CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to provide adequate supervision and a secured environmen...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to provide adequate supervision and a secured environment for one (Resident #1) out of three residents sampled with exit seeking behaviors. This deficient practice led to Resident #1 exiting the facility undetected at approximately 5:45AM on 5/22/23. The facility's lack of adequate supervision and failure to ensure an adequate and effective alert monitoring system was in place enabled the resident to elope undetected by staff on 5/22/23 at approximately 5:45 AM. The resident was located at approximately 7:23 AM on 5/22/23 by law enforcement at a local high school 1.7 miles away from the facility. Law enforcement reported the resident's location to the facility's Director of Nursing (DON) after the resident was identified by a staff member dropping her child off at the local high school. There were 50 residents residing in the facility at the time of the survey.
The Administrator was informed of the possible existence of the immediate jeopardy (IJ) on 06/05/2023 at approximately 12:45PM. The IJ Template was provided to the administrator on 06/05/2023 at 5:49PM.
On 06/06/2023, it was determined the Immediate Jeopardy was Past Non-Compliance due to the corrective actions implemented and quality assurance implemented prior to the start of the survey.
Refer to F835.
The Findings Included:
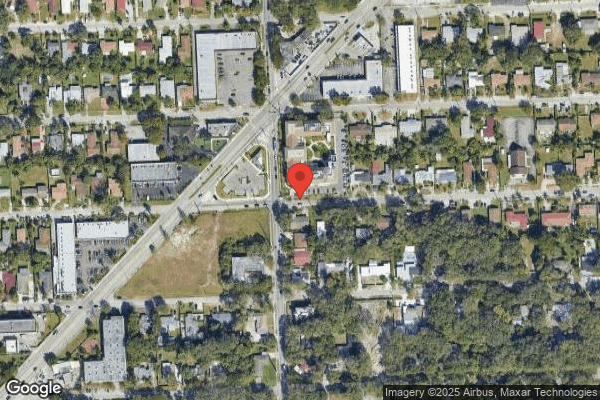
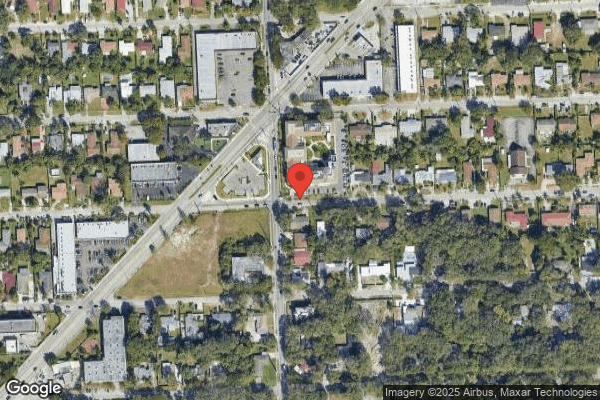
On 6/5/23 at 9:05 AM during an observational tour of the facility with the Director of Maintenance (DOM), surveyors retraced the path Resident #1 took to exit the facility. Resident #1 exited the north station second floor exit door, down two flights of stairs to the first floor, exited the north station first floor exit door that led to the facility's parking lot, where there was an open gate leading out to a residential street. The facility is in an area that has a high traffic volume and is located on the corner of a busy intersection near a major roadway. At the time of the tour the alarms on all three of the emergency doors surveyors exited through alarmed. On the second floor of the facility, there were four emergency exits. On the first floor, there are three emergency exits and the main entrance to the facility. At the time of the tour, all the emergency exit doors in the facility were in working order and had a functional alarm system.
Residents #2 and #3, who exhibited exit seeking behavior were observed wearing wander guards with a continuous flashing light displaying they were in working order.
Review of the facility's Policy and procedures titled, Incidents and Accidents revision date 03/03/23 states: It is the policy of this facility for staff to report, investigate and review any accidents or incidents that occur or allegedly occur, on facility property and may involve or allegedly involve a resident and to ensure residents receive adequate supervision to prevent accidents.
Review of the facility's policy and procedures titled, Elopement and Wandering Residents revision date 03/16/2023 states: The facility ensures that residents who are at risk for elopement receive adequate supervision to prevent accidents and receive care in accordance with their person-centered plan of care addressing the unique factors contributing to their elopement risk.
The procedure for locating missing resident:
a. Any staff member becoming aware of a missing resident will alert personnel using the facility approved protocol (e.g., internal alert code).
b. The designated facility staff will look for the resident in the building or on the grounds.
c. If the resident is not located in the building or on the grounds, the Administrator or designee will notify the police department and serve as the designated liaison between the facility and the police department. The Administrator or designee should also notify the Regional Director of Operations and/or Regional Nurse Consultant.
d. Director of Nursing (DON) or designee shall notify the physician and family member or legal representative.
e. Facility will conduct a head count to ensure all other residents have been accounted for.
f. All parties will be notified of the outcome once the resident is located.
g. Reporting to the State Survey agency shall be conducted if applicable.
Interview on 06/05/2023 at 8:55 AM with Director of Maintenance stated that the company that conducts maintenance to all the doors of the facility is a [Local Company] for the door systems. All the doors have a system, if the door is pushed a low sounding alarm goes off and for 15 seconds the door will not open, after 15 seconds the door will open, and a louder alarm will go off. All the nursing stations received the alert, and it tells the location of the alarm going off. Magnetic cards are used by staff to go in and out of the facility through all doors. For residents with wander Guards, the sound is louder for the entrance door, and it will go off as the resident approaches the door. For emergency doors, residents with wander guards will have to push the doors, the doors will make a sound and will not open for 15 seconds, after 15 seconds the door will open, and a very loud alarm goes off. All the emergency doors operate the same way.
Interview on 6/5/23 at 9:30AM with Licensed Practical Nurse (Staff A) for the 2nd floor north station stated she has been working here for 15 days, and stated she was not on shift but she heard about the resident eloping from the facility, stated when the alarm goes off from the exit door it is very loud and you cannot help but to hear it, when the alarm goes off, usually a silver code alert is announced and then all staff know what they need to do and go to the area and receive instructions on what to do from the staff at the location.
