CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to protect the resident's right to be free from neglect ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to protect the resident's right to be free from neglect by not ensuring staff implemented measures to mitigate the risk and prevent elopement for 1 of 3 residents reviewed for Elopement, of a total sample of 23 residents, (#1).
These failures contributed to the elopement of resident #1 and placed her at risk for serious injury, impairment, and/or death. While resident #1 was out of the facility unsupervised, there was likelihood she could have fallen, been accosted by unknown persons, become lost or been hit by a vehicle.
On 12/28/2023 at approximately 3:30 PM, resident #1, a vulnerable [AGE] year old female was admitted to the facility from the hospital. While she was at the hospital, doctors determined she was at risk of wandering unsafely without 24-hour supervision, and she required care and services to monitor her and implement measures to ensure freedom from harm and prevent known risks of endangerment.
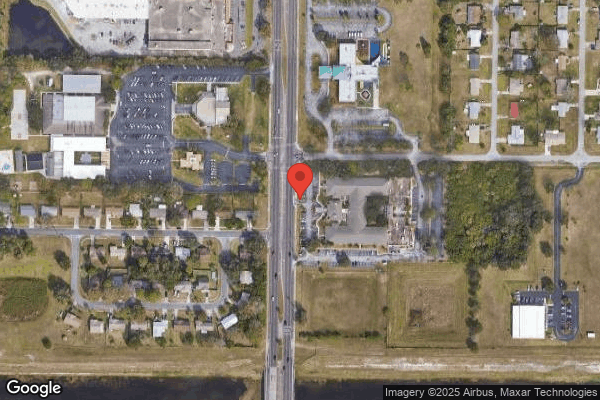
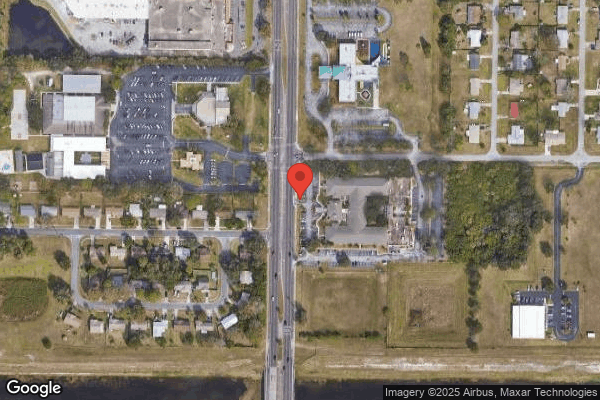
On 12/30/23 at approximately 12:00 PM, the facility failed to provide appropriate care and services to prevent a physically and cognitively impaired vulnerable resident, assessed to be an elopement risk from exiting the facility unsupervised. The resident was allowed to exit the building and walked approximately 0.3 miles down a heavily trafficked 4 lane highway with speed limit of 45 miles per hour. The route along the way was noted to have uneven, sloped terrain/pavement, curbs, and a retention ditch. The facility was unaware of the resident's elopement until she was returned to the facility by her daughter who received a phone call from police when the resident was found wandering at a nearby pharmacy. The facility failed to implement preventive interventions per standards of care to mitigate the resident's risk of elopement.
The facility's failure to identify the need for adequate supervision and ensure a secure environment contributed to resident #1's elopement and placed all residents who wandered at risk. This failure resulted in Immediate Jeopardy starting on 12/30/23. The Immediate Jeopardy was removed on 1/12/24 and the facility corrected the noncompliance at F600 on 1/19/24. The noncompliance at F600 was determined to be past noncompliance.
Findings:
Cross reference F689
Review of the medical record revealed resident #1 was admitted to the facility from an acute care hospital on [DATE] with diagnoses including encephalopathy (brain dysfunction), cognitive communication deficit, dementia, lack of coordination, difficulty in walking, unsteadiness on feet, muscle weakness, stroke, heart attack, and pulmonary embolism (blood clot in a lung). The admission Data Collection form dated 12/28/23 revealed resident #1 was alert, confused, oriented only to person, and did not require assistive mobility devices. The assessment identified resident #1 was at risk for elopement, received high-risk anticoagulant (blood thinner) medication, and had poor balance and an unsteady gait (walking pattern).
The Minimum Data Set 5-day assessment with Assessment Reference Date 12/31/23 revealed resident #1 was unable to complete the Brief Interview for Mental Status (BIMS). The Staff Assessment for Mental Status noted the resident had short term and long term memory problems. She was unable to recall the current season, location of her room, staff name and faces, nor what type of facility she was at. Staff documented Cognitive Skills for Daily Decision Making as moderately impaired. No behaviors were noted, and wandering was noted as having occurred in the past 1 to 3 days. Walking and using up to 4 steps were noted as independent, and she used a wheelchair with supervision.
The hospital Discharge Summary documented resident #1 required 24-hour supervision. The Cognition Status and Precautions read, Fall risk, impulsive, poor insight, poor judgement, easily distracted, memory deficit., and coordination section read, . difficulty following commands and poor planning and sequencing.
