CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide care and treatment services in accordance with...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide care and treatment services in accordance with professional standards of practice as evidenced by not identifying on admission that resident had transparent dressing and providing treatment for a change in condition for two (Resident #2 and Resident # 21) out of three residents sampled for skin.
Findings included:
1. On 12/12/2022 at 1:29 PM, Resident #2's left forearm was observed with an undated adhesive bandage dressing
that appeared old and loosely attached. The dressing partially covered a quarter size elevated mass. The admission Business Office Manager (BOM) asked Resident #2 about the bandage and the Resident responded, I scratched it.
Medical record review of the admission Record form revealed Resident #2 has resided at the facility for close to a year and is geriatric in age. The diagnosis listed rash and other nonspecific skin eruption dated 7/16/202. Unspecified skin changes 6/26/2021 and superficial mycosis (fungus) 1/12/2021.
Review of Skin assessment dated on 12/06/2022 reflected no impairment, skin intact. Nursing progress notes were omitted of documentation related to the left forearm.
Review of a dermatology consult dated 09/05/2022 did not reflect Resident #2 left forearm.
On 12/13/2022 at 12:00 PM, Resident #2 was observed up in his Geri chair and smiled when approached. His left forearm contained 2 inches by 2-inches bordered dressing dated 12/13/2022.
Review of nursing notes dated 12/13/2022 time stamped 09:15 Skin/Wound Note Text: Patient has been and evaluated this morning by the wound care nurse as ordered by doctor [name of doctor] due to left forearm skin lesion. Patient was noted with a pink hyper granular growth to the left posterior forearm, with slightly elevated aspect, rolled and well-defined edges, no signs of infection, patient refers itching sometimes, no drainage or bleeding noted. Doctor [name of doctor] was notified about patient's skin condition, order given for Dermatology consult.
Further review of the notes dated 12/13/2022 at 9:36 Skin/Wound Note, Note Text: New order received from doctor [name of doctor] to apply dry dressing to the left forearm skin lesion until the patient is seen by Dermatology, order carried out.
On 12/14/2022 at 4:20 PM, an interview was conducted with the Wound Nurse. She reported there was a doctor order for her to look at Resident #2's arm.
On 12/15/2022 at 10:00 AM, an interview was conducted with Minimum Data Sheet staff member who at that time, confirmed there was no Physician order in place for the Wound Nurse to assess Resident #2's arm.
On 12/15/2022 at 10:30 AM, during an interview the BOM confirmed she had notified the nurse on the unit about Resident #2's bandage. She stated, On Monday (12/12/2022) right after you (surveyor) asked him about the band aid ®.
2. On 12/12/22 at 12:35 PM, Resident #21 was alert and receptive to an interview. Both of his forearms presented with large areas of petechia (pinpoint, round spots) and small scattered scabs. The right forearm contained a 4 inch by 4-inch transparent dressing that started just above his ID bracelet. Under the dressing the skin reflected dark red ruby-colored patches. No lumps, bumps, lesions, and nor open areas were present. No date was on the dressing. Resident #21 stated the dressing to his right arm was from the hospital. He stated, they put it on.
Medical record review revealed admission Record form that Resident #21 was admitted to the facility on [DATE] for short term rehabilitation. The form contained diagnosis information that included other specific disorders of the skin and subcutaneous tissue, chronic kidney disease (CKD), rash and other nonspecific skin eruptions.
Review of progress notes dated 12/12/2022 2:15 PM (14:15) Skin/Wound Note Text: Patient is [age] male, alert and oriented times 3 (AOx3), readmitted to the facility from [local hospital. readmission skin assessment done by the wound care nurse. Patient has significant ecchymosis discolorations with dry scabs and venipuncture sites to bilateral upper extremities (BUE's). Revealed omission of the transparent dressing on Resident #21's right arm.
Further review of the note read the Physician [Physician name] was notified of current patient's skin condition, order given for treatment, consult with [physician name], air mattress, offloaded heels while in bed, incontinence care as needed, barrier cream to bilateral lower extremities (BLE's), turn and reposition every 2 hours and as needed (PRN). Patient is at risk for skin breakdown related to advanced age, impaired mobility, unsteady gait, difficulty walking, muscle weakness, declining in functions, diabetes mellitus (DM), heart failure (HF), hypertension (HTN), CKD, aortic stenosis. Responsible party, [ name of responsible party] aware of patient skin condition and interventions in place, no concerns.
On 12/13/2022 at 10:20 AM Resident #21 received a midline catheter to his left arm, just below the antecubital area. The transparent dressing remained in place. The center of the dressing now revealed a small area reflecting the size of a pencil eraser that was green to yellow in color.
On 12/14/2022 at 9:50 AM, Resident #21 was lying in bed and recalled the surveyor's name while he smiled when approached. The transparent dressing remained in place to his right arm. The center of the dressing contained a yellow-colored thick drainage, that now reflected the size of a five-cent piece (nickel) (photographic evidence obtained).
At 10:00 a.m. Staff E, a Registered Nurse was asked about Resident # 21 and the left arm transparent dressing, she looked at it and stated, It's from the hospital, I will have to check with wound care.
At 11:30 AM an interview was conducted with the Wound Care Registered Nurse that confirmed she had performed an admission skin assessment for Resident #21. The Wound Nurse confirmed she had documented in Resident #21 medical record the bilateral upper extremities with significant ecchymosis, discolorations, with dry scabs, and venipuncture sites. The Wound Nurse confirmed she knew about the transparent dressing being in place at the time of her assessment. She stated, It was from a line removal. It was bumpy, and elevated. If I were to remove it there is a risk for skin break down. When asked about the monitoring of the dressing she stated, there is an order in place to monitor for bruising or bleeding to the upper arms. The Wound Nurse confirmed the admission skin assessment, nor the medical records reflected that a transparent dressing was is in place. She went on to say that she had seen his arm this morning, I didn't see yellow tissue. The Wound Nurse along with the Director of Nursing (DON) observed Resident #21's arm. The arm no longer contained the transparent dressing. She stated, it's not open it was closed all the time. The DON confirmed that the medical record should contain an accurate assessment and description of the skin to include dressings that are in place for 7 days.
Review of Physician orders dated 12/14/2022 Monitor for bruising and bleeding/thromboembolism every shift.
