her to have choices about when she ate, when she went to sleep or when she was able to take a shower. The unit doors did not open and the resident could not come and go to other parts of the building. She expressed feeling angry and confused as to why she had been moved to the unit she was on.
C. Record review
The comprehensive care plan, revised 1/8/24, revealed the resident had a self care deficit related to a stroke with one sided paralysis. The resident required assistance from staff to complete activities of daily living (ADL) to include one to two person staff assistance with toileting, transferring, bed mobility, and dressing. Interventions included evaluation and treatment from physical, occupational, and speech-language therapy.
The resident had a diagnosis of depression with a history of sadness, decreased appetite, and increased fatigue. Interventions included to arrange for psychological consultation as indicated and encourage the resident to express her feelings.
-The care plan did not include wandering or elopement behaviors or interventions attempted prior to a secure unit placement.
The March 2024 CPO revealed the following physician orders:
Admit to secure memory care unit effective 2/23/24-ordered on 3/7/24 (during the survey).
-No physician orders were located for placement on the secure unit prior to the survey. No behavior tracking was located to monitor for wandering or exit seeking behaviors.
An elopement evaluation dated 1/5/24 revealed the resident was physically immoble with intermittent confusion. She had no history of elopements and did not make statements regarding a desire to leave the facility.
-No other elopement evaluations were located in the resident's medical record.
A review of the hospital referral for placement dated 1/5/24 failed to reveal the resident had a history of elopements or wandering in the community. The resident had been living alone in the community with limited social support outside of a home health care agency. She suffered two falls at home and was admitted to the hospital. A St. Louis University Mental Status (SLUMS) examination assessment was done at the hospital and the resident had scored a six out of 30 indicating the probability of a diagnosis of dementia. She was oriented only to herself during the hospital stay. The hospital physician indicated a suspicion of dementia, however a neurological (the specialized field of diagnosing and treating disorders of the brain and nervous system) follow up was needed. The hospital referral included an evaluation of the resident including her condition at time of admission on [DATE]. The nurses indicated the resident presented with poor hygiene and signs of diminished care as well as signs and behaviors of suspected dehydration.
A SLUMS examination assessment for cognitive impairments was administered at the facility with the resident on 1/8/24. The resident could not recall date, complete mental subtraction, list multiple animals within a minute, count serial numbers backwards, correctly draw a clock with accurate time, identify shapes, or recall all the details of a story after a brief delay. She scored a ten out of 30 indicating the probability of a diagnosis of dementia. This score was an improvement from her previous SLUMS on 1/5/24.
-This SLUMS assessment had been administered three days after the resident admitted to the facility after a hospitalization and was not repeated after the resident acclimated to the new living environment.
A physician authorization for the special care unit dated 2/23/24 indicated the resident habitually wandered and would not be able to find her way back if she wandered out of the building and least restrictive alternatives had been unsuccessful in preventing harm to self or others. The authorization form indicated the resident was not a danger to herself or others and did not have serious behavior concerns disrupting the rights of other residents. The authorization form had not been signed by the physician.
The preadmission secure unit evaluation and review form dated 2/23/24 revealed the resident had displayed exit seeking behaviors and wandering without intent. The section describing the least restrictive interventions attempted and why the attempts were unsuccessful only indicated the resident was wandering. The NHA, the social services director (SSD) and director of nursing (DON) had signed the form; however, the independent reviewer had not signed the form.
Occupational therapy notes dated 2/29/24 revealed the resident stated to the therapist she wanted to return to where she came from (the prior unit). The resident displayed increased agitation and continued verbalizations of desiring to return to the long term care unit.
A speech therapy (ST) evaluation and plan of treatment dated 3/4/24 revealed the resident was recently transferred to the secure memory care unit due to an increased risk of elopement. At the time of the evaluation, the resident could understand others and could make herself understood. She was able to follow one-step directions and was cooperative. A cognitive assessment revealed the resident had a moderate cognitive decline. An interpretation by the evaluator revealed the resident had decreased knowledge of current/recent events, reduced memory of personal history, and an inability to complete complex tasks. According to the interpretation, there was the possibility for the resident to retain the capacity for new learning with the use of visual aids and recognition of familiar people/places/and routines.
The facility census of admissions and room moves was reviewed on 3/5/24 at 2:10 p.m. The resident was admitted on [DATE]. The resident was moved to a different room on 1/11/24. The resident was moved again to a different room on 1/18/24. The resident was then moved to the secure memory care unit on 2/23/24.