The Florida Agency for Health Care Administration 5000-3008 Medical Certification for Medicaid Long Term Care Services and Patient Transfer Form dated 12/27/23 revealed resident #1's decision making capacity required a surrogate. She was at risk for falls, and required assistance with transfers and ambulation.
Review of physician's orders dated 12/28/23 revealed resident #1 required a responsible party to go out of the facility, and received the high-risk medication Apixaban twice daily for blood clot prevention with monitoring for abnormal bleeding. Review of Order Audit reports noted orders were entered by the Weekend Supervisor on 1/01/24 and were backdated to 12/30/23 at 11:42 AM, for a wander prevention device and monitoring.
The Functional Status Evaluation/admission noted the resident needed assistance from another person when walking from room to room and planning regular tasks. The form showed evaluations for how the resident usually bent or stooped from standing, went up and down 1 or more steps, and/or a curb, and walked 10 feet or more on uneven or sloping surfaces (indoor or outdoor) such as turf or gravel was not attempted due to a medical condition or safety concern, and a wheelchair had normally been used in the previous 7 days.
A Transfer/Mobility Status Criteria assessment dated [DATE] noted the resident needed hands on support when moving from sitting to standing with a gait belt.
The Physical Therapy Evaluation Assessment Summary completed on 12/29/23 noted the resident was referred to therapy for decreased functional mobility, strength, functional limitations with ambulation, balance, and increased need for assistance from others. She presented with balance deficits, decreased insight, safety awareness, strength and cognition impairments. The assessment documented the resident required stand by assistance for bed mobility, transfers, and ambulation without an assistive device for 250 feet with safety instructions when challenged with obstacles. Her gait speed indicated she functioned at limited community ambulator level, and she was at risk for falls.
An Elopement Risk Evaluation completed after the elopement incident dated 12/30/23, noted her Wandering Risk score was 3 out of 3 that indicated she was at high risk for elopement. The Elopement Risk Evaluation section included positive responses to the following: independently mobile (ambulatory or wheelchair), cognitively impaired with poor decision making, exit-seeking behaviors, wandering oblivious to safety needs, and ability to exit the facility. The evaluation noted staff were to report all residents at risk to the Director of Clinical Services and on the 24-hour report.
The Baseline Care Plan dated 12/28/23 documented resident #1 was at risk of falling. The care plan did not include preventive measures or interventions for elopement risks.
A Care Plan Focus was initiated on 12/30/23 after the elopement incident for elopement risk/wanderer, related to impaired cognition, dementia, and ambulatory status. The goal noted the resident would not leave the facility unattended and included interventions for an electronic monitoring device placed on her left ankle and one-one supervision. An Elopement Risk Evaluation dated 12/30/23 completed after the elopement, noted her Wandering Risk score was 3 out of 3 that indicated she was at high risk for elopement. The Elopement Risk Evaluation section included positive responses to the following: independently mobile (ambulatory or wheelchair), cognitively impaired with poor decision making, exit-seeking behaviors, wandering oblivious to safety needs, and ability to exit the facility. The evaluation noted staff were to report all residents at risk to the Director of Clinical Services and on the 24-hour report.
The admission Data Collection form dated 12/28/23 completed by Registered Nurse (RN) A noted resident #1 was alert, confused, oriented only to person, and she did not require assistive mobility devices. The assessment identified the resident was at risk for elopement, received high-risk anti-coagulant (blood thinner) medication, and she had poor balance and an unsteady gait.
During an interview with RN A on 4/01/24 at 4:16 PM, he recalled he completed resident #1's admission assessments on 12/28/23 soon after she had arrived at approximately 3:30 PM, on a Thursday. The RN explained, he determined the resident was a high elopement risk, she wandered around the facility, and she was, exit-seeking. He said nurses had standing physician's orders to implement a wander prevention device and/or increased supervision if needed. The RN stated, I didn't put a wander prevention device on her, that was my mistake; I should have put a wander prevention device on her.
On 4/03/24 at 3:32 PM, the Director of Nursing (DON) explained the Interdisciplinary Team (IDT) discussed all new admissions every weekday morning during clinical meetings. He said all risk assessments, orders, and medication reconciliation, and 24-hour reports were reviewed to identify any concerns. He said there was nothing abnormal about the day following resident #1's admission. The DON acknowledged the resident was assessed as high elopement risk by RN A on the admission Data Collection form on 12/28/23. He noted there were no safety interventions implemented like a wander prevention device or increased supervision prior to her elopement and stated, the team should have caught it.
On 4/02/24 at 1:54 PM, Licensed Practical Nurse (LPN) E recalled resident #1 was included in her assignment during the 7:00 AM to 3:00 PM shift on 12/29/23, the day after the resident was admitted . She said the resident was very anxious at the beginning of the shift, and more comfortable later when her daughter visited. She explained it was the nurse's duty to implement a wander prevention device or increased supervision. She indicated the information and photo was then placed in Elopement Risk binders kept at all nurses' stations, therapy, and reception when residents were identified as exit seeking. The LPN said resident #1 did not have a wander prevention device nor increased staff supervision at the end of her shift.