Review of the facility's policy titled Assessment of Skin Condition and Integrity that did not contain a date, Policy, and Procedures: The purpose of this policy is to provide information regarding the assessment of skin condition and integrity. Skin Assessment 1. Conduct a comprehensive head to toe skin assessment upon admission, at least weekly, and as needed. A. During the skin assessment, inspect for; i. Presence of skin impairment(s); ii. Type of skin impairment (s; and iii. Location of skin impairment(s); 2. Observed the skin daily when performing or assisting with personal care or ADLs. Documentation: The following information should be recorded in the resident's medical record: 1. The findings of the skin assessment. 2. The date and time of type of skin care provided, if applicable. 3. The condition of resident's skin. 4. Any change(s) in the skin condition, if applicable. Reporting: 2. Notify the physician of new skin alteration(s) noted. 3. Notify family, guardian or residents responsible party of new skin alteration(s) noted. 4. Report other information in accordance with facility policy and professional standards of practice.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to coordinate care related to dialysis for two residents ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to coordinate care related to dialysis for two residents (Resident #28 and Resident #100) out of 2 residents reviewed for dialysis related to medication administration, weights, and diet orders.
Findings included:
1) Review of Resident #28's admission record revealed he was admitted to the facility on [DATE] from an acute care hospital with diagnoses that included but not limited to encounter for orthopedic aftercare following surgical amputation, acquired absence of right leg below the knee, acquired absence of left leg below the knee, type 2 diabetes mellitus with diabetic chronic kidney disease, end stage renal disease, and dependence on renal dialysis.
Review of Resident #28's physician order summary report revealed an order to start on 9/19/2022 with no end date for hemodialysis (inhouse) TX Freq [treatment frequency]: T, TH, S [Tuesday, Thursday, Saturday] .
Review of Resident #28's physician orders revealed an order for Mircera Solution prefilled syringe 100 mcg/0.3 ml (100 micrograms per 0.3 milliliters). Inject one dose subcutaneously one time a day every 14 days related to end stage renal disease with a start date of 9/20/22. Further review revealed another physician order for Mircera solution prefilled syringe 100 mcg/0.3 ml. Use 100 mcg intravenously one time a day every 2 weeks on Thu (Thursday) for anemia dialysis to administer.
Review of Resident #28's Interim Medication Regimen Review dated 12/13/2022 revealed Medication: Mircera
Recommendation: There are 2 active orders in the med [medical] record.
During an interview with the Director of Nursing (DON) and the Nursing Home Administrator (NHA) conducted on 12/14/22 at 3:47 PM, it was brought to the DON and NHA attention that there are two Mircera orders, one to be administered subcutaneous and one to be administered intravenously. The intravenous order indicated to be administered by dialysis. The DON did not know why there were 2 orders for Mircera . in her opinion she thinks the two orders were a transcription error .The DON was not able to answer if dialysis provides all medications. The DON was not able to answer if her staff were expected to administer the physician ordered Mircera to be administered subcutaneously given it did not indicate that dialysis was to administer it.
A phone interview was conducted with Staff G, Nurse Manager for dialysis center on 12/15/22 at 9:14 AM. Staff G confirmed coordination of care should occur between the dialysis center and the facility. Staff G stated: We have Dietitians and Social Workers; they go and see the patients every month. We do monthly labs, the Dietitian at the dialysis center communicates the labs with the facility's Dietitian and that is documented in our EMAR [Electronic Medical Record]. We do not share our documentation with the facility. We don't share our notes with them. They have their notes, and we have ours. It is expected that our nurses do a verbal pre and post handoff report to the facility's floor nurse .we administer Mircera because that is part of the bundle, The bundle includes Erythropoietin stimulating's hormone (Mircera) and Epogen, we also get paid by Medicare as a bundle on dialysis labs, treatment, and supplies. Everything is paid together and in that bundle fee medications are included so we have to provide medications for the patients. The facility should keep the Mircera order on their MAR to give every 2 weeks. On the hand off report medications that were administered should be reported to the floor nurse. We do not have access to the facility's medical record, but we are trying to get access. In dialysis, typically Mircera is given IV [intravenous] during treatment but it can also be given Sub Q [subcutaneous]. The facility is responsible for weighing the patient before dialysis and after but sometimes the patient after dialysis is hard to weigh. She confirmed they would just guess the weight if they were hard to weighed afterwards based on the amount of fluid they took off during dialysis.
A review was conducted of the Provider's Monthly Dietitian Note dated 11/23/22 for Resident #28. The note revealed the resident's lab values and noted that the resident's albumin was not within target as 3.6, as the target was a value higher than 3.8. The Interventions were noted to be education to the resident on how to increase protein and/or calorie intake. Also, a protein supplement was checked as an intervention. Comments were documented at the end of the note which indicated the dietitian met with the patient to review his lab report. A recommendation was made by the dietitian to start the patient on a dialysis liquid supplement and add double protein portions to each meal.
A review of the facility's quarterly nutritional assessment dated [DATE] revealed the resident's diet order was renal with dialysis, regular texture, thin consistency diet with no supplements.
The resident's diagnoses included Type 2 Diabetes, End Stage Renal Disease, and a below the knee amputation of the right leg. The resident's weight was 176 lbs. (80 kg) with a comparison of weights from November and September. The note included that the comparison was based on post dialysis weights, but there was no reference to the resident's estimated dry weight determined by the dialysis provider.
The resident's weight had remained consistent from September until current, based on the post weights.
A review of the diet orders for Resident #28 revealed he had been ordered and was receiving a Renal with Dialysis Diet, Regular texture, thin consistency. The diet order did not reflect the recommendation made by the Dialysis Dietitian to add extra protein portions to the meals or the liquid supplement.
A prior note by the facility dietitian, dated 12/05/2022 reviewed the resident's weight gain to 181 lbs., post dialysis. The note included the current diet as CCHO (consistent carbohydrate) renal with dialysis diet, with no supplement.
There was no obvious coordination of care between the facility and the provider dietitian to reflect the need for the consistent carbohydrate diet, the extra protein at meals and the additional protein and calories provided by the liquid supplement as recommended by the provider dietitian.
A review of Flow Sheets provided by the dialysis provider revealed pre and post weights did not match the facility's weights. In interviews with the facility DON and the provider's Nurse Manager, the protocol was for the provider to use facility obtained weights pre and post dialysis.
On 12/01/2022 the facility pre dialysis weight was documented as 182.4 (82.9 kg) and the post weight was 180.2 (81.9 kg). The provider Flow Sheet used the pre dialysis weight of 82 kg and the post dialysis weight of 80 kg.
On 12/03/2022 the facility obtained pre dialysis weight was 183 lbs. (83.18 kg) and the post dialysis weight was 181.2 lbs. ( 82.36 kg). The provider Flow Sheet used the pre dialysis weight of 82 kg and the post dialysis weight of 80 kg.
