CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility's staff and interdisciplinary team (IDT) neglected to identify,...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility's staff and interdisciplinary team (IDT) neglected to identify, communicate, and provide necessary care and services to ensure the safety of a resident who wandered; neglected to respond to a missing resident in a timely and efficient manner; and failed to recognize and address an unsecured area as an environmental hazard to prevent a vulnerable, cognitively impaired resident from exiting the facility, for 1 of 4 residents reviewed for elopement, out of a total sample of 32 residents, (#25). These failures contributed to the elopement of resident #25 and placed her at risk for serious injury/impairment/death. While resident #25 was out of the facility unsupervised, there was a likelihood she could have fallen, been accosted by unknown persons, become lost, drowned, or been hit by a car.
On [DATE] at approximately 8:30 AM, resident #25 left the [NAME] Wing dining room and walked away from the unit. Along the way, the resident informed another resident's private caregiver that her ride did not show up, so she would walk home. Facility staff did not notice the resident as she wandered along the hallway or redirect her when she opened a door that led to the courtyard. The resident crossed the courtyard, opened the latch on an unlocked gate, and walked away from the property at approximately 8:38 AM. Resident #25 headed towards the heavily trafficked road in front of the facility, flagged down a passing car, and asked the driver to take her to the high school. The unknown person drove the resident to a high school located over three miles away, left her there, then called 911 to request a wellness check due to concerns about the resident's cognitive status. Meanwhile, at the facility, the private caregiver informed a staff member that resident #25 verbalized her intent to leave and was no longer present in the vicinity of the [NAME] Wing. The staff member disregarded the information and did not alert nursing staff or attempt to locate the resident. Resident #25's assigned nurse discovered she was missing at approximately 9:15 AM and staff initiated a search of the building and its surroundings. The facility was not aware of resident #25's whereabouts until approximately 10:00 AM when law enforcement contacted the resident's son, who retrieved his mother from the high school and returned her to the facility.
The facility's failure to implement policies and procedures to prevent neglect, maintain a secure environment, and respond appropriately to a report regarding a missing resident placed all residents who wandered and/or had access to the courtyard at risk. This failure resulted in Immediate Jeopardy starting on [DATE]. The Immediate Jeopardy was removed on [DATE]. The scope and severity of the deficiency was decreased to D, no actual harm, with potential for more than minimal harm, that is not Immediate Jeopardy after verification of the facility's immediate corrective actions.
Findings:
Cross reference F607, F641, F656, F689, and F835.
Review of the medical record revealed resident #25 was an [AGE] year-old female who was admitted to the facility on [DATE], with diagnoses including Alzheimer's Disease, dementia, insomnia, and anxiety.
Resident #25's admission Wandering/Elopement Risk Assessment dated [DATE], revealed she was cognitively impaired, independently ambulatory, and verbalized her intent to leave the facility. The assessment form included a recommendation to initiate a care plan to address the identified risk factors for elopement; however, the document showed no care plan was developed at that time.
Review of the facility's policy and procedure Wandering and Elopements (undated) revealed the facility would identify residents at risk for unsafe wandering. The document read, If identified to be at risk for wandering, elopement, or other safety issues, the resident's care plan will include strategies and interventions to maintain the resident's safety.
Review of resident #25's medical record from [DATE] to [DATE] revealed nursing notes that described the resident as confused, wandering, and requiring frequent redirection. Three days after admission, a Daily Skilled Note dated [DATE] indicated nursing staff deemed it necessary to place an electronic monitoring device on the resident to address her behaviors. The medical record revealed resident #25's behaviors escalated over the next two days. A Daily Skilled Note dated [DATE] revealed the resident was anxious and confused as she wandered throughout the facility. She repeatedly verbalized her intent to leave and successfully managed to open an emergency exit door. On [DATE], resident #25's assigned nurse noted she continuously wandered around the unit and informed staff she wanted to leave the facility and go home. A Clinical Note dated [DATE], two weeks after the electronic monitoring device was placed, revealed resident #25 eloped from the facility.
The Minimum Data Set (MDS) admission assessment with assessment reference date of [DATE] revealed resident #25 was admitted to the facility from the community. Her Brief Interview for Mental Status Score was 4 out of 10 which indicated severe cognitive impairment. In conflict with nursing progress notes, the MDS assessment showed the resident had no behavioral symptoms and did not wander or use a wander alarm. The document indicated it was very important to the resident to have her family involved in discussions regarding her care.
Review of the medical record revealed resident #25 had a care plan for elopement risk related to exit seeking behavior initiated on [DATE] at the time her electronic monitoring device was placed. The care plan goal was the resident would not have any successful elopement attempts. The interventions developed on [DATE] were to update elopement manuals with the resident's information, encourage activities of choice, and check the placement and function of her left ankle electronic monitoring device. The care plan did not incorporate any person-centered approaches that reflected IDT collaboration and input from the resident's family. In addition, the document did not provide instructions for direct care staff regarding effective approaches to address the resident's wandering and exit-seeking behaviors.
On [DATE] at 1:21 PM, the MDS Coordinator stated she attended daily clinical meetings with other members of the IDT. She explained the team discussed new admissions, new physician orders, incidents, and any other issues that affected residents. The MDS Coordinator stated the IDT would develop appropriate care plans and interventions to meet residents' needs based on the discussions. She stated in addition to the IDT process, a care plan meeting was held with each resident and/or a representative two to three weeks after admission, to identify any additional areas of concern or necessary services. The MDS Coordinator stated resident #25's care plan meeting was not held prior to her elopement. She validated the resident's elopement care plan with basic interventions were created on [DATE], the day she had the electronic monitoring device placed. The MDS Coordinator acknowledged the care plan did not show evidence of review or revisions by the IDT prior to her elopement to ensure the resident received care and services for her escalating behaviors.
In interviews on [DATE] at 1:30 PM and [DATE] at 9:49 AM, the Director of Nursing (DON) confirmed resident #25 had an electronic monitoring device applied on her fourth day in the facility as she was ambulatory and wandered. The DON confirmed the facility's IDT process included daily meetings to review residents' status, changes in condition, and care needs. She said, I was not aware of [the resident's] nighttime agitation and wandering. The DON acknowledged the IDT process therefore did not effectively identify or address the care and services required for resident #25. She confirmed resident #25 eloped from the facility on [DATE] by accessing the courtyard. She stated the resident wore an electronic monitoring device but there were no sensors at either the door to the courtyard or the gate. The DON explained the gate had a latch, but was never locked, and resident #25 quickly opened it and left the premises. The DON stated the incident investigation indicated another resident's private caregiver notified an Activity Department staff member that the resident stated she was leaving the facility. The DON explained the staff member did not inform anyone or initiate a search for the resident, but resumed her regular activities. The DON stated when the resident's assigned nurse noted she was missing at approximately 9:15 AM, all staff stopped what they were doing and searched the premises. She stated the facility followed policies and procedures by notifying the resident's family and law enforcement. The DON recalled resident #25's son and daughter arrived soon after being called, and she thought the Administrator notified law enforcement within 20 to 30 minutes after the resident was discovered to be missing. The facility was not able to show law enforcement had been notified by the Administrator. When asked what the facility's policy indicated regarding timeframe for notification of law enforcement, she explained there was no specific time period, and staff were to complete a search of the premises including the nine-story independent living facility next door first. The DON said, I believe the policy states a thorough search prior to call. She acknowledged while the cognitively impaired resident was outside the facility, she faced many potential safety hazards. The DON listed dangers that included a busy road, unleveled ground, traffic from the nearby neighborhood and schools, a construction site, woods, and a swimming pool. She stated a deputy sheriff responded to a call from dispatch regarding a wellness check request made by a concerned citizen who had picked up resident #25 at an unknown location and dropped her off at a high school. The DON stated the resident's son received a call from the deputy at approximately 10:00 AM, left to retrieve his mother, and the deputy followed them back to the facility. She recalled the deputy instructed her if the facility was ever again unable to find a resident, staff should call for assistance immediately.
Review of the facility's Procedures for an Elopement/Missing Resident (undated) revealed instructions to check the sign out log for evidence of authorized leave of absence, and then make a thorough search of the building and premises. The document indicated if the resident was not located, staff would notify the Administrator, DON, Risk Manager, the resident's representative, the attending physician, and law enforcement before continuing .an extensive search of the surrounding area. The attached document, Elopement Drill Instructions (undated) revealed details regarding assigned locations to be searched by designated staff. The search included all areas of the facility, including the Assisted Living Facility. Two maintenance staff were directed to .walk the entire perimeter of the entire campus, going in opposite directions. The document did not reference the nearby eleven-story independent living facility, nor instruct staff to delay law enforcement notification until that building was searched.
Review of the staff assignment sheet for Monday [DATE], noted resident #25's assigned Certified Nursing Assistant (CNA) for the 7:00 AM to 3:00 PM shift was CNA L. However, on [DATE] at 2:57 PM, CNA L stated she did not work on [DATE] and heard about resident #25's elopement on the following day when she returned to work. CNA L recalled someone told her CNA G was assigned to care for resident #25.
On [DATE] at 3:04 PM, CNA G explained she usually worked on the 3:00 PM to 11:00 PM shift and on occasion, she would pick up a 7:00 AM to 3:00 PM shift, but usually arrived at 8:30 AM. CNA G recalled on [DATE] she was seated in the [NAME] Wing dining room assisting a resident with breakfast and saw resident #25 eating at another table. CNA G said. I am not sure I was on [resident #25's] hallway that morning. She was finishing up breakfast and next thing they said they did not see her, and we started to look for her. CNA G could not recall how many CNAs were assigned to the unit on that shift, and when asked who monitored her assigned residents from the start of the shift at 7:00 AM until 8:30 AM when she arrived, she said, Everybody gives an eye on the team until I get here. CNA G did not recall any interaction with resident #25 prior to seeing her in the dining room and could not state with certainty that she was actually assigned to the resident on the morning she eloped from the facility.
On [DATE] at approximately 6:00 PM, the Staffing Coordinator provided a revised staff assignment sheet dated [DATE] which had been corrected to show CNA L did not work, and CNA G was assigned to care for resident #25. In response to multiple requests, the facility was unable to provide timeclock punch times for all CNAs who worked on the [NAME] Wing on [DATE] on the day shift. The facility provided a Payroll Punch Variance Form for CNA G. The form indicated CNA G worked from 7:00 AM to 7:15 PM, and in the comment section she wrote, No time clock. When asked to clarify the discrepancy between her earlier statement and the variance form, CNA G stated she forgot she started the day shift at 7:00 AM on [DATE].
On [DATE] at 8:47 AM, the private caregiver explained she worked in the facility six days weekly and was familiar with many of the residents, including resident #25. She stated the resident was usually confused and described her as kind of antsy on the morning she eloped. The private caregiver said, I saw her walking past the door.That day she looked like she was on a mission. She recalled resident #25 told her she had to get a ride or walk home and then headed towards the front lobby. The private caregiver stated she was worried the resident would try to go out the front door so after a while, she walked to the lobby to check on the resident's location. She stated resident #25 was not in the lobby, and the receptionist was on the telephone. She recalled Activity Aide K was working at a board in the lobby and she told her resident #25 said she was going home. The private caregiver stated Activity Aide K denied seeing the resident and continued working at the board. The private caregiver stated she then walked towards the therapy gym and on the way she asked two or three other staff members if they had seen the resident. She recalled she eventually heard an overhead page Code Purple which she was told meant there was a missing resident.
On [DATE] at 2:39 PM, Activity Aide K recalled the morning resident #25 eloped. She confirmed she was in the lobby posting the activity calendar and decorating the notice board. She confirmed the private caregiver approached her and told her resident #25 was confused and said she wanted to go home. Activity Aide K said, I am doing my stuff and I did not see her. I don't know where she went through. She had confusion at times and often says she wants to home. I didn't really pay attention and I continued on doing what I was doing. Activity Aide K stated she did not report the information to the nurse as she had to finish decorating the activity board.
On [DATE] at 12:40 PM, during a tour of the facility with the Maintenance Supervisor, he explained there were sensors for the electronic monitoring system at the front lobby door and the double doors in the hallway that led to the therapy gym. He explained alarms sounded when the sensors were triggered but the doors did not lock, so a resident with an electronic monitoring device could walk through the doors unimpeded. Demonstration of the electronic monitoring system revealed the alarms sounded only at the keypad at a low volume. He stated there were doors on two separate hallways that led into the courtyard, but neither had a sensor to alert staff if residents with monitoring devices exited the building. The Maintenance Supervisor explained prior to resident #25's elopement, residents, visitors, and staff had unlimited access to the courtyard. He verified the gate at the far end of the courtyard had a vertical pull latch that was never locked.