Interview on 6/5/23 at 10:10AM with the Interim Nursing Home Administrator (NHA) it was stated, on 5/22/23 in the morning the Registered Nurse (Staff B) went immediately to the door when the alarm sounded, all staff have magnetic key cards in the facility. Staff B magnetic key card did not work, the alarm kept going off, the nurse panicked and instead of pressing the emergency exit door to open it, she went around to the front of the second floor and took the elevator to the 1st floor, exited out of the side/ambulance entrance, went around the building to where the door was alarming to look for the resident, she did not see the resident. We do not have surveillance cameras at the facility. The resident exited the emergency exit door on the first-floor north station that leads out to the parking lot of the facility. The search was expanded, a head count was completed in the facility to figure out who was the missing resident. On 5/22/23 the staff called the Director of Nursing (DON) to notify her about the missing resident, the DON called me, in the meanwhile the staff was searching the building and the neighborhood for the resident. As I was calling the police station to report the incident, I received a call from the DON. The DON stated she received a call from the local Police station stating that they have the resident. The DON went to pick the resident up and brought him back to the facility. The resident was found at the local high school 1.7 miles away from the facility. A staff member was dropping her child off to school and noticed the resident with the police, the staff member gave the police the contact number for the DON.
When the NHA was asked what plans were in place and what plans are currently in place to prevent resident elopements from occurring it was stated, all emergency exit doors have a regular door alarm and a screamer alarm, the staff is notified by hearing the very loud sound. The training we provided is when the alarm goes off, 1-2 persons go through the door to see who went out the door, the remaining staff do a head count to identify which resident is missing, once the staff determine which resident is missing, we do a code silver alert-it is an elopement code for a person we cannot find. Everyone goes to the floor where the resident's room is located and receives an assignment from the designated staff at the location.
When the resident returned to the facility, we completed a head-to-toe assessment of the resident, and placed the resident on 1 to1 supervision. All the residents in the facility were reassessed for wandering and elopement. Currently we have two residents at risk for elopement, they have wander guards, their pictures and face sheets are in an elopement binder at every nursing station and at the front desk. Staff were retrained on the Egress door system-going out through the emergency exit doors with the 15 second push. We activated key cards for all doors for every staff member. Previously some staff members had limited access with their assigned cards and there was an all-access key card on every medication cart that opened all the facility's doors. We educated all the staff on abuse and neglect training, including all contracted staff in the rehabilitation department, environmental and dietary. All the trainings were completed on 6/1/23.
Interview on 06/06/23 at 11:07 AM with Registered Nurse (Staff B) via telephone it was stated, that she has been working in the facility since December of last year, her shift is usually 7:00 PM to 7:00 AM three days a week. When the alarm went off on 05/22/23 at 5:45 AM I ran to the door where the alarm was going, but my key did not work thus the CNAs went running to take the elevator to see if a resident had gone out. We looked everywhere and we could not find anybody. We went to the street to look, and we did not see anything, so we went back to the facility and kept looking and called the DON.
Interview on 06/06/23 at 11:25 AM with Certified Nursing Assistant (Staff C) via telephone it was stated, that she has been working in the facility since November of last year, her schedule is 7:00 PM to 7:00 AM three days a week. She was working the night shift when the resident eloped on 05/22/23. She looked for the resident in the facility and the surroundings and she went in her car with the nurse to look for the resident in the neighborhood, but they could not find him, and they both came back to the facility. Since then, she has been taking more in-service trainings on elopements, elopement drills, abuse and neglect, and resident rights.
Interview on 6/6/23 at 1:57PM with the Director of Nursing (DON) it was stated, I have been working here as the interim DON since 4/17/23. She reported around 6:15AM on 5/22/23 I got a phone call alerting me that the facility had a code silver alert (Elopement), Resident #1 was missing, I arrived to the facility approximately at 6:30 AM, retraced the resident's path through the facility, (from the second floor north station, down the stairs out to the parking lot) at this time staff was already searching the neighborhood on foot, I jumped in my car and began searching in the neighborhood. At 7:23am, I received a call from the local Police department stating that they had the resident at the local high School, and we could come and pick him up. I picked up the resident, gave the police the information they requested about the resident, returned to the facility with the resident, did a head-to-toe assessment, the resident was okay, vital signs were within normal limits, the resident ate his breakfast, received his morning medications, notified family, and let them know the resident was doing well. The family stated they will be coming to the facility right away. The resident's wife usually stays with the resident all day, at the time the resident eloped the wife was not here, and the resident gets very agitated when his wife is not around, the resident's wife stayed with the resident all the time from 5/22/23 until 5/24/23 until he was discharged .
Since this incident happened as the DON, and prior to the incident I had identified that the residents at risk for elopement were all on the first floor, I moved all the elopement residents to the first floor, and it appears that the residents got a little confused with the change of location. I moved 7 residents at risk for elopement from the first floor to the second floor, they seemed to become a little more active after the move, not all at the same time, each resident at different times, this was all a part of my audit as a new DON coming to a new building. I instructed the receptionist to keep their eye on the elevators, educated the nursing staff on the increased anxiety among residents and what to look for. On 4/19/23 I conducted an in-service on elopement, wander guard, care-plans, orders all relating to elopement risk for the nursing staff. Including the Certified Nursing Assistants to check for the functioning of the wander-guards, when in working order, the wander guards should show a continuous flash of red light. Prior to the elopement incident, we identified that we could not meet the needs of the residents at risk of elopement with the increase exit seeking behavior, the whole administrative team and regional office decided that we would start to discharge the residents to locked unit facilities because we could not meet their needs because of the increased activity the residents were displaying.
Review of the Demographic Face Sheet for Resident #1 revealed the resident was initially admitted to the facility on [DATE] and readmitted on [DATE]. Clinical diagnoses included but were not limited to: Alzheimer's Disease, Dementia, unspecified, severity, without behavioral disturbance, Psychotic disturbance, Mood disturbance, Anxiety, Type II Diabetes Mellitus without complications, Hypertension, Seizures and Acute Kidney Failure. Resident #1 was discharged from the facility on 05/24/23.