On 12/06/2022 the facility obtained pre dialysis weight was 183.4 lbs. (83.36 kg) and the post dialysis weight was 181 lbs. (82.27 kg). The provider Flow Sheet used the pre dialysis weight of 81.5 kg and the post dialysis weight of 80 kg.
Care plans were reviewed and noted for the care plans related to the resident's dialysis treatment did not include coordinating care between the facility and the provider.
2 ) A review was conducted of Resident #100's progress notes to identify documentation related to the resident's dialysis status and coordination of care between the facility and provider. Resident #100 was admitted to the facility on [DATE] with multiple diagnoses including End Stage Renal Disease (ESRD). An admission note dated 12/07/2022, written at 00:40, included the resident's cognitive status as alert and oriented times 3, and ESRD as one of his diagnoses. The note read: Resident has a dialysis port to the upper left portion of chest, scheduled days are MWF (Monday, Wednesday, Friday) for dialysis. Port is patent and thrill and bruit present.
A review of the progress notes written by the nurses did not include any references to the resident while he was receiving dialysis on 12/08/2022, 12/10/2022, and 12/13/2022.
An admission Nutrition assessment dated [DATE], written at 15:00 reviewed the resident's diagnosis, medications, labs from the hospital dated 11/30/2022, and skin concern (unstageable pressure injury to left heel). The Assessment documented the resident's diet at 2-gram sodium, regular texture, thin consistency fluids. There was no supplement ordered. Intake at meals was 50-75%. The resident was 66 tall and weighed 165 lbs. (pounds)/ 75 kg (kilograms) on 12/06/2022. The dietitian summarized her assessment to include concerns of the unstageable pressure injury to the left heel for which she recommended a multivitamin, zinc sulfate, and a high protein supplement to promote wound healing. The resident was taking a diuretic and on ESRD, so weight fluctuations were expected. The Dietitian recommended a renal with dialysis diet with a liquid high calorie, high protein supplement to better meet the resident's needs.
A nephrology consult was obtained on 12/09/2022 with the note written at 14:51. The Nurse Practitioner documented the resident's use of a tunneled dialysis catheter. The plan included to continue with hemodialysis treatment, two hours three times a week.
Care plans were developed from the resident's admission date with focus areas of renal failure, hemodialysis received in house, the resident's nutritional status related to multiple diagnoses including ESRD and hemodialysis, and the resident's risk for skin breakdown and the presence of a catheter for hemodialysis. None of these care plans identified the need to coordinate care with the outside provider.
A review of Resident #100's dialysis weight log documented by the facility listed the resident's pre-dialysis weight on 12/08/2022 as 152.4 lbs. (pounds)/ 69.27 kilograms (kg) and the post-dialysis weight as 150.2 lbs. (68.27 kg). Weights used on the Hemodialysis Flowsheet were 76 kg pre dialysis and 75 kg post dialysis. Duration (length of dialysis treatment) was documented at 180 minutes or three hours.
The resident was dialyzed on 12/10/2022 for 180 minutes. The facility's dialysis weight log listed the resident's pre-dialysis weight on 12/10/2022 as 153 lbs. or 69.545 kg and the post dialysis weight on 12/10/2022 as 150.8 lbs. or 68.545 kgs.
Pre dialysis weight as listed on the Flow Sheet on 12/10/2022 was documented as 76 kg and post dialysis weight was documented as 75 kg. A note at the end of the treatment session documented that the blood flow rate had been decreased by the Nephrologist from 400 to 350.
On 12/13/2022 the resident was dialyzed for 180 minutes with the BFR (blood flow rate) as 350 according to the new order from 12/10/2022. The pre-dialysis weight was documented as 69.30 kgs which matched the facility's pre-weight of 152.6 lbs. or 69.3 kgs. The post dialysis weight was documented as 69.3 kg which was not the same weight as the facility had documented post dialysis. The facility had documented 150.4 lbs. or 68.36 kgs.
The provider's documentation during dialysis compared to the facility's documentation of weights differed on two of the three days that the resident received dialysis. A Nephrologist's consult dated 12/09/2022 ordered the duration of the dialysis treatment sessions as 2 hours or 120 minutes. The three dialysis sessions that the resident received had a duration of 180 minutes. During the Quality Assurance (QA) interview held on 12/15/2022 at approximately 11:00 AM., there was no reference to residents receiving dialysis by an outside contractor.
A review was conducted of the facility's policy related to the Care of a Resident with End-Stage Renal Disease. The Policy statement read: Residents with end-stage renal disease (ESRD) will be cared for according to currently recognized standards of care. Under Policy Interpretation and Implementation, point #3 read: Agreements between this facility and the contracted ESRD facility include all aspects of how the resident's care will be managed, including:
a. how the care plan will be developed and implemented.
b. how information will be exchanged between facilities.
A review of the agreement between the facility and the provider of dialysis at the facility. The agreement listed the provider's responsibilities which included coordination between the ESRD IDT (interdisciplinary team) and the facility's IDT; dialysis treatments provided for facility residents based on the written orders by the Nephrologist; consultation provided by the Social Worker and Dietitian regarding the dialysis resident; and incorporation of services provided to the facility's residents into the facility's Quality Assessment and Performance Improvement Program. Shared responsibilities between the provider and the facility included: written communication to include treatment orders, medication orders, patient assessments, and any change in the resident's condition. In addition, shared responsibilities included a collaborative review and revision of care plans.
An interview was conducted on 12/14/2022 beginning at 9:14 AM with the Director of Nurses (DON) about the coordination of care between the facility and the dialysis provider. The DON reported that the resident's nurse would check vitals before treatment to ensure the resident was okay for dialysis and after treatment to assess the resident's condition. She confirmed the nurses work 12-hour shifts, but there would be additional notes related to the additional vitals and assessments conducted pre and post dialysis. The DON reported that she would obtain documentation from the dialysis provider for the residents' dialysis treatments as she confirmed the facility did not receive the documentation otherwise. The DON reported that the facility weighed the resident before and after treatment and the dialysis nurse would use those weights for the treatment. The DON added that it was a verbal handoff of the resident's status between the facility nurse and the dialysis nurse that occurred prior to and after dialysis.