On [DATE] at 2:02 PM, the Social Services Director (SSD) confirmed resident #25 was confused, alert to self only, and regularly wandered around the facility searching for her deceased mother and father. The SSD explained the resident was admitted to the facility for long-term care as she was no longer safe living in the community and required 24-hour care. The SSD verified she participated in discussions about residents during daily IDT meetings and was also responsible for completion of MDS assessment sections related to cognitive status and behavioral symptoms such as wandering. She acknowledged the MDS assessment did not accurately show resident #25's status and exit-seeking behaviors, and her elopement care plan did not reflect details of the care and services to be provided by the facility.
On [DATE] at 10:41 AM, in a telephone interview with resident #25's daughter, she confirmed on the day of admission, the DON asked if her mother wandered. The daughter said, I told her she had gotten out twice when she had a urinary tract infection. She would unlock the gate by sticking her hand through it. The daughter explained her mother left her house and walked to a neighbor's house and had to be brought back home. She stated the family even had to block the front door to prevent her mother from getting out. Resident #25's daughter reiterated the facility was aware of her mother's wandering, agitation, and desire to leave. She explained during the weeks that preceded the elopement, the facility called several times to inform her that her mother was agitated and verbalized wanting to leave and go somewhere.
The facility's policy and procedure Abuse Neglect Exploitation Mistreatment and Misappropriation of Property dated [DATE] revealed it was the policy of the facility to protect its residents from neglect. The document defined neglect as .the failure of the facility, its employees or service providers to provide goods and services to a resident that are necessary to avoid physical harm, pain, mental anguish or emotional distress.
The Facility Assessment Tool dated [DATE], revealed the facility was able to care for residents with impaired cognition, depression, anxiety disorder, behaviors that required interventions, Alzheimer's Disease, and dementia. The document indicated the facility would provide person-centered care by preventing abuse and neglect and identify hazards and risks for residents.
Review of the immediate actions to remove the Immediate Jeopardy implemented by the facility revealed the following, which were verified by the survey team:
*On [DATE], resident #25 eloped from the facility at approximately 8:39 AM. The facility initiated a search, and the resident was not found on the premises. She was located by law enforcement and returned to the facility at approximately 10:14 AM. On return, the resident was immediately assessed by the Nurse Practitioner, noted to have no injuries or abnormalities, and was placed on one-to-one supervision.
*On [DATE], the facility obtained an estimate to add magnet/code alarms to the doors that did not currently have electronic monitoring system sensors/alarms in place. The installation date was scheduled for [DATE].
*On [DATE] at approximately 10:30 AM, a staff member was placed at both emergency exits without electronic monitoring system alarms for 24 hours.
*As of [DATE] at approximately 6:00 PM, all the doors in the facility that did not have the electronic monitoring system alarm were armed with an emergency screamer alarm with a key override. The alarms were checked every two hours to ensure they were in place and functioned. All electronic monitoring devices are checked every shift for placement and functioning. All residents, regardless of cognitive status will have a staff member accompany them when spending time in the courtyard. Every two hours the courtyard gate is checked to ensure that it remains locked.
*On [DATE], the Staff Development Coordinator initiated an in-service to cover Abuse, Neglect, and Reporting Abuse and/or Neglect; and notification to management if a resident begins to seek an exit or express a desire to leave the facility. In-services were also conducted covering the elopement policy, procedure, and prevention. A total of 97% of the staff were in-serviced by [DATE].
*On [DATE], an emergency Quality Assurance and Performance Improvement (QAPI) committee meeting was held to address the identified non-compliance.
*As of [DATE], the DON sends the Corporate Nursing team the projected staffing hours every morning to ensure adequate staff was scheduled to care for the residents.
*On [DATE], the Corporate Nurse Consultant assessed the knowledge of the management team regarding abuse, neglect, elopement, risk management, and reporting specific incidents to specific agencies. The Corporate Nurse Consultant educated the management team on Elopement Prevention, Risk Management, Adverse Incidents, and Reporting.
*On [DATE], the Corporate Nurse Consultant gave instruction on how to conduct, and reviewed the Standards of Care Meeting with the interdisciplinary team. In this weekly meeting, run by the DON, all residents who are potentially at risk for any type of decline, have recently had a change in condition, or been involved in any type of incident are discussed to ensure their needs are anticipated and being met.
*As of [DATE], the Nurse Management Team assesses the residents in the facility and completes an acuity report. This report breaks down specific needs and explains how many residents in the facility require that specific type of care. The Corporate team, and the management team utilize the weekly acuity report in conjunction with the daily staffing hours to ensure there is adequate staff in relation to the acuity of the residents.
*On [DATE], the Corporate Nurse Consultant observed the care of residents provided by all direct care staff throughout the facility for all shifts. The Corporate Nurse Consultant spoke with multiple direct care staff to ensure they were able to adequately care for the current residents.
*On [DATE], the Corporate Nurse Consultant visited multiple patient rooms, spoke with them about the care they received, and reviewed multiple charts to assess whether resident's needs were being met.
*As of [DATE], safety checks were conducted on each resident at risk for elopement.
*On [DATE], the QAPI committee held an emergency meeting on [DATE] to address the identified noncompliance with F600.
*On [DATE], all cognitively intact residents were interviewed by the management team and asked the following questions: a) Have you ever been treated in a way that you feel was abusive by the staff? b) Have you felt neglected by any member of the staff? c) Has anyone spoken to you in way that was verbally abusive? d) Do you feel safe in this facility? e) Do you feel there is adequate staff here at all times to meet your needs?
*On [DATE], a questionnaire was initiated for staff in the facility, asking the following: a) Have you been educated on Abuse, and Neglect? b) If you have been, approximately when was the last time? c) Do you feel that you are knowledgeable about what is expected of you here at work? d) Do you feel that you have everything you need to provide the care that is required of you? e) Do you feel that all the residents are appropriate for this environment and that their needs can be met by the staff? f) Do you feel that there is adequate staff present during all shifts to meet the resident's need?
*On [DATE], responses to the above questions were reviewed with no findings of any residents who felt neglected by the staff. All staff members reported they were recently educated on neglect and abuse and could meet the needs of the residents in their care.
*As of [DATE], all residents regardless of their cognitive status will have a staff member accompany them into the courtyard.
Review of Courtyard Gate Lock Check forms from [DATE] to [DATE] revealed staff completed gate checks with varying frequencies, between every two hours to every six hours.
Review of in-service attendance sheets revealed staff signatures to reflect participation in education on the topics listed above.
On [DATE], interviews were conducted with five Licensed Practical Nurses, three CNAs, one Personal Care Attendant, two Rehab staff, one Activities staff, one maintenance staff and one housekeeper. All verbalized understanding of the education provided.
The resident sample was expanded to include three additional residents who were at risk for elopement. Observations, interviews, and record reviews revealed no concerns for residents #11, #12, and #19 related to neglect.
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide adequate supervision and monitoring of the st...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide adequate supervision and monitoring of the status and activities of a vulnerable, cognitively impaired resident to prevent unsupervised exit from the facility through an unmonitored courtyard for 1 of 4 residents reviewed for elopement, out of a total sample of 32 residents, (#25). This failure contributed to the elopement of resident #25 and placed her at risk for serious injury/impairment/death. While resident #25 was out of the facility unsupervised, there was a likelihood she could have fallen, been accosted by unknown persons, become lost, drowned, or been hit by a car.
On [DATE] at approximately 8:30 AM, resident #25 left the [NAME] Wing dining room and walked away from the unit. Along the way, the resident informed another resident's private caregiver that her ride did not show up, so she would walk home. Facility staff did not notice the resident as she wandered along the hallway or redirect her when she opened a door that led to the courtyard. The resident crossed the courtyard, opened the latch on an unlocked gate, and walked away from the property at approximately 8:38 AM. Resident #25 headed towards the heavily trafficked road in front of the facility, flagged down a passing car, and asked the driver to take her to the high school. The unknown person drove the resident to a high school located over three miles away, left her there, then called 911 to request a wellness check due to concerns about the resident's cognitive status. Meanwhile, at the facility, the private caregiver informed a staff member that resident #25 verbalized her intent to leave and was no longer present in the vicinity of the [NAME] Wing. The staff member disregarded the information and did not alert nursing staff or attempt to locate the resident. Resident #25's assigned nurse discovered she was missing at approximately 9:15 AM and staff initiated a search of the building and its surroundings. The facility was not aware of resident #25's whereabouts until approximately 10:00 AM when law enforcement contacted the resident's son, who retrieved his mother from the high school and returned her to the facility.
The facility's failure to provide the appropriate level of supervision and frequency of monitoring for a resident with known exit-seeking behavior contributed to resident #25's elopement and placed all residents who wandered at risk for serious injury/impairment/death. This failure resulted in Immediate Jeopardy which began on [DATE] and was removed on [DATE].
Findings:
Cross reference F600, F607, F641, F656, and F835.
Review of the medical record revealed resident #25 was an [AGE] year-old female who was admitted to the facility on [DATE], with diagnoses including Alzheimer's Disease, dementia, insomnia, and anxiety.
Review of a Wandering/Elopement Risk Assessment dated [DATE], revealed on admission, nursing staff identified resident #25 was at risk for elopement as she was cognitively impaired, independently ambulatory, and verbalized her intent to leave the facility. Although the assessment form included a recommendation to initiate an elopement care plan to address the identified risk factors for elopement, the admission nurse did not follow the instruction, and resident #25's plan of care did not include approaches to ensure her safety.
Review of the facility's policy and procedure Wandering and Elopements (undated) revealed the facility would identify residents at risk for unsafe wandering. The document read, If identified to be at risk for wandering, elopement, or other safety issues, the resident's care plan will include strategies and interventions to maintain the resident's safety.
Review of resident #25's medical record revealed a physician's order dated [DATE] that read, May go on leave with responsible party. An order dated [DATE] indicated the resident could be treated by a psychologist, and an order dated [DATE] read, Electronic monitoring device to alert staff of residents risk for exit seeking behavior, check placement on left ankle [every shift].
Resident #25 had a care plan for elopement risk related to exit seeking behavior initiated on [DATE] at the time her electronic monitoring device was placed. The care plan goal was the resident would not have any successful elopement attempts. The interventions developed on [DATE] were to update elopement manuals with the resident's information, encourage activities of choice, and check placement and function of her left ankle electronic monitoring device. The care plan did not specify the level of supervision or frequency of monitoring required, nor provide instructions on approaches to ensure the resident's safety during periods of heightened behaviors.
Review of a Daily Skilled Note dated [DATE] revealed the resident was anxious and confused as she wandered throughout the facility, repeatedly verbalized her intent to leave, and successfully managed to open an emergency exit door. Review of the medical record revealed neither the progress notes nor the elopement care plan reflected additional, effective nursing interventions related to verbalization of intent to elope and the actual elopement attempt. The medical record did not show involvement of nursing management or the determination that resident #25 required increased supervision or more frequent monitoring when wandering or exit-seeking. The following day, on [DATE], resident #25's assigned nurse noted she continuously wandered around the unit and informed staff she wanted to leave the facility to go home. Review of a clinical nursing note dated [DATE] revealed resident #25's assigned nurse, Registered Nurse (RN) F, observed the resident in the [NAME] Wing dining room at approximately 8:30 AM that morning. The note indicated RN F discovered the resident was missing approximately 30 to 45 minutes later, and a search of the facility was initiated. The document revealed resident #25 was found away from the facility, and she was retrieved and returned to her room at about 10:30 AM. The elopement care plan was revised on [DATE], after the resident's elopement, to show she required one-to-one supervision.
Review of resident #25's Physical Therapy Plan of Treatment for Rehabilitation dated [DATE] revealed the resident exhibited decreased safety awareness, decreased bilateral lower extremity strength, and impaired overall mobility. The evaluation indicated resident #25 was at increased risk of falls and injury due to decreased awareness of her physical limitations. A Speech Therapy Plan of Treatment for Rehabilitation dated [DATE] revealed the reason for the referral was long-term care placement .due to increasing confusion from Alzheimer's disease resulting in a functional decline in cognitive skills, safety awareness.
