CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to protect one (Resident #1) out of three residents samp...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to protect one (Resident #1) out of three residents sampled during the time of this survey. The facility's staff (Staff A Licensed Practical Nurse (LPN), Staff C LPN and Staff D, Certified Nursing Assistant) failed to supervise and implement adequate measure to prevent the elopement of Resident #1 who was exit seeking, wandered the unit, and wandered near exit doors. The facility neglected to adequately monitor and address Resident #1's displayed exit seeking behaviors and intent of elopement. The facility's system failure, lack of adequate supervision and a failure in ensuring an adequate alert monitoring system was in place allowed the resident to elope undetected by staff on 1/19/2024 at 1:34 AM on foot and the facility's staff did not begin the search until 2:50 AM and did not find the resident. The facility is located in an area where there is heavy 40 miles per hour 2 lane traffic. The resident still has not been located at the time of the survey.
Refer to F 607, F 689, F 835, and F 867.
The findings included:
Record review of the facility's policy titled, Abuse, Neglect, Exploitation and Misappropriation Prevention Program Policy and Procedure revision date was on 04/2021, the policy documented: The facility will provide a safe resident environment and protect all residents from abuse. Therefore, each resident has the right to be free from abuse, neglect, misappropriation of resident property and exploitation of any type by anyone. Neglect means failure of the facility, its employees or service providers to provide goods and services to a resident that are necessary to avoid physical harm, pain, mental anguish, or emotional distress. A prompt thorough investigation will be conducted by the facility immediately.
Review of the Demographic Face Sheet for Resident #1 documented the resident was initially admitted on [DATE] with a diagnosis that include but not limited to Alzheimer's disease, seizures, and glaucoma.
Review of Resident's #1's Elopement care plan dated 4/21/2021 documented the resident has a potential for elopement risk related to cognitive impairment, who was exit seeking, wandered the unit and wandered near exit doors; Goal: Resident will be safe and will refrain from leaving facility unsupervised thru the next review date; Interventions: Perform frequent observations of residents whereabouts every shift; Provide redirection when observed going towards exit door; Apply alarm bracelet as ordered on right wrist; Verify placement every shift and check for proper functioning weekly.
Review of the progress notes documented the following: Dated 1/19/2024 time stamped 06:25-Narrative Nurses Note: 1900 during initial round, resident was seen walking around the hallway and was redirected to her room. 2130 resident was found walking in the hallway again and said, I want to go home. Due meds given and was putting back to her bed. All safety measures were in place. 2300 while passing by the laundry area, noticed the resident was getting her hair groomed by a CNA( Certified Nursing Assistant). 0000 observed resident putting to bed by her CNA and stayed in the room with her to make sure she stays in bed. 0030 resident was observed walking out of her room towards the nursing station. Initiated and placed resident in a chair to sit in the nurse's station. 1:19 am observed resident standing in front of nurses station counter and was redirected to her room. 1:22 AM observed resident walking in hallway while doing routine check and redirected back to her room. 2:40 AM while making routine round alarm heard, resident was . missing from assigned room. Initiated elopement protocol, code green initiated. 3:25 AM police . notified about resident missing. ADON (Assistant Director of Nursing) was notified. Message left for family member. Medical doctor was notified. The progress notes written by Staff C, Licensed Practical Nurse (LPN). Dated 1/19/2024 time stamped 10:30 AM Narrative Nurses Note: Administrator spoke to the family when she returned the call. Administrator informed the family about patient elopement and gave the family the report of the actual situation.
Review of the Physician's Order Sheets (POS) and Medication Administration Records (MAR) for December 2023 and January 2024 documented the resident was receiving the following medications: Namenda 10mg (milligrams) tab (tablet) 1 tab PO (by mouth) BID (twice a day) for mood; Donepezil HCL (hydrochloric acid) 10mg tab 1 tab PO HS (at night) for dementia and apply [wander management] alarm bracelet to right wrist. Check for placement shift and functioning Q (every) week. Report any issues immediately to supervisor. The order start date was 8/24/2022. The [wander management] alarm bracelet was checked every day for December 2023 and January 2024 and indicated the resident was wearing it.
Review of the Elopement Risk Assessment/Evaluation dated 3/23/2023 and 6/29/2023 documented: The resident is at low risk for elopement, does not wander and has never eloped.
On 1/30/2024 at 9:54 AM, the Administrator/Risk Manager/QAA (Quality Assessment and Assurance) stated: I received a call at approximately 3:30 AM and received a report of a missing person and they didn't retrieve the person. I immediately got in my car and was on my way to the facility for coming to assist with the search. I called [local state agency] and they accepted the case. The [local law enforcement] was in contact with the facility. On 1/19/2024, the incident occurred. I submitted the one-day report to the [local state agency] with the information given. When I arrived, to the facility the corporate team and other Administration personnel were at the facility investigating the elopement. The investigation was ongoing with the corporate team. I participated in QA (quality assurance) with the department heads. I reached out to the resident's family member. I let her know her great aunt was missing, and we are actively looking for her and would provide updates. The resident's niece let us know that she missed out on the calls from the facility earlier. The resident's niece stated the resident's responsible party on file was currently in a nursing home and is hard to reach. The resident remains missing at this time. The [ local state agency] five (5) day report indicated the elopement was attributed to the lack of supervision by the two (2) nurses- one (1) Registered Nurse (RN), one (1) Licensed Practical Nurse (LPN) and one (1) Certified Nursing Assistant (CNA), they were all placed on suspension on 1/19/2024. We immediately got to work on the response plan. The findings were as stated in the [local state agency] 5-day report, the allegation of neglect was substantiated. The [wander management] alarm bracelet red light never came on but the door with the egress alarm did go off.
On 1/30/2024 at 10:06 AM, the Registered Nurse (RN), Regional Clinical Director stated: Based on the footage from the camera, it appears that the resident did not have an [wander management] alarm bracelet on, the red light did not go off as it should when a resident with a [wander management] bracelet gets near the exit door. She did not have a [wander management] alarm bracelet. The egress door alarm did go off. We educated the licensed nurses to review the elopement assessment. Clinical and non-clinical staff and agency staff were educated on elopement and abuse and neglect, and this would include ongoing education with new hires. The nurses and CNA involved in the resident's elopement were terminated and reported to the board of nursing.
On 1/30/2024 at 10:36 AM, Staff A, Licensed Practical Nurse (LPN) via telephone stated, I was working on the 11-7 AM shift on 1/19/2024, I was sitting at the desk and doing daily assessments and the resident was sitting with me, she got up and walked to the side. At 1900 I prepared to make rounds, upon making rounds all 30 residents were accounted for awake and alert. I accepted Medication Cart #2 keys, counted narcotics, and started with med pass. Around 11:30 PM, I stopped to eat. At around 12:00 AM, I started charting sitting at the desk. At that time the resident was at the nursing station with me. The resident got up and walked around the South side of the nursing station. Between 1:45 AM, the call light went off in room [ROOM NUMBER], bed C, I went to assess the resident. When I returned to the nurse's station I saw the light at the back door blinking. I realized that someone had opened or touched the door. I went to the door to check it. I never heard an alarm on the door go off. I just saw the red-light blinking. I was facing the door and went to check the resident's (Resident #1) room and she was not in the room. I went to the resident's room because she was the only resident that was up at that time by the nurses' station. I was not the nurse assigned to the resident. I alerted everyone and a code green was called, and we started the search. I took my truck and drove around the facility looking for the resident. Sometimes the resident would be up at night at the nurse's station. This was common for her to be up at night. I don't recall her having on an [wander management] alarm bracelet. I then ran into the [law enforcement officer] and brought the [law enforcement officer] back to the facility to take a profile of the resident we were looking for. I was suspended from the facility on 1/19/2024. They didn't tell me how long I would be suspended and then I resigned on 1/23/2024.
On 1/30/2024 at 10:59 AM, Staff B, RN (Registered Nurse) via telephone stated: The staff realized that the resident was missing, and we started a search. I called the ADON (Assistant Director of Nursing) to let administration know what was going on. I was the RN in the building that night. I was assigned to the South wing. [ Staff C, LPN] was assigned to the resident.
On 1/30/2024 at 11:04 AM, Staff C, LPN via telephone stated, I am busy at the moment and doing something. Call me back in five hours. Attempted a second contact at the designated time and did not receive any response.
On 1/30/2024 at 11:08 AM, Staff D, Certified Nursing Assistant (CNA) via telephone stated: After 11:00 PM, I signed into work. I made rounds and I didn't see the patient in the room. I told the nurse [Staff C, LPN] and she said the patient is here with me. The resident liked to walk around. I go to the laundry room and pick up my cart. The patient was in the hallway. I talked to her and told her to come with me. I took her to her room and had her sit on the bed. Every day she walked around. [Staff A, LPN and Staff C, LPN] were at the nursing station. I noticed the patient was missing at 2:30 AM. I made rounds; I didn't see the patient in her room. I called the nurse and told her I could not find the resident. I opened the bathroom door, and I didn't see her. I went outside and I didn't see her.
On 1/30/2024 at 11:35 AM observation of the video of the resident exiting the building and interview with the Regional Director of Operations stated, The resident walked out of the door and the alarm for the door went off and the nurse [Staff A, LPN] was sitting at the North wing nurses station and did not get up. The resident was wearing an alarm bracelet and the alarm on the [wander management] alarm bracelet did not sound off. According to our investigation and interviews with the nurses, the resident was not wearing a [wander management] alarm bracelet. I have been checking the ME's (Medical Examiner's) office every day since the resident left. She has not been found yet.
During observational review of the facility's video footage via the computer that was approximately 3 to 4 minutes in duration with the Regional Director of Operations on 1/30/2024 at 11:35 AM. The video footage revealed that on 1/19/2024 at 1:33 AM, Resident #1 was dressed in a black dress with pink socks and a white blanket wrapped around her shoulders was pacing back and forth in the North wing hallway, during this time Staff A, LPN was sitting at the North wing nurses station with her head down. On 1/19/2024 at 1:34 AM Resident #1 pushed the door without any difficulty at 1:34 AM on 1/19/2024 and exited the facility undetected by staff. The resident walked out of the facility with no assistive device and proceeded through the north egress (emergency exit) double door that lead to the facility's courtyard on the north wing. The alarm on the exit door was not audible for staff to hear throughout the facility within the care areas beyond the double doors.
The scope and severity of F600, was lowered to a (D) for No actual harm with a potential for more than minimal harm that is not immediate jeopardy as of 2/01/2024. The scope and severity were lowered as a result of the facility's corrective actions implemented as of 2/01/2024. These corrective actions were verified by the survey team through observation, record review and interview from 1/30/2024 to 2/01/2024.
The facility's immediate jeopardy removal plan included:
The staff (128 persons) at 100% were in-serviced/trained on 1/19/2024 to 1/29/2024, regarding: how to respond to call lights promptly, elopement drills, codes, and emergencies responses, how to respond to door alarms, competency for elopement training, how to deal with patients that have behaviors, behavior management for exit seeking resident, abuse, neglect and exploitation training, accidents, and hazards and the QAPI process with the administrative team. The facility conducted a thorough inspection of all eight (8) exit doors and their existing alarm systems to make sure they are in working order in the facility, each exit door has a wander guard alarm, a screamer alarm (installed 1/19/2024) and an egress maglock (magnetic lock) alarm with a 15 second opening delay. The alarm systems are audible and can be heard at their loudest in the area where it goes off and is reasonably audible throughout the facility.
Nurses are assigned to check residents with wander guards at least once per shift for placement and functionality. The Elopement Risk Book was revised on 01/28/2024, contains-List of Residents, Guidelines for elopement /Unsafe Wandering Prevention, Facility Floor Plan, Pictures of Residents for elopement, Face sheets, Elopement Drill Schedule, and Elopement Mock Drills protocol.
A 6-foot fence was installed to the north courtyard to ensure that residents are not able to exit to the neighborhood and busy streets from the facility's courtyard on the north wing.
Maintenance staff or their qualified designee will conduct weekly door audits to ensure all doors are in proper working order, including checking that the alarm is audible at the nursing station and care areas.
An audit of all residents who reside in the facility was conducted to evaluate the risk of leaving the facility without informing staff and/or if they may desire to leave the facility. Additional Audits-Dated 1/19/2024 to 1/27/24; Elopement Drill Audit, Dated 1/20/2024 to 1/28/2024; [Wander management alarm] bracelet Audit, Dated 1/21/2024 to 1/26/2024; Daily Door Audits (All shifts), Dated 1/21/2024 to 1/27/2024; Elopement Drill/Actual Event Evaluation, Dated 1/28/2024; Facility Search Grid.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Abuse Prevention Policies
(Tag F0607)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, the facility failed to implement their abuse and neglect policy as evidenced by staffs' ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, the facility failed to implement their abuse and neglect policy as evidenced by staffs' failure implement the facility's policy related to wandering and elopement and failed to provide care and services including adequate supervision for one (Resident #1) out of three residents sampled. This deficient practice enabled Resident #1 to exit the facility at 1:34 AM on 01/19/2024, undetected. The facility's system failure, lack of adequate supervision and a failure in ensuring an adequate and effective alert monitoring system was in place, allowed the resident to elope undetected. The resident has not been located as of 02/01/2024.