Review of the Physician's Orders Sheet for May 2023 revealed, Resident #1 had orders that included but were not limited to: 04/19/23 Wander guard to Right Ankle due to: Increased Wandering. Medications included: Divalproex Sodium Tablet Delayed Release 500 Milligram (MG)- Give 1 tablet by mouth three times a day for seizure, Carbamazepine Suspension 100 MG/5ML(milligrams/milliliter) - Give 2.5 ml by mouth every 6 hours for seizure, Mirtazapine Tablet 7.5 MG- Give 1 tablet by mouth at bedtime for depression, Donepezil HCl (Hydrochloride) 5 MG Tablet- Give 1 tablet by mouth at bedtime for Dementia, Valproic Acid Oral Solution 250 MG/5ML (Valproate Sodium) - Give 5 ml by mouth three times a day for Mood stabilization, Lorazepam Tablet 0.5 MG- Give 5 ml by mouth three times a day for Mood stabilization, Olanzapine Tablet 5 MG- Give 5 ml by mouth three times a day for Mood stabilization, Risperidone Tablet 0.5 MG- Give 1 tablet by mouth every 12 hours related to unspecified psychosis not due to a substance or known physiological.
Further review of the Electronic Medical Records (EMAR) for Resident #1 revealed the resident received all his prescribed medications as ordered on the 5/21/23 at night and on 5/22/23 at 9AM in the morning.
Record review of Resident #1 's Quarterly Minimum Data Set (MDS) dated [DATE] revealed: Section C for Cognitive Patterns documented Brief Interview for Mental Status Score was unable to be determined. Section D for Mood documented no response for mood interview. Section E for Behavior documented no physical behavioral symptoms directed towards others (e.g., hitting, kicking, pushing, scratching, grabbing, abusing others sexually), Other behavioral symptoms not directed towards others (e.g., physical symptoms such as hitting or scratching self, pacing, rummaging, public sexual acts, disrobing in public, throwing or smearing food or bodily wastes, or verbal/vocal symptoms like screaming, disruptive sounds)-behaviors of this type occurred 1-3 days, Section E 900 documented no wandering behavior exhibited. Section G for Functional Status documented extensive assistance with two-persons physical assistance required for Activities of daily living. Section J for Health Conditions documented no falls and no shortness of breath. Section N for Medications documented resident received antianxiety and antidepressants in the last 7 days. Section P for physical restraints documented no physical restraints used, no wander/elopement alarm used.
Record review of Resident # 1's Care Plans Reference Date 03/18/23 revealed: Resident is an elopement risk/wanderer related to Impaired safety awareness, actively exit seeking. Goal: The resident's safety will be maintained through the review date. Interventions: supervision for safety, 30-minute frequent monitoring for elopement risk, distract resident from wandering by offering pleasant diversions, structured activities, food, conversation, television, book, Wander alert Guard, and Increased observations for safety
Record review of the Elopement Risk Assessment/Evaluation dated 3/18/23 and 5/22/23 documented: History of elopement/wandering - Resident has history of wandering in past 3 months (post hospitalization or history from resident/family and/or observed wandering behaviors). Cannot follow instructions, cannot communicate. Mobility - Is ambulatory, Adjustment to facility placement - Content with placement, Elopement Risk Score - H, at Risk to Elopement
Record review of the progress notes documented the following:
Dated 05/22/23 timestamped 05:45 Upon providing wound care to resident in room [ROOM NUMBER] with the assistance of one Certified Nursing Assistant (CNAs) staff, the alarm located close to room [ROOM NUMBER] went on. Search made to look for every single resident. Resident in room [ROOM NUMBER] could not be found. All staff kept searching in every single room, then in the parking lot. DON made aware.
Dated 05/22/23 timestamped 08:15 Physician (MD) and resident's family made aware. Resident returned to facility in stable condition. Assessment done, respiration even and unlabored, no complaint of pain voiced. Skin intact, dry and warm to touch; old bruises noted at bilateral arms. Vitals checked: BP 117/68, P 81, R 20, T 97.6, O2 97% room air. Safety and comfort measures maintained, call light within reach. Will continue to monitor.
Dated 05/22/23 time stamped 09:18 Resident placed on 1:1 supervision. Family made aware. Per family they will be coming in to stay with resident to provide supervision.
Physician Progress note Dated 5/22/2023 time stamped 20:57- Situation: The Change In Conditions (CIC) reported on this CIC Evaluation are/were: Behavioral symptoms (e.g. agitation, psychosis). At the time of evaluation resident/patient vital signs, weight and blood sugar were: Blood Pressure: BP 113/63 - 5/22/2023 07:40 Position: Sitting r/arm (Right arm). Pulse: P 63 - 5/22/2023 07:40 Pulse Type: Regular. RR: R 16 - 5/22/2023 07:40. Temperature: T 97.8 - 5/22/2023 07:40 Route: Forehead (non-contact). Weight: W 134.5 lbs. - 5/8/2023 12:13 Scale: Standing. Pulse Oximetry: O2 97.0 % - 5/21/2023 08:27 Method: Room Air. Blood Glucose: BS 100.0 - 3/26/2023 18:14. Resident/Patient is in the facility for: Long Term Care, Relevant medical history is: Dementia. Resident/Patient had the following medications changes in the past week: n/a.
Outcomes of Physical Assessment: Positive findings reported on the resident/patient evaluation for this change in condition were:
Mental Status Evaluation: No changes observed.
Functional Status Evaluation: No changes observed.
Behavioral Status Evaluation: No changes observed- Respiratory Status Evaluation.
Nursing observations, evaluation, and recommendations are: Resident has exit seeking behaviors. Family with resident.
Primary Care Provider Feedback: Primary Care Provider responded with the following feedback:
A. Recommendations: Continue to monitor closely and seek alternative placement within a secured unit.
Maintain aspiration precautions. Assistance with ADLs.
Dated 05/24/23 time stamped 11:31 SW met with resident today. The resident's wife continues to remain at bedside, daughter will be here tonight to provide 1:1 assistance. Resident's mood is calm, no anxious or sad mood observed. Wife voiced resident has remained calm as she remains at beside with resident. Resident's cognition remains impaired, diagnosis of Alzheimer's Disease. Resident has been accepted into locked skilled nursing home and will be transported to facility tonight. Wife and daughter informed and in agreement. The resident's wife translated such to resident.