On [DATE] at 12:13 PM, Speech Therapist O validated resident #25 did not have the reasoning ability to function in the community. She explained the resident would not be safe unsupervised, whether in the facility, at home or outside the facility. Speech Therapist O said, If she was discharged home, our recommendation would be 24-hour care.
Review of a Psychiatric Evaluation Note dated [DATE] revealed facility staff informed the Psychiatric Nurse Practitioner that resident #25 was confused, wandered the hallways, and was an elopement risk. A Brief Interview for Mental Status exam resulted in a score of five, which indicated severe cognitive impairment. A Psychiatric Subsequent Note dated [DATE] revealed clinical staff reported the resident continued with confusion and anxiety and paced the halls. During the visit, the resident reported the year was 1958, and the practitioner noted the resident had disorganized thought process and loose associations.
Review of a Sheriff's Office Case Report revealed a Deputy Sheriff responded to a report of a suspicious person at a local high school on [DATE] at 9:15 AM. The document indicated the involved party was resident #25 who was described as confused and disoriented. The Deputy Sheriff wrote, She advised she needed to get to school, or she would be late for class. She was convinced that she was a student in school. The report revealed resident #25 was initially seen by a citizen in the area of a nearby middle school and she solicited a ride to the high school. The report indicated the citizen was concerned and called law enforcement to report the encounter. The Deputy Sheriff noted he was able to contact resident #25's son by telephone, and the son explained his mother had severe dementia and was a resident of the facility. The document revealed the resident's son arrived on scene to transport his mother back to the facility.
On [DATE] at 9:35 AM, in a telephone interview, the Deputy Sheriff confirmed he received the initial call for service on [DATE] at 9:15 AM, and responded to the local high school. He stated he learned resident #25 left the facility and walked along the main road in front of the facility and was picked up by a citizen. The Deputy Sheriff stated when he questioned resident #25, she thought she was in Ohio, but was able to provide her name and he was eventually able to find telephone contact information for her son. The deputy stated the son came to the high school to collect his mother and he followed them back to the facility. He stated facility administration informed him new owners had taken over that morning so there was a lot of activity. He said, I confirmed that the Director of Nursing (DON) was there from the previous administration. In the end, I expressed to them there was too much reliance on technology, and it cannot supersede human supervision. He explained although resident #25 wore an electronic monitoring device, it was not a foolproof intervention. The Deputy Sheriff stated there was a pool at the Independent Living facility next door which could be a danger to a confused, wandering resident. He explained he informed the DON that memory care services required a secure facility and adequate supervision. When informed resident #25 had verbalized her intent to leave the facility for weeks and even on the morning she eloped, the Deputy Sheriff said, I told them there are major issues. A predictable event is preventable.
On [DATE] at 1:09 PM, in a telephone interview, resident #25's son stated he was aware his mother eloped from the facility on [DATE]. He said, All I know is she got out and wandered up the road. She got three miles away. They picked her up by the high school. He explained his mother lived in her own home prior to admission to the facility in [DATE]. The son stated the family decided to place her at the facility as there was no one at home to supervise her during the day and she also suffered extreme anxiety when left alone. The son confirmed his mother had wandered to a neighbor's home in the past.
On [DATE] at 1:30 PM, the DON confirmed resident #25 eloped from the facility on [DATE] and was found by law enforcement at a local high school. The DON explained although resident #25 had an electronic monitoring device, there was no sensor with an alarm at the exit door to the courtyard and the gate was not locked. She stated the resident was last seen in the [NAME] Wing dining room by multiple Certified Nursing Assistants (CNAs) and another resident's private caregiver at about 8:30 AM. The DON stated resident #25 left the dining room, informed the private caregiver she was leaving the facility, and the private caregiver shared that information with Activity Aide K. The DON acknowledged Activity Aide K did not act on the report and returned to her duties. Review of staff statements with the DON revealed none of the CNAs on the [NAME] Wing were aware resident #25 left the unit until the assigned nurse noticed she was missing approximately 30 to 45 minutes later. The DON stated the facility notified the resident's family that their mother was missing and when the son arrived he was upset, asked how it happened, and said, This is why we brought her here.
On [DATE] at 3:04 PM, CNA G stated on the day resident #25 eloped she last saw her in the [NAME] Wing dining room at approximately 8:30 AM. CNA G did not recall if she was assigned to care for the resident that day and she was not aware resident #25 was missing until an overhead page alerted all staff to search for her. CNA G recalled when resident #25 was returned to the facility, her jeans were wet, almost to her knees. She said, If she went through the ditch, that's probably why. We had rain a few days.
On [DATE] at 2:02 PM and 3:30 PM, the Social Services Director (SSD) confirmed resident #25 was confused, had memory deficit, and often wandered throughout the facility searching for her deceased mother and father. The SSD explained the resident was admitted for long-term care and would not be safe in the community without 24-hour care. She said, Once we accept new residents we have to meet their needs.
On [DATE] at 1:11 PM, the Maintenance Supervisor described resident #25's elopement route. He stated security camera footage showed the resident pushed on the [NAME] Wing hallway exit doors to the courtyard, followed the path to the far end of the courtyard, unlatched the gate and walked away, out of camera range. The Maintenance Supervisor demonstrated how resident #25 would have easily been able to reach through the bars on the gate and release the latch located at waist-level. He stated the elopement occurred a few days after a hurricane brought between nine and fourteen inches of rainfall to the area. The Maintenance Supervisor said, There was a lot of standing water for a while. He stated water in the [NAME] in front of the facility was above ankle-deep, and there was a deeper drainage ditch and culvert on the opposite side of the street.
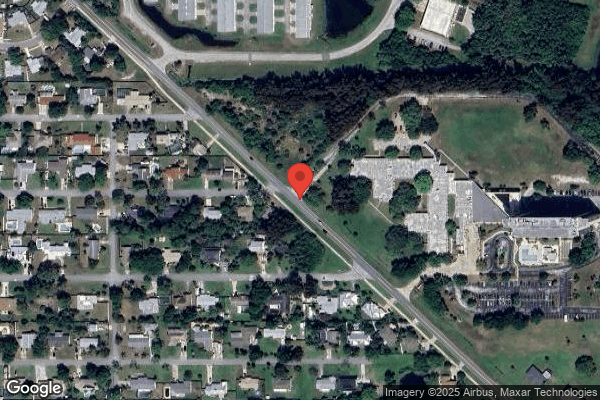
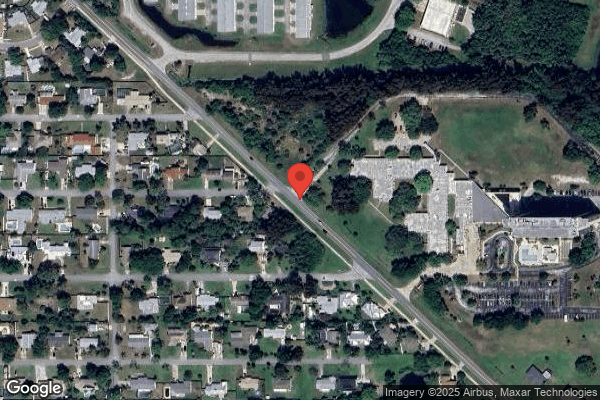
Review of the area map revealed resident #25 walked away from the facility towards the south, and followed the heavily trafficked, major thoroughfare for approximately 0.5 miles until she arrived at the middle school. There was no sidewalk on that side of the road, and she would have crossed a driveway, passed a heavily wooded area, and walked through standing water of unknown depths along the uneven terrain. The resident was picked up by a citizen who drove her approximately 3.5 miles to the high school which was located near a major intersection and a six-lane highway (retrieved on [DATE] from www.google.com/maps).
On [DATE] at 5:20 PM, RN F stated she was resident #25's assigned nurse on the day she eloped. She recalled she saw the resident eating breakfast and approximately 30 to 45 minutes later she realized the resident was nowhere to be found. RN F stated the resident would often ask about the location of the front door or where she could get a taxi or the bus. She explained staff would try to redirect her, but that strategy was not usually very effective. RN F explained the electronic monitoring device was in place to prevent elopement and was checked by nurses every shift. She stated she had not yet checked the resident's device when she eloped. RN F said, I knew she had to be watched, absolutely.
On [DATE] at 9:49 AM, the DON stated resident #25's family did not inform the facility she had exit-seeking behavior prior to admission. However, she acknowledged within four days of admission, the facility identified the resident was at risk for elopement and placed an electronic monitoring device, an intervention to promote her safety. The DON was informed the medical record included frequent nursing documentation after placement of the device related to the resident's behaviors such as wandering, exit-seeking, and verbalizing her intent to leave the facility. She stated she was not aware of the extent and impact of resident #25's behaviors, especially the nighttime agitation and wandering, and acknowledged the care plan did not show additional interventions including increased supervision were discussed by nursing management.
On [DATE] at 10:41 AM, in a telephone interview, resident #25's daughter stated on the day of admission, she informed the DON her mother had wandered away from home on two occasions in the past. She stated her mother was definitely not safe during the period she was out of the facility unsupervised. She said, It was days after the hurricane and there was water ankle-deep to waist-deep outside the facility. The daughter recalled when her mother was found she wore canvas slip-on shoes with low-cut socks, and her jeans were wet to the knees. She stated she was concerned as her mother could not swim. On return to the facility, the daughter noted and informed staff that her mother had a loose ankle bracelet. The resident's daughter recalled her mother informed her she had been trying to remove the device the previous day.
The Facility Assessment Tool dated [DATE] revealed the facility was able to care for residents with impaired cognition, Alzheimer's Disease, dementia, depression, anxiety, and behaviors that required interventions. The document indicated staff received mandatory dementia management training and were competent in caring for residents Alzheimer's Disease and other dementias.
Review of the immediate actions to remove the Immediate Jeopardy implemented by the facility revealed the following, which were verified by the survey team:
*On [DATE], resident #25 eloped from the facility through the courtyard gate at approximately 8:39 AM. The facility initiated a search, and the resident was not found on the premises. She was located by law enforcement and returned to the facility at approximately 10:14 AM. On return, the resident was immediately assessed by the Nurse Practitioner, and there were no injuries or abnormalities. Resident #25 was immediately placed on one-to-one supervision.
*On [DATE], the facility completed a facility-wide re-assessment of each resident's risk for elopement. All residents deemed to be at risk were provided with an electronic monitoring device to alert staff of resident's risk of exit seeking. The residents deemed to be at risk for elopement had care plans updated to reflect this assessment. No additional residents were determined to have exit seeking behaviors or made statements in reference to leaving facility. All residents deemed to be at risk for elopement, receive safety checks every 15 minutes to ensure they are safely in the facility.
* As of [DATE], upon admission, all residents will be assessed to determine their elopement risk. Residents identified to be at risk for elopement will be provided with an electronic monitoring device, and an elopement risk care plan, and will receive safety checks every 15 minutes to ensure that they are still safely in the facility.
*On [DATE], the facility obtained an estimate to add magnet/code alarms to the doors that did not currently have electronic monitoring system sensors/alarms in place. The installation date was scheduled for [DATE].
*On [DATE] at approximately 10:30 AM, a staff member was placed at both emergency exits without electronic monitoring system alarms for 24 hours.
*As of [DATE] at approximately 6:00 PM, all the doors in the facility that did not have the electronic monitoring system alarm were armed with an emergency screamer alarm with a key override. The alarms were checked every two hours to ensure they were in place and functioned. All electronic monitoring devices are checked every shift for placement and functioning. All residents, regardless of cognitive status will have a staff member accompany them when spending time in the courtyard. Every two hours the courtyard gate is checked to ensure that it remains locked.
*On [DATE], the Staff Development Coordinator initiated an in-service to cover elopement prevention, electronic monitoring alarm system, screamer alarm system, courtyard supervision, monitoring of residents who are at risk for elopement; and notifying management of residents who are exit-seeking, and those that express a desire to leave the facility. A total of 97% of the staff were in-serviced by [DATE].
*On [DATE], an emergency Quality Assurance and Performance Improvement (QAPI) committee meeting was held to address the identified non-compliance.
* As of [DATE], safety checks are conducted on each resident at risk for elopement.
*On [DATE], the QAPI committee held an emergency meeting on [DATE] to address the identified noncompliance with F689.
Review of Courtyard Gate Lock Check forms from [DATE] to [DATE] revealed staff completed gate checks with varying frequencies, between every two hours to six hours.
Review of in-service attendance sheets revealed staff signatures to reflect participation in education on the topics listed above.