The findings included:
Review of the facility policy titled Abuse, Neglect, Exploitation and Misappropriation Prevention Program revised April 2021 documented: Residents have the right to be free from abuse, neglect, misappropriation of resident property and exploitation. This includes but not limited to freedom from corporal punishment, involuntary seclusion, verbal, mental, sexual, or physical abuse, and physical or chemical restraint nit required to treat the resident's symptoms.
Policy Interpretation and Implementation
The resident abuse, neglect and exploitation or misappropriation of property by anyone including, but not necessarily limited to:
2. Develop and implement policies and protocols to prevent and identify:
a. abuse or mistreatment of residents
b. neglect of residents; and/or
c. theft, exploitation, or misappropriation of resident property
6. Provide staff orientation and training/orientation programs that include topics such as abuse prevention, identification and reporting of abuse, stress management, and handling verbally or physically aggressive resident behavior.
7. implement measures to address factors that may lead to abusive situations, for example:
a. Adequately prepare staff for caregiving responsibilities.
8. Identify and investigate all possible incidents of abuse, neglect, mistreatment, or misappropriation of resident property.
11. Establish and implement a QAPI review and analysis of reports, allegations or findings of abuse, neglect mistreatment or misappropriation of property.
Record review of the facility's policy titled Wandering and Elopements revision date March 2019 documented: The facility will identify residents who are at risk of unsafe wandering and strive to prevent harm while maintaining the least restrictive environment for residents.
Policy Interpretation and Implementation
1 If identified as a risk for wandering, elopement, or other safety issues, the resident's care plan will include strategies and interventions to maintain the resident's safety.
2 If an employee observes a resident leaving the premises, he/she should:
a.
Attempt to prevent the resident from leaving in a courteous manner.
b.
Get help from other staff members in the immediate vicinity, if necessary; and
c.
Instruct another staff member to inform the charge nurse or director of nursing services that a resident is attempting to leave or has left the premises.
3 If a resident is missing, initiate the elopement/missing resident emergency procedure:
a.
Determine if the resident is out on an authorized leave or pass.
b.
If the resident was not authorized to leave, initiate a search of the building(s) and premises; and
c.
If the resident is not located, notify the administrator and the director of nursing services, the resident's legal representative, the attending physician, law enforcement officials, and (as necessary) volunteer agencies (i.e. emergency management, rescue squads, etc.)
4 When the resident returns to the facility, the director of nursing services or charge nurse shall:
a.
Examine the resident for injuries.
b.
contacts the attending physician and report findings and conditions of the resident.
c.
notifies the resident's legal representative (sponsor)
d.
notify search teams that the resident has been located.
e.
complete and file an incident report; and
f.
document relevant information in the resident's medical record
Review of the medical records for Resident #1 revealed the resident was admitted to the facility on [DATE] and re-admitted on [DATE]. Clinical diagnoses included but not limited to: Alzheimer's disease, Dementia, anxiety, and Seizures.
Review of the Physician's Orders Sheet for January 2024 revealed Resident #1 had orders that included but not limited to: order dated 8/24/2022- Apply/maintain [wander management] alarm bracelet to right wrist. Check for placement and functioning every shift. Report any issues immediately to the supervisor. Medications Include: Namenda Tablet 10 MG (Memantine HCl)-Give 1 tablet by mouth two times a day for mood. Donepezil HCl Tablet 10 MG-Give 1 tablet by mouth at bedtime for dementia.
Record review of the Electronic Medication Administration Record (EMAR) for 1/1/2024 to1/18/2024 revealed Resident #1 was checked off on the EMAR as having an [wander management] alarm bracelet on by assigned nurses.
Record review of Resident #1 's Quarterly Minimum Data Set (MDS) dated [DATE] revealed: Section C for Cognitive Pattern documented Brief Interview for Mental Status score (BIMS) 5 on a 0-15 scale indicating the resident is cognitively impaired. Section E for behaviors documented Resident experiences Delusions (misconceptions or beliefs that are firmly held, contrary to reality). Resident wandered 1to 3 days. Section GG for Functional abilities documented no impairment of upper and lower extremity, no mobility devices used, supervision for sitting to standing position, chair to bed transfer, toilet transfer, tub/shower transfer, and walking 10 feet. Partial assistance for walking 50 feet and substantial assistance for walking 150 feet.and Section P for restraints documented wander elopement alarm used daily.
Review of the Elopement Risk Assessment/Evaluation dated 3/23/2023 and 06/29/2023 documented: Score of 0-9. LOW RISK for elopement. No interventions at this time.
Record review of Resident #1's most recent Psychological consult dated 2/2021 documented: Resident appears calm, cooperative, in no apparent distress at this time.
Record review of Resident #1 's Elopement Care Plans Reference Date 04/12/2021 revealed: Resident has a potential for elopement due to: cognitive impairment, has periods of increased confusion, is exit seeking, is (I) ambulatory, wanders the unit & wanders near exit doors, has a history of elopement. 01/19/2024 elopement. Interventions Include: Educate resident/responsible party regarding sign out procedures as needed. Perform frequent observations of resident's whereabouts every shift. Provide redirection when observed going towards exit doors. Encourage resident to participate in activities of choice; provide 1:1s as needed. Apply [wander management] alarm bracelet as ordered (R) wrist. Verify placement every shift. Check for proper functioning weekly. Include resident in Elopement Book and Update physician and responsible party if resident elopes.
Review of the Narrative Nurses notes for Resident #1 dated 01/19/2024 timestamped 06:25 documented: Administrator spoke to the family member when she returned the call, Administrator informed the family about patient elopement and give the family the report of actual situation.
1900 During initial rounds, resident was seen walking around the hallway and was redirected to her room. Resident was found walking in the hallway again and said, I want to go home. Medications due were given to the resident and resident was placed in bed. All safety measures were in place.
At 2300 while passing by the laundry area, nurse noticed the resident was getting her hair groomed by a Certified Nursing Assistant (CNAs).
At 0000 observed resident being put to bed by her CNAs and stayed in the room with her to make sure she stayed in bed.
At 0030 Resident was observed walking out of her room towards the nursing station. Initiated and placed resident in a chair to sit in the nurse's station.
At 1:19 AM observed the resident standing in front of nurses' station counter and redirected to her to her room.
At 1:22 AM observed resident walking in the hallway while doing routine check and redirected back to her room.
At 2:40 AM while making routine rounds, alarm heard, resident was found missing from assigned room. Initiated elopement protocol, code green initiated.
At 3:25 AM police .notified about the resident missing. Assistant Director of Nursing (ADON) was notified, message left for family member, medical doctor was notified.
The National Weather Service (www.weather.gov) Climate Data for the Miami area on January 19, 2024, ranged from temperatures of 69 degrees Fahrenheit (F) to 77 degrees F.
Interview on 01/30/2024 at 10:00 AM Administrator (NHA), Risk Manager, Quality Assurance (QA), stated: I received a call at approximately 3:00 AM to 3:30 AM on 1/19/2024, I was out of town, I got report that there was a missing person at the facility, immediately I got in the car and was on my way to facility, When I got to the facility the corporate response team were already there. I called the police, [Local State Agency] and made the report on my way to the facility. [Local State Agency] accepted the case, I submitted the immediate report to Agency for Health Care Administration (AHCA), when I arrived at the facility the corporate team and other Administration personnel were at the facility investigating the elopement. The investigation was ongoing with the corporate team. I participated in QA with the department heads, I reached out to the resident's family members, the resident's niece let us know that she missed out on the calls from the facility earlier, the resident's niece stated the resident's responsible party on file was currently in a nursing home and is hard to reach. I was placed on leave/suspension on 1/19/2024 by the corporate team while the investigation continued. I was reinstated on Friday afternoon 1/26/2024. The AHCA five (5) day report indicated the elopement was attributed to the lack of supervision by the two (2) nurses- one (1) Registered Nurse (RN), one (1) Licensed Practical Nurse (LPN) and one (1) Certified Nursing Assistant (CNA), they were all placed on suspension on 1/19/2024. The resident is still missing at this time, we immediately got to work on the response plan. The findings were as stated in the AHCA 5-day report, it was substantiated. The [wander management] alarm bracelet red light never came on but the door with the egress alarm did go off.
Interview on 1/30/2024 at 10:15 AM The Regional Clinical Director (RCD) stated: Based on the footage from the camera, it appears that the resident did not have a [wander management] alarm bracelet on, the red light did not go off as it should when a resident with a [wander management] alarm bracelet gets near the exit door. The egress door alarm did go off. Clinical and non-clinical staff and agency staff were educated on elopement, and abuse and neglect and this would include ongoing education with new hires. The nurses and CNA involved in the resident's elopement were terminated and reported to the board of nursing.
Interview on 1/30/2024 at 10:36 AM Licensed Practical Nurse (LPN) (Staff A) via telephone stated: I was working on the 11 to 7 AM shift on 1/19/2024, all I remember is that I was sitting at the desk doing skin assessments checks, the resident was sitting with me, she got up and walked to the side. At 1900 I clocked in and made rounds, the 30 residents were accounted for, awake and alert, I accepted Medication Cart #2 keys, counted narcotics and started with med pass, around 11:30 PM ,I stopped to eat, at 12:00 AM I started charting sitting at the desk, at this time resident was at nursing station with me, resident got up and walked around the south side of the nurses station, between 1:45 AM the call light went off in room [ROOM NUMBER] bed C, I went to assess the resident, when I returned to the nurse's station I saw the light at the back door blinking, I realized that someone had opened or touched the door, I went to the door. I never heard an alarm go off, I just saw the red-light blinking, I went to check the resident's room, the resident was not in the room, I alerted everyone, and a code green was called, I went to the resident's room because she was the only resident that was up at that time by the nurses' station. I took my truck and went around the facility looking for the resident. Sometimes the resident would be up at night at the nurse's station, I do not recall if the resident had on an [wander management] Alarm bracelet. I then ran into the police officer and brought the officer back to the facility to take a profile of the resident we were looking for. I was not the nurse assigned to the resident. I was suspended from the facility on 1/19/2024 and I ended up resigning on 1/23/2024.
Interview on 1/30/24 at 11:03 AM Registered Nurse (RN) (Staff B) via telephone stated: On 1/19/2024, the staff realized that the resident was missing, we started a search, I called the ADON (Assistant Director of Nursing to let administration know what was going on. I was the RN in the building that night, I was assigned to the South Wing. [Staff C, LPN] was assigned to the resident.
Interview on 1/30/2024 at 11:07 AM Staff C, LPN via telephone stated: I am busy at the moment, call back in 5 hours.Another surveyor on the team called Staff C back at the designated time and did not receive any response.
Interview on 1/30/2024 at 11:09 AM CNA (Staff D) via telephone stated: I started to work at 11:00 PM on 1/18/2024, I did my rounds, I did not see the resident in her room, I called Staff C and told her, the resident was not in her room, the nurse said the resident was at the nurses' station. I went to get linen to start doing my job, I saw the resident in the hallway, I took her by the hand and led her into her room and had her sit on the bed. Everyday this resident walks around. The nurses [Staff A and Staff C] were at the nursing station. Around 2:30 AM I made my rounds, I did not see the resident in her room, I called the nurse and told her I could not find the resident, I checked all the rooms and the shower rooms, I checked outside and did not find the resident. Staff D ended the interview and hung up the phone.
Interview on 1/30/2024 at 11:40 AM Regional Director of Operations (RDO) showed surveyors a video dated 1/19/2024 via the computer that lasted approximately 3 to 4 minutes (time stamped 1:31 AM to 1:34 AM) in duration, depicting Resident #1 walking back and forth in the hallway on the north wing/unit and eventually exiting through the door leading to the unfenced/open courtyard. The video also shows a nurse sitting at the nurse's station on the north wing/unit. The RDO stated: According to our investigation and interviews with the nurses, the resident was not wearing an [wander management] alarm bracelet.
Interview on 1/31/2024 at 7:36 AM the NHA stated: According to the footage the resident left the facility around 1:33 AM, based on the staff account the search for the resident started at 2:30 AM.