An interview was conducted by phone with the Nurse Manager of the contracted dialysis service provider (provider) on 12/15/2022 beginning at 9:26 AM. When asked about how patient care was coordinated between the facility (the nursing home) and the dialysis center, she revealed that the dialysis provider's Dietitian and Social Worker monitor the patients monthly with a documented note and they attend care plan meetings with the dialysis center interdisciplinary team monthly. She confirmed that the facility does not attend the dialysis provider's care plan meetings, and notes and care plans from the meetings are not shared with the facility. She reported that the facility nurse and the dialysis provider's nurse conduct a verbal handoff before and after the resident's dialysis treatment.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review the facility failed to prevent unnecessary medication administration for one resident ( Re...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review the facility failed to prevent unnecessary medication administration for one resident ( Resident #28) out of 4 residents reviewed for unnecessary medications. Related to the administration of a blood pressure medication (Clonidine) out of physician ordered parameters.
Findings included:
Review of Resident #28's admission record revealed he was admitted to the facility on [DATE] from an acute care hospital with diagnoses that included but not limited to encounter for orthopedic aftercare following surgical amputation, acquired absence of right leg below the knee, acquired absence of left leg below the knee, type 2 diabetes mellitus with diabetic chronic kidney disease, end stage renal disease, dependence on renal dialysis, and hypertension.
Review of Resident #28's physician orders revealed an order for Clonidine HCL tablet 0.2 mg (milligrams) give 1 tablet by mouth every 6 hours for HTN SBP (hypertension systolic blood pressure) greater than 160 mm HG (millimeters of mercury) with a start date of 9/15/2022 and discontinued on 12/14/2022.
Review of Resident #28's medication administration record (MAR) for December 2022, revealed 0.2 mgs of Clonidine was administered out of the physician ordered parameters 21 times out of 54 opportunities.
Further review of Resident #28's MAR for the month of November revealed 0.2 mgs of Clonidine was administered out of the physician ordered parameters 55 times out of 120 opportunities.
An interview and record review with the facility's Assistant Director of Nursing (ADON) was conducted on 12/14/22 at 1:00 PM; The ADON reviewed the Clonidine order and stated the resident should get Clonidine when his systolic blood pressure is above 160. The DON reviewed the December MAR and confirmed Resident #28 received Clonidine when his systolic blood pressure was below 160.
An interview was conducted with the Director of Nursing (DON) on 12/14/22 at 1:38 PM, the DON revealed that after she was asked to print out the pharmacy recommendations she recognized the Clonidine was given out of parameters and the facility started education with all the nurses. The physician was called, and he came in early and evaluated the resident to ensure there was no adverse reactions. The DON stated: I take this very seriously and there will be disciplinary action for the nurses who administered the medication out of parameters.
Review of the physician note dated 12/14/22 at 1:31 PM revealed: Patient was reevaluated today to clarify Clonidine orders. Pt (patient) is hemodynamically stable, Pt is oriented about his diagnosis, prognosis, treatment, and medication s/e [side effect]. All labs test results reviewed. Pt . discussed with staff to D/C [discharge] planning. I ordered to change Clonidine order to (0.1 mg) PO (by mouth) every 6 hours PRN [as needed] if BP [blood pressure] equal or more than 160/90. The RN [Registered Nurse] was advised call me if any abnormality occurs.
Review of Resident #28's care plan initiated on 9/15/2022 revealed:
Focus: I have altered cardiovascular status r/t [related to] hypertension, PVD [peripheral vascular disease], hyperlipidemia.
Goal: I will be free from s/sx [signs/symptoms] of complications of cardiac problems through the review date. I will exhibit reduction of my cardiac symptoms through the review date.
Interventions include but are not limited to Administer medications as ordered. Monitor effectiveness and for side effects .
The facility's unnecessary medications policy provided revealed Psychotropic Medication Use undated, revealed Policy statement Residents will not receive medications that are not clinically indicated to treat a specific condition .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
Based on observation, interview, and medical record review the facility failed to ensure that outside services were collaborated for one (Resident #2) out of three residents sampled with Hospice servi...
Read full inspector narrative →
Based on observation, interview, and medical record review the facility failed to ensure that outside services were collaborated for one (Resident #2) out of three residents sampled with Hospice services.
Findings included:
1. On 12/12/2022 at 1:29 PM. Resident #2 indicated that hospice services are following him. He did not recall how often they see him on a weekly basis. He appeared comfortable and in no distress, an adhesive bandage was present to his left forearm that was not dated nor firmly attached to his skin. The area that was not attached revealed a quarter size elevated mass. Resident #2 indicated it was covered because, I scratched it.
Review of nursing notes dated 12/13/2022 09:15 Skin/Wound Note Text: Doctor [name of doctor] was notified about patient's skin condition, order given for Dermatology consult. Notes dated 12/13/2022 at 9:36 Skin/Wound Note, Note Text: New orders received for a treatment until the patient is seen by Dermatology.
Medical record review of the admission Record form revealed Resident #2 has resided at the facility for close to a year and is geriatric in age. The diagnosis listed metabolic encephalopathy, respiratory failure, encounter for palliative care dated 7/18/2022.
Review of Hospice Initial Certification, date of admission to Hospice 07/18/2022 Primary Hospice Diagnosis; Alzheimer's disease unspecified.
Review of Resident #2 care plan Focus: I have terminal prognosis r/t (related to) end stage pulmonary disease, patient it under [name of service] hospice care DX (diagnosis) end stage Chronic obstructive pulmonary disease (COPD), end stage Alzheimer's dementia 07/19/2022 start continuous care. Interventions: Work cooperatively with hospice team to ensure the residents spiritual, emotional, intellectual, physical, and social needs are met.
Review of IDT Care Plan Meeting Review dated 10/25/2022 at 11:00 Meeting Attendance did not reflect any Hospice members were in attendance.
Review of the Hospice Health Care Binder did not reflect a care plan.
On 12/15/2022 at 8:30 AM the Director of Social Services (DSS) was interviewed and asked about Resident #2 hospice care plan. The DSS indicated it was in the Hospice Care Binder. The DSS reviewed the binder and pointed out the Nursing -Updated Comprehensive Assessments and stated, it was the resident care plan. The DSS confirmed she is responsible for coordinating the care conferences and indicated part of the process it to notify hospice. She indicated she had notified hospice about Resident #2's conference that was scheduled but failed to document the notification.
On 12/15/2022 at 8:50 AM, the DSS provided a copy of the sign in sheet for Resident #2's Interdisciplinary Care Conference Attendance Record dated 10/25/2022. The DSS pointed to a signature next to attendees listed as other and stated it was from Hospice. The signature was not legible, nor did it contain a title that would indicate who had attended.
On 12/15/2022 at 8:55 AM, the Minimum Data Sheet Coordinator indicated she had attended Resident #2's Interdisciplinary Care meeting and she did not remember if a Hospice nurse had attended.