On [DATE], interviews were conducted with five LPNs, three CNAs, one Personal Care Attendant, two Rehab staff, one Activities staff, one maintenance staff and one housekeeper. All verbalized understanding of the education provided.
The resident sample was expanded to include three additional residents who were at risk for elopement. Observations, interviews, and record reviews revealed no concerns for residents #11, #12, and #19 related to supervision.
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility's administration failed to effectively utilize its resources to...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility's administration failed to effectively utilize its resources to mitigate vulnerabilities in the electronic wander monitoring system; failed to maintain a secure environment to prohibit unauthorized entry and egress through the courtyard; and failed to oversee the implementation of policies and procedures and interdisciplinary team (IDT) processes to ensure the safety of 5 of 5 physically and/or cognitively impaired residents identified to be at risk for elopement, of a total sample of 32 residents, (#11, #12, #14, #19 & #25). These failures contributed to the elopement of resident #25 and placed her at risk for serious injury/impairment/death. While resident #25 was out of the facility unsupervised, there was likelihood she could have fallen, been accosted by unknown persons, become lost, drowned, or been hit by a car.
On 10/03/22 at approximately 8:30 AM, resident #25 left the [NAME] Wing dining room and walked away from the unit. Along the way, the resident informed another resident's private caregiver that her ride did not show up, so she would walk home. Facility staff did not notice the resident as she wandered along the hallway or redirect her when she opened a door that led to the courtyard. The resident crossed the courtyard, opened the latch on an unlocked gate, and walked away from the property at approximately 8:38 AM. Resident #25 headed towards the heavily trafficked road in front of the facility, flagged down a passing car, and asked the driver to take her to the high school. The unknown person drove the resident to a high school located over three miles away, left her there, then called 911 to request a wellness check due to concerns about the resident's cognitive status. Meanwhile, at the facility, the private caregiver informed a staff member that resident #25 verbalized her intent to leave and was no longer present in the vicinity of the [NAME] Wing. The staff member disregarded the information and did not alert nursing staff or attempt to locate the resident and instead, returned to her duties. Resident #25's assigned nurse discovered she was missing at approximately 9:15 AM and staff initiated a search of the building and its surroundings. The facility was not aware of resident #25's whereabouts until approximately 10:00 AM when law enforcement contacted the resident's son, who retrieved his mother from the high school and returned her to the facility.
The facility's failure to maintain a safe and secure environment and implement policies and procedures to prevent neglect and elopement placed all residents who wandered and/or had access to the courtyard at risk. This failure resulted in Immediate Jeopardy starting on 10/03/22. The Immediate Jeopardy was removed on 11/09/22. The scope and severity of the deficiency was decreased to D, no actual harm, with potential for more than minimal harm, that is not Immediate Jeopardy after verification of the facility's immediate corrective actions.
Findings:
Cross reference F600, F607, F641, F656, and F689.
Review of the medical record revealed resident #25 was an [AGE] year-old female who was admitted to the facility on [DATE], with diagnoses including Alzheimer's Disease, dementia, insomnia, and anxiety.
On 11/07/22 at 1:30 PM, the facility's Administrator and Director of Nursing (DON) confirmed resident #25 eloped from the facility on 10/03/22. The DON stated the incident investigation identified the root cause as a weak link in facility security related to the absence of electronic monitoring system sensors at the courtyard doors and an unlocked gate. The Administrator and DON could not provide documentation of an investigation with a focus on identification and prohibition of Neglect according to regulatory requirements and facility policy and procedure. The Administrator acknowledged the facility took actions to secure the courtyard after the elopement occurred.
On 11/09/22 at 12:21 PM, the Administrator explained he did not have access to the reporting system required for submission of investigations related to allegations of abuse and neglect although he was the facility's designated Risk Manager.
Review of the facility's policy and procedure Abuse Prevention Program revised in July 2020, indicated the facility would identify and assess all possible incidents of abuse, neglect, or mistreatment. The document revealed the Administrator was responsible for overall implementation of the policies and procedures that prohibited neglect.
Review of the facility's policy and procedure for Wandering and Elopements revised in December 2020 revealed the facility would identify residents who were at risk for wandering and elopement and develop appropriate strategies and interventions to maintain safety.
Review of the facility's policy and procedure Care Plans, Comprehensive Person-Centered revised in November 2020 revealed the Interdisciplinary Team (IDT) was responsible for review and revision of residents' care plans when the desired outcome is not met.
On 11/09/22 at 9:49 AM, the DON stated she was not made aware of the concerns related to resident #25's continuous, escalating wandering and exit-seeking behaviors in IDT meetings. The DON confirmed the IDT conducted daily meetings and group huddle meetings prior to the resident's elopement. She validated the IDT discussion process was not as effective as it should have been.
On 11/09/22 at 11:33 AM, the Medical Records staff stated she attended daily IDT meetings during which orders and incidents were reviewed. She confirmed information related to issues such as placement of resident #25's electronic monitoring device, her increased behaviors, and elopement attempts should be discussed. When asked about the effectiveness of IDT meeting discussions, the Medical Records staff said, Sometimes there are lots of side conversations.
On 11/07/22 at 2:08 PM, the Administrator retraced the resident's elopement route through the courtyard. He acknowledged prior to the event; the facility's administration was aware there were no sensors for the electronic monitoring system at the courtyard doors to alert staff that residents with these devices had exited the building. Observation of the exterior exit gate revealed standing A-frame sign boards that measured approximately three feet from the ground on both sides of the gate. The signs had instructions regarding not using the gate for entry or egress. The Administrator moved the signs and unlatched the gate. He stated the gate was never locked as it was a fire exit, but the new security system would enable the gate to be locked and automatically open if the fire alarm triggered. The Administrator acknowledged the gate remained an unsecured point of entry and exit.
On 11/08/22 at 12:40 PM, the Maintenance Supervisor demonstrated and acknowledged weaknesses in the facility's electronic monitoring system included protected doors did not lock to prevent exit when the alarm was triggered; alarms sounded from the keypads and were not audible in other areas of the facility such as nurses' stations; and the system was not installed at the doors that led to the courtyard. The Maintenance Supervisor explained he had been on staff for over seven years, and during that time the courtyard doors never had alarms, and the gate was always unlocked. He confirmed prior to resident #25's elopement, residents, visitors, and staff had unlimited access to the courtyard.
Review of the medical records revealed concerns related to placement of electronic monitoring devices on wheelchairs rather than on the residents' extremities. Resident #11 had a physician's order dated 7/25/22 for an electronic monitoring device to his wheelchair. Resident #12 had a physician's order dated 9/20/22 for an electronic monitoring device to be attached to his wheelchair and resident #19 had an order dated 9/19/19 for a device on her wheelchair.
On 11/08/22 at approximately 5:30 PM, the Administrator, DON, and Corporate Nurse were informed that review of physician orders revealed some residents had electronic monitoring devices placed on their extremities and others had the devices placed on their wheelchairs. They were unaware of any manufacturer's recommendations regarding placement of the monitoring devices.
Review of the electronic monitoring system manufacturer's instructions revealed the device was to be worn on either the wrist or ankle. The User Guide read, The range, accuracy, function, and performance. of the device may be affected by factors including metal objects in the vicinity and placement of the device.
On 11/09/22 at 4:14 PM, the Staff Development Coordinator (SDC) stated she had been on staff for almost six years and was never made aware of the manufacturer's recommendations regarding placement of electronic monitoring devices. The SDC stated after the administrative team was questioned about the different locations of residents' devices, they reviewed the manufacturer's manual and discovered the device must be placed on the resident and not on wheelchairs.
On 11/09/22 at 4:23 PM, the Administrator stated the facility's Quality Assurance and Performance Improvement (QAPI) committee met once monthly to review of quality measures, grievances and customer service issues, Resident Council meeting minutes, and other key indicators. The Administrator stated in addition to the monthly QAPI meetings, the IDT reviewed issues that impacted resident care and services including changes in resident status in daily morning meetings and huddle meetings. He explained the QAPI committee also received information from employees by way of concerns reported to a supervisor or in town hall meetings, staff meetings and departmental meetings. The Administrator stated prior to resident #25's elopement, the facility's administration was aware the courtyard gate was unlocked, and that the electronic monitoring system did not trigger doors to lock in response to wandering and elopement attempts. He explained, No [resident] had gone in and out of the back gate until that resident left. The Administrator confirmed the IDT, administrative team, and QAPI committee had not identified concerns related to person-centered care plans.
The Facility Assessment Tool dated 11/19/21, revealed the facility would provide person-centered care by identifying hazards and risks for residents. The assessment listed physical environment and building needs but did not include the electronic monitoring system or the courtyard fencing and gate.
Review of the immediate actions to remove the Immediate Jeopardy implemented by the facility revealed the following, which were verified by the survey team:
*On 10/03/22, resident #25 eloped from the facility through the courtyard gate at approximately 8:39 AM. The facility initiated a search, and the resident was not found on the premises. She was located by law enforcement and returned to the facility at approximately 10:14 AM. On return, the resident was immediately assessed by the Nurse Practitioner, and there were no injuries or abnormalities. Resident #25 was immediately placed on one-to-one supervision.
*On 10/03/22, the facility obtained an estimate to add magnet/code alarms to the doors that did not currently have electronic monitoring system sensors/alarms in place. The installation date was scheduled for 11/10/22.
*On 10/04/22, the Nurse Consultant of Education educated the management team on Elopement Prevention, Risk Management, and Adverse Incidents.
*As of 10/03/22, upon admission, all residents will be assessed to determine their elopement risk. Residents identified to be at risk for elopement will be provided with an electronic monitoring device, and an elopement risk care plan.
*On 10/03/22, the DON conducted an Elopement drill to obtain a baseline and assess for weakness in following the protocol.
*As of 10/03/22, elopement drills will be conducted monthly on a different shift each month. Each shift will have an elopement drill at least once every quarter.
* On 10/04/22, an Emergency QAPI committee meeting was held to address the identified non-compliance.
*On 10/18/22, another elopement drill was conducted to assess improvement after education.
*On 11/08/22, the user manual for the Wander guard system was reviewed to ensure that all components are being utilized as intended.
*On 11/08/22, the QAPI committee held an emergency meeting to address the identified noncompliance with F835.
Review of in-service attendance sheets revealed management staff signatures to reflect participation in education on the topics listed above, and staff signatures for participation in elopement drills.
The resident sample was expanded to include three additional residents who were at risk for elopement. Observations, interviews, and record reviews were conducted for residents #11, #12, and #19 revealed concerns related to placement of their electronic monitoring devices.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to inform the resident representative(s) of a change in condition rela...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to inform the resident representative(s) of a change in condition related to placement of an electronic monitoring device for exit-seeking behavior, for 1 of 4 residents reviewed for elopement of a total sample of 32 residents, (#25).
Findings:
Review of resident #25's medical record revealed she was admitted to the facility on [DATE]. Her diagnoses included Alzheimer's Disease, dementia, insomnia, and anxiety. The resident's demographic information sheet listed her son and daughter as responsible parties.
A Wandering/Elopement Risk Assessment dated 9/16/22 revealed on admission, the resident's elopement risk score was two on a scale from zero to nine. The assessment did not trigger a care plan with interventions related to monitoring resident #25 for wandering and/or exit seeking behaviors.
The Minimum Data Set (MDS) admission assessment with assessment reference date of 9/22/22 revealed resident #25 had a Brief Interview for Mental Status score of four, which indicated she had severe cognitive impairment. Section F0400 Interview for Daily Preferences revealed it was very important to the resident to have her family involved in discussions regarding her care. Section Q0100 of the MDS assessment noted the resident's family participated in the assessment.
Review of a Daily Skilled Note dated 9/19/22 indicated resident #25 was confused, ambulated up and down the hallways, and required frequent redirection. Licensed Practical Nurse (LPN) P noted an electronic monitoring bracelet was placed on the resident.
Review of the September 2022 Physician Order Sheet revealed on 9/20/22, resident #3's attending physician ordered an electronic monitoring device to alert staff of residents risk for exit seeking behavior. Review of an order detail form dated 9/20/22 at 8:49 AM showed the order was obtained and signed by the facility's Assistant Director of Nursing (ADON).
A care plan for elopement risk related to exit seeking was initiated on 9/20/22. The interventions included check placement and function of an electronic monitoring device placed on resident #25's left ankle.