Interview on 1/31/2024 at 7:39 AM the Regional Clinical Director (RCD) stated: I interviewed all the staff before the shift was over, I interviewed [Staff A], she stated she was in the resident's room, I was busy doing resident care, no mention of what resident she was taking care of, we let the nurses know (Staff A and Staff C) we reviewed the camera footage and showed [Staff A] the camera footage. [Staff A] acknowledged she was sitting at the desk, stated she did hear an alarm .thought it was a call light or a resident who I know that really does not need anything. We asked her if she heard the alarm, [Staff A] replied, yes I heard the alarm. The video showed that [Staff A] did not get up from the nurses' station when the alarm went off. The RCD stated: In the immediate report the information about [Staff A] responding to the South Egress note is a typo by the NHA, he was driving from [NAME] in his car and doing the report at the time. On 12/20/2023 the [wander management] alarm bracelet was checked specifically for this resident. [Staff As stated] she heard the alarm go off, thought it was a call light. Staff in the facility responded to the alarm at 2:30AM. According to the orders the maintenance Director checks the [wander management] Alarm bracelet monthly, the last audit for the resident's [wander management] Alarm bracelet was completed on 12/20/2023. According to the video the alarm started going off at 1:33 AM and staff responded at 2:30 AM. Three staff members got into their cars and went in opposite directions searching for the resident for approximately 30 minutes. The alarm was turned off by the Maintenance Director at approximately 4:00 AM on 1/19/2024. No one on the staff on the morning of 1/19/2024 had a code to turn off the alarm. The resident was being closely monitored at the nurse's station from the night of 1/18/2024 into the morning of 1/19/2024. The resident's room is right next to the nursing station, and she was monitored frequently.
Interview on 1/31/2023 at 7:57AM, the Maintenance Director stated: I was checking the [wander management] Alarm bracelet weekly before the incident and currently they are checked daily every shift. I check the alarm using the [wander management] alarm bracelet tag remote hand-held device by setting off the alarms at each exit door. I test the [wander management] alarm bracelet to see if the [wander management] alarm bracelet is active and if the battery is low and I check the resident's [wander management] alarm bracelets against the exit doors. On 12/20/2023 the resident's [wander management] alarm bracelet was checked, and it was functioning according to the audit received from the facility.
Interview on 1/31/2024 at 9:41AM; the Assistant Director of Nursing (ADON) stated: I was contacted at 3:30AM on 1/19/2024, by Registered Nurse [Staff B] who stated that [Resident #1] is missing, and the staff have searched all over the building and outside of the facility and they did not find the resident. She then stated that they called the police around 3:20 AM and the police told them that there was a lady that was hit by a train near the facility .I cannot remember hearing the alarm going off when I was on the phone with [Staff B]. I know the nurse was on the south wing when she was speaking to me on the phone [Staff B] attempted to contact other administrative personnel, I was the first person to answer, after speaking with the nurse, I called the NHA and corporate personnel who answered. When I came to the facility around 6:00 AM, there were two police officers at the facility and they wanted to see all the exit doors, I had the maintenance director show the police officers all the exit doors, The Director of Nursing (DON) and myself drove around the facility looking for the resident. The road was blocked off by the railroad tracks close to the facility, we saw the cops there, they told us that an older female was hit by the train, and she did not have any identifiable information on her. I believe the cops said the person passed away and was sent to Medical Examiner's office and they were awaiting confirmation on the identification of the person who was killed. We have not received any information as to who was hit by the train and killed on 1/19/2024.
Interview on 2/1/2024 at 8:07AM Maintenance Director stated: The exit/egress door alarms are monitored weekly by activating the door-pushing up against the door, waiting for the 15 second door opening delay, making sure the alarm sounds once the door is opened, the maglock ensures the 15 second delay before the door opens, once someone tries to open the door. I then open the door, close the door, then reset the alarm, and make sure that the door is locked. The screamers, which are the red boxes located on the inside on the top of the door were installed on 1/19/2024, they are battery operated. A key is needed to turn the screamers off once the door is opened after the 15 second delay. The [wander management] alarm bracelet monitors are all installed close to the exit doors and are checked for proper functioning.
Interview on 2/1/2024 at 1:16 PM the Director of Nursing (DON) stated: As of 1/27/2024 we have two residents on elopement risk, we had an additional resident on elopement risk that went to the hospital on 1/27/2024. The two residents currently on elopement risk have orders for [wander management] alarm bracelets, the residents' names and pictures are in the elopement book, their rooms are located close to the North Wing nurses' station. We have 1 elopement book at each nursing station (North and South), one at the reception desk at the entrance of the building and one in the therapy room. The nursing staff are instructed to check placement every shift and functionality daily. For functionality nurses have to physically take the resident close to an exit door and make sure that the [wander management] alarm bracelet is active, this new order was placed into practice starting 1/19/2024. The two residents that are currently on elopement risk are confused residents, they may have periods of clear cognition, [Resident #2] ambulates with a slow gate sometimes, [Resident #3] is always in her wheelchair. [Resident #1] had a [wander management] in place, the 7:00 AM to 7:00 PM north wing nurse on 1/18/2024 was interviewed and stated the resident had a [wander management] alarm bracelet on during her shift, the 7:00 PM to 7:00 AM nurse (Staff C) stated that the resident did not have a [wander management] alarm bracelet, but she signed at the beginning of the shift that the resident did have a [wander management] alarm bracelet on. In the interview later on 1/19/2024 [Staff C] stated that the resident did not have an [wander management] Alarm bracelet. The DON stated we always had the elopement risk book in the 4 locations mentioned. When I started working here in March 2023 the elopement books were in place already. [Resident #1] was on the elopement risk list in the book. We have a facility educator (ADON) who conducts education and training and in addition a corporate educator, NHA, DON, ADON, and supervisors are the master drill persons in charge during the elopement drills at the facility that is done every shift (3 shifts) starting 1/19/2024.
The scope and severity of F607 was lowered to a (D) for No actual harm with a potential for more than minimal harm that is not immediate jeopardy as of 02/01/2024. The scope and severity were lowered as a result of the facility's corrective actions implemented as of 02/01/2024. These corrective actions were verified by the survey team through observation, record review and interview on 01/30/2024 to 02/01/2024.
The facility's immediate jeopardy removal plan included:
The staff (128 persons) at 100% were in-serviced/trained on 1/19/2024 to1/29/24, regarding: how to respond to call lights promptly, elopement drills, codes, and emergencies responses, how to respond to door alarms, competency for elopement training, how to deal with patients that have behaviors, behavior management for exit seeking resident, abuse, neglect and exploitation training, accidents, and hazards and the QAPI process with the administrative team. The facility conducted a thorough inspection of all eight (8) exit doors and their existing alarm systems to make sure they are in working order in the facility, each exit door has an [wander management] alarm, a screamer alarm (Installed 1/19/2024) and an egress maglock (magnetic lock) alarm with a 15 second opening delay. The alarm systems are audible and can be heard at their loudest in the area where it goes off and is reasonably audible throughout the facility.
Nurses are assigned to check residents with [wander management] alarm bracelets at least once per shift for placement and functionality. The Elopement Risk Book was revised on 01/28/2024, contains-List of Residents, Guidelines for elopement /Unsafe Wandering Prevention, Facility Floor Plan, Pictures of Residents for elopement, Face sheets, Elopement Drill Schedule, and Elopement Mock Drills protocol.
A 6-foot fence was installed to the north courtyard to ensure that residents are not able to exit to the neighborhood and busy streets from the facility's courtyard on the north wing.
Maintenance staff or their qualified designees, conduct weekly door audits to ensure all doors are in proper working order, including checking that the alarm is audible at the nursing station and care areas.
An audit of all residents who reside in the facility was conducted to evaluate the risk for leaving the facility without informing staff and/or if they may desire to leave the facility. Additional Audits-Dated 1/19/2024 to 1/27/2024; Elopement Drill Audit, Dated 1/20/2024 to/128/2024; [wander management] alarm bracelet Audit, Dated 1/21/2024 to1/26/2024; Daily Door Audits (all shifts), Dated 1/21/2024 to 1/27/2024; Elopement Drill/Actual Event Evaluation, Dated 1/28/2024; Facility Search Grid.
On 02/01/2024 at 8:18 AM during an observation, inspection and walk through with the facility's Maintenance Director, the eight (8) exit doors in the facility were inspected and opened to make sure the [wander management] alarm bracelet, screamers and door alarms were in working order. When pushed open all 8 exit door alarms went off (alarmed) before and after the 15 second door opening delay, the alarms were loud/audible in the immediate area and could be heard throughout the facility. All 8 exit doors were equipped with screamer alarms, egress maglock door alarms and [wander management] alarm bracelet monitors that were tested and were all in working order. A 6-foot fence was installed around the courtyard in the north wing unit.
These corrective actions were verified by the survey team through observation, record review and interview on 01/30/2024 to 02/01/2024.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to provide adequate supervision and a secured environmen...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to provide adequate supervision and a secured environment for one (Resident #1) out of three sampled residents with exit seeking behaviors. This deficient practice enabled Resident #1 to exit the facility at 1:34 AM on 01/19/2024, undetected. The facility's system failure, lack of adequate supervision and failure in ensuring an adequate and effective alert monitoring system was in place, allowed the resident to elope undetected. The resident has not been located as of 02/01/2024.
The findings included:
Record review of the facility's policy titled Wandering and Elopements revision date March 2019 documented: The facility will identify residents who are at risk of unsafe wandering and strive to prevent harm while maintaining the least restrictive environment for residents.
Policy Interpretation and Implementation
1 If identified as a risk for wandering, elopement, or other safety issues, the resident's care plan will include strategies and interventions to maintain the resident's safety.
2 If an employee observes a resident leaving the premises, he/she should:
a.
Attempt to prevent the resident from leaving in a courteous manner.
b.
Get help from other staff members in the immediate vicinity, if necessary; and
c.
Instruct another staff member to inform the charge nurse or director of nursing services that a resident is attempting to leave or has left the premises.
3 If a resident is missing, initiate the elopement/missing resident emergency procedure:
a.
Determine if the resident is out on an authorized leave or pass.
b.
If the resident was not authorized to leave, initiate a search of the building(s) and premises; and
c.
If the resident is not located, notify the administrator and the director of nursing services, the resident's legal representative, the attending physician, law enforcement officials, and (as necessary) volunteer agencies (i.e. emergency management, rescue squads, etc.)
4 When the resident returns to the facility, the director of nursing services or charge nurse shall:
a.
Examine the resident for injuries.
b.
contacts the attending physician and report findings and conditions of the resident.
c.
notifies the resident's legal representative (sponsor)
d.
notify search teams that the resident has been located.
e.
complete and file an incident report; and
f.
document relevant information in the resident's medical record
Review of the facility's policy titled Accidents and Incidents-Investigating and Reporting revision date July 2017 documented: All accidents or incidents involving residents, employees, visitors, vendors etc., occurring on our premises shall be investigated and reported to the Administrator.
Policy Interpretation and Implementation
1 The Nurse Supervisor/Charge Nurse and/or the department director or supervisor shall promptly initiate and document investigation of the accident or incident.
Review of the facility's policy titled Safety and Supervision of Residents revision date July 2017 states: Our facility strives to make the environment as free from accident hazards as possible. Resident safety and supervision and assistance to prevent accidents are facility-wide priorities.
Review of the medical records for Resident #1 revealed the resident was admitted to the facility on [DATE] and re-admitted on [DATE]. Clinical diagnoses included but not limited to: Alzheimer disease, Dementia, and seizures.
Review of the Physician's Orders Sheet for January 2024 revealed Resident #1 had orders that included but not limited to: 8/24/2022- Apply/maintain [wander management] Alarm bracelet to right wrist. Check for placement and functioning every shift. Report any issues immediately to the supervisor.
Record review of the Electronic Medication Administration Record (EMAR) for 1/1/2024 to 1/18/2024 revealed Resident #1 was checked off on the EMAR that the resident had the [wander management alarm bracelet] on by assigned nurses.
Record review of Resident #1 's Quarterly Minimum Data Set (MDS) dated [DATE] revealed: Section C for Cognitive Pattern documented Brief Interview for Mental Status (BIMS) score of 5 on a 0-15 scale indicating the resident is cognitively impaired. Section E for behaviors documented Resident experiences Delusions (misconceptions or beliefs that are firmly held, contrary to reality). Resident wandered 1 to 3 days. Section GG for Functional abilities documented no impairment of upper and lower extremity, no mobility devices used, supervision for sitting to standing position, chair to bed transfer, toilet transfer, tub/shower transfer, and walking 10 feet. Partial assistance for walking 50 feet and substantial assistance for walking 150 feet. Section P for restraints documented wander elopement alarm used daily.