Dated 05/24/23 time stamped 17:01 Social Worker (SW) contacted resident's daughter to discuss alternate placement options as resident has eloped from facility and continues to be at risk for elopement. Staff and social workers previously discussed that all exit doors in facility can be pushed open after 15 seconds. SW informed daughter that resident requires a locked unit, daughter and resident's wife in agreement. SW contacted locked skilled nursing home and spoke to admissions representative. Clinicals sent to facility via email, Clinicals reviewed by Director of Nursing (DON), resident not accepted at facility. SW contacted admissions representative, at another locked skilled nursing home, clinicals emailed, resident accepted into facility. SW informed daughter and wife, both in agreement with transfer. Facility information provided to daughter. Resident will be transported today to Locked skilled nursing home. Resident will be transported to facility via Transit, pickup time - 8:00 p.m. Resident's wife will accompany resident to facility. Resident provided assistance with packing belongings. Family voiced satisfaction with care rendered while a resident in the facility.
Dated 05/24/23 time stamped 21:00 Resident left facility via stretcher in stable condition accompanied by spouse and two attendants. No complaint of pain or discomfort voiced; no sign of apparent distress noted. Skin intact, dry and warm to touch. Vitals checked: BP 119/71, P 70, R 18, O2 97% room air, T 97.5. Resident left facility with all of his belongings.
The facility's immediate jeopardy removal plan included:
On 5/22/23 - Manager on Duty checklist and schedule developed.
On 5/22/23 - 6/30/23; Active Manager on Duty schedule in place.
On 5/22/23 - Elopement risk re-evaluations were completed for 100% of residents currently residing in the facility. No new residents identified at risk for elopement based on re-evaluations.
On 05/22/23 to 05/31/23 - Elopement drills or door activation drills followed by a full elopement drill were conducted each shift.
Elopement risk alert binders were reviewed by the DON/designee for accuracy and were confirmed to have demographics present for all residents at risk for elopement.
On 6/6/23 - Observation of the first and second floor north nursing and entrance reception area-risk alert binders in each station and entrance with the demographic sheet of the residents and picture confirming that the resident is at risk for elopement.
On 5/22/23-Orders were reviewed by the DON/designee for presence of wander guard placement and function for residents at risk for elopement. Wander guards were verified to be functioning. Observation on 6/6/23 revealed currently there are only two residents in the facility at risk for elopement. The two residents observed wearing wander guards on their wrists, and the wander guards were working correctly.
On 5/22/23 - Care plans were reviewed for residents at risk for elopement, 6/6/23 care plans confirmed to be present and revised as indicated.
On 5/23/23 - Facility egress doors checked for alarm/functioning by maintenance director. Outside door vendor, [A .], evaluated all doors for proper function. Egress doors are determined to be alarming/functioning properly. Screamers verified to be functioning appropriately.
On 5/23/23 - Administrator (NHA) Job description reviewed with NHA by President of Clinical services. NHA educated on how to access support services from regional team.
On 5/23/23 - Director of Nursing (DON) Job description reviewed with DON by President of Clinical services.
The DON initiated staff education on Accidents/Incidents, Abuse & Neglect, and Elopements with Post-tests, including possible elopement risk factors and providing adequate supervision to help prevent accidents and elopements.
On 05/23/23-06/01/23; Abuse and Neglect Training, elopement training/drills, Egress Door, and Door Activation training, and accidents and incidents training completed for all staff, including pre and post test. Attendees-Eighty-four (84) staff to include Registered Nurses, licensed Practical Nurses, Certified Nursing Assistants, Housekeeping staff, Dietary Staff, Speech therapists, Occupational therapists, Physical therapists, Activities Supervisor, Activities staff, Receptionists, Social Services Director, Central Supply Staff, Maintenance Director, Administrator, Marketing staff, Minimum data Set Coordinator, and Admissions Staff.
On 5/23/23-6/01/23 - Staffing reviewed by NHA and DON daily.
On 5/31/23 Elopement risk status added to the Gray Bar in electronic medical record for all residents at risk for elopement. Record review revealed that a field was added; Special Instruction reads: Elopement Risk.
Record review revealed on 05/23/23 Maintenance Director installed additional screamers. On 05/24/23 the Maintenance Director changed the internal mechanism inside the screamers to provide a continuous alarm until manually reset by the key.
On 5/23/2023 - DON continued staff education on Accidents/Incidents, Abuse & Neglect, and Elopement with post tests including door egress process. Elopement drills or door activation drills followed by a full elopement drill continued each shift.
On 5/24/2023 - Staff education continues relating to Accidents/Incidents, Abuse and Neglect, and Elopements with post-tests including door egress procedures.
A root cause analysis was completed on the event and review of action plan. A Quality Assurance and Quality Improvement meeting was conducted to discuss the event, the root cause analysis, and the performance improvement plan. Door screamers were changed to alarm continuously until manually reset by key. Magnetic cards to unlock the stairwell doors were activated to allow staff immediate access. Elopement drills and door activation drills continue.
On 5/24/23 further record review of root cause analysis revealed: Problem Statement, one sentence description of event or problem: Resident was able to exit unit via stairwell without being detected. Why - 15 sec egress upon pushing on door. Why -Staff was unable to open the door. Why-Door locks and appropriate magnetic card were not utilized, and staff did not use 15 second egress. Why- Lack of education. Root Cause(s)- Failure to provide appropriate education.
On 5/25/2023 and 5/26/2023 - The Orientation packet was reviewed to ensure current elopement procedures were included, education was given to licensed nurses about notification of changes related to increased anxiety and exit seeking behaviors. Nurses were educated on adding additional interventions and oversight to exit seeking residents. Elopement drills and door activation drills continue.
From 5/26/2023 to 6/1/2023, staff education continued until 100% compliance was obtained on elopement drills.
On 6/1/2023 - Elopement drills and door activation drills continue.
The DON or designee will conduct quality reviews on new admissions/readmissions for elopement risk status to ensure care plan was in place and interventions in place for residents identified at risk for elopement weekly x 4 weeks. Quality reviews to be continued monthly x 3 months. Reviews were ongoing.
The DON or designee will conduct elopement competency reviews with 10 staff weekly x 4 weeks to ensure staff remain competent on elopement process. Competency reviews to be continued monthly x 3 months. Reviews ongoing.