Review of Daily Skilled Note forms and a Clinical Notes Report for September and October 2022 revealed no documentation of notification of resident #25's representatives regarding placement of their mother's electronic monitoring device or her exit-seeking behavior.
On 11/09/22 at 11:33 AM, the Medical Records staff stated she thoroughly reviewed resident #25's medical record and did not find any Situation, Background, Assessment, Recommendations (SBAR) forms which were used to document changes in condition and notifications made to the physician and resident's representative.
On 11/09/22 at 11:35 PM, the Registered Nurse Staff Development Coordinator confirmed placement of an electronic monitoring device would require notification to a resident's representative. She explained the medical record should include documentation of details of the notification in an SBAR form or a nursing progress note.
On 11/09/22 at 12:21 PM, the Director of Nursing confirmed a change in condition form was necessary when resident #25's behaviors escalated and the physician determined she required an electronic monitoring device. She stated nursing staff should have notified the resident's family regarding her escalating behavior and the need for a device as it was a change in her treatment.
On 11/09/22 at 1:41 PM, LPN P confirmed she was the assigned nurse on the day the ADON obtained the physician's order to place an electronic monitoring device on resident #25. She stated she did not contact the resident's family regarding the new order. LPN P explained she was not aware a change in condition form was required in that situation. However, she said, Family should have been notified.
On 11/09/22 at 10:41 AM, in a telephone interview, resident #25's daughter stated the facility did not notify her when her mother received an electronic monitoring device. The daughter explained she noticed the device on her mother's ankle on 10/03/22, the day she eloped from the facility.
On 11/09/22 at 11:07 AM, in a telephone interview, resident #25's son stated he was listed as his mother's primary contact but was never notified by the facility of placement of an electronic monitoring device. Resident #25's son explained he found out about the device on the day his mother eloped and had to be brought back to the facility. He said, My sister saw it and told me.
Review of the facility's policy and procedure Change in a Resident's Condition or Status revised in August 2021, revealed the facility would promptly notify the resident's representative of changes in condition and/or status. The document indicated a nurse was expected to notify the resident's representative of any significant change in the resident's medical or mental condition or status. The policy described a significant change in condition as a decline or improvement that would not resolve itself without intervention and requires interdisciplinary review and/or revision to the care plan.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to implement policies and procedures to identify and prevent neglect ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to implement policies and procedures to identify and prevent neglect by thoroughly investigating and accurately reporting an elopement incident for 1 of 4 residents reviewed for elopement, out of a total sample of 32 residents, (#25).
Findings:
Cross reference F600, F641, F656, F689, and F835.
Review of resident #25's medical record revealed she was admitted to the facility on [DATE] with diagnoses including Alzheimer's Disease, dementia, insomnia, and anxiety.
Review of a clinical nursing note dated 10/03/22 revealed resident #25's assigned nurse, Registered Nurse (RN) F, observed the resident in the [NAME] Wing dining room at approximately 8:30 AM that morning. The note indicated RN F discovered the resident was missing approximately 30 to 45 minutes later, and a search of the facility was initiated. The document revealed at about 10:00 AM, RN F was informed resident #25 had been found outside the facility, and she was retrieved and returned to her room at about 10:30 AM.
Review of the facility's policy and procedure Abuse Prevention Program revised in July 2020, defined neglect as a failure to provide a resident with the goods and services necessary to avoid physical harm, mental anguish, or emotional distress. The policy indicated the facility would identify and assess all possible incidents of abuse, neglect or mistreatment.
The facility's policy and procedure Abuse Neglect Exploitation Mistreatment and Misappropriation of Property dated October 2020 revealed it was the policy of the facility to protect its residents from neglect. The document indicated the facility would conduct prompt and thorough investigations of any allegation or suspicion of neglect. The procedure revealed the facility's Risk Manager would oversee and direct investigations, which involved interviewing witnesses and documenting all information, compiling a report that included statements, photographs and copies of records, and reporting investigative findings to the appropriate agencies.
On 11/07/22 at 1:18 PM, the facility's Administrator stated he was the Risk Manager and confirmed he was responsible for the investigation and reporting of adverse incidents and allegations of abuse and neglect. He stated the facility submitted the required Federal 1-day and 5-day reports and also the 15-day State adverse incident report. He was not able to provide proof of submission of the Federal reports or documentation of an investigation related to suspicion of possible neglect related to resident #25's elopement. The Administrator explained the Director of Nursing (DON) had a binder with complete documentation of the incident investigation.
On 11/07/22 at 1:30 PM, during review of the facility's elopement investigation binder with the DON, she was unable to show that the incident was investigated with a focus on determining if neglect occurred, and she could not provide copies of the required Federal 1-day and 5-day reports. The DON showed statements collected from resident #25's assigned nurse and other staff who were in the facility at the time of the elopement, but none specified which Certified Nursing Assistant (CNA) was assigned to care for the resident. The DON stated the facility's investigation revealed on 10/03/22, the resident exited the facility's courtyard through a gate at approximately 9:05 AM and was found and returned to the facility by a law enforcement officer at approximately 10:14 AM. She stated law enforcement was notified within 20 to 30 minutes after staff noted the resident was missing. However, the facility's call to law enforcement was not recorded in the investigation documentation. The DON stated she obtained and documented a verbal statement from the law enforcement officer regarding the circumstances of his encounter with the resident, but she was unable to show either the statement or a copy of the sheriff's office report in the investigation binder. When asked if the facility had security cameras near the exit doors and/or courtyard area, the DON said, There was video footage but it recorded over itself and we do not have a copy. The DON stated when resident #25 eloped she was dressed appropriately in jeans, a shirt, and tennis shoes, and when she returned there was no evidence of a fall or any injuries.
On 11/07/22 at 3:04 PM, CNA G stated on the day resident #25 eloped, she last saw her in the [NAME] Wing dining room eating breakfast. CNA G did not remember if she was assigned to care for the resident on that day. CNA G recalled when resident #25 was found and returned to the facility, she assisted with removing her clothing. CNA G stated the legs of resident #25's jeans were wet, almost to her knees. She said, If she went through the ditch, that's probably why. We had rain a few days. She stated the resident was not wearing tennis shoes, rather she wore soft, canvas, slip-on flats.
Review of CNA G's written statement revealed she last saw resident #25 on 10/03/22 at approximately 8:45 AM, but it did not reflect responses to effective investigative questions by the Risk Manager or DON. The document did not indicate she was the assigned staff member, nor provide details of her interactions with the resident from the beginning of the day shift until she eloped from the facility unsupervised. The statement omitted a description of the resident's clothing or status upon return to the facility.
On 11/08/22 at 1:05 PM, during a tour of facility's courtyard, the Maintenance Supervisor pointed to the locations of security cameras. He confirmed he watched videos that showed resident #25 enter and cross the courtyard before she exited through the gate on the day she eloped. Contrary to the DON's statement on 11/07/22 at 1:30 PM, the Maintenance Supervisor stated the facility retained a copy of the video.
On 11/08/22 at 2:58 PM, review of the video recording of resident #25's elopement with the Administrator, DON, and Maintenance Supervisor showed the resident opened the door that led from the [NAME] Wing hallway to the courtyard at approximately 8:36 AM, and she exited through the gate at the far side of the courtyard at approximately 8:38 AM. The timestamped video conflicted with the facility's incident investigation report which indicated the resident exited through the courtyard gate at 9:05 AM. The video also showed the resident did not wear tennis shoes as reported by the DON.
On 11/09/22 at 9:27 AM, the DON was asked to clarify the discrepancies and omissions identified in the the facility's investigation, and to explain how the facility investigated and ensured neglect was not substantiated related to the elopement. She stated the facility's process was for the Social Services Director, Administrator and herself to investigate all avenues related to allegations of neglect and abuse. She confirmed the resident was transported back to the facility by her son and not the deputy sheriff as noted in the facility's investigation. The DON explained the facility's timeline was determined by staff statements and not the video. The DON acknowledged she saw the video prior to submitting the final State adverse incident report, but she was not aware of the timestamp and discrepancies with the staff statements.
On 11/09/22 at 12:21 PM, the Administrator was informed the required Federal 1-day and 5-day reports were never submitted by the facility as evidence that a thorough investigation had been conducted to rule out neglect. He said, We investigated the incident and it was a good faith effort. The Administrator verified he had been the facility's Risk Manager for about one year, but did not have access to the system used to file reports related to possible abuse or neglect.
Review of the job description for Nursing Home Administrator (undated), revealed he would effectively manage the operations of the facility according to federal and state regulations. The Administrator's duties and responsibilities included ensure all staff strictly adhere to the Facility abuse policies and procedures.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to report an alleged violation of verbal abuse for 1 of 2 residents re...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to report an alleged violation of verbal abuse for 1 of 2 residents reviewed for abuse/neglect of a total sample of 32 residents, (#41).
Findings:
Review of resident #41's medical record revealed he was re-admitted to the facility on [DATE] with diagnoses of hemiplegia, intracranial hemorrhage, falls, cognitive communication deficit and anxiety disorder. Review of the quarterly Minimum Data Set (MDS) assessment dated [DATE] revealed a Brief Interview for Mental Status score of 14/15 that indicated he was cognitively intact.
Review of the facility incident log showed resident #41 voiced an allegation of abuse dated 9/16/22. Review of the medical record revealed documentation of Alleged Abuse by the Director of Nursing (DON) dated 9/16/22 which read, Resident came back from appointment for a doppler test .resident was upset with aide .he states she was on the phone the whole time, when he told her to get off the phone, she told him to [Shut up] and knocked his hat off his head. She also said, [this is my phone, I pay the bill, I can use it when I want] .
On 11/9/22 at 11:27 AM, the Social Services Director (SSD)/Abuse Coordinator said, the DON informed me there was a situation at an appointment involving resident #41 and Certified Nursing Assistant (CNA) G. The SSD said, the facility filed an immediate report but did not do a 5-day report. The SSD added she was new to the Abuse Coordinator position and the Administrator and DON were helping her with the investigation.
On 11/9/22 at 11:40 AM, the Administrator reviewed the alleged abuse documentation dated 9/16/22 by the DON and acknowledged the facility should have reported this abuse allegation to the State Agency by doing an immediate and 5-day report.
On 11/9/22 at 3:36 PM, the DON said she was not able to provide statements collected from CNA G regarding the incident as the forms were located offsite and not available. She explained that when she called her corporate office to report the incident, they instructed her to contact Department of Children and Family Services (DCF). She indicated the incident did not meet DCF's criteria and they did not accept the case. She acknowledged the facility did not file an immediate or 5-day report with the State Agency and noted, You are right, we should have and because the SSD is new to Abuse Coordinator role, her idea of an immediate report was notifying DCF and she did not realize that 1 and 5-day reports to the State Agency were required. The DON acknowledged that for a caregiver to tell a resident to shut up would be considered verbal abuse. She noted an immediate report was not filed and they did not have supporting documentation such as resident, CNA, or van driver statements that would have been included with doing a thorough investigation.
Review of the facility policy and procedure for Abuse Prevention Program revised 7/2020, read, Our residents have the right to be free from abuse .This includes, but is not limited to .verbal .As part of the resident abuse prevention, the administration will .Report all allegation of abuse within timeframes as required by federal requirements and immediately notify the following: a. Report the allegation immediately to Department of Children and Families .Notify AHCA immediately per federal and state reporting requirements .Verbal Abuse is defined as the use of oral written or gestured language. That willfully includes disparaging and derogatory terms to residents .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to provide written notification of transfer and discharge to their re...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to provide written notification of transfer and discharge to their residents/representatives nor copy to the Ombudsman for 1 of 3 residents reviewed for appropriate discharge out of a total sample of 32 residents, (#53).
Findings:
Review of resident #53's medical record revealed he was admitted to the facility on [DATE] and readmitted on [DATE]. His diagnoses included chronic obstructive pulmonary disease, atrial fibrillation, and heart failure.
Review of the discharge Minimum Data Set (MDS) with Assessment Reference Date (ARD) of 7/14/22 revealed resident #53 was transferred to an acute care hospital and his return was anticipated. A second discharge MDS with ARD 8/16/22 revealed resident #53 had a planned discharge to the community and his return was not anticipated.