Progress notes were reviewed from 1/5/24 to 3/11/24 revealed:
A nurse practitioner (NP) progress note dated 1/8/24 revealed the resident admitted to the facility after a fall at home. The resident was admitted for medical management and rehabilitation. The resident had intermittent confusion and was alert to herself and situations.
A social services summary progress note dated 1/12/14 revealed the resident exhibited short term memory loss as evidenced by disorientation of time and difficulty with recall abilities. Her BIMS score was a twelve out of 15. Her speech was clear and she was able to make her needs known to others.
A daily skilled progress note dated 1/16/24 revealed the resident showed intermittent confusion but responded well to verbal commands.
A social services progress note dated 2/23/24 revealed the social services staff contacted the resident's representative to consent to the resident being moved to the secure memory care unit temporarily for the resident's safety.
A nursing progress note dated 2/25/24 revealed the resident was eating poorly due to not being able to pick and choose what she would like to eat.
A behavior progress note dated 3/1/24 revealed during nurse rounds, the resident refused to use the restroom or have her brief changed. The resident grabbed the certified nurse aide (CNA) by the wrist and squeezed leaving a bruise. The resident displayed agitation and stated to the nurse she did not like the unit. She could not pick her own meals, she had to do what the staff told her to do, and verbalized hating being on the unit. The resident was redirected to an activity with assistance from another CNA.
A NP progress note dated 3/2/24 revealed the resident was residing in the secure memory care unit due to the need for closer supervision and for safety.
A social services progress note dated 3/7/24 (during survey) revealed the social services director (SSD) conducted a psychosocial check in with the resident. The resident told the SSD the unit was fine and nice. The resident did not voice any concerns.
-No further progress notes were located demonstrating exit seeking behaviors or least restrictive alternatives attempted and failed.
III. Staff interviews
Registered nurse (RN) #2 was interviewed on 3/11/24 at 10:40 a.m. She said Resident #19 had behaviors of verbal aggression towards staff but no physical behaviors. The resident had not made attempts to elope from the secure unit since admitting. RN #2 knew the resident when she resided on the other unit of the facility. The resident had several room moves but RN #2 did not know why. The resident had confusion where her room was and had approached the double doors leading to the assisted living section of the facility but had not tried to exit. RN #2 said the resident frequently expressed feeling unhappy and restricted on the secure memory care unit.
CNA #11 was interviewed on 3/11/24 at 10:52 a.m. Resident #19 has not made attempts to elope since coming to the secure unit. CNA #11 was told the resident had tried to leave when living on the other side of the facility in the long term care unit, but CNA #11 said she had only ever seen the resident approach the double doors but not attempt to leave them.
The NP was interviewed on 3/11/24 at 11:18 a.m. He said Resident #19 would benefit from the programs and increased interaction on the secure unit. He did not know why she was initially moved over to the secure unit. The NP said he had not personally observed any exit seeking or wandering behaviors from the resident and said she would not be able to go very far in a wheelchair.
The SSD and assistant nursing home administrator (ANHA) were interviewed on 3/11/24 at 1:01 p.m. The SSD said if a resident was determined to meet criteria for the secure memory care unit, a physician authorization form, a consent from the responsible party, and a physician's order for placement were obtained prior to the resident admitting to the secure unit. The facility worked with an external behavioral health agency to provide the independent reviewer for the evaluation process. The independent reviewer was part of the preadmission evaluation of the resident. The criteria for an existing resident to move to the secure memory care unit would be wandering into other resident's rooms, exit seeking behaviors, as well as behaviors disruptive to other residents. The SSD said she did monthly audits on the documents required for secure unit placement for all the residents residing on the unit. She did not have documentation of the audits.
The SSD was aware the resident had initially moved from the rehabilitation part of the facility to the long term care side before moving to the memory care unit but did not know how many times she was moved total between 1/5/24 and 2/23/24. She was not aware if this impacted the resident's behaviors or cognition. The SSD said it was noted the resident had gone towards the exit doors leading from the long term care side to the assisted living part of the facility. This was the determination for movement to the secure memory care unit. She did not know what least restrictive interventions had been attempted before placement.
The ANHA was not aware of the state or facility requirements for secure unit placement. She said preadmission evaluations needed to be signed by all managers involved and the independent reviewer. The physician authorization for placement was signed by the physician. These documents were signed within seven days of a resident's moving to the secure unit. The responsible party consent and physician order were in place before moving onto the secure unit.
The DON was interviewed on 3/11/24 at 2:56 p.m. A physician order, responsible party consent, documentation of evidence of wandering, and a preadmission evaluation are in place prior to admission to the secure memory care unit. Least restrictive interventions should be attempted first and documented. Interventions included assessing the resident for intentions with wandering and for unmet needs provoking wandering or exit seeking behaviors. Administration had received an email documenting Resident #19 was observed near the double doors leading from the long term care unit to the assisted living area. The DON did not know if there was a wandering risk assessment completed or if there was documentation in the chart of wandering behaviors.