On 4/02/24 at 1:09 PM, the Discharge Planner LPN recalled resident #1 was included in her assignments when she worked regular shifts on 12/29/23 during 3:00 PM to 11:00 PM, and 12/30/23 during 7:00 AM to 3:00 PM, the day the resident eloped. She explained, nurses were expected to implement elopement precautions when wandering or risk was identified that included a wander prevention device first and/or 15-minute checks. She said the resident did not have a wander prevention device nor increased supervision during her shifts before she eloped. She explained, early into the 7:00 AM to 3:00 PM shift on 12/30/23, she observed the resident pacing, looking for her daughter. She stated, we came to the conclusion she was maybe looking to leave. The LPN did not explain why elopement precautions were not implemented before the resident exited the facility, unsupervised.
The Change in Condition form completed by the Discharge Planner, LPN on 12/30/23 read, . resident left facility unattended, law enforcement notified family, and family returned the resident to the facility .
On 4/04/24 at 2:19 PM, Certified Nursing Assistant (CNA) B recalled on 12/30/23, prior to the elopement at approximately 11:00 AM, resident #1 was confused and wandered the facility. She said the resident was exit-seeking, panicking, and upset because she was looking for her daughter and said she wanted to go home. The CNA explained she became concerned the resident may attempt to leave the building through the front entrance. She said she let nurses know about her concerns and she called the Receptionist. She provided the Receptionist with a detailed physical description and alerted her to look out for the resident. The CNA stated, she was ready to go; she was waiting for the right opportunity for an open door; she had her purse and everything ready; she was just trying to find the right outing.
In a joint interview on 4/03/24 at 10:40 AM with the DON and Regional Clinical Director, the DON said resident #1 should have had a wander prevention device in place immediately after she was identified as high elopement risk. She explained elopement precautions should have been implemented before she got out when other nurses and CNAs became concerned. The Regional Clinical Director indicated the facility's investigation revealed the Receptionist neglected to verify who the resident was before she opened the door and the admitting nurse identified the resident as high risk for elopement but neglected to initiate any interventions.
In a telephone interview with the former Medical Director on 4/05/24 at 10:33 AM, he recalled resident #1's elopement incident and said the facility had notified him. He explained the root cause was nurses lack of timely implementation of safety precautions and stated, she fell through the cracks.
On 4/05/24 at 12:50 PM, the current Medical Director said he was aware of the elopement incident. He explained, residents at risk of elopement with cognitive deficits were especially vulnerable as they were not well protected without supervision outside the facility. He stated, trying to prevent serious injuries from occurring is important to all residents.
The facility's standards and guidelines titled, Abuse Neglect, Exploitation, and Misappropriation, N-1265, dated 11/28/17 read, . Neglect is the failure of the center, it's employees or service providers to provide goods and services to a resident that are necessary to avoid physical harm, pain, mental anguish, or emotional distress. Examples include but are not limited to: . Failure to adequately supervise a resident known to wander from the facility without the staff knowledge.
The Facility Assessment Tool dated 3/27/24 read, . Using our facility admission evaluation process, residents are carefully evaluated pre admission to ensure that we can meet their needs and have the required competencies and training to do so .
Review of the facility's corrective corrective actions were verified by the survey team and included the following:
On 12/30/23 at 1:00 PM, resident #1 was assessed by nurses and no injuries were noted. The resident was placed on 1:1 supervision with an electronic wander prevention device until she was discharged home on [DATE].
*On 12/30/23, at 1:00 PM, a facility wide head count was conducted to ensure all residents were accounted for.
*On 12/30/23, the facility reviewed all current residents' records to ensure no other residents were affected.
*On 12/30/23, the facility reviewed the previous 30 days admissions to ensure elopement assessments were accurate and interventions were in place for any identified elopement risks.
*On 12/30/23, the facility conducted one on one training with RN A for elopement evaluation accuracy and timely interventions for identified residents at risk. Education was provided to all staff responsible for Receptionist duties on visitor sign in/out processes and the importance of identity validation prior to unlocking the door for exit. Any future new staff appointed for Reception desk responsibilities to receive the same training.
*On 12/30/23, a visitor badge requirement was implemented.
*From 12/30/23 to 1/02/24, facility nursing management completed quality reviews for all residents identified as at risk for elopement to ensure accuracy of orders, care plans, assessments, [NAME], and precaution binders were in place and accurate with every shift daily monitoring of wander prevention device placements and daily exit door functions.
*On 12/31/23, the facility ordered additional electronic monitoring devices and created a par level to ensure availability of adequate supply.
*On 1/01/24, the Maintenance Director conducted facility wide door function, safety, and security checks and no concerns were identified.
*From 1/01/24 to 1/12/24, daily elopement drills were conducted across all shifts. The frequency of drills were reduced to weekly through 1/27/24 and continued monthly for ongoing review of improvements as needed.
*From 1/03/24 to 1/12/24, 100% of all licensed nurses were educated on elopement assessments and timely implementation of safety interventions for any resident identified at risk.