Review of the Elopement Risk Assessment/Evaluation dated 3/23/2023 and 06/29/2023 documented: Score of 0-9. LOW RISK for elopement. No interventions at this time.
Record review of Resident #1's most recent Psychological consult dated 2/2021 documented: Resident appears calm, cooperative, in no apparent distress at this time.
Record review of Resident #1's Elopement Care Plans Reference Dated 04/12/2021 revealed: Resident has a potential for elopement due to: has cognitive impairment, has periods of increased confusion, is exit seeking, is (I) ambulatory, wanders the unit & wanders near exit doors, has a history of elopement. 01/19/2024 elopement. Interventions Include: Educate resident/responsible party regarding sign out procedures as needed. Perform frequent observations of resident's whereabouts every shift. Provide redirection when observed going towards exit doors. Encourage resident to participate in activities of choice; provide 1:1s as needed. Apply [wander management alarm bracelet] as ordered (R) wrist. Verify placement every shift. Check for proper functioning weekly. Include resident in Elopement Book and Update physician and responsible party if resident elopes.
Review of the Narrative Nurses notes for Resident #1 dated 01/19/2024 timestamped 06:25 documented: Administrator spoke to the family member when she returned the call, Administrator informed the family about patient elopement and give the family the report of actual situation.
1900 During initial rounds, resident was seen walking around the hallway and was redirected to her room. Resident was found walking in the hallway again and said, I want to go home. Medications due were given to the resident and resident was placed in bed. All safety measures were in place.
At 2300 while passing by the laundry area, nurse noticed the resident was getting her hair groomed by a Certified Nursing Assistant (CNA).
At 0000 observed resident being put to bed by her CNA and stayed in the room with her to make sure she stayed in bed.
At 0030 Resident was observed walking out of her room towards the nursing station. Initiated and placed resident in a chair to sit in the nurses' station.
At 1:19 AM observed the resident standing in front of nurses' station counter and redirected to her to her room.
At 1:22 AM observed resident walking in the hallway while doing routine check and redirected back to her room.
At 2:40 AM while making routine rounds, alarm heard, resident was found missing from assigned room. Initiated elopement protocol, code green initiated.
At 3:25 AM police .notified about the resident missing. Assistant Director of Nursing (ADON) was notified, message left for family member, medical doctor was notified.
The National Weather Service Climate Data for the Miami area January 19, 2024, ranged from temperatures of 69 degrees Fahrenheit (F) to 77 degrees F (http://www.weather.gov/).
During an interview on 01/30/2024 at 10:00 AM, the Administrator (NHA), Risk Manager, Quality Assurance (QA), stated: I received a call at approximately 3:00 to 3:30 AM on 1/19/2024, I was out of town, I got report that there was a missing person at the facility, immediately I got in the car and was on my way to facility, When I got to the facility the corporate response team were already there. I called the police, [State Agency] and made the report on my way to the facility. [State Agency] accepted the case, I submitted the immediate report to AHCA (Agency for Healthcare Administration), when I arrived at the facility the corporate team and other administration personnel were at the facility investigating the elopement. The investigation was ongoing with the corporate team. I participated in QA with the department heads. I reached out to the resident's family members, the resident's niece let us know that she missed out on the calls from the facility earlier, the resident's niece stated the resident's responsible party on file was currently in a nursing home and is hard to reach. I was placed on leave/suspension on 1/19/2024 by the corporate team while the investigation continued. I was reinstated on Friday afternoon 1/26/2024. The AHCA five (5) day report indicated the elopement was attributed to the lack of supervision by the two (2) nurses- one (1) Registered Nurse (RN), one (1) Licensed Practical Nurse (LPN) and one (1) Certified Nursing Assistant (CNA), they were all places on suspension on 1/19/2024. The resident is still missing at this time, we immediately got to work on the response plan. The findings were as stated in the AHCA 5-day report, it was substantiated. The [wander management] alarm bracelet red light never came on but the door with the egress alarm did go off.
Interview on 1/30/2024 at 10:15 AM, the Regional Clinical Director (RCD) stated: Based on the footage from the camera, it appears that the resident did not have an [wander management] alarm bracelet on, the red light did not go off as it should when a resident with a [wander management alarm bracelet] gets near the exit door. The egress door alarm did go off. Clinical and non-clinical staff and agency staff were educated on elopement, and abuse and neglect and this would include ongoing education with new hires. The nurses and CNA involved in the resident's elopement were terminated and reported to the board of nursing.
Interview on 1/30/24 at 10:36 AM LPN, Staff A via telephone stated: I was working on the 11:00 to 7:00 AM shift on 1/19/2024, all I remember is that I was sitting at the desk doing skin assessments checks, the resident was sitting with me, she got up and walked to the side. At 1900 I clocked in and made rounds, the 30 residents were accounted for, awake and alert. I accepted Medication Cart #2 keys, counted narcotics, and started with med pass, around 11:30 PM, I stopped to eat, at 12:00 AM I started charting sitting at the desk, at this time the resident was at nursing station with me. The resident got up and walked around the south side of the nurses station, between 1:45 AM the call light went off in room [ROOM NUMBER] bed C, I went to assess the resident, when I returned to the nurses' station I saw the light at the back door blinking, I realized that someone had opened or touched the door, I went to the door. I never heard an alarm go off, I just saw the red-light blinking, I went to check the resident's room, the resident was not in the room, I alerted everyone, and a code green was called, I went to the resident's room because she was the only resident that was up at that time by the nurses' station. I took my truck and went around the facility looking for the resident. Sometimes the resident would be up at night at the nurse's station, I do not recall if the resident had on a [ wander management] alarm bracelet. I then ran into the police officer and brought the officer back to the facility to take a profile of the resident we were looking for. I was not the nurse assigned to the resident. I was suspended from the facility on 1/19/2024 and I ended up resigning on 1/23/2024.
Interview on 1/30/2024 at 11:03 AM, Registered Nurse (RN) (Staff B) via telephone stated: On 1/19/2024, the staff realized that the resident was missing, we started a search, I called the Assistant Director of Nursing (ADON) to let administration know what was going on. I was the RN in the building that night, I was assigned to the South Wing. [Staff C, LPN] was assigned to the resident.
Interview on 1/30/2024 at 11:07 AM Licensed Practical Nurse (LPN) (Staff C) via telephone stated: I am busy at the moment, call back in 5 hours. Another surveyor on the team called Staff C back at the designated time and did not receive any response.
Interview on 1/30/2024 at 11:09 AM Staff D, via telephone stated: I started to work at 11:00 PM on 1/18/2024, I did my rounds, I did not see the resident in her room, I called [Staff C] and told her, the resident was not in her room, the nurse said the resident was at the nurses' station. I went to get linen to start doing my job, I saw the resident in the hallway, I took her by the hand and led her into her room and had her sit on the bed. Everyday this resident walks around. The nurses [Staff A and Staff C] were at the nursing station. Around 2:30 AM I made my rounds, I did not see the resident in her room, I called the nurse and told her I could not find the resident, I checked all the rooms and the shower rooms, I checked outside and did not find the resident. Staff D then ended the interview and hung up the phone.
Interview on 1/30/2024 at 11:40 AM, the Regional Director of Operations (RDO) showed surveyors a video dated 01/19/2024 time stamped from 1:31 AM to 1:34 AM via the computer, depicting the resident walking back and forth in the hallway for approximately 3 to 4 minutes in duration on the north wing/unit and eventually exiting through the door leading to the unfenced/open courtyard. The video also shows a nurse sitting at the nurse's station on the north wing/unit. RDO stated according to our investigation and interviews with the nurses, the resident was not wearing an [wander management] alarm bracelet.
Interview on 1/31/2024 at 7:36 AM the NHA stated: According to the footage the resident left the facility around 1:33 AM, based on the staff account the search for the resident started at 2:30 AM.
Interview on 1/31/2024 at 7:39 AM the Regional Clinical Director (RCD) stated: I interviewed all the staff before the shift was over, I interviewed [Staff A], she stated she was in the resident's room, I was busy doing resident care, no mention of what resident she was taking care of, we let the nurses know (Staff A and Staff C) we reviewed the camera footage and showed [Staff A] the camera footage. [Staff A] acknowledged she was sitting at the desk, stated she did hear an alarm, I thought it was a call light or a resident who I know that really does not need anything. We asked her if she heard the alarm, [Staff A] replied, yes I heard the alarm. The video showed that [Staff A] did not get up from the nurse's station when the alarm went off. The RCD stated in the immediate report the information about Staff A responding to the South Egress note is a typo by the NHA, he was driving from [NAME] in his car and doing the report at the time .When I interview the day shift nurse stated the [wander management alarm bracelet] was off. [Staff A] stated she heard the alarm go off, thought it was a call light. Staff in the facility responded to the alarm at 2:30 AM. According to the orders the maintenance Director checks the [wander management alarm] monthly, the last audit for the resident's [wander management alarm] was completed on 12/20/2023. According to the video the alarm started going off at 1:33 AM but staff responded at 2:30 AM. Three staff members got into their cars and went in opposite directions searching for the resident for approximately 30 minutes. The alarm was turned off by the Maintenance Director at approximately 4:00 AM on 1/19/2024. None on the staff on the morning of 1/19/2024 had a code to turn off the alarm. The resident was being closely monitored at the nurse's station from the night of 1/18/23 into the morning of 1/19/2023. The resident's room is right next to the nursing station, and she was monitored frequently.
Interview on 1/31/2023 at 7:57 AM, the Maintenance Director stated: I was checking the [wander management alarm] weekly before the incident and currently they are checked daily every shift. I check the alarm using the [wander management alarm bracelet] .by setting off the alarms at each exit door. I test the [wander management alarm] to see if the [ wander management alarm bracelet]is active and if the battery is low and I check the resident's [wander management] Alarm bracelets against the exit doors. On 12/20/23 the resident's [wander management] alarm bracelet, and it was functioning according to the audit received from the facility.
Interview on 1/31/2024 at 9:41 AM, the Assistant Director of Nursing (ADON) stated: I was contacted at 3:30 AM on 1/19/2024, by Registered Nurse (Staff B) who stated that [Resident #1] is missing, and the staff have searched all over the building and outside of the facility and they did not find the resident. She then stated that they called the police around 3:20 AM and the police told them that there was a lady that was hit by a train near the facility. I cannot remember hearing the alarm going off when I was on the phone with Staff B. I know the nurse was on the south wing when she was speaking to me on the phone. Staff B attempted to contact other administrative personnel, I was the first person to answer, after speaking with the nurse, I called the NHA and corporate personnel who answered. When I came to the facility around 6:00 AM, there were two police officers at the facility and they wanted to see all the exit doors, I had the maintenance director show the police officers all the exit doors. The Director of Nursing (DON) and myself drove around the facility looking for the resident. The road was blocked off by the railroad tracks close to the facility, we saw the cops there, they told us that an older female was hit by the train, and she did not have any identifiable information on her. I believe the cops said the person passed away and was sent to Medical Examiner's office and they were awaiting confirmation on the identification of the person who was killed. We have not received any information as to who was hit by the train and killed on 1/19/2024.
Interview on 2/1/2024 at 8:07 AM, the Maintenance Director stated: The exit/egress door alarms are monitored weekly by activating the door-pushing up against the door, waiting for the 15 second door opening delay, making sure the alarm sounds once the door is opened, the maglock ensures the 15 second delay before the door opens, once someone tries to open the door. I then open the door, close the door, then reset the alarm, and make sure that the door is locked. The screamers, which are the red boxes located on the inside on the top of the door were installed on 1/19/2024, they are battery operated. A key is needed to turn the screamers off once the door is opened after the 15 second delay. The [wander management alarm] monitors are all installed close to the exit doors and are checked for proper functioning.
During an interview on 2/1/2024, at 1:16 PM the Director of Nursing (DON) stated: As of 1/27/2024 we have two residents on elopement risk, we had an additional resident on elopement risk that went to the hospital on 1/27/2024. The two residents currently on elopement risk have orders for [wander management bracelets], the residents' names and pictures are in the elopement book, their rooms are located close to the North Wing nurses' station. We have 1 elopement book at each nursing station (North and South), one at the reception desk at the entrance of the building and one in the therapy room. The nursing staff are instructed to check placement every shift and functionality daily. For functionality nurses have to physically take the resident close to an exit door and make sure that the [wander management bracelet] is active, this new order was placed into practice starting 1/19/2024. The two residents that are currently on elopement risk are confused residents, they may have periods of clear cognition, [Resident #2] ambulates with a slow gate sometimes, [Resident #3] is always in her wheelchair. [Resident #1] had [wander management bracelet] in place, the 7:00 AM to 7:00 PM north wing nurse on 1/18/2024 were interviewed and stated the resident had a [wander management bracelet] on during her shift, the 7:00 PM to 7:00 AM nurse [Staff C] stated that the resident did not have a [wander management alarm bracelet], but she signed at the beginning of the shift that the resident did have a [wander management bracelet] on. In the interview later on 1/19/2024 [Staff C] stated that the resident did not have a [wander management bracelet]. We always had the elopement risk book in the 4 locations mentioned. When I started working here in March 2023 the elopement books were in place already. [Resident #1] was on the elopement risk list in the book. We have a facility educator [ADON] who conducts education and training and in addition a corporate educator. NHA, DON, ADON, and supervisors are the master drill persons in charge during the elopement drills at the facility that is done every shift (3 shifts) starting 1/19/2024.