The NHA was interviewed on 3/11/24 at 3:32 p.m. He provided an email dated 2/23/24 from the assistant director of therapy revealing the resident had been found trying to leave the double doors leading from the long term care unit to the assisted living area. He provided another email from the social services staff dated 2/23/24 revealing the resident was to be moved to the secure memory unit due to risk of elopement. The resident was moved immediately after this incident. The NHA did not know if additional or alternative interventions were tried prior to admitting to the secure unit. He did not know if the SSD or social services staff had assessed the resident to determine the motivation or intent, if there were unmet needs, or if the secure memory care unit was the only appropriate intervention available.
IV. Facility follow up
On 3/12/24 at 4:45 p.m. documents were provided by the NHA:
The previously reviewed note from the referral packet from the hospital dated 1/2/24 indicating the resident had a SLUMS score of six out of 10.
The previously reviewed facility SLUMS assessment dated [DATE] with a score of 10 out of 30.
A care plan review dated 2/22/24 revealed the resident had short term memory loss and difficulty with memory recall. The resident had been having difficulty locating and identifying where her room was in the long term care unit.
-The note did not reflect the census which showed the resident had three room changes between 1/5/24 and 1/18/24 on the long term care unit.
A CNA alert charting note dated 2/22/24 at 10:00 a.m. documenting the resident had tried to leave the health care center (long term care side of building) double doors and the CNA and therapy staff redirected her.
The preadmission secure unit placement evaluation form from 2/23/24 with a signature from the independent reviewer but the date remained 2/23/24.
-The form reviewed during the survey was dated 2/23/24 without independent reviewer signature.
A social services progress note dated 2/26/24 marked as a late entry revealing the SSD had reached out to the resident's son to advise him she would be the resident's new social worker on the secure memory care unit. The representative was agreeable to the move and had no concerns.
-This note was not located in the progress notes when reviewed on 3/11/24 (during survey) and there was no date/time stamp for the late entry.
A physician progress note dated 3/5/24 (during survey) marked as a late entry revealing the resident was more mobile in her wheelchair and rarely found in her room. She had been wandering to the outside of the facility at times and had been unable to find her way back. She had asked the provider during the visit where she was supposed to go, indicating to the provider she did not know where her room was.
-As of 3/5/24, the resident had moved four times since admission on [DATE] and was already residing in the secure memory care unit.
-This note was not located in the progress notes when reviewed on 3/11/24 (during survey) and there was no date/time stamp for the late entry.
An interdisciplinary team progress note dated 3/12/24 revealing the resident was reviewed and continued to meet criteria for secure memory care unit placement.
A behavior progress note created on 3/12/24 backdated 2/23/24 revealing the occupational therapist had redirected the resident away from the double doors leaving the long term care unit. She stated to the therapist she wanted to get out of here.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to provide and document sufficient preparation and orientation to one...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to provide and document sufficient preparation and orientation to one (#191) of three out of 53 sample residents to ensure a safe discharge from the facility.
Specifically, the facility failed to provide evidence and documented confirmation that home health services were arranged upon Resident #191's discharge from the facility, per physician orders.
Findings include:
I. Facility policy and procedure
The Discharge Planning Process policy and procedure, revised December 2023, was provided by the nursing home administrator (NHA) on 3/11/24 at 4:09 p.m. It read in pertinent part, The discharge process should effectively transition them to post-discharge care, and minimize clinical or other factors which are related to the possibility of a readmission.
The facility's discharge planning process shall provide and document sufficient preparation.
II. Resident #191 status
Resident #191, age [AGE], was admitted on [DATE], and discharged on 2/4/24. According to the February 2024 computerized physician orders (CPO), diagnoses included cellulitis (bacterial infection of skin) of right lower limb, type 2 diabetes mellitus, and acquired absence of left leg below the knee (amputation).
The 2/4/24 discharge minimum data set (MDS) assessment revealed the resident was cognitively intact with a brief interview for mental status (BIMS) score of 15 out of 15. She required substantial/maximal assistance with toileting hygiene, shower/bathing, upper and lower body dressing, personal hygiene, and transfers lying to sit. She was dependent on the use of a manual wheelchair for mobility.
A. Resident representative interview
The resident's representative (RR) was interviewed on 3/12/24 at 1:37 p.m. She said that Resident #191 was discharged home alone on 2/4/24 without home health (HH) services in place. The RR said she was not aware that the HH company did not accepted the facility's referral until the day after Resident #191 had been discharged (2/5/24).