*On 1/08/24, the facility's clinical leadership ensured 100% of current residents had accurate records of elopement evaluations and did not identify any additional concerns.
*On 12/30/23, the facility filed an Immediate Federal report related to the allegation of neglect for resident #1 and initiated a full investigation.
*From 12/30/23 to 1/19/24, Ad Hoc Quality Improvement Performance Committee meetings were held for root cause analysis, plan of correction, and monitoring.
*On 1/05/24, the facility submitted a 5-day report to the State Agency (SA).
*From 12/30/23 to 1/12/24, 100% of the facility's regular and contracted staff received education on facility policy and procedures for elopement procedures and from 12/29/23 to 1/12/24, the facility educated 100% of their facility staff for identification of neglect. This was confirmed with post tests.
*Additional QAPI meetings held 1/2/24, 1/5/24, 1/12/24 and 1/18/24 to discuss plan of correction progress.
Review of the in-service attendance sheets noted staff participated in education on the topics listed above.
From 4/04/24 to 4/05/24, interviews were conducted with 27 staff members who represented all shifts. The facility's staff included 53 CNAs, and 34 licensed nurses. All staff, including 15 CNAs, 4 LPNs, 4 RNs, 1 Housekeeper, 1 Receptionist, 1 Social Services Director, and 1 Certified Occupational Therapy Assistant (COTA) verbalized their understanding of the education provided.
The resident sample was expanded to include 2 additional residents identified as at risk for elopement/neglect. Observations, interviews, and record reviews revealed no concerns related to elopement for residents #2, and #3.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide adequate supervision and a secure environment...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide adequate supervision and a secure environment to prevent elopement for 1 of 3 sampled residents reviewed for elopement, of a total sample of 23 residents, (#1). These failures contributed to the elopement of resident #1 and placed her at risk for injury, impairment, or even death. While resident #1 was out of the facility unsupervised, there was high likelihood she could have fallen and sustained serious injury, become lost, been accosted by a stranger, or hit by a car and died.
On [DATE] at approximately 3:30 PM, resident #1, a vulnerable [AGE] year-old female was admitted to the facility from the hospital. While at the hospital, she was determined to be at risk of wandering unsafely without 24-hour supervision and required care and services to monitor her to ensure her safety.
On [DATE] at 12:05 PM, resident #1 exited the facility's front entrance when the receptionist unlocked the door for her to leave the facility. She walked through a parking lot, turned right, and continued along uneven terrain and sloped declines. She headed northward along uneven, cracked sidewalks, past a retention ditch, through another parking lot at a major intersection until she reached and entered a local retail pharmacy. The store's staff alerted law enforcement after they became concerned resident #1 might be lost. Law enforcement officers found resident #1's daughter's phone number in the resident's pocket and contacted her. The resident's daughter immediately came to the store and transported her mother back to the facility at approximately 1:00 PM. The resident's whereabouts were unknown to the facility until her daughter brought her back, one hour after she left.
The facility's failure to identify and provide adequate supervision and ensure a secure environment contributed to resident #1's elopement and placed all residents who wandered at risk. This failure resulted in Immediate Jeopardy starting on [DATE]. The Immediate Jeopardy was removed on [DATE] and the facility corrected the noncompliance at F689 on [DATE]. The noncompliance at F689 was determined to be past noncompliance
Findings:
Cross reference F600
Review of the medical record revealed resident #1 was admitted to the facility from an acute care hospital on [DATE] with diagnoses including encephalopathy (brain dysfunction), cognitive communication deficit, dementia, lack of coordination, difficulty in walking, unsteadiness on feet, muscle weakness, stroke, heart attack, and pulmonary embolism (blood clot in a lung). The admission Data Collection form dated [DATE] revealed resident #1 was alert, confused, oriented only to person, and did not require assistive mobility devices. The form also indicated resident #1 was at risk for elopement, received high-risk anticoagulant medication, and had poor balance and an unsteady gait (walking pattern).
The Minimum Data Set 5-day assessment with Assessment Reference Date [DATE] revealed resident #1 was unable to complete the Brief Interview for Mental Status (BIMS). The Staff Assessment for Mental Status noted the resident had short term and long-term memory problems, she was unable to recall the current season, location of her room, staff name and faces, nor what type of facility she was at. Staff documented Cognitive Skills for Daily Decision Making as moderately impaired. No behaviors were noted, and wandering was noted as occurred 1 to 3 days. Walking and using up to 4 steps were noted as independent, and she used a wheelchair with supervision.
The hospital Discharge summary dated [DATE] documented resident #1 required 24-hour supervision. The cognition status and precautions read, Fall risk, impulsive, poor insight, poor judgement, easily distracted, memory deficit , and coordination read, . difficulty following commands and poor planning and sequencing.