The scope and severity of F689 was lowered to a (D) for No actual harm with a potential for more than minimal harm that is not immediate jeopardy as of 02/01/2024. The scope and severity were lowered as a result of the facility's corrective actions implemented as of 02/01/2024. These corrective actions were verified by the survey team through observation, record review and interview on 01/30/2024 to 02/01/2024.
The facility's immediate jeopardy removal plan included:
The staff (128 persons) at 100% were in-serviced/trained from 1/19/2024 to 1/29/2024, regarding: how to respond to call lights promptly, elopement drills, codes, and emergencies responses, how to respond to door alarms, competency for elopement training, how to deal with patients that have behaviors, behavior management for exit seeking resident, abuse, neglect and exploitation training, accidents, and hazards and the QAPI process with the administrative team. The facility conducted a thorough inspection of all eight (8) exit doors and their existing alarm systems to make sure they are in working order in the facility, each exit door has a [ wander management alarm], a screamer alarm installed 1/19/2024 and an egress maglock (magnetic lock) alarm with a 15 second opening delay. The alarm systems are audible and can be heard at their loudest in the area where it goes off and is reasonably audible throughout the facility.
Nurses are assigned to check residents with [wander management alarm bracelets] at least once per shift for placement and functionality. The Elopement Risk Book was revised on 01/28/2024, contains-List of Residents, Guidelines for elopement /Unsafe Wandering Prevention, Facility Floor Plan, Pictures of Residents for elopement, Face sheets, Elopement Drill Schedule, and Elopement Mock Drills protocol.
A 6-foot fence was installed to the north courtyard to ensure that residents are not able to exit to the neighborhood and busy streets from the facility's courtyard on the north wing. Maintenance staff or their qualified designees will conduct weekly door audits to ensure all doors are in proper working order, including checking that the alarm is audible at the nursing station and care areas.
An audit of all residents who reside in the facility was conducted to evaluate residents at risk for leaving the facility without informing staff and/or if they may desire to leave the facility. Additional Audits-Dated 1/19-27/2024; Elopement Drill Audit, Dated 1/20-28/2024; [wander management alarm] Audit, Dated 1/21-26/2024; Daily Door Audits (All shifts), Dated 1/212024 to 1/27/2024; Elopement Drill/Actual Event Evaluation, Dated 1/28/2024; Facility Search Grid.
On 02/01/2024 at 8:18 AM during an observation, inspection and walk through with the facility's Maintenance Director, the eight (8) exit doors in the facility were inspected and opened to make sure the [wander management alarm], screamers and door alarms were in working order. When pushed open all 8 exit door alarms went off (alarmed) before and after the 15 second door opening delay, the alarms were loud/audible in the immediate area and could be heard throughout the facility. All 8 exit doors were equipped with screamer alarms, egress maglock door alarms and [wander management] alarm bracelet monitors that were tested and were all in working order. A 6-foot fence was observed to have been installed around the courtyard in the north wing unit.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews,observations and interviews the facility's administration failed to implement, provide, and ensure effec...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews,observations and interviews the facility's administration failed to implement, provide, and ensure effective and efficient preventative measures were in place to prevent the neglect and elopement of one resident (Resident #1) out of three sampled residents who displayed exit seeking behaviors. As evidenced by inadequate safety measures that included failure to ensure exit door alarm was audible in all areas of the facility in the event of an emergency and failure by staff to implement assigned level of supervision for resident #1 who had exit seeking behaviors, wandered the unit and wandered near exit doors and had the potential for elopement. These deficient practices enabled resident #1 to exit the facility undetected at 1:34 AM through a north egress (emergency exit) back door in the back of the facility on foot on 1/19/2024 placing the resident at risk for harm and or injury.
The findings included:
Record review of the facility's policy titled, Abuse, Neglect, Exploitation and Misappropriation Prevention Program Policy and Procedure revision date was on 04/2021, the policy documented: The facility will provide a safe resident environment and protect all residents from abuse. Therefore, each resident has the right to be free from abuse, neglect, misappropriation of resident property and exploitation of any type by anyone. Neglect means failure of the facility, its employees or service providers to provide goods and services to a resident that are necessary to avoid physical harm, pain, mental anguish, or emotional distress. A prompt thorough investigation will be conducted by the facility immediately.
Review of the facility's policy titled, Wandering and Elopements Policy and Procedure revised March 2019 documented: Policy Heading: The facility will identify residents who are at risk of unsafe wandering and strive to prevent harm while maintaining the least restrictive environment for residents. Policy Interpretation and Implementation: 1) If identified as at risk for wandering, elopement, or other safety issues, the resident's care plan will include strategies and interventions to maintain the resident's safety and 3) If a resident is missing, initiate the elopement/missing resident emergency procedure.
Review of the Job Description for the Nursing Home Administrator documented: The Administrator is responsible for developing, managing, and supervising the overall functions of the facility in accordance with current Federal, state, and local standards and established nursing policies and procedures. He/she is also responsible for providing a positive, caring, and homelike environment for the residents.
Review of the Job Description for the Director of Nursing documented: The Director of Nursing is responsible for planning, organizing, developing, and directing the day-to-day functions of the nursing department in accordance with current Federal, state, and local standards and established nursing policies and procedures. He/she is also responsible for providing a positive, caring, and homelike environment for the residents.
Review of the Job Description for the Assistant Director of Nursing documented: The Assistant Director of Nursing is responsible for supervising the day-to-day nursing activities in accordance with current Federal, state, and local standards and established nursing policies and procedures. In the absence of the Director of Nursing Services, he/she is charged with carrying out the resident care policies. He/she is also responsible for providing a positive, caring, and homelike environment for the residents.
Review of the Job Description for the Registered Nurse documented: The primary purpose of your job description is to provide direct nursing care the residents and to supervise the day-to-day nursing activities performed by nursing assistants. Such supervision must be in accordance with current federal, state, and local standards, guidelines and regulations that govern our facility and as may be required by the Director of Nursing services to ensure that the highest degree of quality care is maintained at all times. He/she is also responsible for providing a positive, caring, and homelike environment for the residents.
Review of the Job Description for the Licensed Practical Nurse documented: The Licensed Practical Nurse is responsible for providing professional care in accordance with established nursing policies and procedures. He/she is also responsible for providing a positive, caring, and homelike environment for the residents.
Review of the Job Description for the Certified Nursing Assistant documented: The Certified Nursing Assistant is responsible for providing professional care in accordance with established certified nursing assistant policies and procedures. He/she is also responsible for providing a positive, caring, and homelike environment for the residents.
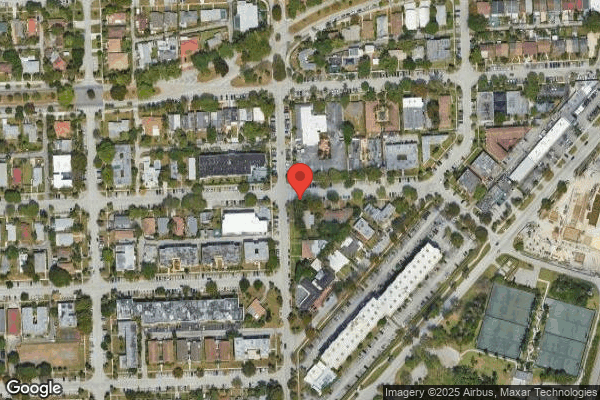
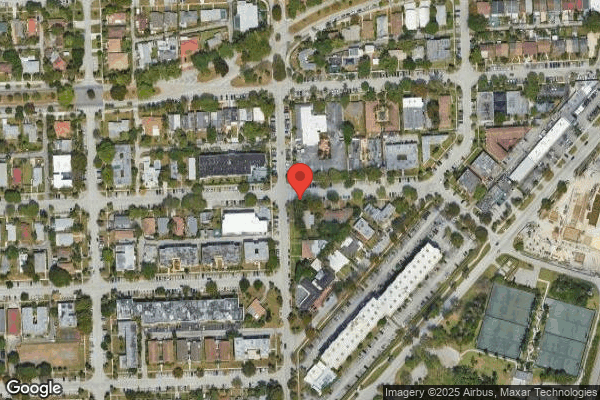
Based on observational tour of the facility's parameter increased risk factors included the fact that, the Facility is in an area that is congested with heavy traffic, with 40 miles per hour 2 lane traffic each way.
Review of Resident's #1 Elopement care plan dated 4/21/2021 documented the resident has a potential for elopement risk related to cognitive impairment, who was exit seeking, wandered the unit and wandered near exit doors; Goal: Resident will safe and will refrain from leaving facility unsupervised thru the next review date; Interventions: Perform frequent observations of residents whereabouts every shift; Provide redirection when observed going towards exit door; Apply alarm bracelet as ordered on right wrist; Verify placement every shift and Check for proper functioning weekly.
Review of the progress notes documented the following: Dated 1/19/2024 time stamped 06:25-Narrative Nurses Note: 1900 during initial round, resident was seen walking around the hallway and was redirected to her room. 2130 resident was found walking in the hallway again and said, I want to go home. Due meds given and was putting back to her bed. All safety measures were in place. 2300 while passing by the laundry area, noticed the resident was getting her hair groomed by a CNA. 0000 observed resident putting to bed by her CNA and stayed in the room with her to make sure she stays in bed. 0030 resident was observed walking out of her room towards the nursing station. Initiated and placed resident in a chair to sit in the nurse's station. 1:19 AM observed resident standing in front of nurses station counter and was redirected to her room. 1:22 AM observed resident walking in hallway while doing routine check and redirected back to her room. 2:40 AM while making routine round alarm heard, resident was found missing from assigned room. Initiated elopement protocol, code green initiated. 3:25 AM police were notified about resident's missing. ADON (Assistant Director of Nursing) was notified. Message left for family member. Medical doctor was notified. The progress notes were written by Staff C, Licensed Practical Nurse (LPN). Dated 1/19/24 time stamped 10:30-Narrative Nurses Note: Administrator spoke to the family when she returned the call. Administrator informed the family about patient elopement and gave the family the report of the actual situation.
Review of the Physician's Order Sheets (POS) and Medication Administration Records (MAR) for December 2023 and January 2024 documented the resident's medications and an or to apply [wander management alarm bracelet] to right wrist, check for placement each shift and functioning Q (every) week. Report any issues immediately to supervisor. The order start date was 8/24/2022. The [wander management alarm bracelet] was checked every day for the month of December 2023 and January 2024 and indicated the resident was wearing it.
Review of the Elopement Risk Assessment/Evaluation dated 3/23/2023 and 6/29/23 documented: The resident is at low risk for elopement, does not wander and has never eloped.
On 1/30/24 at 9:54 AM, the Administrator/Risk Manager/QAA (Quality Assessment and Assurance) stated: I received a call at approximately 3:30 AM and received a report of a missing person and they didn't retrieve the person. I immediately got in my car and was on my way to the facility for coming to assist with the search. I called [ local state agency] and they accepted the case. The [local law enforcement] was in contact with the facility. On 1/19/2024, the incident occurred. I submitted the one-day report to the [local state agency] with the information given. When I arrived, to the facility the corporate team and other administration personnel were at the facility investigating the elopement. The investigation was ongoing with the corporate team. I participated in QA (quality assurance) with the department heads. I reached out to the resident's family member. I let her know her great aunt was missing, and we are actively looking for her and would provide updates. The resident's niece let us know that she missed out on the calls from the facility earlier. The resident's niece stated the resident's responsible party on file was currently in a nursing home and is hard to reach. The resident remains missing at this time. The [local state agency] five (5) day report indicated the elopement was attributed to the lack of supervision by the two (2) nurses- one (1) Registered Nurse (RN), one (1) Licensed Practical Nurse (LPN) and one (1) Certified Nursing Assistant (CNA), they were all placed on suspension on 1/19/2024. We immediately got to work on the response plan. The findings were as stated in the [local state agency] 5-day report, the allegation of neglect was substantiated. The [wander management alarm], red light never came on but the door with the egress alarm did go off.
