REHAB & HEALTHCARE CENTER OF CAPE CORAL




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
The Rehab & Healthcare Center of Cape Coral has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #665 out of 690 facilities in Florida places it in the bottom half of nursing homes statewide and #18 out of 19 in Lee County, suggesting very few local options are better. The facility is experiencing a worsening trend, with problems increasing from 4 issues in 2024 to 14 in 2025, and has been assessed with $74,301 in fines, which is higher than 86% of Florida facilities and raises concerns about compliance. Staffing is relatively stable with a 3 out of 5 star rating and a turnover rate of 36%, which is below the state average, and there is more RN coverage than 84% of facilities, which is a positive aspect. However, specific incidents of concern include a critical failure to supervise a cognitively impaired resident who wandered outside unnoticed for two hours and multiple residents not having their call lights within reach, potentially leaving them unable to request assistance when needed. Overall, while there are some strengths, the significant issues highlighted make this facility a concerning choice for families.
- Trust Score
- F
- In Florida
- #665/690
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 36% turnover. Near Florida's 48% average. Typical for the industry.
- Penalties ✓ Good
- $74,301 in fines. Lower than most Florida facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 51 minutes of Registered Nurse (RN) attention daily — more than average for Florida. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 36 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (36%)
12 points below Florida average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Below Florida average (3.2)
Significant quality concerns identified by CMS
Near Florida avg (46%)
Typical for the industry
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 36 deficiencies on record
May 2025
3 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
Based on observation, residents and staff interviews, the facility failed to ensure reasonable accommodation of needs by failure to ensure the call light was within reach to request assistance as need...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected multiple residents
Based on record review, review of facility's policies and procedures, and staff interviews, the facility failed to protect residents' rights to be free from neglect by failing to provide the necessary...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected multiple residents
Based on review of the clinical record and staff interviews, the facility failed to provide specialized rehabilitative services as directed by the plan of care for 1(Resident #999) of 3 residents for ...
Read full inspector narrative →
Feb 2025
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to accommodate smoking needs and preferences for 1 (Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, review of the clinical record, and resident and staff interviews, the facility failed to develop a care pl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, staff and resident interviews, and review of facility policy and procedure, the fa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and staff interviews, the facility failed to provide appropriate care and services to prev...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, review of facility policy and procedure, record review and staff interview the facility failed to follow physician's orders for an abdominal binder over a feeding tube for 1 (Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure short peripheral catheter (a thin, flexible tube is inserted into a vein, usually in the back of the hand, the lower pa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observations, staff interviews and record reviews, the facility failed to provide a safe, sanitary, and homelike environment as evidenced by dry wall damage in resident's rooms. Failure to id...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, review of job description, clinical record review, staff and resident interviews, the facility failed to p...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and staff interviews, the facility failed to have documentation nursing staff addressed a reported chang...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, clinical record review and staff interviews the facility failed to ensure a medication error rate less than 5 percent. 29 opportunities, 5 residents and four different nurses wer...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Review of the clinical record for Resident #107 revealed an admission date of 11/27/24 and re-admission date of 1/21/25. Diagnos...
Read full inspector narrative →
May 2024
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on review of facility records, review of facility policies and procedure and resident and staff interviews the facility failed to ensure appropriate corrective action to resolve the expressed co...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, review of facility policy and procedure, staff and resident interviews the facility failed to ensure a saf...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, review of the clinical record, and staff and resident interviews, the facility failed to provide the neces...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected multiple residents
Based on observation, and resident and staff interviews, the facility failed to maintain an effective pest control program and a sanitary environment free from pests for residents residing in the skil...
Read full inspector narrative →
Jun 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected 1 resident
Based on review of facility policies and procedures, and resident and staff interviews, the facility failed to maintain an effective pest control program and a sanitary environment free from pests for...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, and staff interviews, the facility failed to maintain a safe, sanitary, and comfortable environment for re...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, review of facility policies and procedures and staff interviews, the facility failed to maintain ice and water dispensers in a clean and sanitary manner for residents, staff and ...
Read full inspector narrative →
Feb 2023
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, resident and staff interview, the facility failed to provide a call light to accommodate th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, record review, and staff interview the facility failed maintain an indwelling catheter (tube inserted into the bladder to drain urine) in a safe and sanitary manner for 1(Residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review, resident's family and staff interview, the facility failed to ensure the administration of intravenous (IV) fluids as prescribed by the physician for 1 (Resident #106) of 2 res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, record review, review of facility policy, and staff interviews, the facility failed to ensure 1(Resident #69) of 1 resident reviewed for accidents was assessed for alternative in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on a review of the Consultant Pharmacist's Medication Regimen Review report, and staff interview, the facility failed to have documentation of monthly medication review for 2 (Resident #93, and ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, staff, and resident interview, the facility failed to provide the necessary care and servic...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
Based on observation, record review, review of facility's policies and procedures, resident and staff interview the facility failed to provide ongoing assessment and failed to provide wound care and i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to remove outdated medications from the refrigerator and...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected multiple residents
Based on observation and staff interview, the facility failed to post the required current daily staffing data in a prominent place readily accessible to residents and visitors.