Review of resident #53's medical record revealed he was hospitalized on [DATE]. A progress note dated 7/14/22 included the resident was observed on the floor on his back by the foot of the bed and legs extended out in front of him and was noted slurring his speech. The Advanced Practice Registered Nurse was contacted and ordered for the resident to be transferred to the hospital. A progress note dated 8/16/22 indicated resident #53 was discharged to his daughter's house with home care services in place. The medical record did not include a copy of the Agency for Healthcare Administration (AHCA) Nursing Home Transfer and Discharge Notice, Form 3120. There was no evidence that written notification of transfer and discharge was given to the resident nor sent to the Ombudsman.
On 11/09/22 at 10:37 AM, the Social Services Director (SSD) indicated she was responsible for initiating the discharge plan upon admission and finalized the process for all residents discharged to the community. She explained throughout the resident's stay, she communicated with the resident and family and members of the interdisciplinary team to learn of the resident's progress and get ready when a discharge date was near. She confirmed resident #53 went home with his daughter. She explained he received a discharge summary and a list of his medications at discharge. When asked for the copy of the AHCA Form 3120, she stated she did not know who completed such form. She indicated the business office completed and provided the resident with the NOMNC. The SSD stated she was not sure who informed the Ombudsman about transfers or discharges. At 1:02 PM and 2:42 PM, the SSD stated she could not locate the AHCA form, and explained the nurses used an internal transfer form when residents were sent to the hospital.
On 11/09/22 at 2:35 PM, the MDS Coordinator stated she handled the discharges before the current SSD began working at the facility. She indicated she was not familiar with the AHCA Form 3120 and did not recall ever seeing it. She noted when she handled the discharges, she never sent notification to the Ombudsman.
On 11/09/22 at 2:46 PM, the Business Office Manager stated the discharge process was done by the SSD. She explained after the SSD left, everyone helped, and she took over handling the NOMNC. She explained she gave the NOMNC within 2 days of the resident's discharge. She indicated therapy usually let her know when they were 5 days from completing their services, which gave her time to give the NOMNC. She explained she was not familiar with the AHCA form. She noted the NOMNC was the only form she was aware of and was issued when a resident requested the discharge or his/her goals were met. She indicated she was not involved when a resident was transferred to the hospital.
On 11/09/22 at 2:50 PM, the Administrator stated there was no SSD when he started working working at the facility, so he divided the SSD duties amongst the staff. He indicated he was familiar with the process of a facility-initiated discharge and it did not include providing the AHCA form for transfers to the hospital as ordered by the physician, when a resident was admitted short-term and met his/her goals or if the resident expressed he/she wanted to go home. He explained the facility used the NOMNC and gave them a 3-day notice and communicated with the resident and the family about the discharge. The Administrator indicated he was aware a list of residents who were discharged needed to be sent to the Ombudsman, usually at the end of the month. He stated he was not aware this was not being sent and said, That is an easy fix.
The job description for the Director of Social Services revealed responsibilities which included, Participate in the development and implementation of discharge plans of care. Involve the resident/family in planning objectives and goals, including discharge, for the resident.
The facility's policy and procedure Transfer/Discharge dated 12/2021 read, The resident and/or representative (sponsor) will be notified of the reason(s) for the transfer or discharge and the reason(s) will be documented in the resident's medical record. The policy did not include information about written notification to its residents nor the Ombudsman.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop a person-centered care plan with specific interventions to ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop a person-centered care plan with specific interventions to ensure the provision of appropriate care and services to meet the needs of 1 of 4 residents reviewed for elopement of a total sample of 32 residents, (#25).
Findings:
Cross reference F600, F607, F641, F689, and F835.
Review of resident #25's medical record revealed she was admitted to the facility on [DATE] with diagnoses including Alzheimer's Disease, dementia, insomnia, and anxiety.
Resident #25's admission Wandering/Elopement Risk Assessment dated 9/16/22, included instructions for nurses on obtaining pertinent information and implementing follow up as indicated. The document read, The following questions are to be asked of the resident and/or responsible party upon admission/readmission to determine the resident's risk for elopement. The assessment showed two questions had responses of yes related to the resident being cognitively impaired and independently ambulatory, and verbalizing her intent to leave the facility. Additional instructions on the form read, If assessment indicates 'YES' to any question, consider initiating a care plan or service plan for elopement risk. However, the section of the document designated for development of a care plan was left blank.
Review of the facility's policy and procedure Wandering and Elopements (undated) revealed the facility would identify residents at risk for unsafe wandering. The document read, If identified to be at risk for wandering, elopement, or other safety issues, the resident's care plan will include strategies and interventions to maintain the resident's safety.
Review of Daily Skilled Note forms revealed on 9/17/22 resident #25 had been awake since early that morning searching for her mother and father. A note dated 9/19/22 indicated she was confused, ambulated up and down the hallways, and required frequent redirection. As a result, staff placed an electronic monitoring device on the resident during that shift. On 9/20/22, nursing documentation read, Resident continues to wander. A note dated 9/21/22 revealed the resident ambulated throughout the facility and successfully opened an emergency exit door. During that shift she was anxious and confused, and repeatedly verbalized her intent to leave the facility. The document read, Resident continues to wander. and attempts to redirect her were only occasionally effective. On 9/22/22, resident #25's assigned nurse noted she continuously wandered around the unit and informed staff she wanted to leave the facility to go home.
Review of the Clinical Notes Report revealed a note dated 9/22/22 at 12:25 AM, that described the resident .walking hallways in distress, redirected to room multiple times by staff. A clinical note dated 10/03/22 revealed resident #25 eloped from the facility, and after she was found and returned to the building, the nurse initiated one-to-one staff supervision to ensure her safety.
Review of the Minimum Data Set (MDS) admission assessment with assessment reference date of 9/22/22 revealed resident #25 had a Brief Interview for Mental Status score of 4 out of 10 which indicated severe cognitive impairment. The document inaccurately noted the resident had not wandered since admission, and did not reflect the frequency and impact of her behavior or use of a wander/elopement alarm as verified in nursing notes. The MDS assessment revealed it was very important to resident #25 to have her family involved in discussions regarding her care, and very important for her to go outside for fresh air when the weather was good.
Resident #25's care plan for elopement risk related to exit seeking behavior was initiated on 9/20/22, the day the facility placed an electronic monitoring device on her ankle. The goal was the resident would not have any successful elopement attempts. Interventions dated 9/20/22 were to update elopement manuals with the resident's information, encourage activities of choice, and check the placement and function of her left ankle electronic monitoring device. However, the care plan did not incorporate the resident's preferences as documented in the MDS assessment, including access to safe outdoor spaces or show the result of collaboration with her family regarding known effective approaches to address her wandering. The care plan interventions did not include instructions to report verbalizations of intent to leave the facility and increased wandering and exit-seeking behaviors to nursing management and/or the physician. The initial care plan failed to note the appropriate frequency of monitoring and level of supervision for resident #25 during periods of active wandering and exit seeking. After the resident eloped on 10/03/22, the care plan interventions were updated to include evaluation by a physician or physician extender, one-to-one staffing, Speech Therapist to in-service staff regarding types of activities to engage or direct the resident, and initiate a program for activities and cognition. However, the care plan still did not include specific instructions for direct care staff regarding preferred activities and appropriate interventions necessary to achieved the goals of care for resident #25.
On 11/08/22 at 1:21 PM and 2:17 PM, the MDS Coordinator stated in addition to information obtained from the medical record, residents' care needs were discussed by the interdisciplinary team (IDT) in daily clinical meetings and then appropriate care plans were developed. The MDS Coordinator acknowledged a care plan was important and should be person-centered to reflect the needs of the individual resident. She described resident #25's elopement risk care plan as basic and said, It covered everything we would do. She explained that two to three weeks after admission, she usually conducted care plan meetings with residents and/or their representatives as part of the comprehensive care planning process. The MDS Coordinator stated she had no documentation of a care plan meeting for resident #25. She explained the meeting was scheduled for the time period during which the resident eloped, and instead of a care plan meeting, the Director of Nursing held discussions with the resident's family. The MDS Coordinator stated to her knowledge, the facility did not have policies and procedures for care planning.
The job description for the MDS Coordinator (undated) revealed she was responsible for the completion of MDS assessments and the development of the individualized plan of care. The document indicated her duties and responsibilities included effective collaboration with staff to ensure the optimal level of care for residents.
Review of the facility's policy and procedure for Care Plans, Comprehensive Person-Centered revised in November 2020, revealed the IDT, the resident, and his or her representative would collaborate to develop a comprehensive, person-centered care plan. The policy noted the care plan was the final stage of the IDT process and would include meaningful and targeted care plan approaches. The document indicated the care planning process would include the resident's personal preferences and describe the services that are to be furnished to attain or maintain the resident's highest practicable physical, mental, and psychosocial well-being.
The Facility Assessment Tool dated 11/19/21, revealed the facility was able to care for residents with impaired cognition, behaviors that required interventions, Alzheimer's Disease, and dementia. The document indicated the facility would provide person-centered care by incorporating information on a resident's preferences and routines in the care planning process, ensuring direct care staff had access to the information, and involving family or representatives.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure care plans were reviewed and revised to reflec...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure care plans were reviewed and revised to reflect interventions after a fall for 1 of 8 residents reviewed for accidents out of a total sample of 32 residents, (#408).
Findings:
Resident #408 was admitted to the facility on [DATE] with previous admissions on 8/19/20 with diagnoses of heart failure, pain, dementia, and falls. The resident was discharged on 2/3/22.
The Minimum Data Set (MDS) discharge assessment with assessment reference date of 2/3/22 revealed the resident had short term memory loss, limited assistance with bed mobility, transfers, walking in room, and supervision needed when walking in the coordinator. Section J of the assessment noted the resident had one fall since admission.
Review of the facility's occurrence report log revealed resident #408 had a fall on 1/30/22 at 9:20 PM.
The resident's care plan dated 3/29/21 and revised 1/5/22 showed he was at risk for falls related to fall history, impaired balance with transfers, and gait. The care plan showed the resident had an increased risk of fractures with falls related to vitamin D deficiency and all interventions for falls were dated 3/29/21. There were no updates or revisions to the care plan after the resident fell on 1/30/22.
On 11/09/22 at 2:22 PM, the Director of Nursing (DON) stated a fall meant a change in condition and care plan interventions to be updated. The DON explained it was the responsibility of the MDS coordinator to update care plans.
On 11/9/22 at 2:14 PM, the MDS Coordinator acknowledged there were no interventions post fall 1/30/22 on the resident's care plan, I missed it. She stated care plans were to be updated after the morning meeting when falls were discussed.
Review of the facility Policy Care Plans, Comprehensive Person-Centered 2001 Med-Pass, Inc (Revised December 2016, November 2020) revealed Policy Interpretation and Implementation 13. Assessments of residents are ongoing and care plans are revised as information about the residents and the residents condition change. 14. The Interdisciplinary Team must review and update the care plan:
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure oxygen therapy was administered per physician's...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure oxygen therapy was administered per physician's orders for 1 of 1 resident reviewed for respiratory therapy of a total sample of 32 residents, (#554).
Findings:
1. Resident #554 was admitted to the facility on [DATE] with diagnoses of dependence on supplemental oxygen, epilepsy, and atherosclerotic heart disease.
On 11/7/2022 at 10:52 AM, resident #554 was in her room sitting in a wheelchair (WC) while wearing a nasal cannula (NC). Her oxygen concentrator device was turned off with the flow rate set at 0.
A review of the medical record revealed physician orders dated 3/17/2022 for oxygen at 2 LPM via NC three times daily and orders directed nurses to change the oxygen tubing and humidifier to start on 3/8/2022.
Resident #554's care plan updated 10/12/2022 included monitoring of sudden declines related to cardiac, respiratory, and neurological conditions with oxygen use.
A review of the annual Minimum Data Set (MDS) assessment dated [DATE] revealed the resident was cognitively intact, did not include rejection of care, and noted the resident received supplemental oxygen.
On 11/7/2022 at 12:16 PM, resident #554 was in her room and and had nasal cannula on. The oxygen concentrator was turned off and the flow rate was set at 0.
On 11/7/2022 at 12:20 PM, Registered Nurse (RN) A stated she was assigned to resident #554 on the current shift. RN A checked the electronic medical record (EMR) and noted the resident had current orders to receive oxygen at 2 LPM. RN A checked resident #554 and verified the device setting was at 0 LPM and the concentrator was turned off. RN A acknowledged the resident was not receiving oxygen.