On 1/30/2024 at 10:06 AM, the Registered Nurse (RN), Regional Clinical Director stated, Based on the footage from the camera, it appears that the resident did not have a [wander management alarm] bracelet on, the red light did not go off as it should when a resident with a [wander management alarm] gets near the exit door. She did not have a [wander management alarm] bracelet. The egress door alarm did go off. We educated the licensed nurses to review the elopement assessment. Clinical and non-clinical staff and agency staff were educated on elopement and abuse and neglect, and this would include ongoing education with new hires. The nurses and CNA involved in the resident's elopement were terminated and reported to the board of nursing.
On 1/30/2024 at 10:36 AM, Staff A, Licensed Practical Nurse (LPN) via telephone stated: I was working on the 11-7 AM shift on 1/19/2024, I was sitting at the desk and doing daily assessments and the resident was sitting with me, she got up and walked to the side. At 1900 I prepared to make rounds, upon making rounds all 30 residents were accounted for awake and alert. I accepted Medication Cart #2 keys, counted narcotics, and started with med pass. Around 11:30 PM, I stopped to eat. At around 12:00 AM, I started charting sitting at the desk. At that time the resident was at the nursing station with me. The resident got up and walked around the South side of the nursing station. Between 1:45 AM, the call light went off in room [ROOM NUMBER], bed C, I went to assess the resident. When I returned to the nurse's station I saw the light at the back door blinking. I realized that someone had opened or touched the door. I went to the door to check it. I never heard an alarm on the door go off. I just saw the red-light blinking. I was facing the door and went to check the resident's (Resident #1) room and she was not in the room. I went to the resident's room because she was the only resident that was up at that time by the nurses' station. I was not the nurse assigned to the resident. I alerted everyone and a code green was called, and we started the search. I took my truck and drove around the facility looking for the resident. Sometimes the resident would be up at night at the nurse's station. This was common for her to be up at night. I don't recall her having on an [wander management alarm] bracelet. I then ran into the [law enforcement officer] and brought the [law enforcement officer back] to the facility to take a profile of the resident we were looking for. I was suspended from the facility on 1/19/2024. They didn't tell me how long I would be suspended and then I resigned on 1/23/2024.
On 1/30/2024 at 10:59 AM, Staff B, RN (Registered Nurse) via telephone stated: The staff realized that the resident was missing, and we started a search. I called the ADON (Assistant Director of Nursing) to let administration know what was going on. I was the RN in the building that night. I was assigned to the South wing [ Staff C, LPN] was assigned to the resident.
On 1/30/2024 at 11:04 AM, Staff C, LPN via telephone stated: I am busy at the moment and doing something. Call me back in five hours. Attempted a second contact at the designated time and did not receive any response.
On 1/30/2024 at 11:08 AM, Staff D, Certified Nursing Assistant (CNA) via telephone stated: After 11:00 PM, I signed into work. I made rounds and I didn't see the patient in the room. I told the nurse [Staff C, LPN] and she said the patient is here with me. The resident liked to walk around. I go to the laundry room and pick up my cart. The patient was in the hallway. I talked to her and told her to come with me. I took her to her room and had her sit on the bed. Every day she walked around. [Staff A, LPN] and [Staff C, LPN] were at the nursing station. I noticed the patient was missing at 2:30 AM. I made rounds; I didn't see the patient in her room. I called the nurse and told her I could not find the resident. I opened the bathroom door, and I didn't see her. I went outside and I didn't see her.
On 1/30/2024 at 11:35 AM observation of the video of the resident exiting the building and interview with the Regional Director of Operations stated: The resident walked out of the door and the alarm for the door went off and the nurse [Staff A, LPN] was sitting at the North wing nurses station and did not get up. The resident was wearing an alarm bracelet and the alarm on the [wander management alarm] did not sound off. According to our investigation and interviews with the nurses, the resident was not wearing a [wander management alarm] bracelet. I have been checking the ME's (Medical Examiner's) office every day since the resident left. She has not been found yet.
During observational review of the facility's video footage via the computer approximately 3-4 minutes in duration with the Regional Director of Operations on 1/30/2024 at 11:35 AM. The video footage revealed that on 1/19/2024 at 1:33 AM, Resident #1 was dressed in a black dress with pink socks and a white blanket wrapped around her shoulders was pacing back and forth in the North wing hallway, during this time Staff A, LPN was sitting at the North wing nurses station with her head down. On 1/19/2024 at 1:34 AM Resident #1 pushed the door without any difficulty at 1:34 AM on 1/19/2024 and exited the facility undetected by staff. The resident walked out of the facility with no assistive device and proceeded through the north egress (emergency exit) double door that lead to the facility's courtyard on the north wing. The alarm on the exit door was not audible for staff to hear throughout the facility within the care areas beyond the double doors.
On 1/31/2024 at 7:35 AM, the Administrator stated: Around 1:33 AM the resident left out of the door of the facility. The search was started about an hour later at 2:30 AM. The Elopement book is kept at the front desk, at each nursing station and in the therapy room. The Elopement book contains the resident's picture, search grids, what to do in case of an elopement and a check list.
On 1/31/2024 at 7:38 AM, RN, Regional Clinical Director stated: We interviewed everyone on the shift. At first, she was helpful [Staff A, LPN] She said she was in the resident's room. I was busy doing resident care . and no mention of what resident she was taking care of. We let the nurses know [Staff A, LPN and Staff C, LPN] we had reviewed the camera footage and showed Staff A] the camera footage. [Staff A] acknowledged, she was sitting at the North nurses' station. She stated she did hear an alarm .thought it was a call light or a resident who .really does not need anything. We asked her if she heard the alarm, [Staff A, LPN] replied, yes I heard the alarm. The video showed that [Staff A] did not get up from the nurse's station when the alarm went off. The alarm is audible for up to 110 ft. It was a typo in the report done by the Administrator. It should be the North egress door, not the South egress door. Her [wander management alarm] bracelet was checked on 12/20/2023. She did have a [wander management alarm] bracelet. The maintenance person checks the [wander management alarm] monthly and nursing checks every shift. The resident was not placed on one to one because the resident was being closely monitored at the nurses' station that night, her room is next to the nurses' station, and she is checked on frequently. [Staff A, LPN] stated she heard the alarm go off, thought it was a call light. Staff in the facility responded to the alarm at 2:30 AM. According to the orders, the Maintenance Director checks the [wander management alarm] monthly, the last audit for the resident's [wander management alarm] was completed on 12/20/2023. According to the video the alarm started going off at 1:33 AM, staff responded at 2:30 AM. Three staff members got into their cars and went in opposite directions searching for the resident for approximately 30 minutes. The alarm was turned off by the Maintenance Director at approximately 4:00 AM on 1/19/2024. No one on staff on the morning of 1/19/2024 had a code to turn off the alarm. The resident was being closely monitored at the nurse's station from the night of 1/18/2024 into the morning of 1/19/2024. The resident's room is right next to the nursing station, and she was monitored frequently.
On 1/31/2024 at 7:57 AM, the Maintenance Director stated, I checked the [wander management alarm] weekly before the incident and now it is checked every day. I have a [wander management alarm] bracelet and I set off the alarm on each door. For the residents, I have a device if the [wander management alarm] bracelet is active or if the battery is low. For the resident, she was last checked on 12/20/2023 and it was functioning. For the alarm bracelets tag, it is placed on the resident, I take it to the door to make sure it is activated. The area outside the North egress door is an outside parking area/street. Since the incident, there is a 6 feet fence enclosing the area.
On 1/31/2024 at 9:41 AM, Assistant Director of Nursing (ADON) stated: It was 3:30 in the morning, Thursday going into Friday in the morning, my phone rings. [Staff B, RN] said I have some bad news. She started to tell me [ Resident #1] was missing. They searched all over the building, staff went looking for her outside of the building and they have not found her. She then went on to say, they called the [local law enforcement] at 3:20 AM or 3:25 AM, the police told them there was a lady hit by a train, near here. I don't remember if the alarm was ringing while we were on the phone. [Staff B, RN] was on the South wing when she called me. She tried to contact the Administrator and was not able to. I tried to contact the Administrator, but he didn't answer. I tried to contact the DON (Director of Nursing) and she didn't answer. I contacted [RN, Regional Clinical Director] about the incident. When I got here to the facility after 6:00 AM, two [local law enforcement officers] were here and they wanted to see all of the exit doors. The Maintenance Director showed them all of the exit doors. The DON and myself drove around the facility to look for the resident. The road was blocked by [local law enforcement officers] and they told us that a lady was hit by a train, and she didn't have any ID (identification) on her. They said the person passed away and was sent to the Medical Examiner's office and they were waiting for confirmation for identification of the person. We still have not received confirmation as to who that was.
On 2/01/2024 at 8:07 AM, the Maintenance Director stated: The exit/egress door alarms are monitored weekly by activating the door-pushing up against the door, waiting for the 15 second door opening delay, making sure the alarm sounds once the door is opened, the maglock ensures the 15 second delay before the door opens, once someone tries to open the door. I then open the door, close the door, then reset the alarm, and make sure that the door is locked. The screamers, which are the red boxes located on the inside on the top of the door were installed on 1/19/2024, they are battery operated. A key is needed to turn the screamers off once the door is opened after the 15 second delay. The wander guard monitors are all installed close to the exit doors and are checked for proper functioning. All exit doors are checked weekly, even before the incident.
The scope and severity of F835 was lowered to a (D) for No actual harm with a potential for more than minimal harm that is not immediate jeopardy as of 2/01/2024. The scope and severity were lowered as a result of the facility's corrective actions implemented as of 2/01/2024. These corrective actions were verified by the survey team through observation, record review and interview on 1/30/2024 to 2/01/2024.
The facility's immediate jeopardy removal plan included:
The staff (128 persons) at 100% were in-serviced/trained on 1/19/2024 to 1/29/2024, regarding: how to respond to call lights promptly, elopement drills, codes, and emergencies responses, how to respond to door alarms, competency for elopement training, how to deal with patients that have behaviors, behavior management for exit seeking resident, abuse, neglect and exploitation training, accidents, and hazards and the QAPI (Quality Assurance Performance Improvement) process with the administrative team. The facility conducted a thorough inspection of all eight (8) exit doors and their existing alarm systems to make sure they are in working order in the facility, each exit door has a [wander management alarm], a screamer alarm (Installed 1/19/2024) and an egress maglock alarm with a 15 second opening delay. The alarm systems are audible and can be heard at their loudest in the area where it goes off and is reasonably audible throughout the facility.
Nurses are assigned to check residents with wander guards at least once per shift for placement and functionality. The Elopement Risk Book was revised on 01/28/2024, contains-List of Residents, guidelines for elopement /Unsafe Wandering Prevention, Facility Floor Plan, Pictures of Residents for elopement, Face sheets, Elopement Drill Schedule, and Elopement Mock Drills protocol.
A 6-foot fence was installed to the north courtyard to ensure that residents are not able to exit to the neighborhood and busy streets from the facility's courtyard on the north wing.
Maintenance staff or their qualified designees, conduct weekly door audits to ensure all doors are in proper working order, including checking that the alarm is audible at the nursing station and care areas.
An audit of all residents who reside in the facility was conducted to evaluate at risk for leaving the facility without informing staff and/or if they may desire to leave the facility. Additional Audits-Dated 1/19/2024 to 1/27/2024; Elopement Drill Audit, Dated 1/20/2024 to 1/28/2024; [wander management alarm bracelet] Audit, Dated 1/21/2024 to 1/26/2024; Daily Door Audits (All shifts), Dated 1/21/2024 to 1/27/2024; Elopement Drill/Actual Event Evaluation, Dated 1/28/2024; Facility Search Grid.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
QAPI Program
(Tag F0867)
Someone could have died · This affected 1 resident
Based on interview and record review, the facility's quality assurance and assessment committee failed to identify quality concerns to implement effective plans of action related to adequate supervisi...
Read full inspector narrative →
Based on interview and record review, the facility's quality assurance and assessment committee failed to identify quality concerns to implement effective plans of action related to adequate supervision resulting in repeated deficient practice. The facility's history includes deficient practice for failing to supervise residents resulting in elopement within the past 10 months. The previous incident resulted in the identification of immediate jeopardy that occurred when another resident eloped from the facility undetected on 3/19/2023 and was found deceased . The facility had surveys with IJ levels citations in the previous three years during surveys. The facility was cited for Free of Accident Hazards, Supervision, Devices, Administration and Quality Assurance and Assessment. On 1/19/2024, the facility was negligent and failed to provide adequate supervision and effective services to prevent the elopement of one (Resident #1) out of three sampled residents with exit seeking behaviors, resulting in Resident #1 eloping from the facility at 1:34 AM, through an egress (emergency exit) back door in the back of the facility on foot undetected. These repeated deficient practices have the potential to affect any of the residents residing in the facility.