In a telephone interview on [DATE] at 2:15 PM, resident #5's daughter recalled she received a telephone call from local police who informed her that her mother had been outside the pharmacy and was assisted inside by store employees. She said she was shocked because she had been assured her mother would be placed in the facility's secure dementia unit when she was admitted . Resident #1's daughter said another facility was not able to accommodate her mother because they didn't have a locked unit. She said when she arrived at the store she had to calm her mother down as she was even more confused than usual, scared, and was crying because she thought she was in trouble. Resident #1's daughter said the police officer told her he had called the facility to inquire if she was a resident but was told by facility staff they didn't know who she was. Resident #1's daughter explained when she arrived at the facility with her mother, the staff had not realized resident #1 had been missing for an hour and told her she must have just left the facility. She said she had to stay with her mother for hours after she returned, and she decided it was safer to take her home with family. Resident #1's daughter explained she was very upset and repeatedly thought about how her mother could have been gravely injured or died. She said she could not understand how her mother got out of the facility through the front door as the Receptionist had to unlock the door for anyone to exit.
On [DATE] at 3:13 PM, in a telephone interview, the manager at the local pharmacy store recalled he was working on [DATE] when resident #1 entered the store. He explained the resident was confused and scared as she thought someone was following her. He said the resident told him she had walked from another area of the county (approximately 15 miles away) but he believed her story didn't seem accurate and thought she could be lost. He said the resident gave him her daughter's phone number from a piece of paper in her pocket and store staff contacted local police.
On [DATE] at 10:40 AM, the Director of Nursing (DON) and Regional Clinical Director acknowledged resident #1 eloped from the facility on [DATE] at approximately 12:05 PM. The DON stated the resident was last seen by staff as she entered her room at approximately 12:00 PM the same day. The DON explained, shortly after her admission, resident #1 was assessed by the admitting Registered Nurse (RN) A to be a high elopement risk but the nurse had not implemented the appropriate preventive measures to safely monitor her for wandering. He said the facility's investigation of the incident revealed staff had alerted the Receptionist that resident #1 was exit seeking with her detailed physical description approximately one hour before she exited the facility unsupervised. The DON said the Receptionist's account was the resident exited with a group of visitors unnoticed. Review of the video footage on the Regional Clinical Director's cellular phone however, showed resident #1 was alone, spoke to the Receptionist, pointed towards the door, and walked out of the building unsupervised after the Receptionist unlocked the door for her at 12:05 PM. The resident was dressed appropriately, wore shoes and carried a purse. She headed to the right as she exited the facility and then was not visible on the video camera.
On [DATE] at 4:16 PM, RN A recalled he completed resident #1's admission assessments on [DATE] soon after she arrived at the facility at approximately 3:30 PM, on a Thursday. The RN explained, he determined resident #1 was a high elopement risk, she wandered around the facility, and was, Exit-seeking. He said nurses had standing physician orders to implement an electronic wander prevention device and/or increased supervision if needed. The RN stated, I didn't put (an electronic wander prevention device) on her, that was my mistake; I should have put (an electronic wander prevention device) on her.
Review of the Order Summary Report with physician orders dated [DATE] revealed resident #1 required a responsible party to go out of the facility and received high-risk medication Apixaban twice daily for blood clot prevention along with monitoring for abnormal bleeding.
The Baseline Care Plan completed on [DATE] noted resident #1 was at risk for falls. The care plan did not include a focus for, or interventions related to elopement risk.
The electronic [NAME] for Certified Nursing Assistants (CNA)s did not note any alerts or precautions for wandering, exit-seeking, or elopement.
On [DATE] at 3:32 PM, the DON explained the Interdisciplinary Team (IDT) discussed all new admissions every weekday morning during clinical meetings. He said all risk assessments, orders, and medication reconciliation were reviewed to identify any concerns. He said there was nothing abnormal about the day following resident #1's admission. The DON acknowledged the resident was assessed as high elopement risk by RN A on the admission Data Collection form on [DATE]. He explained appropriate safety interventions, like an an electronic wander prevention device, increased supervision or placement of the resident's information into the elopement precaution binders were not implemented prior to her elopement. He stated, The team should have caught it.
On [DATE] at 1:54 PM, Licensed Practical Nurse (LPN) E recalled resident #1 was on her assignment during the 7:00 AM to 3:00 PM shift on [DATE], the day after the resident was admitted . She said resident #1 was very anxious at the beginning of the shift, and more comfortable later when her daughter visited. LPN E explained it was the nurse's duty to implement an electronic wander prevention device or increased supervision and place high risk resident information and photo into the elopement risk binders kept at all nurses' stations, therapy, and in reception when residents were identified as exit seeking. LPN E said resident #1 did not have an electronic wander prevention device nor had increased staff supervision on [DATE] at the end of her shift.
On [DATE] at 1:09 PM, the Discharge Planner LPN recalled resident #1 was included in her assignments when she worked regular shifts on [DATE] from 3:00 PM to 11:00 PM and [DATE] from 7:00 AM to 3:00 PM, the day resident #1 eloped. She explained, nurses were expected to implement elopement precautions such as an electronic wander prevention device and/or 15-minute checks when a resident was found to be wandering or if a wander risk was identified. The Discharge Planner LPN said resident #1 did not have an electronic wander prevention device nor increased supervision during her shifts before she eloped. She explained, early into the 7:00 AM to 3:00 PM shift on [DATE], she observed resident #1 pacing and looking for her daughter. The Discharge Planner LPN stated, We came to the conclusion she was maybe looking to leave. The Discharge Planner LPN did not explain why safety precautions were not implemented before the resident left the facility unsupervised as per facility procedure.