On 11/7/2022 at 12:48 PM, the Director of Nursing (DON) was asked to clarify resident #554's physician order for oxygen in the EHR and stated, it's continuous referring to the order for oxygen. She explained nurses were expected to check residents who received supplemental oxygen for proper placement, saturations if needed, and concentrator functioning during any assessment or interaction. She added, if a resident who required continuous oxygen had a concentrator turned off, that is a problem.
On 11/7/2022 at 12:44 PM Advanced Practice Nurse Practitioner (APRN) B verified resident #554 required continuous supplemental oxygen. She added, nurses should be aware of all oxygen orders and whether continuous or as needed therapy is required, and it should be clearly documented in the medical record.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. A review of resident #11's medical record revealed the resident was admitted to the facility on [DATE] with diagnoses that in...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. A review of resident #11's medical record revealed the resident was admitted to the facility on [DATE] with diagnoses that included prostate cancer.
A review of resident #11's quarterly MDS assessment with ARD 10/2/2022 indicated the resident did not show any wandering behaviors and was not being monitored by using alarms.
A review of resident #11's current physician orders revealed an order for a wander alarm initiated on 7/25/2022 with instructions to check the placement and functioning every shift.
A review of resident #11's comprehensive care plan included a focus for the potential risk of elopement due to exit seeking behavior and attempts to follow visitors out the front door in his wheelchair updated 8/17/22. The interventions included the use of a wander alarm.
On 11/8/22 at 1:05 PM, review of a facility elopement book located at the west unit nurses station revealed resident #11 was included and considered by the facility to be an elopement risk.
On 11/9/22 at 9:20 AM, the MDS Coordinator verified resident #11's quarterly MDS with ARD 10/2/2022 was incorrectly assessed to indicate the resident's status did not include using alarms. She added resident #11's care plan included an intervention for using a wander alarm initiated 7/25/2022.
On 11/08/22 at 2:17 PM, the MDS Coordinator stated the facility did not have a policy and procedure regarding MDS assessment accuracy. She explained all staff who completed MDS assessments followed the MDS Resident Assessment Instrument (RAI) Manual.
2. Review of resident #19's medical record revealed she was readmitted to the facility on [DATE] with diagnoses that included dementia with behavioral disturbance, cognitive communication deficit and anxiety.
Review of the annual MDS assessment with Assessment Reference Date of 10/7/22 revealed resident #19's Brief Interview for Mental Status score of 4 out of 10 which indicated severe cognitive impairment. The MDS showed resident #19 exhibited wandering behavior between 4 to 6 days in the look back period. The assessment included this behavior placed the resident at significant risk of getting to a potentially dangerous place and significantly intruded on the privacy or activities of others. The assessment revealed behaviors were worse compared with prior assessments. Review of Section P of the assessment noted electronic device that monitors resident movements and alerts staff when movement is detected, not used.
Review of the physician's order revealed an order dated 10/4/22 for, Electronic monitoring device to wheelchair to alert staff of residents risk for exit seeking behavior check function qs (every shift).
Review of resident #19's Care Plan Report for potential risk of elopement updated on 10/26/22 revealed interventions that included check placement and function as ordered .
On 11/09/22 at 9:27 AM, the MDS Coordinator stated the most recent MDS assessment completed for resident #19 was a comprehensive annual assessment on 10/7/22. She reviewed section E and confirmed wandering behavior occurred daily, the behavior placed the resident at risk for her safety, intruded in the privacy of others and the behavior was worse than the previous assessment. The MDS Coordinator reviewed Section P and stated it was not assessed for wander/elopement alarm. She indicted the care plan for elopement risk originated on 9/10/19. She stated it was important the MDS reflected accurate information for the development of the care plan.
Based on interview and record review, the facility failed to ensure Minimum Data Set (MDS) assessments accurately reflected wandering behaviors and use of wander/elopement alarms for 3 of 4 residents reviewed for elopement of a total sample of 32 residents (#25, #19 & #11).
Findings:
Cross reference F600, F607, F656, F689, and F835.
1. Review of resident #25's medical record revealed she was admitted to the facility on [DATE]. Her diagnoses included Alzheimer's Disease, dementia, insomnia, and anxiety.
The MDS admission assessment with assessment reference date (ARD) of 9/22/22, revealed in Section E0900 Wandering - Presence & Frequency resident #25 did not exhibit wandering behaviors during the seven-day lookback period. Section P0200 Alarms showed the resident did not use a wander/elopement alarm during the lookback period. Review of Section Z Assessment Administration revealed the Social Services Director (SSD) completed Section E on 9/21/22, and the MDS Coordinator completed Section P on 9/26/22. The document indicated their signatures certified the accuracy of the resident assessment information.
Review of the September 2022 Physician Order Sheet revealed on 9/20/22, resident #3's attending physician ordered an electronic monitoring device to alert staff of residents risk for exit seeking behavior.
Review of Daily Skilled Note forms completed during the MDS admission assessment lookback period, from 9/16/22 to 9/22/22, revealed nursing documentation of resident #25's wandering behaviors and use of an electronic monitoring device. A nursing note for the day shift on 9/17/22 revealed resident #25 had been awake since early that morning, searching for her mother and father. A note for the day shift on 9/19/22 indicated she was confused, ambulated up and down the hallways, and required frequent redirection. As a result, staff placed an electronic monitoring device during that shift. Notes on 9/19/22 for the night shift and 9/20/22 for the day shift indicated the electronic monitoring device remained in place. A skilled note for the evening shift on 9/20/22 read, Resident continues to wander. and she still wore an electronic monitoring device. On 9/20/22 on the night shift and on 9/21/22 on the day shift, skilled nursing notes again documented resident #25's electronic monitoring device. A note for the evening shift on 9/21/22 revealed the resident ambulated throughout the facility and opened an emergency exit door. During that shift she repeatedly verbalized her intent to leave the facility. The document read, Resident continues to wander. and noted her electronic monitoring device was present. Skilled notes on 9/21/22 for the night shift and on 9/22/22 for the day shift again documented the resident's electronic monitoring device. On 9/22/22 during the evening shift, resident #25's assigned nurse noted she continuously wandered around the unit and informed staff she wanted to leave the facility to go home. Review of the Clinical Notes Report revealed a note dated 9/22/22 at 12:25 AM that described resident #25 .walking hallways in distress, redirected to room multiple times by staff.
On 11/08/22 at 1:21 PM, the MDS Coordinator validated resident #25's MDS admission assessment showed she had no wandering behaviors and did not use an electronic monitoring device. She reviewed the resident's medical record and confirmed during the lookback period, there was a physician order for an electronic monitoring device and several nursing notes that described continuous wandering and exit-seeking behaviors. The MDS Coordinator verified she completed Section P of the MDS assessment regarding wander/elopement alarms and acknowledged it was inaccurate.
On 11/08/22 at 2:02 PM, the SSD explained she usually gathered information for MDS assessments by reviewing nursing progress notes and assessments, observing residents, and communicating with nursing staff and the interdisciplinary team. The SSD acknowledged she completed Section E of resident #25's MDS admission assessment and confirmed it did not reflect the resident's significant wandering behavior.
The job description for the MDS Coordinator (undated) revealed her duties and responsibilities included .completion of the Minimum Data Set (MDS) and Plan of Care in an accurate and timely manner.
Review of the Long-Term Care Facility Resident Assessment Instrument 3.0 User's Manual Version 1.17.1 dated October 2019 revealed steps for assessment of Section E0900 Wandering - Presence & Frequency included instructions to review the medical record and interview staff to determine whether wandering occurred during the 7-day look-back period.If wandering occurred, determine the frequency of the wandering during the 7-day look-back period. The RAI Manual indicated the steps for assessment for Section P0200 Alarms included review the resident's medical record (e.g., physician orders, nurses' notes, nursing assistant documentation) to determine if alarms were used during the 7-day look-back period.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #11 was admitted to the facility on [DATE] with diagnoses of prostate cancer, need for assistance with personal care...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #11 was admitted to the facility on [DATE] with diagnoses of prostate cancer, need for assistance with personal care, and palliative care.
Review of resident #11's quarterly MDS with assessment reference date (ARD) 10/2/2022 revealed the resident had moderate cognitive impairment. The resident required extensive assistance with bed mobility, transfers, toilet use, and personal hygiene, was always incontinent of bladder and bowel, and there were skin tears present.
Review of resident #11's comprehensive care plan included focus and interventions for risk of pressure injuries and skin impairments.
Review of resident #11's daily skilled notes indicated on 4/15/2022, open area on side of nose will need assessment by wound care. The nursing daily skilled note dated 4/16/2022 documented, the resident has a red crusted spot on the bridge of his nose. Needs follow up with wound care.
Review of resident #11's medical record revealed the resident was being followed by a wound care physician. The provider's progress notes for 8/23, 8/30, 9/6, 10/4, 10/11, 10/17, 10/27, and 11/3/2022 included orders for Bacitracin, a topical antibiotic to be applied to the nose bridge every two days and as needed.
Review of resident #11's current orders and treatments revealed the orders to treat the skin lesion on the nose were not noted.
On 11/7/2022 at 2:38 PM, resident #11 was observed sitting in a wheelchair in his room. A dark purple/black colored skin lesion was present on the right side of the resident's nose. The resident stated, it may be cancer.
On 11/8/2022 at 9:03 AM, the DON explained wound care orders were expected to be given verbally to the ADON during wound rounds who transcribed the orders into the medical record.
On 11/8/2022 at 1:13 PM, LPN D stated resident #11 had a skin lesion on his nose and explained, they are not planning any kind of in-depth treatment and the area had varied from improving to worsening. LPN D verified there were no orders for treatment in the EMR and added the resident was being seen by the wound specialty physician.
On 11/8/2022 at 1:36 PM, RN F recalled she had resident #11 on her assignment the previous week and there were no treatment orders for the nasal skin lesion.
On 11/8/2022 at 1:44 PM, the DON reviewed resident #11's EMR and acknowledged there were skilled nursing notes dated 4/15-4/16/2022 that showed skin lesion on the resident's nose with recommendations for a wound care referral, and a referral by the primary care physician (PCP) for evaluation and treatment by a dermatologist on 8/12/2022. The DON explained the EMR also revealed recommendations for Bacitracin to the nose bridge to be applied every 2 days and as needed on 8/30/2022 that were not transcribed to the medication administration record (MAR) or treatment administration record (TAR). She recalled a conversation with the resident's family approximately four or five months earlier about the dermatology referral and stated, the family said no because he's hospice. She could not locate any documentation related to refusal of treatment. The DON acknowledged there was no evidence of nursing follow up for wound care and noted there was an order to treat the nasal skin lesion, and resident #11 never received the treatment per physician's orders.
On 11/8/2022 at 2:08 PM, resident #11 was observed sitting in a wheelchair near the west unit nurse's station. The resident stated the lesion was, probably cancer and added he, would like to know more about it. The resident recalled the lesion had been present for approximately one year and explained the nurses, don't do much of anything to treat it.
On 11/9/2022 at 9:15 AM, the Social Services Coordinator stated resident #11 had a power of attorney (POA) and health care surrogate (HCS) as he was deemed incapacitated. She recalled the resident had recommendations to see dermatology and a conversation with the family in the hallway conveyed they didn't want to put him through further treatment due to his terminal condition. She could not provide any documentation related to refusal of treatment.
The policy and procedure (P&P) for Wound Care revised October 2010 revealed The purpose of this procedure is to provide guidelines for the care of wounds to promote healing. Preparation (1.) Verify that there is a physician's order for this procedure.
Based on observation, interview, and record review, the facility failed to provide appropriate care and services for 2 of 3 residents reviewed for non-pressure wounds out of a total sample of 32 residents, (#49, #11).
Findings:
1. Resident #49 was readmitted to the facility on [DATE] with diagnoses of left breast mastectomy open wound and cellulitis to chest wall.
The 5 Day Minimum Data Set (MDS) assessment dated [DATE] documented she had severe cognitive impairment, required extensive assistance with activities of daily living and had a surgical wound which required wound care.
Review of resident #49's medical record revealed physician order for wound care dated 10/17/22 that read, Dressing Change One Time Daily Staring 10/18/22. Notes: Apply Mupirocin to Maxorb rope [calcium alginate] and insert into undermining, secure with optifoam every day and prn [as needed]. The order did not specify what to clean the wound with or it's location.
Resident #49's care plan updated on 10/21/22 indicated she returned from the hospital with cellulitis of chest wall related to an infection and internal surgical wound abscess from left mastectomy in March 2022. The goal was for wound to be free of signs and symptoms of infection with completion of antibiotics as ordered and wound treatments. Interventions included to monitor left chest for drainage, temperature and treatment changed to mastectomy wound site .