Further review of Hospice Nursing -Updated Comprehensive Assessment dated 12/14/2022, revealed the nurse had reviewed facility report and had received report from [facility nurse name] nurse. The Comprehensive Assessment was omitted of Resident #2 change in skin condition that was identified on 12/13/2022, nor did it reflect new orders for treatment, and a Dermatology consult.
On 12/15/22 at 9:00 AM, an interview was conducted with the Director of Nursing (DON)she confirmed she was not able to identify the signature on the Interdisciplinary Care Conference Attendance Record dated 10/25/2022. The DON additionally confirmed hospice care plans were not in the Hospice Health care Binder. The DON indicated at that time she made a call out to the provider.
Review of the policy titled Hospice Program that did not contain a date Policy statement: Hospice services are available to resident at the end of life. Policy Interpretation and Implementation 1. Our facility has an agreement in place with at least one Medicare-certified hospice to ensure that residents who wish to participate in a hospice program may do so. 5. Hospice providers who contract with this facility: a. must have a written agreement with the facility outlining (in detail) the responsibilities of the facility and the hospice agency; and b are held responsible for meeting the same professional standards and timeliness of services as any contracted individual or agency associated with the facility. 9. In general, it is the responsibility of the hospice to manage the residents care as sit relates to the terminal illness and relates to conditions, including the following. A. determining the appropriate hospice plan of care. 10 In general it is the responsibility of the facility to meet the residents personal care and nursing needs in coordination with the hospice representative and ensure that the level of care provided is appropriately based on the individual resident's needs. These responsibilities the following c. notifying the hospice about the following: 1) a significant change in condition in the resident's physical, mental. Social or emotional status. 12. Our facility has designated the social services department to coordinate care provide to the resident by our facility staff and the hospice staff. He or she is responsible for the following a collaborating with hospice representatives and coordination facility staff participation in the hospice care planning process for residents receiving these services. d. Obtaining the following information from hospice: (1) the most recent hospice plan of care specific to each resident. 13. The coordinated car plan will reflect the resident goals and wishes, as stated I his or her advanced directives and during ongoing communication with the resident or representative, including c. medical treatment and diagnosis tests.
Review of the Agreement for Nursing Facility, Inpatient and Inpatient Respite Services dated 4/27/21. 1.7 Hospice plan of Care means a written care plan established. Maintained, and modified as necessary) for each Hospice patient by the appropriate Interdisciplinary team. 2.1.7 Plan of Care. Per section 2.1 of Appendix C and Section 2.2 of Appendix D of the agreement, [name of provider] shall establish, modify as appropriate, and provide facility with a copy of Hospice Plan of Care for each Hospice Patient admitted to facility.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0808
(Tag F0808)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) Review of Resident #3's admission record revealed she is a [AGE] year-old resident admitted on [DATE] from and acute care hos...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) Review of Resident #3's admission record revealed she is a [AGE] year-old resident admitted on [DATE] from and acute care hospital with diagnosed that include but are not limited to Dementia, nonspecific abnormal finding of lung field, pneumonia, Gastroesophageal reflux disease (GERD) dysphagia, and Alzheimer's disease.
Review of Resident #3's physician order summary revealed an order for regular diet, pureed texture, nectar consistency for aspiration started on 11/8/2022.
Further record review revealed a chest x-ray dated 11/5/2022 revealed IMPRESSION: Patchy opacity is seen in both lungs, stable.
A meal observation was conducted on 12/13/22 at 12:25 PM; the lunch cart came to Resident #3's hallway. The Assistant Director of Nursing (ADON) was observed taking lunch trays out of tray cart and passing the trays to other staff members, staff sanitized their hands in between each resident.
On 12/13/22 at 12:32 PM, Resident #3 was observed to be sitting in her wheelchair at her bedside with her lunch tray in front of her. The resident was observed to have her fork in her hand picking at a pile of potatoes that were cut in half. The resident had fish cut into pieces, cut green beans, and potatoes cut in half with Nectar thick lemon water with a chunk of fish in her water cup. Review of her meal ticket revealed MO3, EC7 Fish, Lemon, Chateau Potatoes, [NAME] Beans cut, Lemon water-MO3
Review of the facility's Select Medical Food and Liquid Conversion to IDDSI [International Dysphagia Diet Standardization Initiative] undated, revealed MO3= moderately thick (old term honey). EC7=easy to chew.
An interview was conducted with Staff E, Registered Nurse (RN) on 12/13/22 at 12:33 PM; Staff E stated she was taking care of Resident #3. She believed the resident was on a puree diet. Staff E reviewed the electronic medical record and confirmed the resident is on a regular diet with puree consistency and thickened liquids. Staff E, RN went into Resident #3's room, removed the lid on Resident # 3's food plate and confirmed the food the resident received was not a puree consistency. Staff E was unsure as to why Resident #3 needed the puree diet. The meal tray was removed from the room by Staff F, a Certified Nursing Assistant (CNA) at this time.
An interview was conducted with the Assistant Director of Nursing (ADON) on 12/13/22 at 12:36 PM. The ADON reviewed Resident #3's medical record and stated the resident was on puree diet then changed to a diet that was regular diet, easy to chew with thickened liquids. So, I don't know why they would downgrade her diet again to puree.
An interview was conducted on 12/13/22 at 12:34 PM with Staff E, RN. Staff E stated when a new diet order gets put in, they change the order in the computer, print out the new order and take the order down to the kitchen office. Or they can give it to the unit secretary, and they can take it down or fax it down to the kitchen office.
During a further interview conducted on 12/13/22 at 4:45 PM, Staff E, RN stated I am the nurse, so I am responsible for making sure the residents receive the correct diet. Normally I am the one passing out the meal trays and I look at the tickets and the orders and make sure the food matches. I'm not sure why the ADON was passing the meal trays today, but I am the nurse for [Resident #3] so I am responsible.
During an interview on 12/13/22 at 4:50 PM, Staff D, RN stated if a physician wants to change a diet order, we input the order he requests and print out the new order provide it to the unit secretary, and they bring it down to the kitchen managers office. If a family wants a diet changed then I have to have speech therapy come and do an evaluation and then the speech therapist will input the order and take down the order or give it to the unit secretary.
An interview was conducted on 12/13/22 at 4:53 PM with Staff B, Receptionist she stated the nurses will let me know when a diet order changes, I will print out the order and I can either fax it to the kitchen office or bring it down to their office. If it is after the office closes, then I just slide it under their door, and they will get it in the morning.