The immediate jeopardy removal plan was verified as completed from June 5 - 6, 2023 by reviewing the above documentation; observing inside and outside surroundings of the facility; observing all the coded, audible alarm exit doors in the facility in working order; interviewing thirty (30) staff members to verify they received elopement, incidents and accidents, abuse and neglect in-services, participated in elopement drills, and egress door and door activation training.
The verification included RN's, LPN's, and CNA's from all shifts, support staff and contracted staff in housekeeping, dietary and rehabilitation.
Reviewed in-services and sign in sheets for:
Dates-05/23/23-06/01/23; Abuse and Neglect Training, elopement training/drills, Egress Door, and Door Activation training, and accidents and incidents training completed for all staff, including pre and post test. Attendees-Eighty-four (84) staff -Registered Nurses, Licensed Practical Nurses, Certified Nursing Assistants, Housekeeping staff, Dietary Staff, Speech Therapists, Occupational Therapists, Physical Therapists, Activities Supervisor, Activities staff, Receptionists, Social Services Director, Central Supply Staff, Maintenance Director, Administrator, Marketing staff, Minimum Data Set Coordinator, and Admissions Staff.
Dates-5/23/23 - 6/2/23; Ongoing elopement drills training for all staff on every shift.
Date-5/31/23 - Quality Improvement and Performance process, performance improvement process and data analysis for audits reviewed, and education provided to the DON and NHA by the [NAME] President of Clinical Services.
Dates-6/2/23-6/6/23 - Ongoing random elopement drills for all staff present in the facility.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews and interviews, the facility's administration failed to implement, provide and to ensure e...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews and interviews, the facility's administration failed to implement, provide and to ensure effective and efficient preventative measures were in place to prevent the elopement of one resident (Resident #1) out of three residents sampled who displayed exit seeking behaviors. As evidenced by inadequate safety measures that included failure to ensure an emergency exit door was able to be opened by staff promptly, ensure the exit door alarm was audible in all areas of the facility in the event of an emergency and failure by staff to implement the assigned level of supervision for resident #1 who was a high risk for elopement. These deficient practices led to Resident #1 exiting the facility undetected through an emergency exit door at approximately 5:45 AM on 5/22/23, placing the resident at risk for injury/harm. There were 50 residents residing in the facility at the time of the survey.
The Administrator was informed of the possible existence of the immediate jeopardy (IJ) on 06/05/2023 at approximately 12:45PM. The IJ Template was provided to the administrator on 06/05/2023 at 5:49PM.
On 06/06/2023, it was determined the Immediate Jeopardy was Past Non-Compliance due to the corrective actions implemented and quality assurance implemented prior to the start of the survey.
Refer to F 689.
The Findings Included:
Review of the facility's Policy and procedures titled, Incidents and Accidents revision date 03/03/23 states: It is the policy of this facility for staff to report, investigate and review any accidents or incidents that occur or allegedly occur, on facility property and may involve or allegedly involve a resident and to ensure residents receive adequate supervision to prevent accidents.
Review of the facility's policy and procedures titled, Elopement and Wandering Residents revision date 03/16/2023 states: The facility ensures that residents who are at risk for elopement receive adequate supervision to prevent accidents and receive care in accordance with their person-centered plan of care addressing the unique factors contributing to their elopement risk.
The procedure for locating missing resident:
a. Any staff member becoming aware of a missing resident will alert personnel using the facility approved protocol (e.g., internal alert code).
b. The designated facility staff will look for the resident in the building or on the grounds.
c. If the resident is not located in the building or on the grounds, the Administrator or designee will notify the police department and serve as the designated liaison between the facility and the police department. The Administrator or designee should also notify the Regional Director of Operations and/or Regional Nurse Consultant.
d. Director of Nursing (DON) or designee shall notify the physician and family member or legal representative.
e. Facility will conduct a head count to ensure all other residents have been accounted for.
f. All parties will be notified of the outcome once the resident is located.
g. Reporting to the State Survey agency shall be conducted if applicable.
Review of the facility's policy and procedure titled, Administration of the Facility revision date 1/12/2022 states: This facility will provide policies and systems to ensure that it is administered in a manner that will focus on attaining and maintaining the highest practicable physical, mental and psychosocial well-being of each resident.
Review of the job description for job titled, Administrator dated 12/2018 revealed: Summary: Lead and direct the overall operation of the facility in accordance with customer needs, government regulations and company policies, with focus on maintaining excellent care for the residents while achieving the facility's business objectives.
Review of the Job Description for job titled, Director of Nursing dated 12/2021 revealed: Summary-Manage the overall operations of the Nursing Department in accordance with Company policies, standards of nursing practices and governmental regulations to maintain excellent care of all residents' needs.
Review of the Job Description for job titled, Registered Nurse dated 04/2020 revealed: Summary- Provide direct nursing care to the residents and provide clinical oversight of the day-to-day nursing activities performed by Licensed Practical Nurses and or Certified Nursing Assistants and/or Patient Care Assistants. Clinical oversight must be in accordance with current Federal, State, and Local standards, guidelines, and regulations that govern the facility.
Review of the Job Description for job titled, Licensed Registered Nurse dated 07/2021 revealed: Summary-Provide direct nursing care to the residents and provide oversight of the day-to-day nursing activities performed by Certified Nursing Assistants and/or Patient Care Assistants. Clinical oversight must be in accordance with current Federal, State, and Local standards, guidelines, and regulations that govern facility.
Review of the Job Description for job titled, Certified Nursing Assistant dated 04/2020 revealed: Summary-Perform direct resident care duties under the supervision of licensed nursing personnel. Assist with promoting a compassionate physical and psychosocial environment for the residents.
On 6/5/23 at 9:05 AM during an observational tour of the facility with the Director of Maintenance (DOM), surveyors retraced the path Resident #1 took to exit the facility. Resident #1 exited the north station second floor exit door, down two flights of stairs to the first floor, exited the north station first floor exit door that led to the facility's parking lot, where there was an open gate leading out to a residential street. The facility is in an area that has a high traffic volume and is located on the corner of a busy intersection near a major roadway. At the time of the tour the alarms on all three of the emergency doors surveyors exited through alarmed. On the second floor of the facility, there were four emergency exits. On the first floor, there are three emergency exits and the main entrance to the facility. At the time of the tour, all the emergency exit doors in the facility were in working order and had a functional alarm system.