On 11/7/22 at 10:50 AM, the resident was observed lying in bed and her son was at the beside. The son said he was concerned that his mother's dressing on her chest kept leaking and he did not think the staff were changing it often enough. He stated she could have an infection. The resident pulled her gown off her left shoulder which showed a dressing on the left chest dated 11/6/22 which was dry and intact.
On 11/8/22 at 1:07 PM, resident #49 was eating lunch and her assigned Certified Nursing Assistant (CNA) C was in the room. The CNA was adjusted the resident's gown to the left shoulder that showed a dressing on her left chest dated 11/6/22 saturated with tan colored drainage leaking through the dressing. The CNA sated she would let the nurse know that the dressing was coming off.
On 11/8/22 at 1:10 PM, the assigned Registered Nurse (RN) F stated she was too busy at this time do take care of the resident's dressing and requested RN E to assist.
On 11/8/22 at 2 PM, RN E gathered supplies to do the resident's wound care. RN E validated the dressing was dated 11/6/22 and was saturated with wound drainage and coming off the left chest area. She stated the wound care was to be done every other day which contradicted the physician order in the medical record that noted daily wound care. When the nurse removed the soiled dressing, the wound was noted to be crescent shaped and approximately 10-12 centimeters (cm.) wide by 2-3 cm. long and ½ to 1 cm. deep with beefy red appearance. RN E proceeded to clean the wound with normal saline, packed the wound with the Maxorb rope with Mupirocin ointment, applied skin prep to peri wound and then covered the area with 2 foam border dressings that were 4 x 4 inches each.
After reviewing the medical record, RN E acknowledged the wound care orders were not clear as they did not include what solution to clean the wound with and the instructions in the Advance Practice Registered Nurses' (APRN) notes indicated wound care every other day, the orders in the electronic medical record were for daily wound care. The APRN's notes also indicated that skin prep should be applied peri wound and the orders in the electronic medical record (EMR) did not include this. On 11/8/22 at 3:30 PM, RN E acknowledged the resident's dressing was not changed on 11/7/22 as ordered.
On 11/9/22 at 4:46 AM, during a telephone interview, Licensed Practical Nurse (LPN) I said she worked the night shift (11 PM to 7 AM) on 11/6, 11/7, and 11/8/22. She stated she was assigned to resident #49 this week and noted the resident was being treated for a wound infection and had just completed her antibiotic therapy. She indicated the resident's wound care was done on the day shift. She explained she did not get report from off going nurse to do the resident's wound care and acknowledged she must have inadvertently signed off on the wound care on 11/7/22. She acknowledged she had not changed her dressing. She stated, I have no idea what happened or how my initials got there, I must have accidentally signed off on doing the wound care on 11/7/22. She could not recall checking the resident's dressing although there were physician orders to check the site every shift.
On 11/9/22 at 10:29, LPN H verified he worked 11/7/22 and 11/8/22 on the 3-11 shift and was assigned to the resident #49. He stated, yes, the off going nurse on 11/7/22 reported she did not have time to do the dressing change on the resident's left chest. He stated he did not get time to do the wound care on his shift and left a written report for the next shift nurse but forgot to inform her verbally.
On 11/9/22 at 1:15 PM, the Director of Nursing (DON) verified that she was aware that resident #49 did not get her dressing change daily as ordered by the physician and the order for wound care dated 10/17/22 was not clear and as it did not include what to clean the wound with nor the application of skin prep to peri wound. The DON explained the process was for the Assistant Director of Nurse (ADON)/Wound Care Nurse to round with the wound APRN and then enter the verbal orders onto the EMR. She added that the ADON was not available to be interviewed at this time. The DON acknowledged if nurses were monitoring the wound drainage per shift as ordered, the dressing would not have looked the way it did on 11/8/22 by the surveyor and RN E.
On 11/9/22 at 2:55 PM, during a telephone interview, the wound care APRN Q said that wound care was to be changed every 2 days in September but she had changed the order during her last visit on 11/3/22. She explained she did not have access to EMR and relied on the nursing staff to enter the wound care orders.
Review of the facility's policy for wound Care revised October 2010, read, Purpose: The purpose of this procedure is to provide guidelines for the care of wounds to promote healing .Preparation: Verify that there is a physician's order for this procedure. Review the resident's care plan to assess for any special needs of the resident .Report other information in accordance with facility policy and professional standards of practice.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to ensure kitchen staff were competent to safely and effectively perform their duties to prevent or minimize the potential for fo...
Read full inspector narrative →
Based on observation, interview and record review, the facility failed to ensure kitchen staff were competent to safely and effectively perform their duties to prevent or minimize the potential for food borne illnesses.
Findings:
On 11/7/22 at 11:11 AM, during the initial kitchen inspection with the Kitchen Supervisor, the walk-in refrigerator was noted with soiled floors, shelves and racks. Dark black/brown mold like stains were observed on the shelves, vertical racks and the floor. The vertical pan rack had build up of white and black substance on each of the tiers. The shelf next to the exit door had a container of blueberry muffin batter mix that had spilled batter on the sides of the container. The Kitchen Supervisor stated the staff should have wiped down the batter mix tub before putting the lid back on. He indicated there was a kitchen cleaning schedule but it had not been followed due to staffing issues.
The dry storage room had a large unopened bag of rice crispy cereal dated February 8, 2019. The Kitchen Supervisor stated he was going to make rice crispy treats from this bag of cereal. There was a large bag of dried cranberries that had been opened but not dated or labeled. The Kitchen Supervisor indicated the staff should have labeled the bag with the date it was opened.
At the salad/sandwich preparation area, the Kitchen Supervisor picked through the lettuce with gloved hands, and removed the wilted lettuce leaves. Using the same gloves, the Kitchen Supervisor, touched the trash can and removed the lid and discarded the browned lettuce leaves. He did not sanitize his hands or change his gloves, but continued to pick through the lettuce and touched the trash can lid two more times. He then proceeded to make a sandwich without discarding the gloves or washing his hands. He placed two pieces of bread on a plate, and placed deli meat on the bread. At that point, the Kitchen Supervisor was instructed to stop, and he was informed of the potential cross contamination as he had not performed hand sanitization or changed gloves.
At the dish washing area, the Dishwashing staff stated the dishwashing machine was high temperature, meaning that it used hot water to sanitize the dishes. The manufacturer's data plate that was affixed to the dishwashing machine noted a wash temperature of 160 degrees Fahrenheit and a final rinse temperature of 180 degrees Fahrenheit. The Dishwashing staff placed racks of dishes into the machine and the temperature gauge revealed the wash temperature was 120 degrees Fahrenheit and the final rinse was also 120 degrees Fahrenheit. The Dishwashing staff stated when he washed the breakfast dishes this morning he did not check either the wash nor the final rinse temperatures. When asked if there was a temperature log for the dishwashing machine, he said no. The Dishwashing staff inspected the hot water booster and said there was an error message. The Kitchen Supervisor was informed the dishwashing machine's wash and rinse temperatures were both 120 degrees Fahrenheit. He proceeded to put away the dishes that had come out of the machine.
A flat top griddle was noted in the cooking area underneath the exhaust hood. A bottle of cooking oil that was three-quarters full was on the bottom shelf of the griddle. The bottom shelf was covered in oil and black debris. The Kitchen Supervisor partially pulled out the grease trap from the griddle, which was full of oil and dark clumps. When he removed the grease trap entirely, dark oily clumps fell on the bottom shelf and the floor. The Kitchen Supervisor then brought the grease trap to a trash can that had paper and other combustible materials, and emptied the used cooking oil and dark clumps into the trash can.
On 11/7/22 at 11:45 AM, the Dietetic Technician Registered (DTR) was informed of the used cooking oil placed into the regular trash can. The Kitchen Supervisor at this time suggested that he could poke holes in the trash bag and let the used cooking oil drain out. A large metal receptacle, for used cooking oil, was observed outside in the dumpster area. The DTR could not explain why the kitchen supervisor did not dump the used cooking oil into this receptacle instead of a regular trash can. The DTR added she would find out about the dishwashing machine and ensure all the dishes were rewashed and rinsed at the appropriate temperatures.
On 11/8/22 at 12:43 PM, the Dishwashing staff was observed washing dishes and the temperature gauge for the final rinse read, 150 degrees Fahrenheit. The DTR was present and the Dishwashing staff explained they had been using surface temperature strips to ensure the final hot water rinse temperature was at 180 degrees Fahrenheit. The Registered Dietician (RD) presented documentation from the Food and Drug Administrative Code that noted surface temperature of 160 degrees Fahrenheit reflected 180 degrees Fahrenheit at the manifold. The RD explained they were using a 165 degree Fahrenheit surface test strip. She said she was made aware of the dishwashing machine temperature concerns and instructed staff to use surface test strips. She noted this would determine if the temperature gauge needed to be replaced. The RD stated she had been at this facility for about 2 weeks, and had been focusing on clinical issues. The DTR was asked about training and education, with regards to sanitation, for the Kitchen Supervisor and the dietary staff. The DTR stated she would try to find the kitchen staff's training records but did not provide them by the end of the survey.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, record review, and interview, the facility failed to maintain the overall cleanliness of the kitchen and ensure food was stored and distributed in a sanitary manner.
Findings:
On...
Read full inspector narrative →
Based on observation, record review, and interview, the facility failed to maintain the overall cleanliness of the kitchen and ensure food was stored and distributed in a sanitary manner.
Findings:
On 11/7/22 at 11:11 AM, the initial kitchen inspection was conducted with the Kitchen Supervisor. He stated there was a kitchen cleaning schedule but it had not been followed due to lack of staff. The shelves in the walk-in refrigerator to the right of the entrance were noted with black substance on the sides. The shelves, vertical pan racks and flooring in the refrigerator were noted with dark black/brown mold like stains.
The preparation table near the walk in refrigerator was noted with a build up of dirt/dust/food debris. The entire wall behind the the table had black/brown stains on the tile and grout. The base plate of the commercial can opener on the preparation table was covered with black and brown spots and the insert had black mold like substance on it that appeared either wet or greasy. The blade and gears of the can opener were observed with dark colored food debris and dirt. There were several 4 inch deep steam table pans stored on the bottom shelf with white and black build-up on the edges.
The open can rack in the dry storage room had heavily stained black/brown mold like substance on each tier. The kitchen staff continued to put cans of food on the rack. Spilled lentils were observed on top of an open case of apple juice, and on the tile floor. There was dark debris and clumps of dust on the shelves, floors and baseboards. The bottom shelves had white strands that appeared to be cobwebs. There was a cardboard case of white taco shells that had a product code, 10205 and a date of 12/17/21 printed on the outside of the case Review of the manufacture's product information revealed the taco shells had a shelf life of 120 days (https://missionfoodscontent.imgix/nutrition/tds_sheets/10105).
The dispensing nozzle on the juice dispenser was noted to have black mold like substance on the underside of the nozzle that had contact with the juice/beverage. The Kitchen Supervisor did not expand on the minimum cleaning the staff had done.
On 11/7/22 at approximately 11:45 AM, the Dietetic Technician, Registered (DTR) was informed of the issues identified in the kitchen
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, and interview, the facility failed to ensure the dumpster and the immediate area was maintained in a safe, functional and sanitary manner.
Findings.
During the initial kitchen in...
Read full inspector narrative →
Based on observation, and interview, the facility failed to ensure the dumpster and the immediate area was maintained in a safe, functional and sanitary manner.
Findings.
During the initial kitchen inspection on 11/7/22 at approximately 11:11 AM, the dumpster area was observed. There was a large dumpster that had two lids that slanted from back to front. The lids did not fit properly and there was a sizable gap between the lids that would not prevent vermin or pests from entering the dumpster. There was a round metal rod that ran through the lids that was bent and prevented the lids from closing properly. The facility's Dietetic Technician Registered (DTR) attempted to slide the lids closer together but was not successful.
A large rectangular shaped used cooking oil receptacle was noted behind the dumpster. The top of this receptacle was noted with dark oily clumps of debris. The DTR stated the receptacle needed to be cleaned or replaced. A stone paneled open trash can that contained cups and other combustible material was situated near the used cooking oil receptacle. The trash can had a square, depressed top that staff had used to place cigarette butts. The DTR stated staff should not be smoking near the dumpster area especially not near the used cooking oil receptacle.