The RR said on the day (2/4/24) of Resident #191's discharge, the nurses had advised her that home health services were not set up, only a physician's order. RR said she received an email from the social services assistant (SSA) that morning saying she had sent a referral to a home health agency for PT (physical therapy), OT (occupational therapy, and RN (Registered nurse).
The RR said the SSA had failed to make personal contact with the home health company to confirm the resident had been accepted. The RR said the facility did not follow physician orders to provide home health services at discharge. She said the resident especially needed a home care nurse to provide wound care to the right calf. The RR said she had to perform the wound care even though she had no medical training or education from the facility.
The RR said on Tuesday (2/6/24), two days after the resident discharged home, Resident #191 had a fall and sliced her right leg. The RR said that emergency services had taken Resident #191 to the emergency room where she had to have eight stitches.
The RR said without home health care confirmed and in place, it was an unsafe discharge for Resident #191. The RR said the SSA did not ensure a safe discharge and placed Resident #191 in an extremely unsafe situation.
The RR said she had to look for a home health agency on her own. She said that the agency started care on 2/19/24. The RR said Resident #191 was home without home healthcare for 15 days.
B. Record review
The discharge care plan, initiated 11/12/23, revealed the resident planned to return home where she lived alone in an apartment. The interventions included encouraging the resident to discuss feeling and concerns with an impending discharge; establishing a pre-discharge plan with the resident, family/caregivers; evaluating the progress and revising the discharge plan as needed; evaluating the resident's motivation to return to the community; evaluating and recording the resident's abilities and strength, with family/caregivers/IDT (interdisciplinary team); determining gaps in the resident's abilities which will affect discharge; making arrangements with required community resources to support independence post-discharge; and preparing and giving the resident, family member and caregiver contact numbers for all community referrals.
A review of the CPOs dated 1/30/24 revealed Right posterior calf wound. Cleanse with wound cleanser, apply collagen powder to wound bed, cover with foam dressing; change three times per week.
A review of the PT home evaluation note on 1/31/24 revealed, Reviewed with team patient's improved level of functional mobility but need for some home health services to optimize safety and carryover.
A review of the OT home evaluation note on 1/31/23 revealed, Reviewed with team patient's improved level of functional mobility but need for home health services to ensure safety and carry over in the home.
A review of the CPOs dated 2/1/24 revealed Discharge is scheduled for 2/4/24 to return home. Home health care will provide PT, OT, RN. Send with belongings.
An email sent to the RR from the SSA on 2/4/24 at 9:07 a.m. documented, Referral sent to (company name) Home Health Care, will provide PT, OT, RN for home health care needs.
-However there was no documentation provided that the home health company had received, accepted and was able to staff the referral.
A review of a text message sent from the RR to assistant nursing home administrator (ANHA) on 2/4/24 at 9:58 a.m. revealed, Resident #191 is set to discharge at 1:30 p.m. today. Nurses have advised there is nothing set up for home health care only a Dr. (doctors) orders.
A review of the facility's physician Discharge summary, dated [DATE] at 9:23 a.m. revealed in pertinent part, Disposition: Discharge to home with home health. History of present illness: Patient discharged to SNF (skilled nursing facility) and then to home with wound vac. However home health care was not successfully arranged.
Rehabilitation process: Resident #191 has achieved the desired rehabilitation goals and collectively deemed safe to transition home with health services. I certify that home health services are medically necessary as the patient is expected to be relatively homebound and any initial trips away from home will require considerable taxing efforts and subsequent office appointments with you or a specialist.
Documentation was requested from NHA on 3/7/24 at 11:53 a.m. for the preferred home health referral from the facility (social services department), and confirmation response from the home health company for accepting the referral.
-No documentation was provided. See NHA interview below.
III. Staff interviews
The NHA was interviewed on 3/11/24 at 9:28 a.m. He said the facility did not receive confirmation from the preferred home healthcare company that they were able to accept the referral for Resident #191. He said the facility discharged the resident without confirmation that home health services were arranged.
The director of nursing (DON) was interviewed on 3/11/24 at 10:25 a.m. She said the discharge process was to receive a physician order to discharge, and the social services department opens up a discharge summary with IDT involvement. She said social services makes a plan that includes needs, goals, appointments, equipment, home healthcare or other ancillary needs. The DON said if there were not any home health companies that were available to take a referral, social services should inform the physician and the resident/responsible party. The DON said if the physician orders were not able to be followed for home healthcare services, they would reconsider the plan.