On 12/13/22 at 4:14 PM, an interview was conducted with the Nursing Home Administrator (NHA) and the Director of Nursing (DON) the DON indicated based on review of [Resident #3's] lunch meal ticket and review of what MO3 and EC7 means [Resident #3] did not receive her ordered diet for lunch. Her lunch meal ticket indicates moderately thick, easy to chew. We did ask the kitchen to review the diets.
An interview was conducted with the Director of Food Services on 12/13/22 at 4:55 PM. The Director of Food Services stated he does not have access to the patient electronic medical record. The secretary's will come down to my office drop off the new diet orders, my diet clerks who work in my office will update our electronic menu software system, with the new diet order, the system will take the diet order and their preferences and create a menu for the day. I have staff here from 5:00 AM to 7:30 PM. Every morning my diet clerks review new orders that were faxed or slid under the door overnight and input them into the system and then print out the menus for each resident for the day and provide them to the line assistants who put the food trays together. The facility provided me with a diet order list for all the residents and I updated our system so the dinner meal tickets reflect their correct diet orders.
An interview was conducted on 12/13/22 at 10:21 AM with Staff J, Respiratory Therapist he stated [Resident #3] is stable from a respiratory standpoint she does receive albuterol twice a day. pulmonology is on board and following her. She is currently stable and doing well 96% on room air.
An observation was conducted on 12/13/22 at 3:06 PM. Resident #3 was observed to be in the activities room working on picking up pegs and placing them on a peg board with other residents and staff members. She was observed without cough, congestion, or respiratory distress on room air.
During a phone interview conducted on 12/13/22 at 1:30 PM, the facility's Speech Therapist indicated she has been consulted for Resident #3 since her admission due to her history of pneumonia, GERD, dementia, and she came to the facility on a puree diet with honey thick liquids. She did an initial evaluation on Resident #3 and determined she would be a good candidate for speech therapy. Resident #3 was able to consume mechanical soft diet with nectar thick liquids. The speech therapist confirmed the residents current order was a pureed because; someone must have been concerned and downgraded her diet. Pulmonology consulted me but I was already on board. Due to the residents age and her fluctuation of tolerance I left the diet order at pureed texture because it seemed the safest for the resident. The speech therapist was informed Resident #3 received an easy to chew diet for lunch; and the Speech Therapist stated in her professional opinion the resident is able to tolerate the easy to chew diet but if there were inconsistencies throughout the day with coughing, pocketing food or tiredness puree diet is the safest consistent diet to be ordered but not unsafe with an easy to chew diet. At the time of this interview the DON was present and stated the Registered Dietitian typically prints out orders from the electronic medical record and delivers it to the kitchen.
A phone interview was conducted with Resident #3's Pulmonology Advanced Registered Nurse Practitioner (ARNP) on 12/14/22 at 10:55 AM. The ARNP stated I first came on board for [Resident #3] when she was coughing and had bilateral pneumonia, when I see an elderly lady with coughing and pneumonia I think she may be aspirating so I changed her diet to puree diet because that is the safest and I ordered a speech evaluation, but speech was already working with her. I don't know what speech suggested her diet should be, but puree is definitely the safest. The ARNP was told the resident did not receive pureed food for lunch on 12/13/22. The ARNP stated: if speech recommended a mechanical soft diet, then I am fine with that too. I saw [Resident #3] on Sunday [12/11/22] her lungs were clear she was on 98% on room air I did not hear her coughing, but I am not there all the time. I don't remember ordering a chest x-ray for her but typically what I do is change the diet and give the patient 2-3 weeks then take another x-ray. I cannot remember when her last chest x-ray was. The ARNP was told the last chest x-ray was on 11/5/2022 which read bilateral opacities (a radiological term that refers to hazy gray areas on the images made by CT scans or X-rays). The ARNP stated: I may do another x-ray on her next week but clinically she is doing much better than she was when I came on board.
Review of Resident #3's care plan revised on 10/21/22 revealed-
Focus: I have a nutritional problem or potential nutritional problem r/t need for altered texture diet, need for thickened liquids . BMI (Body mass index) < (less than) 23, poor PO (by mouth) intake
Goal:
I will consume > (greater than) 50% of meals, snacks and supplements offered to me
I will maintain my CBW w/ no sig wt. [significant weight] changes
I will tolerate my ordered altered texture diet and thickened liquids
Interventions:
Provide and serve diet as ordered .
Review of the facility's Therapeutic Diets policy undated revealed
Policy statement
Therapeutic diets are prescribed by the attending physician to support the resident treatment and plan of care and in accordance with his or her goals and preferences.
Policy Interpretation and Implementation
1.
Diet will be determined in accordance with the resident's informed choices, preferences, treatment goals and wishes. Diagnosis alone will not determine whether the resident is prescribed a therapeutic diet.
2.
A therapeutic diet must be prescribed by the resident's attending physician (or non-physician provider). The attending physician may delegate this task to a registered or licensed dietitian as permitted by state law.
3.
Diet order should match the terminology used by the food and nutrition services department.
4.
A therapeutic diet is considered a diet ordered by a physician, practitioner or dietitian as part of the treatment for disease or clinical condition, to modify specific nutrients in the diet, or to alter the texture of a diet, for example:
a.
diabetic/calorie-controlled diet.
b.
low sodium diet.
c.
cardiac diet; and
d.
Altered consistency diet
Review of the facility's policy Interdepartmental Notification of Diet undated revealed
Policy Statement
Nursing services shall notify the food and nutrition services department of a resident's diet order, including any changes in the resident's die, meal service, and food preferences.
Policy Interpretation and Implementation
1.
When a new resident is admitted or a diet has been changed, the licensed nurse or designee shall ensure that the food and nutrition services department receive written notice of the diet order.
2.
The food and nutrition services department will be notified verbally if the diet change or report occurs one hour or less before a scheduled meal, or if circumstances indicate that the written procedure will not be adequate to ensure services at the next meal
Based on observation of residents at meals, interview with facility staff, and review of residents' diet orders as ordered by the Physician, the facility failed to ensure 15 residents ( Resident #1, Resident #3, Resident #6, Resident #7, Resident #18, # Resident 20, Resident #24, Resident #28, Resident #50, Resident #53, Resident #100, Resident #103, Resident #104, Resident #105, Resident #251) of 47 residents who were receiving nourishment by mouth, were receiving the correct Physician ordered diets. Observations of Resident #100 and Resident # 3 while at lunch were made to confirm the Physician ordered diet had not been served.
Findings included:
1) Resident #100 was admitted to the facility on [DATE] with multiple diagnoses including End Stage Renal Disease (ESRD). An admission note dated 12/07/2022, written at 00:40, included the resident's cognitive status as alert and oriented times 3, and ESRD as one of his diagnoses.