Review of the medical record revealed after resident #1 eloped on [DATE], a Care Plan focus was initiated for elopement risk/wanderer related to impaired cognition, dementia, and ambulatory status. The goal noted the resident would not leave the facility unattended and included interventions for an electronic wander prevention device placed on her left ankle and one-to-one supervision.
In a telephone interview with the former Medical Director on [DATE] at 10:33 AM, he recalled the facility had notified him of resident #1's elopement incident. He explained the root cause was the nurse's lack of timely implementation of safety precaution interventions and stated, She fell through the cracks.
On [DATE] at 12:50 PM, the current Medical Director said he assumed the position on [DATE] and was aware of the elopement incident. He explained, residents at risk of elopement with cognitive deficits were especially vulnerable as they were not well protected without supervision outside the facility. The Medical Director stated, Trying to prevent serious injuries from occurring is important to all residents.
Telephone calls were made on [DATE] at 2:12 PM and 5:56 PM to the Receptionist who was no longer employed at the facility. She did not return the calls.
Review of the facility's standards and guidelines dated [DATE] titled Clinical Guideline Elopement/Wandering Risk read, . To evaluate and identify patients/residents that are at risk for elopement and develop individualized interventions. If a patient/resident is identified as being at risk complete an Elopement Risk Alert and obtain a full body photograph. Initiate patient centered interventions based on resident's risk. Document patient centered interventions in the patient/resident Care Plan and [NAME]. If utilizing a wander monitoring system device check placement of the device every shift and functionality every day. Maintain the Elopement Risk Alerts in an easily accessible location.
Review of the facility's corrective actions were verified by the survey team and included the following:
*On [DATE], the facility reviewed all current resident records to ensure no other residents were affected.
*On [DATE], the facility reviewed the previous 30 days admissions to ensure elopement assessments were accurate and interventions were in place for any identified elopement risks.
*On [DATE], the facility conducted one-on-one training with RN A for elopement evaluation accuracy and timely interventions for identified residents at risk. Education was provided to all staff responsible for Receptionist duties on visitor sing in/out processes and importance of identity validation prior to unlocking the door for exit. Any future new staff appointed for Reception desk responsibilities to receive the same training.
*On [DATE], a visitor badge requirement was implemented.
*From [DATE] to [DATE] facility nursing management completed quality reviews for all residents identified as at risk for elopement to ensure accuracy of orders, care plans, assessments, [NAME], and precaution binders were in place and accurate with every shift daily monitoring of wanderguard placements and daily exit door functions.
*On [DATE], the facility ordered additional electronic monitoring devices and created a par level to ensure availability of adequate supply.
*From [DATE] to [DATE], daily elopement drills were conducted across all shifts. The frequency of drills were reduced to weekly through [DATE] and continued monthly for ongoing review of improvements as needed.
*From [DATE] to [DATE], 100% of all licensed nurses were educated on elopement assessments and timely implementation of safety interventions for any resident identified at risk.
*On [DATE], the facility's clinical leadership ensured 100% of current residents had accurate records of elopement evaluations and did not identify any additional concerns.
*On [DATE], the facility filed an Immediate Federal report related to the allegation of neglect for resident #1 and initiated a full investigation.
*From [DATE] to [DATE], Ad Hoc Quality Improvement Performance Committee meetings were held for root cause analysis, plan of correction, and monitoring.
*On [DATE], the facility submitted a 5-day report to the State Agency.
*From [DATE] to [DATE], 100% of the facility's regular and contracted staff received education on facility policy and procedures for elopement and drill procedures. This was confirmed with post tests.
*Additional QAPI meetings held [DATE], [DATE], [DATE] and [DATE] to discuss plan of correction progress.
Review of the in-service attendance sheets noted staff participated in education on the topics listed above.
From [DATE] to [DATE], interviews were conducted with 27 staff members who represented all shifts. The facility's staff included 53 CNAs, and 34 licensed nurses. All staff, including 15 CNAs, 4 LPNs, 4 RNs, 1 Housekeeper, 1 Receptionist, 1 Social Services Director, and 1 Certified Occupational Therapy Assistant verbalized their understanding of the education provided.
The resident sample was expanded to include 2 additional residents identified as at risk for elopement. Observations, interviews, and record reviews revealed no concerns related to Elopement for residents #2, and #3.
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Transfer Requirements
(Tag F0622)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure an appropriate discharge process to the community was follo...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure an appropriate discharge process to the community was followed for facility-initiated discharges for 2 of 3 residents reviewed for discharge status of a total sample of 23 residents, (#21 and #29). The facility's failure to safely discharge a resident to the community resulted in actual harm.