The DON said communication between the home health company and the discharge planner was important to ensure a safe discharge. The DON said she would not have wanted Resident #191 discharged without home health services in place because Resident #191 at high risk of infection and hospitalization.
The SSD, ANHA, and SSA were interviewed on 3/11/24 at 12:20 p.m. The SSD said the discharge process was to set up a care conference/IDT to see what was needed such as medical equipment, where going at discharge (i.e. home), home healthcare and other supportive services. The ANHA said a discharge date was then scheduled, and the physician would complete a discharge assessment. The SSA said if home health service were not available, she would offer outpatient therapy to the resident.
The SSA said she was the case manager who arranged Resident #191's discharge home. She said Resident #191 was referred to a home health agency that the family preferred and that had cared for the resident in the past. The SSA said she sent the home health referral on Friday 2/2/24. She said the home health agency had accepted the referral. She said she did not have any documentation that the home health had received and accepted Resident #191's referral. The SSA said she found out on Monday 2/5/24 from the RR that the home health company did not accept the referral. The SSA said she did not follow up with the preferred home health company, nor offer to arrange alternate home health services.
The referred home health company was contacted on 3/11/24 at 1:43 p.m. The home health referral coordinator (HHRC) said she received a fax referral from the facility for Resident #191 on 2/2/24. The HHRC said they did not receive a call from the facility to confirm or follow up. The HHRC said she called the facility to advise that the agency could not accept the referral because they did not have the staffing available.
IV. Facility follow-up
On 3/12/24 at 5:00 p.m., the NHA provided the following information via email:
It revealed the INHA and SSA called the preferred home health provider following the survey on 3/12/24 to follow up on the home health care needs for Resident #191.
The home health director of nursing (HHDON) responded in an email on 3/12/24 at 1:48 p.m. to the ANHA and revealed in pertinent part, Resident #191 was a client with (company name) home health for two years. In that time, she fired all clinicians and would constantly make complaints, which were unfounded. Since Resident #191 had declined all of our clinicians, we were unable to meet her needs to staff appropriately. Staffing was the reason why we could not take her back.
Additionally, Resident #191 wrote a review about (company name) home health, rated very poorly, stating that we should, 'close our doors.' This was not a factor to decline the referral, only to give more details. When she would call about a complaint or issue, each time would end with her abruptly hanging up the phone until time passed and history would repeat itself. If you have any questions or would like more clarity, please let me know.
- The documentation confirmed the preferred home health company declined the facility referral for Resident #191 due to staffing and the facility failed to follow up to ensure Resident #191 had a safe discharge and home health services at home per physician order and therapist recommendations.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to assist one (#60) of two sample residents reviewed for vision/ancil...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to assist one (#60) of two sample residents reviewed for vision/ancillary services out of 53 sample residents.
Specifically, the facility failed to offer to arrange Resident #60 an appointment for optometry services.
Findings include:
I. Facility policy
The Hearing and Vision Services policy and procedure, revised March 2023, was provided by the nursing home administrator (NHA) on 3/11/24 at 4:04 p.m.
It revealed in pertinent part,
The facility will utilize the comprehensive assessment process for identifying and assessing a resident's vision and hearing abilities in order to provide person-centered care. Employees should refer any identified need for hearing or vision services/appliances to the social worker/social service designee.
The social worker/social service designee is responsible for assisting residents, and their families, in locating and utilizing any available resources (Medicare or Medicaid program payment, local health organizations offering items and services which are available free to the community), for the provision of the vision and hearing services the resident needs.
Once vision or hearing services have been identified, the social worker/social service designee will assist the resident by making appointments and arranging for transportation.
II Resident status
Resident #60, age [AGE], was admitted on [DATE]. According to the March 2024 computerized physician orders (CPO), diagnoses included Horner's disease (disrupted nerve pathway on one side of the brain to the face and eye) and acute respiratory failure.
The 12/15/23 minimum data set (MDS) assessment revealed the resident was cognitively intact with a brief interview for mental status (BIMS) score of 14 out of 15. She required extensive assistance from two people with most of her daily activities. The resident required a corrective lens.
III. Resident interview
Resident #60 was interviewed on 3/5/24 at 2:56 p.m. She said she had asked staff for an optometry appointment since she was admitted . She could not see well and it was affecting her ability to do activities that she liked to do. Resident #60 said she thought she may have cataracts and wanted to see an eye doctor for a checkup.
IV. Record review
According to an activity note dated 10/25/23 the resident asked the activities staff about getting an optometrist appointment. The activities staff advised the resident to talk to social services.