Refer to F 600, F 607, F 689 and F835.
The findings included:
Record review of the facility's Quality Assurance Performance Improvement (QAPI) Program Policy and Procedure (revised February 2020) documented the following: Policy-This facility shall develop, implement and maintain an ongoing, facility-wide, data-driven QAPI Program that is focused on indicators of the outcomes of care and quality of life for our residents; QAPI purpose is a type of quality management program which takes a systematic, interdisciplinary, comprehensive and data-driven approach to maintaining and improving safety and quality. Policy Explanation and Compliance Guidelines: 1) The QAPI program includes the establishment of a Quality Assessment and Assurance (QAA) Committee and a written QAPI Plan; 2) The QAA Committee shall be interdisciplinary and shall: b) Meet at least quarterly and as needed to coordinate and evaluate activities under the QAPI program; 3) b) Policies and procedures for feedback, data collection systems and monitoring, c) Process addressing how the committee will conduct activities necessary to identify and correct quality deficiencies. Key components of this process include, but are not limited to, the following: i.) Tracking and measuring performance, iii.) Identifying and prioritizing quality deficiencies, iv.) Systematically analyzing underlying causes of systemic quality deficiencies and v.) Developing and implementing corrective action or performance improvement activities.
Review of the Quality Assurance and Performance Improvement (QAPI) Committee Meeting Sign-in Sheets dated 11/30/2023, 12/20/2023 and 1/11/2024 documented the facility had a QAA Committee meeting monthly. Attendees included: Administrator/Risk Manager, Medical Director, Director of Nursing (DON), Infection Control and Prevention Officer, Admissions Coordinator, Rehab Director, Social Services Director, Dietitian, Business Office Manager, Activities Director, Food Service Director, MDS (Minimum Data Set) Coordinator, Maintenance Director, Housekeeping Director, Human Resources Manager and Licensed Nurses.
On 2/01/2024 at 3:33 PM, the Administrator/Risk Manager/QAA stated, The QAA Committee meets every month on the second Thursday of the month. The committee consist of the Medical Director, Administrator, DON, and all interdisciplinary team members. The purpose of QAA is to use evidence-based data, reports and feedback to identify trends and capitalize on systems that are working and if any negative trends to put measures in place to remedy those.
The facility's removal plan also indicates:
The Administrator and the department heads were educated on the QAPI/QAA Processes with emphasis on identifying quality concerns to implement effective plans of action related to adequate supervision resulting in repeated deficient practice to include failure to supervise residents in previous incidents resulting in an immediate jeopardy.
The facility held an Adhoc QAPI on 1/19/24 regarding the following below to check for compliance:
March 20, 2023, last IJ deficiencies
Last Annual survey cited deficiencies.
On 1/31/24, as part of the continuation of the Adhoc QAPI initiated on 1/19/24, the administrator conducted a meeting with the interdisciplinary team on the following Immediate jeopardy deficient practice received from the Agency for Health Care Administration (AHCA) office on the following areas as stated above, (F600, F607, F689, F835, F867).
- Included in the discussion is the plan of correction initiated and some completed prior to this meeting.
The following education and/or corrective actions were completed on 1/26/24 as follows:
F 600 Abuse and Neglect, F 607, F 689, F 835,F 867
Education Plan:
The staff, newly hired staff, and agency staff will be educated on the following below:
F 600 Abuse/Neglect, F 607, F 689 with emphasis on Resident with an exit seeking behavior,
F 835 administration ,867 QAPI/QAA Process
Elopement drill with emphasis on prompt and timely response to door alarms
Behavior Management on Resident with Exit Seeking behavior.
The physician's order for [wander management] includes checking for placement q shift and function daily for licensed nurses.
Upon receipt of physician order for [wander management], the licensed nurse will transcribe this to the Medical record (ETAR/EMAR).
The licensed nurse who received the order will apply the [wander management] when available, however in the event that it is not, the resident will be placed on a one-on-one supervision until the [wander management system] becomes available.
The succeeding shift will check for placement and location of the [wander management] as observed.
In order to monitor the accuracy of the medical record documentation, the 7P-7A licensed nurses will perform an audit of physician orders with emphasis on the [wander management] placement and physically check the placement and location of the
The Administrator and the department heads were educated on the QAPI/QAA Processes with emphasis on identifying quality concerns to implement effective plans of action related to adequate supervision resulting in repeated deficient practice to include failure to supervise residents in previous incidents resulting in an immediate jeopardy.
The facility held an Adhoc QAPI on 1/19/24 regarding the following below to check for compliance:
March 20, 2023, last IJ deficiencies
Last Annual survey cited deficiencies.
On 1/31/24, as part of the continuation of the Adhoc QAPI initiated on 1/19/24, the administrator conducted a meeting with the interdisciplinary team on the following Immediate jeopardy deficient practice received from the Agency for Health Care Administration (AHCA) office on the following areas as stated above, (F600, F607, F689, F835, F867).
- Included in the discussion is the plan of correction initiated and some completed prior to this meeting.
The following education and/or corrective actions were completed on 1/26/24 as follows:
F 600 Abuse and Neglect, F 607, F 689,F 835,F 867
Education Plan
The staff, newly hired staff, and agency staff will be educated on the following below:
F 600 Abuse/Neglect, F 607
F 689 with emphasis on Resident with an exit seeking behavior.
F 835 Administration
F 867 QAPI/QAA Process
Elopement drill with emphasis on prompt and timely response to door alarms.
Behavior Management on Resident with Exit Seeking behavior.
The physician's order for [wander management] includes checking for placement q shift and function daily for licensed nurses.
Upon receipt of physician order for [wander management], the licensed nurse will transcribe this to the Medical record (ETAR/EMAR).
The licensed nurse who received the order will apply the [wander management] when available, however in the event that it is not, the resident will be placed on a one-on-one supervision until the [wander management] becomes available.
The succeeding shift will check for placement and location of the [wander management] as observed.
In order to monitor the accuracy of the medical record documentation, the 7P-7A licensed nurses will perform an audit of physician orders with emphasis on the
[wander management] placement and physically check the placement and location of the
equipment on the resident.
DON/ADON/Nurse Supervisor and/or designee will evaluate the [wander management] order process daily to ensure implementation and accuracy.
admission Process on reviewing newly admitted and re-admitted resident's medical record with emphasis on Elopement assessment and order for [wander management] as needed.
The staff will be educated on the DOOR ALARM SYSTEMS:
Types of Alarms in Building
Mag Lock Alarm (15 seconds to respond)- Sound: Audible continuous alarming sound.
Exit Alarm Screamer- Sound: Audible- High Pitch continuous sound activated when door is opened.
[Wander management] alarm: Sound: Audible High Pitch continuous sound activated when a [wander management] crosses the threshold.
[Wander management] Annunciator is located at each Nursing Station and Front Desk and identifies the specific exit door that is open and activated by Wander Guard.
If necessary, education will be provided via telephone and/or mail to ensure compliance is attained by the DON/Staff Developer/designee.
Elopement education/competency will be changed from once a year to twice a year.
Elopement drill will be done by the regional/consultant team on a quarterly basis x 1 year.
The education set forth above will continue for the newly hired employees and staff agency.
Monitoring will be ongoing.
The DON and/or designee will conduct an elopement drill every shift starting on 1/19/2024 x 14 days then daily x 7 days then weekly for 4 weeks and monthly thereafter.
Elopement book audits will be completed by the DON and/or designee daily x 14 days then weekly x 4 weeks then monthly thereafter.
Residents with [wander management] will be audited for placement q shift and functioning daily.
The maintenance director will check the [wander management] system functioning daily.
Nursing will monitor the [wander management] order process daily.
Results of audits will be reported to the QAPI committee monthly to sustain compliance.
Exit doors will be monitored q shift for alarm functioning x 14 days then daily x 4 weeks then weekly thereafter.
Random Door alarm staff response observation.
Education and competency will be monitored by the Regional Clinical Educator and/or designee for 100% completion and will continue to newly hired employees and agency staff.
The revised elopement packet will be shared with existing contracted staffing agencies.
Elopement education and competency will be done twice a year.
Discussed audits/findings in the monthly QAA/QAPI meeting to sustain compliance; may revise POC as needed. The findings will be shared with the [consultant company] for additional oversight.
DON/ADON/Nurse Supervisor and/or designee will evaluate the [wander management] order process daily to ensure implementation and accuracy.
admission Process on reviewing newly admitted and re-admitted resident's medical record with emphasis on Elopement assessment and order for [wander management] as needed.
The staff will be educated on the DOOR ALARM SYSTEMS:
Types of Alarms in Building
Mag Lock Alarm (15 seconds to respond)- Sound: Audible continuous alarming sound.
Exit Alarm Screamer- Sound: Audible- High Pitch continuous sound activated when door is opened.
Wander Guard Alarm: Sound: Audible High Pitch continuous sound activated when a [wander management] crosses the threshold. [Wander management] Annunciator is located at each Nursing Station and Front Desk and identifies the specific exit door that is open and activated by [wander management system]. If necessary, education will be provided via telephone and/or mail to ensure compliance is attained by the DON/Staff Developer/designee.
Elopement education/competency will be changed from once a year to twice a year. Elopement drill will be done by the regional/consultant team on a quarterly basis x 1 year. The education set forth above will continue for the newly hired employees and staff agency. Monitoring will be ongoing. The DON and/or designee will conduct an elopement drill every shift to start on 1/19/2024 x 14 days then daily x 7 days then weekly for 4 weeks and monthly thereafter.
Elopement book audits will be completed by the DON and/or designee daily x 14 days then weekly x 4 weeks then monthly thereafter. Residents with [wander management] will be audited for placement q shift and functioning daily.
The maintenance director will check the [wander management] system functioning daily. Nursing will monitor the: The Administrator and the department heads were educated on the QAPI/QAA Processes with emphasis on identifying quality concerns to implement effective plans of action related to adequate supervision resulting in repeated deficient practice to include failure to supervise residents in previous incidents resulting in an immediate jeopardy.
The facility held an Adhoc QAPI on 1/19/24 regarding the following below to check for compliance:
March 20, 2023, last IJ deficiencies. Last Annual survey cited deficiencies. On 1/31/24, as part of the continuation of the Adhoc QAPI initiated on 1/19/24, the administrator conducted a meeting with the interdisciplinary team on the following Immediate jeopardy deficient practice received from the Agency for Health Care Administration (AHCA) office on the following areas as stated above, (F600, F607, F689, F835, F867). Included in the discussion is the plan of correction initiated and some completed prior to this meeting. The following education and/or corrective actions were completed on 1/26/24 as follows: F 600 Abuse and Neglect, F 607, F 689, F 835, F 867
Education Plan: The staff, newly hired staff, and agency staff will be educated on the following below:
F 600 Abuse/Neglect 607, F 689 with emphasis on Resident with an exit seeking behavior.,
F 835 Administration 867 QAPI/QAA Process. Elopement drill with emphasis on prompt and timely response to door alarms. Behavior Management on Resident with Exit Seeking behavior. The physician's order for [wander management] includes checking for placement q shift and function daily for licensed nurses. Upon receipt of physician order for [wander management] the licensed nurse will transcribe this to the Medical record (ETAR/EMAR). The licensed nurse who received the order will apply the [wander management] when available, however in the event that it is not, the resident will be placed on a one-on-one supervision until the [wander management system] becomes available. The succeeding shift will check for placement and location of the [wander management]] as observed.
In order to monitor the accuracy of the medical record documentation, the 7P-7A licensed nurses will perform an audit of physician orders with emphasis on the [wander management] placement and physically check the placement and location of the equipment on the resident. DON/ADON/Nurse Supervisor and/or designee will evaluate the [wander management] order process daily to ensure implementation and accuracy. admission Process on reviewing newly admitted and re-admitted resident's medical record with emphasis on Elopement assessment and order for [wander management] as needed. The staff will be educated on the DOOR ALARM SYSTEMS: Types of Alarms in Building. Mag Lock Alarm (15 seconds to respond)- Sound: Audible continuous alarming sound .Exit Alarm Screamer- Sound: Audible- High Pitch continuous sound activated when door is opened. [Wander management Alarm]: Sound: Audible High Pitch continuous sound activated. The Administrator and the department heads were educated on the QAPI/QAA Processes with emphasis on identifying quality concerns to implement effective plans of action related to adequate supervision resulting in repeated deficient practice to include failure to supervise residents in previous incidents resulting in an immediate jeopardy. The facility held an Adhoc QAPI on 1/19/24 regarding the following below to check for compliance: March 20, 2023, last IJ deficiencies. Last Annual survey cited deficiencies.
