NEW CASTLE HEALTH AND REHABILITATION CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
New Castle Health and Rehabilitation Center has received a Trust Grade of F, indicating significant concerns about the facility's overall quality and care. It ranks #34 out of 43 nursing homes in Delaware, placing it in the bottom half of facilities in the state. Although the facility is improving, with issues decreasing from 29 in 2024 to just 5 in 2025, there are still critical concerns, including a recent incident where a resident at risk of aggression did not receive the necessary 1:1 observation, which could lead to safety issues. Staffing is a relative strength, with a rating of 4 out of 5 stars, but the 45% turnover rate is average, meaning staff changes are common. On a positive note, the facility has not incurred any fines, which is encouraging, but there have been issues such as failure to properly label and store food, raising potential health risks for residents.
- Trust Score
- F
- In Delaware
- #34/43
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 45% turnover. Near Delaware's 48% average. Typical for the industry.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Delaware facilities.
- Skilled Nurses ✓ Good
- Each resident gets 48 minutes of Registered Nurse (RN) attention daily — more than average for Delaware. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 45 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (45%)
3 points below Delaware average of 48%
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Below Delaware average (3.3)
Below average - review inspection findings carefully
Near Delaware avg (46%)
Typical for the industry
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 45 deficiencies on record
May 2025
5 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Cross refer to F610, F658 example 2
Review of R5's clinical record revealed:
1/20/23 - R5 was admitted to the facility for lo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and review of a clinical record and other documentation as indicated, it was determined that for one (R5) out of five residents reviewed for accidents, the facility failed to have e...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0627
(Tag F0627)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, it was determined that for one (R5) out of three residents reviewed for discharge, the fac...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined that for two (R1 and R5) out of five residents sampled for accidents, the facility failed to meet professional standards of the Delaware Board o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R1) out of four residents reviewed for accidents, the facility failed to have his advanced directive and copy of his DPOA (Durable...
Read full inspector narrative →
Nov 2024
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interviews, the facility failed to assess a resident for self-administration of medication for one of one resident (Resident (R) 7) reviewed for self-administr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews, the facility failed to ensure residents had access to call lights when nee...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, record review, and facility policy review, the facility failed to protect two of four residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record review, and review of the facility's policy, the facility failed to report allegations of abuse to t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interviews, and facility policy review, the facility failed to ensure a thorough investigation was compl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, interview, and facility policy review, the facility failed to ensure the care plan was upda...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0691
(Tag F0691)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to ensure proper nephrostomy tube care for one of thr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interviews, record review, and review of the facility's policy, the facility failed to ensure personal protective equipment (PPE) was utilized properly with proper hand hygiene d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, document review, and interview, the facility failed to ensure all pureed foods on the menu were served to the seven residents who received pureed diets out of a total census of 1...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and facility policy review, the facility failed to ensure foods were labeled, dated, sealed, and stored according to professional standards for food service safety in ...
Read full inspector narrative →
Feb 2024
19 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and record review, it was determined that the facility failed to promote R2's dignity by keeping R2's urinary collection bag in a privacy bag. Findings include:
7/1/15 - R2 was a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined that for one (R474) out of one resident reviewed for choices, the facility failed to ensure the right to self-determine when R474's preference fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, it was determined that the facility failed to ensure that R106 was free from...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, it was determined for one (R106) out of three residents review for resident assessment the facility failed to accurately document R106's side rails ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined that for one (R84) out of three residents reviewed for PASARR, the facility failed to ensure a referral for a new PASARR screening after changes ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review for one (R106) out of three residents reviewed for careplans, it was determined that the facility failed to accurately develop and implement a compreh...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
Based on record review, interview and review of facility documentation, it was determined that for one (R524) out of two residents reviewed for discharge, the facility failed ensure that R524's discha...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview it was determined that for one (R476) out of three residents reviewed for accidents the fac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, it was determined that for one (R31) out of three residents reviewed for bowe...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined that for one ( R475) out of four residents reviewed for nutrition the facility failed to implement interventions related to risk for weight loss ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on interview, record review and review of other facility documentation, it was determined that for two (R525 and 274) out of five residents reviewed for pain, the facility failed to ensure that ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to accurately assess R106's medical condition for the ne...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, it was determined for one (R274) out of five sampled residents for pain the facility faile...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined that for two (R54, R98) out of five residents (R2, R43, R54, R98, R106) reviewed for unnecessary medications, the facility failed to ensure that...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
Based on interview and record review, it was determined that for six (R25, R29, R31, R43, R56 and R119) out of six residents reviewed for advance directive, the facility failed to offer the opportunit...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected multiple residents
Based on record review and interview, it was determined that for three (R29, R43 and R99) out of six residents reviewed for physician services, the facility failed to ensure each resident was seen for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on record review and interview it was determined that for five (E19, E22, E23, E24 and E25) out of five CNAs (certified nurse's aides) reviewed, the facility failed to provide proof of annual pe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, it was determined that the facility failed to ensure that the start dates were documented when over the counter medications (bottles) were opened in ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on record review and interview, it was determined that for eight (R25, R29, R31, R50, R56, R99, R123 and R276) out of thirty (30) residents clinical records reviewed, the facility failed to ensu...