According to the vision care plan dated 11/17/23, the resident was at risk for impaired visual function due to a nuclear cataract (clouding that develops in the lens). Interventions included the following: Arrange a consultation with an eye care practitioner as required. Encourage the resident to wear visual appliances for safety and to promote independence. Monitor, document, and report signs of acute eye problems to the physician. Remind the resident to wear glasses when she is up.
V. Staff interviews
The social services director (SSD) was interviewed on 3/11/24 at 10:03 a.m. The SSD said the department was in charge of assisting with optometry appointments.
The SSD said Resident #60 did require glasses. The SDD said the resident did not have insurance covering the in-house optometrist. The SDD said the social services department would assist with scheduling and transportation to an outside provider.
The SSD said she could not obtain documentation showing the resident was offered optometry services.
The director of nursing (DON) was interviewed on 3/11/24 at 3:27 p.m. The DON said the social services department assisted with ancillary care. The DON said when a resident had concerns with an optometry appointment they should inform the nursing staff and they would inform the appropriate person.
The DON said Resident #60 should have had an optometry appointment when she told the staff.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to ensure one (#101) of three residents reviewed for ox...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review and interviews, the facility failed to ensure one (#101) of three residents reviewed for oxygen therapy was provided respiratory care consistent with professional standards of practice out of 53 sample residents.
Specifically, the facility failed to:
-Ensure Resident #101 received oxygen as ordered by the physician; and,
-Ensure Resident #101's oxygen saturation level (amount of oxygen in the blood) was monitored appropriately.
Findings include:
I. Facility policy and procedure
The Oxygen Administration policy and procedure, reviewed June 2023, was provided by the nursing home administrator (NHA) on 3/11/24 at 4:13 p.m. It read in pertinent part,
It is the policy of this facility that oxygen therapy is administered, as ordered by the physician or as an emergency measure until the order can be obtained.
Document all appropriate information in medical record: oxygen therapy, respiratory assessment finding, method of oxygen delivery, flow rate, patency of cannula, resident's response and any adverse reactions or side effects.
II. Resident #101
A. Resident status
Resident #101, age [AGE] , was admitted on [DATE] and readmitted on [DATE]. According to the March 2024 computerized physician orders (CPO), diagnoses included chronic obstructive pulmonary disease with acute exacerbation (COPD) and morbid obesity with hypoventilation (shallow breathing).
The 1/23/24 minimum data set (MDS) assessment revealed the resident was cognitively intact with a brief interview for mental status (BIMS) score of 14 out of 15. He required substantial/maximal assistance with toileting, personal hygiene, transfers, set up assistance with eating and supervision with bed mobility.
B. Observations and resident interview
On 3/5/24 at 11:38 a.m., Resident #101 was lying flat in bed on room air with an oxygen nasal cannula lying on the bedside table. The oxygen concentrator was set at five liters per minute (LPM) of oxygen.
On 3/6/24 at 12:57 p.m., Resident #101 was lying flat in bed on room air with an oxygen nasal cannula in a plastic bag hanging on the oxygen concentrator. The oxygen concentrator was set at five LPM.
On 3/7/24 at 10:28 a.m., Resident #101 was lying flat in bed with an oxygen nasal cannula in his nose and the oxygen concentrator was set at five LPM.
On 3/7/24 at 4:00 p.m., Resident #101 was lying in bed with an oxygen nasal cannula in his nose and the oxygen concentrator was set at five LPM.
On 3/11/24 at 11:00 a.m., Resident #101 was lying in bed with an oxygen nasal cannula in his nose and the oxygen concentrator was set at five LPM.
Resident #101 was interviewed on 3/6/24 at 10:40 a.m. Resident #101 said the nurse had taken him off of his oxygen this morning (3/6/24) and left it on the bedside table. He said the staff had been placing him on five LPM of oxygen. He said staff had not checked his oxygen saturation level that morning (3/6/24).
C. Record review
The oxygen therapy care plan, initiated 11/22/22, indicated Resident #101 required oxygen related to ineffective gas exchange. Interventions included assist with ambulation as indicated, give medications as ordered by physician, monitor for signs and symptoms of respiratory distress including pulse oximetry, oxygen setting at 4 (four) LPM via nasal cannula, promote lung expansion and improve air exchange by proper body positioning with head of bed at 45 degrees.
-A review of the oxygen therapy care plan did not reveal any personalized interventions added after his readmission on [DATE].
The 1/30/24 physician orders documented apply oxygen via nasal cannula up to 4 (four) liters of oxygen to keep oxygen saturations at or above 90 percent (%), titrate (adjust) as indicated. The order was discontinued on 3/6/24.
The 3/6/24 physician orders documented apply oxygen via nasal cannula up to four liters of oxygen at night and as needed to keep oxygen saturation at or above 88%, titrate as indicated.