The findings included:...
Read full inspector narrative →
Jan 2023
3 deficiencies
2 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, review of surveillance camera video recording, review of the facility's abuse and neglect p...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, review of surveillance camera video recording, Resident representative and staff interviews...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0843
(Tag F0843)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to have a written transfer agreement
in effect with one or more hospitals approved for participation under the Medicaid and Medicare
p...
Read full inspector narrative →
Jul 2021
3 deficiencies
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0563
(Tag F0563)
Could have caused harm · This affected multiple residents
Based on observation, review of the facility's policies and procedures, staff, resident, and family member interview, the facility failed to ensure residents' right to receive visitors of his or her c...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interview, the facility failed to have documentation of a discharge summary including recapitulation...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
3. Review of the Quarterly Activities Assessment for Resident #5 dated 4/15/21 revealed documentation Resident #5 requires physical assistance to and from activities, resident would benefit from large...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 36% turnover. Below Florida's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 2 life-threatening violation(s), $74,301 in fines, Payment denial on record. Review inspection reports carefully.
- • 36 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $74,301 in fines. Extremely high, among the most fined facilities in Florida. Major compliance failures.
- • Grade F (6/100). Below average facility with significant concerns.
About This Facility
What is Rehab & Healthcare Center Of Cape Coral's CMS Rating?
CMS assigns REHAB & HEALTHCARE CENTER OF CAPE CORAL an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Florida, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Rehab & Healthcare Center Of Cape Coral Staffed?
CMS rates REHAB & HEALTHCARE CENTER OF CAPE CORAL's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 36%, compared to the Florida average of 46%. This relatively stable workforce can support continuity of care. RN turnover specifically is 56%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Rehab & Healthcare Center Of Cape Coral?
State health inspectors documented 36 deficiencies at REHAB & HEALTHCARE CENTER OF CAPE CORAL during 2021 to 2025. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 33 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Rehab & Healthcare Center Of Cape Coral?
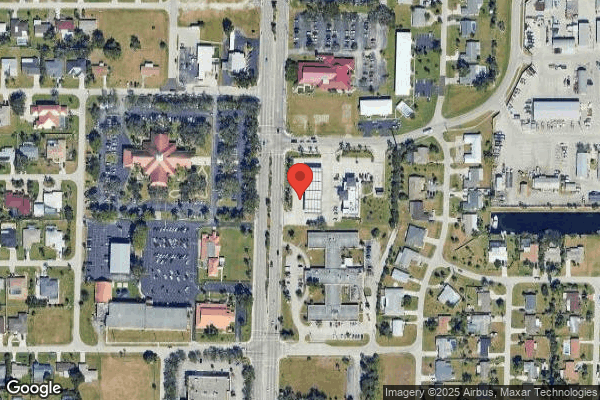
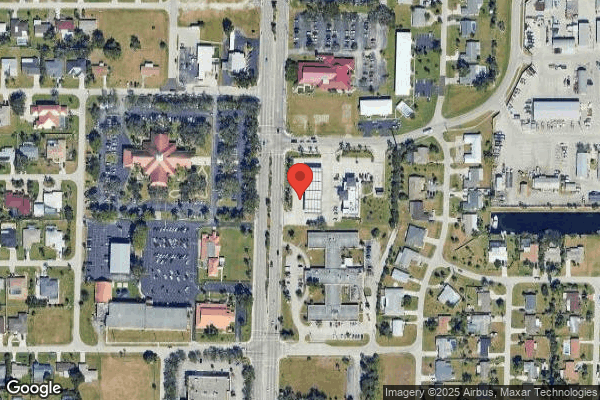
REHAB & HEALTHCARE CENTER OF CAPE CORAL is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility is operated by FLORIDA INSTITUTE FOR LONG-TERM CARE, a chain that manages multiple nursing homes. With 118 certified beds and approximately 107 residents (about 91% occupancy), it is a mid-sized facility located in CAPE CORAL, Florida.
How Does Rehab & Healthcare Center Of Cape Coral Compare to Other Florida Nursing Homes?
Compared to the 100 nursing homes in Florida, REHAB & HEALTHCARE CENTER OF CAPE CORAL's overall rating (1 stars) is below the state average of 3.2, staff turnover (36%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Rehab & Healthcare Center Of Cape Coral?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Rehab & Healthcare Center Of Cape Coral Safe?
Based on CMS inspection data, REHAB & HEALTHCARE CENTER OF CAPE CORAL has documented safety concerns. Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Florida. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Rehab & Healthcare Center Of Cape Coral Stick Around?
REHAB & HEALTHCARE CENTER OF CAPE CORAL has a staff turnover rate of 36%, which is about average for Florida nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Rehab & Healthcare Center Of Cape Coral Ever Fined?
REHAB & HEALTHCARE CENTER OF CAPE CORAL has been fined $74,301 across 6 penalty actions. This is above the Florida average of $33,822. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Rehab & Healthcare Center Of Cape Coral on Any Federal Watch List?
REHAB & HEALTHCARE CENTER OF CAPE CORAL is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.