Read full inspector narrative →
Sept 2021
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined that the facility failed to promote and facilitate self determination for one (R100) out of one resident investigated for choices. Review of the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and clinical record review, it was determined that the facility failed to immediately consult with the resident's physician for one (R100) out of five residents sampled for nutritio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on interview and clinical record review, it was determined that the facility failed to identify the need for a Significant Change in Status Assessment (SCSA) for one (R100) out of five sampled r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, it was determined that for one (R60) out of six sampled residents for medication administration observation, the facility failed to ensure to veri...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review, interview, and review of the facility's policy and procedure, it was determined that the facility failed to implement policies and procedures for the monthly Medication Regimen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on clinical record review and interview, it was determined that for one (R3) out of five sampled residents for unnecessary medication review, the facility failed to ensure R3's PRN antianxiety m...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observation, interviews and record review, it was determined that the facility failed to accommodate a food preference for one (R88) out of 41 sampled residents. Findings include:
9/14/21 at ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record review, it was determined that the facility failed to ensure activities of daily living (ADL) related to showers and/or baths were provided to one (R100) ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, interviews and review of facility policy, it was determined that the facility failed to ma...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation and staff interviews it was determined that three out of three medication carts
reviewed contained improperly stored medications. Findings include:
9/21/21 9:45 AM - Medication c...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected most or all residents
Based on observation, resident council interview and other resident interviews, it was determined for 103 residents the facility failed to provide an option to file a grievance anonymously. Findings i...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Delaware facilities.
- • 45% turnover. Below Delaware's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 1 life-threatening violation(s). Review inspection reports carefully.
- • 45 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • Grade F (38/100). Below average facility with significant concerns.
About This Facility
What is New Castle Center's CMS Rating?
CMS assigns NEW CASTLE HEALTH AND REHABILITATION CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Delaware, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is New Castle Center Staffed?
CMS rates NEW CASTLE HEALTH AND REHABILITATION CENTER's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 45%, compared to the Delaware average of 46%. This relatively stable workforce can support continuity of care. RN turnover specifically is 70%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at New Castle Center?
State health inspectors documented 45 deficiencies at NEW CASTLE HEALTH AND REHABILITATION CENTER during 2021 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 44 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
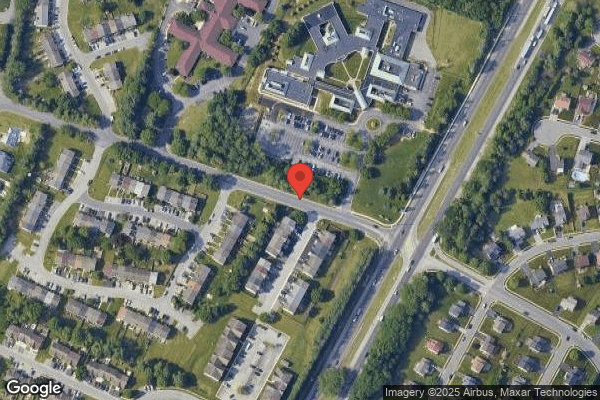
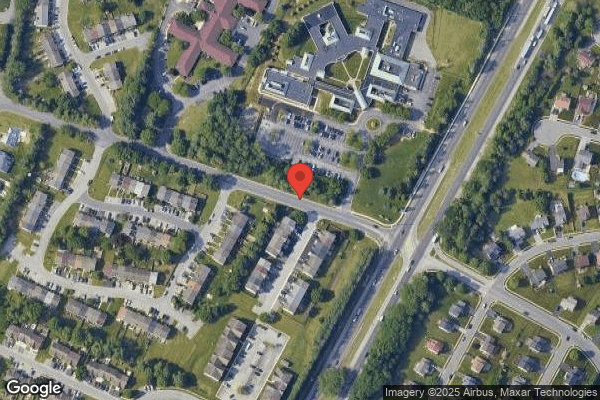
Who Owns and Operates New Castle Center?
NEW CASTLE HEALTH AND REHABILITATION CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by SABER HEALTHCARE GROUP, a chain that manages multiple nursing homes. With 120 certified beds and approximately 114 residents (about 95% occupancy), it is a mid-sized facility located in NEW CASTLE, Delaware.
How Does New Castle Center Compare to Other Delaware Nursing Homes?
Compared to the 100 nursing homes in Delaware, NEW CASTLE HEALTH AND REHABILITATION CENTER's overall rating (2 stars) is below the state average of 3.3, staff turnover (45%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting New Castle Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is New Castle Center Safe?
Based on CMS inspection data, NEW CASTLE HEALTH AND REHABILITATION CENTER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Delaware. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at New Castle Center Stick Around?
NEW CASTLE HEALTH AND REHABILITATION CENTER has a staff turnover rate of 45%, which is about average for Delaware nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was New Castle Center Ever Fined?
NEW CASTLE HEALTH AND REHABILITATION CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is New Castle Center on Any Federal Watch List?
NEW CASTLE HEALTH AND REHABILITATION CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.