The resident's oxygen saturations were documented as follows:
-3/5/24 at 7:14 a.m. 89% on room air;
-3/6/24 at 4:48 p.m. 97% at four liters per minute;
-3/7/24 at 12:17 p.m. 98% on room air;
-3/7/24 at 6:11 p.m. 90% on oxygen via nasal cannula. No flow rate was documented;
-3/7/24 at 9:51 p.m. 90% on oxygen via nasal cannula. No flow rate was documented;
-3/8/24 at 5:32 p.m. 96% on oxygen via nasal cannula. No flow rate was documented;
-3/9/24 at 6:53 a.m. 95% on oxygen via nasal cannula. No flow rate was documented;
-3/9/24 at 5:10 p.m. 93% on oxygen via nasal cannula. No flow rate was documented;
-3/10/24 at 5:22 p.m. 95% on oxygen via nasal cannula. No flow rate was documented; and,
-3/11/24 at 7:09 a.m. 93% on room air.
A comprehensive review of the resident's oxygen saturations revealed it was documented only once on 3/5/24, 3/6/24, 3/8/24 and 3/10/24.
A comprehensive review of the resident's oxygen saturations failed to reveal documented flow rates on 3/7/24, 3/8/24, 3/9/24, 3/10/24.
-A comprehensive review of the resident's medical record failed to reveal physician ordered parameters on how often oxygen saturations should be checked.
D. Staff interviews
Licensed practical nurse (LPN) #1 was interviewed on 3/11/24 at 10:14 a.m. LPN #1 said oxygen flow rates along with parameters were ordered by the physician and were populated on the treatment administration record (TAR). She said, for any resident on oxygen therapy, if their oxygen saturation level fell below 90% on the prescribed oxygen flow rate and required more oxygen than the prescribed flow rate, the physician should be notified. She said residents on oxygen therapy required vital signs with oxygen saturations checked and documented every eight hours. She said it was the nurse's responsibility to ensure it was documented. LPN #1 said documentation included if the oxygen saturation was on room air or nasal cannula and the oxygen flow rate if oxygen was being used. She said Resident #101 was on four liters per nasal cannula at night and as needed to keep oxygen saturations at or above 88%.
-However, observations revealed the resident's oxygen concentrator was set to five LPM (see observations above).
The director of nursing (DON) was interviewed on 3/11/24 at 3:00 p.m. The DON said every resident on oxygen therapy should have a physician order for oxygen liter flow and parameters for titration and monitoring. She said oxygen therapy and the parameters were care planned and placed on the task assignments for the certified nurse aides (CNA). She said if a resident on oxygen therapy required more oxygen outside of the ordered parameters the physician should be notified. The DON said oxygen saturation monitoring depended on physician orders but typically it was done at least once a shift.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record review, the facility failed to maintain an infection control program designed to provide a safe, sanitary and comfortable environment to help prevent the d...
Read full inspector narrative →
Based on observations, interviews and record review, the facility failed to maintain an infection control program designed to provide a safe, sanitary and comfortable environment to help prevent the development and transmission of disease and infection in one of three units.
Specifically, the failed to:
-Ensure clean technique was followed during wound care for Resident #72; and,
-Ensure wound care scissors were cleaned and disinfected according to standards of practice.
Findings include:
I. Clean technique during wound care
A. Manufacturer recommendations
Harmony Lab and Safety Supplies. (2024). Micro Kill+ Disinfectant Wipes. https://harmonycr.com/micro-kill-disinfectant-wipes/, retrieved on 3/13/24.
Environmental Protection Agency (EPA) registered disinfectant wipe kills 13 different infectious microorganisms, including athlete's foot fungus in five minutes; Tuberculosis, E. coli, hepatitis B and C, Salmonella and Vancomycin resistant enterococci (VRE) in two minutes and HIV (human immunodeficiency virus) in one minute.
B. Observations
Licensed practical nurse (LPN) #2 and LPN #3 were observed providing wound care to Resident #72's right foot wounds and left heel wound on 3/11/24 at 10:50 a.m.
LPN #2 was observed placing a clean disposable absorbent pad down on a bedside table and opening clean supplies onto the pad.
-LPN #2 did not wipe down the bedside table before placing the absorbent pad and clean supplies onto the table.
LPN #2 performed hand hygiene and donned clean gloves. She tried removing the bloody kerlix dressing from Resident #72's right foot. She picked up a wound cleanser bottle and sprayed the dressing to facilitate removal of the dressing.
-LPN #2 placed the wound cleanser bottle, with a visibly bloody handle onto the clean absorbent pad with the clean supplies.