Residents #2 and #3, who exhibited exit seeking behavior were observed wearing wander guards with a continuous flashing light displaying they were in working order.
Review of the Demographic Face Sheet for Resident #1 revealed the resident was initially admitted to the facility on [DATE] and readmitted on [DATE]. Clinical diagnoses included but were not limited to: Alzheimer's Disease, Dementia, unspecified, severity, without behavioral disturbance, Psychotic disturbance, Mood disturbance, Anxiety, Type II Diabetes Mellitus without complications, Hypertension, Seizures and Acute Kidney Failure.
Review of the Physician's Orders Sheet for May 2023 revealed, Resident #1 had orders that included but were not limited to: 04/19/23 Wander guard to Right Ankle due to: Increased Wandering.
Record review of Resident #1 's Quarterly Minimum Data Set (MDS) dated [DATE] revealed: Section C for Cognitive Patterns documented Brief Interview for Mental Status Score was unable to be determined. Section D for Mood documented no response for mood interview. Section E for Behavior documented no physical behavioral symptoms directed towards others (e.g., hitting, kicking, pushing, scratching, grabbing, abusing others sexually), Other behavioral symptoms not directed towards others (e.g., physical symptoms such as hitting or scratching self, pacing, rummaging, public sexual acts, disrobing in public, throwing or smearing food or bodily wastes, or verbal/vocal symptoms like screaming, disruptive sounds)-behaviors of this type occurred 1-3 days, Section E 900 documented no wandering behavior exhibited. Section G for Functional Status documented extensive assistance with two-persons physical assistance required for Activities of daily living. Section J for Health Conditions documented no falls and no shortness of breath. Section N for Medications documented resident received antianxiety and antidepressants in the last 7 days. Section P for physical restraints documented no physical restraints used, no wander/elopement alarm used.
Record review of Resident # 1's Care Plans Reference Date 03/18/23 revealed: Resident is an elopement risk/wanderer related to Impaired safety awareness, actively exit seeking. Goal: The resident's safety will be maintained through the review date. Interventions: supervision for safety, 30-minute frequent monitoring for elopement risk, distract resident from wandering by offering pleasant diversions, structured activities, food, conversation, television, book, Wander alert Guard, and Increased observations for safety
Record review of the Elopement Risk Assessment/Evaluation dated 3/18/23 and 5/22/23 documented: History of elopement/wandering - Resident has history of wandering in past 3 months (post hospitalization or history from resident/family and/or observed wandering behaviors). Cannot follow instructions, cannot communicate. Mobility - Is ambulatory, Adjustment to facility placement - Content with placement, Elopement Risk Score - H, at Risk to Elopement
Record review of the progress notes documented the following:
Dated 05/22/23 timestamped 05:45 Upon providing wound care to resident in room [ROOM NUMBER] with the assistance of one Certified Nursing Assistant (CNAs) staff, the alarm located close to room [ROOM NUMBER] went on. Search made to look for every single resident. Resident in room [ROOM NUMBER] could not be found. All staff kept searching in every single room, then in the parking lot. DON made aware.
Dated 05/22/23 Timestamped 08:15 Physician (MD) and resident's family made aware. Resident returned to facility in stable condition. Assessment done, respiration even and unlabored, no complaint of pain voiced. Skin intact, dry and warm to touch; old bruises noted at bilateral arms. Vitals checked: BP 117/68, P 81, R 20, T 97.6, O2 97% room air. Safety and comfort measures maintained, call light within reach. Will continue to monitor.
Dated 05/22/23 time stamped 09:18 Resident placed on 1:1 supervision. Family made aware. Per family they will be coming in to stay with resident to provide supervision.
Physician Progress note Dated 5/22/2023 time stamped 20:57- Situation: The Change In Conditions (CIC) reported on this CIC Evaluation are/were: Behavioral symptoms (e.g. agitation, psychosis). At the time of evaluation resident/patient vital signs, weight and blood sugar were: Blood Pressure: BP 113/63 - 5/22/2023 07:40 Position: Sitting r/arm (Right arm). Pulse: P 63 - 5/22/2023 07:40 Pulse Type: Regular. RR: R 16 - 5/22/2023 07:40. Temperature: T 97.8 - 5/22/2023 07:40 Route: Forehead (non-contact). Weight: W 134.5 lbs. - 5/8/2023 12:13 Scale: Standing. Pulse Oximetry: O2 97.0 % - 5/21/2023 08:27 Method: Room Air. Blood Glucose: BS 100.0 - 3/26/2023 18:14. Resident/Patient is in the facility for: Long Term Care, Relevant medical history is: Dementia. Resident/Patient had the following medications changes in the past week: n/a.
Outcomes of Physical Assessment: Positive findings reported on the resident/patient evaluation for this change in condition were:
Mental Status Evaluation: No changes observed.
Functional Status Evaluation: No changes observed.
Behavioral Status Evaluation: No changes observed- Respiratory Status Evaluation.
Nursing observations, evaluation, and recommendations are: Resident has exit seeking behaviors. Family with resident.
Primary Care Provider Feedback: Primary Care Provider responded with the following feedback:
A. Recommendations: Continue to monitor closely and seek alternative placement within a secured unit.
Maintain aspiration precautions. Assistance with ADLs.
Interview on 06/05/2023 at 8:55 AM with Director of Maintenance stated that the company that conducts maintenance to all the doors of the facility is a [Local Company] for the door systems. All the doors have a system, if the door is pushed a low sounding alarm goes off and for 15 seconds the door will not open, after 15 seconds the door will open, and a louder alarm will go off. All the nursing stations received the alert, and it tells the location of the alarm going off. Magnetic cards are used by staff to go in and out of the facility through all doors. For residents with wander Guards, the sound is louder for the entrance door, and it will go off as the resident approaches the door. For emergency doors, residents with wander guards will have to push the doors, the doors will make a sound and will not open for 15 seconds, after 15 seconds the door will open, and a very loud alarm goes off. All the emergency doors operate the same way.