An admission Nutrition assessment dated [DATE], written at 15:00 reviewed the resident's diagnoses, medications, labs from the hospital dated 11/30/2022, and skin concerns (unstageable pressure injury to left heel). The Assessment documented the resident's diet was 2-gram sodium, regular texture, thin consistency fluids. There was no supplement ordered. Intake at meals was 50-75%. The resident was 66 tall and weighed 165 pounds (lbs.) / 75 kilograms (kg) on 12/06/2022. The Dietitian recommended a renal with dialysis diet with a liquid high calorie, high protein supplement to better meet the resident's needs.
An observation of Resident #100 at lunch on 12/13/2022 at approximately 12:30 PM; revealed he had received a large, breaded pork chop, roasted potatoes, and green beans with vanilla pudding for dessert. The resident reported he was enjoying the meal. The resident also had received and had consumed most of a bowl of chicken broth. He confirmed he had eaten most of the broth but reported it was very salty.
A review of the resident's diet slip revealed he had been provided with a 2-gram sodium diet.
A review of the menu for 12/13/2022 revealed the Renal Chef Select Menu was planned to provide residents with a turkey burger on a bun, a garden salad without tomato, carrot and celery sticks and a cookie for dessert. An alternate menu was planned for the Renal Chef Select diet which would have provided the resident with Chicken and Mozzarella, no tomato, with spaghetti, green beans, and a garden salad. Resident #100 had received neither of those planned meals, which would have corresponded to his recommended Renal with dialysis diet.
An interview was conducted on 12/15/2022 at approximately 11:30 AM; with the Dietary Manager who reported that the facility's planned Heart Healthy Diet included the sodium modified to 2 grams. The Dietary Manager confirmed that the 2-gram sodium diet was based on the Heart Healthy Diet.
The Registered Dietitian's recommendation to change Resident #100's diet from 2-gram sodium ordered at admission to a renal with dialysis diet had not been implemented seven days later.
Resident #4 Physician ordered diets was reviewed and compared to the diet slips used to guide the tray line in preparing the meal trays for the residents revealed the wrong diet provided.
Further review revealed of the 47 residents who had Physician ordered diets for by mouth nourishment, 15 residents (32%) had received the wrong diet, related to either the Therapeutic modification or the texture modification.
The following identifies the diet received on 12/13/2022 at lunch as compared to the Physician ordered diet:
Resident #7 received a 2-gram sodium diet at lunch, but her Physician's ordered diet was a regular.
Resident # 100 received a 2-gram sodium diet at lunch, but his Physician's ordered diet was a renal with dialysis diet.
Resident # 18 received a minced and moist, 2-gram sodium, carbohydrate-controlled diet but her Physician's ordered diet was a soft & bite sized, 2-gram sodium, carbohydrate-controlled diet.
Resident #103 received a 2-gram sodium diet, but her Physician's ordered diet was 2-gram sodium, carbohydrate-controlled diet.
Resident # 20 received a 2-gram sodium diet, but her Physician's ordered diet was an easy to chew diet.
Resident # 1 received a heart healthy diet, but his Physician's ordered diet was regular.
Resident # 104 received a soft & bite sized with carbohydrate-controlled diet, but her Physician's ordered diet was soft & bite sized.
Resident # 3 received a soft & bite sized diet with moderately thick liquids, but her Physician's ordered diet was pureed with mildly thick liquids.
Resident # 251 received an easy to chew diet, but her Physician's ordered diet was easy to chew with high protein high calorie foods.
Resident # 105 received a heart healthy, 2-gram sodium, carbohydrate-controlled diet but her Physician's ordered diet was a heart healthy, 2-gram sodium, fat restricted, carbohydrate-controlled diet.
Resident # 28 received a renal without dialysis diet, but his Physician's ordered diet was a renal with dialysis diet.
Resident # 50 received a 2-gram sodium, easy to chew diet, but his Physician's ordered diet was a soft and bite sized diet.
Resident # 24 received a heart healthy, 2-gram sodium, fat restricted diet but her Physician's ordered diet was a heart healthy, fat restricted diet.
Resident # 6 received a heart healthy diet, but her Physician's ordered diet was a heart healthy, easy to chew diet.
Resident #53 received a 2-gram sodium diet, but her Physician's ordered diet was a heart healthy, 2-gram sodium diet.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interview and facility record review, the facility failed to ensure call lights were maintained and...
Read full inspector narrative →
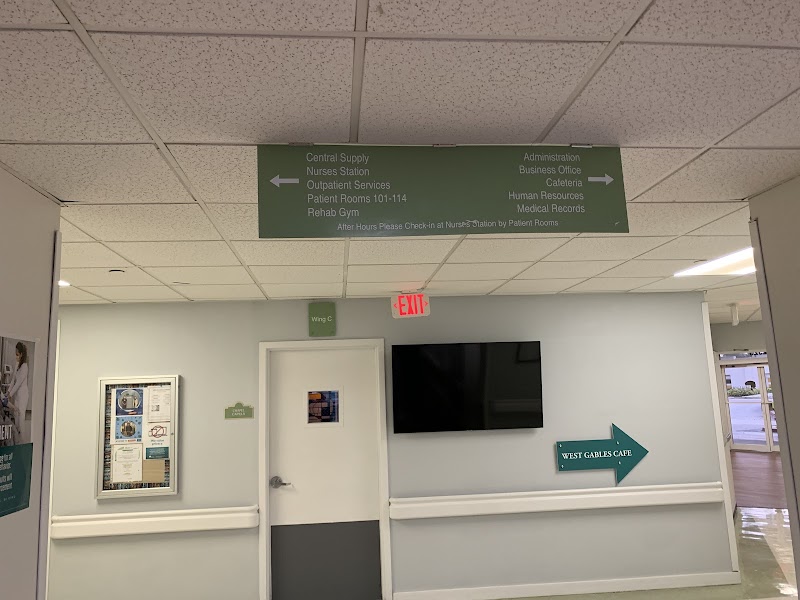
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interview and facility record review, the facility failed to ensure call lights were maintained and working effectively in three of thirty-three resident rooms, on three of three halls (wing A, wing B, and wing D). It was determined when pressing the pneumatic plastic bulbs, the call system did not activate.