-LPN #2 did not clean off the handle of the wound cleanser bottle.
-LPN #2 removed her soiled gloves, performed hand hygiene and donned clean gloves. She picked up the wound cleanser bottle with the visibly bloody handle and sprayed wound cleanser onto a clean gauze and cleaned the right ankle wound.
-LPN #2 placed the wound cleanser back onto the clean absorbent pad without cleaning.
LPN #2 obtained Resident #72's designated scissors and wiped them with an alcohol prep pad. She then cut the clean hydrofera blue dressing to fit the wound.
-LPN #2 did not use an appropriate EPA registered disinfectant wipe to clean the scissors.
-After completing the resident's wound care, LPN #2 wiped Resident #72's scissors with an alcohol prep pad (instead of a disinfectant wipe) and placed the scissors into the bag with the resident's clean dressing supplies.
-LPN #2 placed the supply bag on the bedside table and the scissors fell to the floor. LPN #2 picked up the scissors, re-wiped the scissors with an alcohol prep pad and placed the scissors back into the clean dressing supply bag.
-LPN #3 cleaned the top of the bloody handle on the wound cleanser bottle with an alcohol prep pad and placed the bottle with the resident's clean dressing supplies.
-LPN #3 did not use an appropriate EPA registered disinfectant wipe to clean the soiled handle.
D. Staff interviews
LPN #2 was interviewed on 3/11/24 at 11:30 a.m. LPN #2 said if any wound dressing supply was contaminated after touching a dirty dressing or contaminated with blood it should not be placed back onto a clean field or placed with clean dressings. She said scissors should be cleaned and disinfected before and after use with the purple top disinfecting wipes and left wet for the manufacturer recommended times.
The director of nursing (DON) was interviewed on 3/11/24 at 11:40 a.m. The DON said dirty contaminated items should be kept separate from the clean field and supplies to prevent cross contamination. She said resident scissors should be cleaned before and after use with Micro Kill disinfectant wipes and kept wet for the manufacturer recommended disinfection times.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0575
(Tag F0575)
Could have caused harm · This affected multiple residents
Based on observations, record review and interviews, the facility failed to post, in a form and manner accessible and understandable to residents, a list of names, addresses (mailing and email) and te...
Read full inspector narrative →
Based on observations, record review and interviews, the facility failed to post, in a form and manner accessible and understandable to residents, a list of names, addresses (mailing and email) and telephone numbers of all pertinent State Agencies and advocacy groups.
Specifically, the group interview revealed the residents were not aware of where the State Agency phone numbers were posted in the facility.
Findings include:
I. Resident group interview
A resident group interview, which included four cognitively intact residents according to facility assessment, was conducted on 3/6/24 at 1:00 p.m. Resident #80, #92, #128 and #302 said they did not know where the State Agency and ombudsman information were posted in the facility. They said they had not been informed of this information during resident council meetings.
Resident #128 said he was not informed of how to make a formal complaint or how to contact the state agency.
II. Observations
Observations conducted throughout the facility on 3/5/24 at 3:00 p.m. revealed the facility failed to ensure the posting of names, addresses (mailing and email) and telephone numbers of pertinent state agencies, such as the state survey agency and the state licensure office, and adult protective services.
Observations conducted with the nursing home administrator (NHA) on 3/6/24 at 2:45 p.m. on the facility's four nursing units revealed the NHA was unable to locate the posting of names, addresses (mailing and email) and telephone numbers of pertinent State Agencies, such as the State Survey Agency and the State licensure office, and Adult Protective Services.
III. Record review
The nursing home administrator (NHA) provided an untitled audit dated January 2024. It documented:
A chart titled infection control documented the following: Check for notification signs to report complaints and recent survey results updated was marked as met.
-However, according to the observations, conducted during the survey process, showed the facility failed to post the State Agency contact information.
-The audit did not provide any additional information regarding where the notification signs were posted and verified as present.
IV. Staff interviews
The NHA was interviewed on 3/6/24 at 2:30 p.m. The NHA said the facility did not have postings regarding information of pertinent State Agencies. He said there had been a posting in the past, but it must have been removed.
The NHA said a corporate clinical consultant was tasked with performing a quarterly audit to verify the required information was posted, however he was unable to locate the postings.
V. Facility follow-up
On 3/6/24 at 3:20 p.m, during the survey process, the NHA provided a copy of a list of names, addresses (mailing and email) telephone numbers of all pertinent State Agencies and advocacy groups. Observations conducted on 3/6/24 at 4:00 p.m. revealed the list was posted in the four units of the facility, after it was brought to the attention of the NHA.