Interview on 6/5/23 at 9:30AM with Licensed Practical Nurse (Staff A) for the 2nd floor north station stated she has been working here for 15 days, and stated she was not on shift but she heard about the resident eloping from the facility, stated when the alarm goes off from the exit door it is very loud and you cannot help but to hear it, when the alarm goes off, usually a silver code alert is announced and then all staff know what they need to do and go to the area and receive instructions on what to do from the staff at the location.
Interview on 6/5/23 at 10:10AM with the Interim Nursing Home Administrator (NHA) it was stated, on 5/22/23 in the morning the Registered Nurse (Staff B) went immediately to the door when the alarm sounded, all staff have magnetic key cards in the facility. Staff B magnetic key card did not work, the alarm kept going off, the nurse panicked and instead of pressing the emergency exit door to open it, she went around to the front of the second floor and took the elevator to the 1st floor, exited out of the side/ambulance entrance, went around the building to where the door was alarming to look for the resident, she did not see the resident. We do not have surveillance cameras at the facility. The resident exited the emergency exit door on the first-floor north station that leads out to the parking lot of the facility. The search was expanded, a head count was completed in the facility to figure out who was the missing resident. On 5/22/23 the staff called the Director of Nursing (DON) to notify her about the missing resident, the DON called me, in the meanwhile the staff was searching the building and the neighborhood for the resident. As I was calling the police station to report the incident, I received a call from the DON. The DON stated she received a call from the local Police station stating that they have the resident. The DON went to pick the resident up and brought him back to the facility. The resident was found at the local high school 1.7 miles away from the facility. A staff member was dropping her child off to school and noticed the resident with the police, the staff member gave the police the contact number for the DON.
When the NHA was asked what plans were in place and what plans are currently in place to prevent resident elopements from occurring it was stated, all emergency exit doors have a regular door alarm and a screamer alarm, the staff is notified by hearing the very loud sound. The training we provided is when the alarm goes off, 1-2 persons go through the door to see who went out the door, the remaining staff do a head count to identify which resident is missing, once the staff determine which resident is missing, we do a code silver alert-it is an elopement code for a person we cannot find. Everyone goes to the floor where the resident's room is located and receives an assignment from the designated staff at the location.
When the resident returned to the facility, we completed a head-to-toe assessment of the resident, and placed the resident on 1 to1 supervision. All the residents in the facility were reassessed for wandering and elopement. Currently we have two residents at risk for elopement, they have wander guards, their pictures and face sheets are in an elopement binder at every nursing station and at the front desk. Staff were retrained on the Egress door system-going out through the emergency exit doors with the 15 second push. We activated key cards for all doors for every staff member. Previously some staff members had limited access with their assigned cards and there was an all-access key card on every medication cart that opened all the facility's doors. We educated all the staff on abuse and neglect training, including all contracted staff in the rehabilitation department, environmental and dietary. All the trainings were completed on 6/1/23.
Interview on 06/06/23 at 11:07 AM with Registered Nurse (Staff B) via telephone it was stated, that she has been working in the facility since December of last year, her shift is usually 7:00 PM to 7:00 AM three days a week. When the alarm went off on 05/22/23 at 5:45 AM I ran to the door where the alarm was going, but my key did not work thus the CNAs went running to take the elevator to see if a resident had gone out. We looked everywhere and we could not find anybody. We went to the street to look, and we did not see anything, so we went back to the facility and kept looking and called the DON.
Interview on 06/06/23 at 11:25 AM with Certified Nursing Assistant (Staff C) via telephone it was stated, that she has been working in the facility since November of last year, her schedule is 7:00 PM to 7:00 AM three days a week. She was working the night shift when the resident eloped on 05/22/23. She looked for the resident in the facility and the surroundings and she went in her car with the nurse to look for the resident in the neighborhood, but they could not find him, and they both came back to the facility. Since then, she has been taking more in-service trainings on elopements, elopement drills, abuse and neglect, and resident rights.
Interview on 6/6/23 at 1:57PM with the Director of Nursing (DON) it was stated, I have been working here as the interim DON since 4/17/23. She reported around 6:15AM on 5/22/23 I got a phone call alerting me that the facility had a code silver alert (Elopement), Resident #1 was missing, I arrived to the facility approximately at 6:30 AM, retraced the resident's path through the facility, (from the second floor north station, down the stairs out to the parking lot) at this time staff was already searching the neighborhood on foot, I jumped in my car and began searching in the neighborhood. At 7:23am, I received a call from the local Police department stating that they had the resident at the local high School, and we could come and pick him up. I picked up the resident, gave the police the information they requested about the resident, returned to the facility with the resident, did a head-to-toe assessment, the resident was okay, vital signs were within normal limits, the resident ate his breakfast, received his morning medications, notified family, and let them know the resident was doing well. The family stated they will be coming to the facility right away. The resident's wife usually stays with the resident all day, at the time the resident eloped the wife was not here, and the resident gets very agitated when his wife is not around, the resident's wife stayed with the resident all the time from 5/22/23 until 5/24/23 until he was discharged .
Since this incident happened as the DON, and prior to the incident I had identified that the residents at risk for elopement were all on the first floor, I moved all the elopement residents to the first floor, and it appears that the residents got a little confused with the change of location. I moved 7 residents at risk for elopement from the first floor to the second floor, they seemed to become a little more active after the move, not all at the same time, each resident at different times, this was all a part of my audit as a new DON coming to a new building. I instructed the receptionist to keep their eye on the elevators, educated the nursing staff on the increased anxiety among residents and what to look for. On 4/19/23 I conducted an in-service on elopement, wander guard, care-plans, orders all relating to elopement risk for the nursing staff. Including the Certified Nursing Assistants to check for the functioning of the wander-guards, when in working order, the wander guards should show a continuous flash of red light. Prior to the elopement incident, we identified that we could not meet the needs of the residents at risk of elopement with the increase exit seeking behavior, the whole administrative team and regional office decided that we would start to discharge the residents to locked unit facilities because we could not meet their needs because of the increased activity the residents were displaying.
The facility's immediate jeopardy removal plan included:
On 5/22/23 - Manager on Duty checklist and schedule developed.
On 5/22/23 - 6/30/23; Active Manager on Duty schedule in place.
On 5/22/23 - Elopement risk re-evaluations were completed for 100% of residents currently residing in the facility. No new residents identified at risk for elopement based on re-evaluations.