Findings:
1. Review of resident #21's medical record revealed she was initially admitted to the facility on [DATE] and readmitted on [DATE] with diagnoses including type 2 diabetes, right below the knee amputation, absence of left toes, anxiety, anemia, chronic heart failure and mood disorder. She was discharged home on 2/21/24.
Review of the Minimum Data Set (MDS) admission assessment with Assessment Reference Date of 1/12/24 revealed a Brief Interview for Mental Status score of 15 out of 15 which indicated intact cognition. The MDS assessment showed resident #21 had impairment on one side in the lower extremity, and used a wheelchair for mobility She required substantial/maximum assistance for toileting hygiene and showers/baths.
Review of resident #21's physician orders included the following:
On 2/19/24, Urinalysis (UA) with culture and sensitivity reflex sediment pathology (Cytology/cell blood) for Urinary Tract Infection (UTI).
On 2/21/24, Cleanse right lateral leg surgical site with normal saline, pat dry, apply Xeroform and cover with bordered gauze dressing every other day.
On 2/21/24, Resident may discharge with medications, belongings, Physical Therapy (PT), Occupational Therapy (OT), Skilled Nursing (SN)/wound care services, Durable Medical Equipment (DME) to include wheelchair.
Review of resident #21's care plan included a discharge plan initiated on 1/15/24. The focus read, HHC (Home Health Care) of choice, DME and services as needed. The goal showed resident #21 would be able to communicate the required assistance post-discharge and the services required to meet her needs before discharge.
Review of resident #21's medical record showed she was initially evaluated by behavioral services on 1/05/24 and most recently on 2/09/24. The progress notes revealed resident #21 suffered from depression, anxiety and insomnia and mentioned she was feeling depressed because she had no income, was not progressing with PT, and had a scab on her leg that could prevent her from using her prosthetic leg.
Review of resident #21's progress notes in the medical record showed the following entries:
*2/1/24 Weekly Interdisciplinary Team (IDT) Utilization Review note included financial concerns commercial insurance authorization approved until 3/16/24 and resident was not wearing her prosthetic leg due to right below knee amputation (R BKA) wound.
*2/8/24 Weekly IDT Utilization Review note indicated resident was non-ambulatory and the discharge plan was to go home alone the week of 2/20/24.
*2/16/24 Weekly IDT Utilization Review note revealed discharge plan was to go home the week of 2/20/24 and financial concerns read, LCD (local coverage determination) 2/19.
Nursing concerns included dressing to right lateral thigh every other day and not wearing prosthetic due to R BKA wound.
*2/21/24 UA result reviewed by APRN (Advanced Practice Registered Nurse) awaiting for sensitivity.
Review of Lab Results Report dated 2/20/24 revealed abnormal results. The UA showed the urine contained a very cloudy appearance, with blood, protein, leukocytes present and nitrite was positive. The culture report was finalized on 2/22/24 and showed the presence of Escherichia Coli (E. coli; a bacteria) in the urine. The sensitivity report included a list of antibiotics that would work best to treat the bacteria.
When treated promptly and properly, lower urinary tract infections rarely lead to complications. But left untreated, UTIs can cause serious health problems. Complications of a UTI may include repeated infections . Permanent kidney damage from a kidney infection due to an untreated UTI. Sepsis, a potentially life-threatening complication of an infection. This is a risk especially if the infection travels up the urinary tract to the kidneys (Retrieved from the Mayo Clinic website at www.mayoclinic.org on 2/09/24).
Review of a physician note dated 2/17/24 revealed resident #21 reported urinary frequency and Oxybutynin 5 milligram (mg) was ordered. The note read, Physical therapy reports patient is now weightbearing on prosthetic and was able to take several steps. Complication: patient has scab on back of stump, which has rubbed on prosthetic, and has some bleeding. Wound care to assist and treat.
Review of the Baseline Care Plan and Summary dated 1/05/24 revealed a manual wheelchair was identified as equipment needed.
Review of a PT Evaluation note dated 1/05/24 revealed resident #21 reported she lived alone in a first-floor apartment with 5-7 steps to enter. At her previous level of function she was walking independently using no assistive device with a right lower extremity (RLE) prosthetic. She had fallen once in the past year and had residual limb wound that led to infection.
Review of a PT Discharge Summary note dated 2/20/24 showed goal to improve the ability to safely transfer to standing position from sitting in a chair, wheelchair, or side of the bed with supervision or stand by assist was not met. A comment read, Sit to stand without prosthesis on moderate assist. Another goal read, Patient will ambulate with RW (rolling walker) using prosthesis 150 ft (feet) SBA (standby assist) to allow for patient to walk into bathroom. Documentation showed this goal was upgraded on 2/08/24 and resident #21 was able to use the prosthesis on the RLE per the physician, but due to an open area on the posterior lateral aspect of the right lower leg it was recommended to withhold the use of the prosthesis until healed. The ambulation and stair/curbs Functional Skills Assessment showed they had not attempted the assessment due to medical conditions or safety concerns. The note indicated resident #21 was discharged home at wheelchair level. The PT discharge recommendations included home health services, a wheelchair, and a slide board.