Findings included:
1. On 12/12/2022 at 10:28 AM the A wing was toured. Upon entering resident room [ROOM NUMBER] at 10:50 AM., both bed (a) and bed (b) call lights were tested for working maintenance. room [ROOM NUMBER] bed (a) was observed with a pneumatic bulb button. Upon pressing/squeezing the pneumatic bulb, it was determined the system did not trigger. Further observations revealed the light out in the hallway above the room door did not illuminate. The pneumatic bulb was pressed/squeezed four times and still the light did not trigger out in the hallway. At 10:55 AM, an interview with Certified Nursing Assistant (CNA) employee C, revealed that all call lights regardless even if the resident is able to use it or not, are to be placed within their reach when in bed and when in the room. Employee C also confirmed that the lights should always be in working order and that she did not know who was responsible for the general maintenance of the call lights.
On 12/13/2022 at 10:00 AM, an interview with the Nursing Home Administrator (NHA) and the Maintenance Director, both revealed that all call lights in rooms and bathrooms are checked monthly per their [] maintenance system, and that this month's (December's) check has not been conducted as of yet. The NHA also indicated that floor staff to include nurses and aides would be responsible to notify maintenance or himself if call lights were not working appropriately. He also confirmed that it is facility policy for all call lights to be functioning, even for the residents who are not able to use them.
The Maintenance Director revealed he would go ahead and do a building-wide check of all the resident rooms and bathrooms to ensure all are working. He provided the last four months (8/2022, 9/2022, 10/2022, 11/2022) of Nurse Call Checks audits for review. Review of the 8/2022 Nurse Call Check audit, revealed all rooms were checked and passed. Review of the 9/2022 Nurse Call Check audit, revealed all rooms were checked and passed. Review of the 10/2022 Nurse Call Check audit, revealed all rooms were checked and passed. Review of the 11/2022 Nurse Call Check audit, revealed all rooms were checked and passed.
During the survey on 12/14/2022, the Maintenance Director performed a call light audit, after the 12/13/2022 observations of call lights not working. The maintenance director and Nursing Home Administrator also revealed that staff should be letting his maintenance department know if there are any lights not working, as they see them. He did not have any current work orders that reflected the above listed non-working lights.
2. On 12/12/22 at 12:06 PM; room [ROOM NUMBER] bed (a) call light was tested and the light outside of the room did not come on. Staff A, CNA tested the call light and confirmed the call light was not working. Staff A stated yesterday it was working and confirmed the resident could use the call light if she needed to.
A second test on the call light was conducted for functionality for room [ROOM NUMBER] bed (a) on 12/15/2022 at 10:00 AM and it was discovered that the call light was still not functioning as intended.
A third test was conducted for functionality on 12/15/22 at 11:45 AM after the facility was made aware by the survey team, and room [ROOM NUMBER] bed A's call light was tested with Staff A, CNA and she confirmed the call light system was functioning as intended. Staff A reported that maintenance told her that the cord gets kinked, so we have to make sure that does not happen.
3. On 12/13/2022 at 12:10 PM, Resident # 100 was observed lying in bed. He agreed to a visit and reported that usually call bell response was good. He activated the call bell to demonstrate and when the surveyor stepped into the hall to see if the light above his door was lit because no sound was heard from the bell, observation revealed the light above the door was not lit. Resident #100 tried to activate the bell several times but the light above his door was not turning on.
A request was made to Staff I, CNA who was present in the hall to try the bell and she had the same results. After confirming that the bell was not working Staff I left the room. The surveyor remained to speak with the resident who reported that he did not know the call bell was not working.
After approximately five minutes, the surveyor left the room and approached Staff I, CNA to determine what her next step was related to the call bell. Staff I reported she had already notified maintenance that the bell was not functioning.
At 12:35 PM, staff were observed approaching Resident #100's room pushing a small cart which was carrying multiple replacement call bells. The staff was able to replace the call bell and the call bell was functioning.
On 12/15/2022 at 10:00 AM, the Nursing Home Administrator provided the facility's Call System, Resident policy and procedure for review. The undated policy heading revealed; Residents are provided with a means to call staff for assistance though a communication system that directly calls a staff member or a centralized workstation. The policy further revealed to include but not limited to:
(1)
Each resident is provided with a means to call staff directly for assistance from his/her bed or other sleeping accommodations.
(2)
The call system communication may be audible or visual. The system may be wired or wireless.
(3)
The resident call system is routinely maintained and tested by the maintenance department.
(4)
Calls for assistance are answered as soon as possible.
(5)
If the call system requires repair, an alternate means of communication is implemented for the affected resident(s).
(6)
Call light function and response should be reviewed as part of the QAPI program.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interviews, and record review it was determined that the dish machine wash temperature did not reach the minimum manufacturer's recommended wash temperature as posted on the dish...
Read full inspector narrative →
Based on observation, interviews, and record review it was determined that the dish machine wash temperature did not reach the minimum manufacturer's recommended wash temperature as posted on the dish machine's face plate.
Findings included:
At 9:30 AM on 12/12/2022, a diet aide was observed running racks of dirty dishes through the dish machine. The wash and rinse temperature gauges were observed to read 150 degrees Fahrenheit (F) for the wash cycle and 180 degrees F for the rinse cycle. Observation of the manufacturer's face plate posted on the dish machine indicated the required temperature for the wash cycle should be at a minimum of 160 degrees F and the rinse cycle temperature should be at a minimum of 180 degrees F.
Several racks of dishes were observed that had been run through the machine without the wash temperature reaching the manufacturer's required minimum of 160 degrees F.
The Dietary Manager reported that he had been told by the service company for the dish machine that the surface of the dish would be at 160 degrees F but the ambient air in the dish machine would reduce the wash water temperature to below 160 degrees F. When it was suggested that the water temperature could be increased to ensure the wash temperature remained at or above 160 degrees F, as the rinse temperature was being maintained at 180 degrees F, there was no response from kitchen staff.
A review of the dish machine temperature log revealed that for every shift on the December 2022 log, the temperatures were documented at 160 degrees F for the wash temperature and 180 degrees F for the rinse temperature.
The dish machine service company provided service to the dish machine on 12/12/2022, with their service report documented at 1:47 PM, for the request description (of the visit) of temperature issue. Service comments on the service call document read: Replace gauge for security, machine work perfect in range temperature. The summary of the visit read: The dishwasher is in perfect condition; the washing temperature reaches 160 degrees F, and the final rinse exceeds 180 degrees F.
The service report indicated a photograph had been taken of the temperature gauge during the wash cycle. Observation of the photograph of the wash temperature gauge revealed the temperature was at approximately 152 degrees F, which is approximately 8 degrees below the manufacturer's guidelines for the minimum temperature during the wash cycle. The photograph of the rinse temperature showed the gauge was at 180 degrees F, which is at the minimum temperature indicated by the manufacturer's guidelines.