On 05/22/23 to 05/31/23 - Elopement drills or door activation drills followed by a full elopement drill were conducted each shift.
Elopement risk alert binders were reviewed by the DON/designee for accuracy and were confirmed to have demographics present for all residents at risk for elopement.
On 6/6/23 - Observation of the first and second floor north nursing and entrance reception area-risk alert binders in each station and entrance with the demographic sheet of the residents and picture confirming that the resident is at risk for elopement.
On 5/22/23-Orders were reviewed by the DON/designee for presence of wander guard placement and function for residents at risk for elopement. Wander guards were verified to be functioning. Observation on 6/6/23 revealed currently there are only two residents in the facility at risk for elopement. The two residents observed wearing wander guards on their wrists, and the wander guards were working correctly.
On 5/22/23 - Care plans were reviewed for residents at risk for elopement, 6/6/23 care plans confirmed to be present and revised as indicated.
On 5/23/23 - Facility egress doors checked for alarm/functioning by maintenance director. Outside door vendor, [A .], evaluated all doors for proper function. Egress doors are determined to be alarming/functioning properly. Screamers verified to be functioning appropriately.
On 5/23/23 - Administrator (NHA) Job description reviewed with NHA by President of Clinical services. NHA educated on how to access support services from regional team.
On 5/23/23 - Director of Nursing (DON) Job description reviewed with DON by President of Clinical services.
The DON initiated staff education on Accidents/Incidents, Abuse & Neglect, and Elopements with Post-tests, including possible elopement risk factors and providing adequate supervision to help prevent accidents and elopements.
On 05/23/23-06/01/23; Abuse and Neglect Training, elopement training/drills, Egress Door, and Door Activation training, and accidents and incidents training completed for all staff, including pre and post test. Attendees-Eighty-four (84) staff to include Registered Nurses, licensed Practical Nurses, Certified Nursing Assistants, Housekeeping staff, Dietary Staff, Speech therapists, Occupational therapists, Physical therapists, Activities Supervisor, Activities staff, Receptionists, Social Services Director, Central Supply Staff, Maintenance Director, Administrator, Marketing staff, Minimum data Set Coordinator, and Admissions Staff.
On 5/23/23-6/01/23 - Staffing reviewed by NHA and DON daily.
On 5/31/23 Elopement risk status added to the Gray Bar in electronic medical record for all residents at risk for elopement. Record review revealed that a field was added; Special Instruction reads: Elopement Risk.
Record review revealed on 05/23/23 Maintenance Director installed additional screamers. On 05/24/23 the Maintenance Director changed the internal mechanism inside the screamers to provide a continuous alarm until manually reset by the key.
On 5/23/2023 - DON continued staff education on Accidents/Incidents, Abuse & Neglect, and Elopement with post tests including door egress process. Elopement drills or door activation drills followed by a full elopement drill continued each shift.
On 5/24/2023 - Staff education continues relating to Accidents/Incidents, Abuse and Neglect, and Elopements with post-tests including door egress procedures.
A root cause analysis was completed on the event and review of action plan. A Quality Assurance and Quality Improvement meeting was conducted to discuss the event, the root cause analysis, and the performance improvement plan. Door screamers were changed to alarm continuously until manually reset by key. Magnetic cards to unlock the stairwell doors were activated to allow staff immediate access. Elopement drills and door activation drills continue.
On 5/24/23 further record review of root cause analysis revealed: Problem Statement, one sentence description of event or problem: Resident was able to exit unit via stairwell without being detected. Why - 15 sec egress upon pushing on door. Why -Staff was unable to open the door. Why-Door locks and appropriate magnetic card were not utilized, and staff did not use 15 second egress. Why- Lack of education. Root Cause(s)- Failure to provide appropriate education.
On 5/25/2023 and 5/26/2023 - The Orientation packet was reviewed to ensure current elopement procedures were included, education was given to licensed nurses about notification of changes related to increased anxiety and exit seeking behaviors. Nurses were educated on adding additional interventions and oversight to exit seeking residents. Elopement drills and door activation drills continue.
From 5/26/2023 to 6/1/2023, staff education continued until 100% compliance was obtained on elopement drills.
On 6/1/2023 - Elopement drills and door activation drills continue.
The DON or designee will conduct quality reviews on new admissions/readmissions for elopement risk status to ensure care plan was in place and interventions in place for residents identified at risk for elopement weekly x 4 weeks. Quality reviews to be continued monthly x 3 months. Reviews were ongoing.
The DON or designee will conduct elopement competency reviews with 10 staff weekly x 4 weeks to ensure staff remain competent on elopement process. Competency reviews to be continued monthly x 3 months. Reviews ongoing.
The immediate jeopardy removal plan was verified as completed from June 5 - 6, 2023 by reviewing the above documentation; observing inside and outside surroundings of the facility; observing all the coded, audible alarm exit doors in the facility in working order; interviewing thirty (30) staff members to verify they received elopement, incidents and accidents, abuse and neglect in-services, participated in elopement drills, and egress door and door activation training.
The verification included RN's, LPN's, and CNA's from all shifts, support staff and contracted staff in housekeeping, dietary and rehabilitation.
Reviewed in-services and sign in sheets for:
Dates-05/23/23-06/01/23; Abuse and Neglect Training, elopement training/drills, Egress Door, and Door Activation training, and accidents and incidents training completed for all staff, including pre and post test. Attendees-Eighty-four (84) staff -Registered Nurses, Licensed Practical Nurses, Certified Nursing Assistants, Housekeeping staff, Dietary Staff, Speech Therapists, Occupational Therapists, Physical Therapists, Activities Supervisor, Activities staff, Receptionists, Social Services Director, Central Supply Staff, Maintenance Director, Administrator, Marketing staff, Minimum Data Set Coordinator, and Admissions Staff.
Dates-5/23/23 - 6/2/23; Ongoing elopement drills training for all staff on every shift.
Date-5/31/23 - Quality Improvement and Performance process, performance improvement process and data analysis for audits reviewed, and education provided to the DON and NHA by the [NAME] President of Clinical Services.
Dates-6/2/23-6/6/23 - Ongoing random elopement drills for all staff present in the facility.