On 1/31/24, as part of the continuation of the Adhoc QAPI initiated on 1/19/24, the administrator conducted a meeting with the interdisciplinary team on the following Immediate jeopardy deficient practice received from the Agency for Health Care Administration (AHCA) office on the following areas as stated above, (F600, F607, F689, F835, F867). Included in the discussion is the plan of correction initiated and some completed prior to this meeting.
The following education and/or corrective actions were completed on 1/26/24 as follows: F 600 Abuse and Neglect, F 607, F 689, F 835, F 867 .The staff, newly hired staff, and agency staff will be educated on the following below:
F 600 Abuse/Neglect 607, F 689 with emphasis on Resident with an exit seeking behavior. F 835 Administration 867 QAPI/QAA Process, Elopement drill with emphasis on prompt and timely response to door alarms, Behavior Management on Resident with Exit Seeking behavior. The physician's order for [wander management] includes checking for placement q shift and function daily for licensed nurses. Upon receipt of physician order for wander management], the licensed nurse will transcribe this to the Medical record (ETAR/EMAR). The licensed nurse who received the order will apply for the [wander management] when available, however in the event that it is not, the resident will be placed on a one-on-one supervision until the [wander management] becomes available. The succeeding shift will check for placement and location of the [wander management] as observed. In order to monitor the accuracy of the medical record documentation, the 7P-7A licensed nurses will perform an audit of physician orders with emphasis on the [wander management] placement and physically check the placement and location of the
equipment on the resident. DON/ADON/Nurse Supervisor and/or designee will evaluate the [wander management] order process daily to ensure implementation and accuracy admission Process on reviewing newly admitted and re-admitted resident's medical record with emphasis on Elopement assessment and order for [wander management] as needed. The staff will be educated on the DOOR ALARM SYSTEMS: Types of Alarms in Building. Mag Lock Alarm (15 seconds to respond)- Sound: Audible continuous alarming sound . Exit Alarm Screamer- Sound: Audible- High Pitch continuous sound activated when door is opened. [Wander management] alarm: Sound: Audible High Pitch continuous sound activated when a [wander management] crosses the threshold. [Wander management] Annunciator is located at each Nursing Station and Front Desk and identifies the specific exit door that is open and activated by [Wander management] If necessary, education will be provided via telephone and/or mail to ensure compliance is attained by the DON/Staff Developer/designee. Elopement education/competency will be changed from once a year to twice a year. Elopement drill will be done by the regional/consultant team on a quarterly basis x 1 year. The education set forth above will continue for the newly hired employees and staff agency. Monitoring will be ongoing. The DON and/or designee will conduct an elopement drill every shift starting on 1/19/2024 x 14 days then daily x 7 days then weekly for 4 weeks and monthly thereafter. Elopement book audits will be completed by the DON and/or designee daily x 14 days then weekly x 4 weeks then monthly thereafter. Residents with [wander management] will be audited for placement q shift and functioning daily. The maintenance director will check the [wander management] system functioning daily. Nursing will monitor the [wander management] order process daily. Results of audits will be reported to the QAPI committee monthly to sustain compliance. Exit doors will be monitored q shift for alarm functioning x 14 days then daily x 4 weeks then weekly thereafter. Random Door alarm staff response observation. Education and competency will be monitored by the Regional Clinical Educator and/or designee for 100% completion and will continue to newly hired employees and agency staff. The revised elopement packet will be shared with existing contracted staffing agencies. Elopement education and competency will be done twice a year. Discussed audits/findings in the monthly QAA/QAPI meeting to sustain compliance; may revise POC (Plan Of Correction) as needed. The findings will be shared with the [consulting company] for additional oversight.
[Wander management] Annunciator is located at each Nursing Station and Front Desk and identifies the specific exit door that is open and activated by [Wander management]. If necessary, education will be provided via telephone and/or mail to ensure compliance is attained by the DON/Staff Developer/designee. Elopement education/competency will be changed from once a year to twice a year. Elopement drill will be done by the regional/consultant team on a quarterly basis x 1 year. The education set forth above will continue for the newly hired employees and staff agency. Monitoring will be ongoing. The DON and/or designee will conduct an elopement drill every shift starting on 1/19/2024 x 14 days then daily x 7 days then weekly for 4 weeks and monthly thereafter.
Elopement book audits will be completed by the DON and/or designee daily x 14 days then weekly x 4 weeks then monthly thereafter. Residents with [wander management] will be audited for placement q shift and functioning daily.
The maintenance director will check the [wander management] system functioning daily.
Nursing will monitor the [wander management] order process daily.
Results of audits will be reported to the QAPI committee monthly to sustain compliance.
Exit doors will be monitored q shift for alarm functioning x 14 days then daily x 4 weeks then weekly thereafter.
Random Door alarm staff response observation.
Education and competency will be monitored by the Regional Clinical Educator and/or designee for 100% completion and will continue to newly hired employees and agency staff.
The revised elopement packet will be shared with existing contracted staffing agencies.
Elopement education and competency will be done twice a year.
Discussed audits/findings in the monthly QAA/QAPI meeting to sustain compliance; may revise POC as needed. The findings will be shared with the [consultants] for additional oversight. Results of audits will be reported to the QAPI committee monthly to sustain compliance. Exit doors will be monitored q shift for alarm functioning x 14 days then daily x 4 weeks then weekly thereafter. Random Door alarm staff response observation.
Education and competency will be monitored by the Regional Clinical Educator and/or designee for 100% completion and will continue to newly hired employees and agency staff. The revised elopement packet will be shared with existing contracted staffing agencies. Elopement education and competency will be done twice a year.
Discussed audits/findings in the monthly QAA/QAPI meeting to sustain compliance; may revise POC as needed.
On 1/30/2024 to 2/01/2024, the corrective actions that were verified by the survey team related the facility's Quality Assurance and Performance Improvement (QAPI) Committee failure to identify quality concerns to implement effective plans of action related to adequate supervision resulting in repeated deficient practice included:
The staff (128 persons) at 100% were in-serviced/trained on 1/19/2024-1/29/2024, regarding: how to respond to call lights promptly, elopement drills, codes, and emergencies responses, how to respond to door alarms, competency for elopement training, how to deal with patients that have behaviors, behavior management for exit seeking resident, abuse, neglect and exploitation training, accidents, and hazards and the QAPI process with the administrative team. The facility conducted a thorough inspection of all eight (8) exit doors and their existing alarm systems to make sure they are in working order in the facility, each exit door has a wander guard alarm, a screamer alarm (Installed 1/19/2024) and an egress maglock alarm with a 15 second opening delay. The alarm systems are audible and can be heard at their loudest in the area where it goes off and is reasonably audible throughout the facility.
Nurses are assigned to check residents with wander guards at least once per shift for placement and functionality. The Elopement Risk Book was revised on 01/28/2024, contains-List of Residents, Guidelines for elopement /Unsafe Wandering Prevention, Facility Floor Plan, Pictures of Residents for elopement, Face sheets, Elopement Drill Schedule, and Elopement Mock Drills protocol. A 6-foot fence was installed to the north courtyard to ensure that residents are not able to exit to the neighborhood and busy streets from the facility's courtyard on the north wing.
Maintenance staff or their qualified designees, conduct weekly door audits to ensure all doors are in proper working order, including checking that the alarm is audible at the nursing station and care areas. An audit of all residents who reside in the facility was conducted to evaluate at risk for leaving the facility without informing staff and/or if they may desire to leave the facility. Additional Audits-Dated 1/19-27/2024; Elopement Drill Audit, Dated 1/20-28/2024; [ wander management alarm] bracelet Audit, Dated 1/21/2024 to 1/26/2024; Daily Door Audits (All shifts), Dated 1/21/2024 to 1/27/2024; Elopement Drill/Actual Event Evaluation, Dated 1/28/2024; Facility Search Grid.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to maintain an accurate record for one (Resident #1) out of three resi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to maintain an accurate record for one (Resident #1) out of three residents reviewed for elopement. The resident had a doctor's order to wear an alarm bracelet and it was documented the resident wore the alarm bracelet every day on each shift, but the resident was not wearing said alrm bracelt as documented in the medical record.
The findings included:
Record review of the Demographic Face Sheet for Resident #1documented the resident was initially admitted on [DATE] and readmitted [DATE] with diagnosis that include but not limited to Alzheimer's disease and seizures.
Review of the Minimum Data Set (MDS) Quarterly Assessment for Resident #1 dated 12/25/2023 documented the resident's Mental Status (BIMS) Summary Score had a BIMS Summary Score of 03 out of 15 indicating severe cognitive impairment and the resident was not able to make her needs known. The resident required partial to moderate assistance for ADL (Activities of Daily Living). The resident had unclear speech, moderately impaired vision with no corrective lenses, had wandering behavior that occurred and a wander/elopement alarm was used daily.
Review of the Physician's Order Sheets (POS) and Medication Administration Records (MAR) for December 2023 and January 2024 documented: apply [wander management alarm] bracelet to right wrist. Check for placement shift and functioning q (every) week. Report any issues immediately to supervisor. The order start date was 8/24/2022. The [wander management alarm] bracelet was checked every day for the month of December 2023 and January 2024 and indicated the resident was wearing it.
Review of Resident's #1 Elopement care plan dated 4/21/2021 documented the resident has a potential for elopement risk related to cognitive impairment, who was exit seeking, wandered the unit and wandered near exit doors; Goal: Resident will safe and will refrain from leaving facility unsupervised thru the next review date; Interventions: Perform frequent observations of residents whereabouts every shift; Provide redirection when observed going towards exit door; Apply alarm bracelet as ordered on right wrist; Verify placement every shift and check for proper functioning weekly.
Review of the Elopement Risk Assessment/Evaluation dated 3/23/2023 and 6/29/2023 documented: The resident is at low risk for elopement, does not wander and has never eloped.
On 1/30/2024 at 10:06 AM, the Registered Nurse (RN), Regional Clinical Director stated: Based on the footage from the camera, it appears that the resident did not have a [wander management] bracelet on, the red light did not go off as it should when a resident with a [wander management] gets near the exit door. She did not have an [wander management] bracelet.
On 1/30/2024 at 10:36 AM, Staff A, Licensed Practical Nurse (LPN) via telephone stated: I was working on the 11:00 to 7:00 AM shift on 1/19/2024, I was sitting at the desk and doing daily assessments and the resident was sitting with me, she got up and walked to the side. At 1900 I prepared to make rounds, upon making rounds all 30 residents were accounted for awake and alert. I accepted Medication Cart #2 keys, counted narcotics, and started with med pass. Around 11:30 PM, I stopped to eat. At around 12:00 AM, I started charting sitting at the desk. At that time the resident was at the nursing station with me. The resident got up and walked around the South side of the nursing station. Between 1:45 AM, the call light went off in room [ROOM NUMBER], bed C, I went to assess the resident. When I returned to the nurse's station I saw the light at the back door blinking. I realized that someone had opened or touched the door. I went to the door to check it. I never heard an alarm on the door go off. I just saw the red-light blinking. I was facing the door and went to check the resident's (Resident #1) room and she was not in the room. I went to the resident's room because she was the only resident that was up at that time by the nurses' station. I was not the nurse assigned to the resident. I alerted everyone and a code green was called, and we started the search. Sometimes the resident would be up at night at the nurses' station. This was common for her to be up at night. I don't recall her having on an [wander management alarm] bracelet.
On 1/30/2024 at 11:35 AM, during observation with Regional Director of Operations of the video showing Resident #1 exiting the building the Regional Director of Operations stated: The resident walked out of the door and the alarm for the door went off and the nurse [Staff A, LPN] was sitting at the North wing nurses' station and did not get up. The resident was wearing an alarm bracelet and the alarm on the [wander management] alarm bracelet did not sound off. According to our investigation and interviews with the nurses, the resident was not wearing a [wander management alarm] bracelet.
On 1/31/2024 at 7:38 AM, the RN, Regional Clinical Director stated, Her [wander management] a bracelet alarm was checked on 12/20/2023. She did have a [wander management alarm] bracelet. The maintenance person checks the [ wander management] alarm bracelet monthly and nursing checks every shift. The resident was not placed on one to one because the resident was being closely monitored at the nurses' station that night, her room is next to the nurses' station, and she is checked on frequently. On 12/20/2023 the [wander management] alarm bracelet was checked specifically for this resident.
On 1/31/2024 at 7:57 AM, the Maintenance Director stated: I checked the [wander management] alarm bracelets weekly before the incident and now it is checked every day. I have a [ wander management] alarm bracelets tag and I set off the alarm on each door. For the resident, she was last checked on 12/20/2023 and it was functioning.