Review of an OT Progress Report dated 2/15/24 read, Patient was steadily progressing toward goals once allowed to use prosthesis, patient is now restricted again from using prosthesis which is hindering progress. It also read, RLE stump shape has changed and the prosthesis is not fitting correctly and the prosthesis company has been called in order to assess fit of device.
Review of an OT Discharge Summary note dated 2/20/24 revealed, Once granted use of prosthesis patient made substantial gains toward goals. Unfortunately experienced a decline once use of prosthesis was declined to potential of developing a wound. The OT discharge recommendations read, Therapy recommendations are for patient to stay at facility to continue services until patient is able/allowed to use prosthesis safely.
Review of the Discharge Plan and Instructions form dated 2/21/24 revealed resident #21 was discharged home alone in a wheelchair van. The form showed the name of the insurance intermediary for the home health services, wound care services and medical equipment supplier. The reason for discharge read, insurance issued NOMNC (Medicare non-coverage). The form incorrectly showed the skin was intact.
On 4/02/24 at 10:58 AM, during a telephone interview, resident #21 stated the day before her discharge, she was called into the Social Services office and told her insurance cut her off and she was being discharged the next day. She indicated she was informed if she wanted to stay longer, it would cost her $300 something per day. The resident stated she was told she had used her insurance days but she knew she had used less than 50 days, not the 60 she had available, and they could have waited for her to get her wheelchair before discharging her. She explained her discharge was unsafe. She shared she was sent home with a transport company the facility arranged with no way to get around . stuck. She stated she had a hard time getting to and from the bathroom without a wheelchair and fell the second day after being home. The resident noted she had not received HHC services and did not have a wheelchair and was admitted to the hospital. She recalled before she was discharged from the facility, she had been told she could borrow a wheelchair from the facility but was later told she could not borrow it.
On 4/04/24 at 7:28 AM, during a second telephone interview, resident #21 stated she told the facility she lived alone, did not have a wheelchair and had no one to help her. She indicated she was told by Social Services she would be discharged the next day and a wheelchair would be delivered the following day. She recalled she asked how she could appeal the discharge decision and was told appeals were only for Medicare patients. She stated she asked about the Ombudsman information and was told if she wanted to stay it would cost about $371.00 each day. The resident said she was not given the results of the urinalysis and was told to follow up with her Primary Care Physician. She mentioned she learned she had a UTI when she was re-admitted to the hospital the day after she was discharged home. She said she fell on her butt in the bathroom and had to call 911. She indicated she now had another wound as a result of the fall. The resident explained she was in the hospital for 12 days and received intravenous antibiotic therapy to treat the UTI for 5 days. While crying, she stated, How do you go home non-weight bearing, with no wheelchair and no way to get around? She indicated therapists knew she needed a wheelchair to move around, and needed to ensure she had one before she was discharged . She stated while at the facility, she could not walk, and had not practiced using a walker to ambulate to the bathroom or in her room. She said she was upset and felt the facility sent me home to fall and die.
On 4/02/24 at 5:42 PM, the Rehabilitation Director stated resident #21 received PT and OT from 1/5/24 to 2/20/24 and as long as she had her prosthesis, she was able to do pretty good. She explained the facility did not perform home evaluations for residents discharged to the community. The Rehabilitation Director stated she shared therapy recommendations with the Discharge Planner. She explained staff from the prosthesis company came and provided a new sleeve to resident #21.
On 4/03/24 at 9:30 AM, the Discharge Planner explained her responsibilities included setting up HHC services and equipment and helping a resident transition from the facility to home. She stated the discharge planning process began on admission and it was determined by the resident's progress and their insurance. She stated resident #21 came with a contract from the hospital and they already knew she would be discharged on 2/21/24. She stated resident #21 knew she was going to be discharged and never expressed a desire to stay long term in the facility, or she would have initiated a different process. She indicated resident #21 needed HHC services with PT, OT, SN, wound care and requested a wheelchair the day before she left. She mentioned resident #21 had one at home, but wanted a bigger one. The Discharge Planner stated she followed therapy and physician's recommendations for discharge. She indicated she followed up with HHC, DME and insurance intermediaries to ensure equipment was delivered and services were initiated. She stated resident #21's wheelchair order was made last minute on the day before she was discharged when the resident told her she did not have one at home. She explained she spoke with therapy about discharging this resident and they said she had a wheelchair and assistance at home. She remembered she received a call from resident #21 wanting to know when her wheelchair would be delivered the day after she discharged home. The Discharge Planner recalled she told resident #21 it would be delivered on 2/22/24. She indicated resident #21 told her she was in the hospital, but she did not ask why. She acknowledged safety was important for discharged residents.
On 4/03/24 at 10:50 AM, the South Wing Unit Manager (UM) explained resident #21's urine specimen was collected and picked up by the laboratory on 2/20/24. She indicated the result report was posted in resident #21's medical record on 2/22/24 at 11:57 AM, but by then, she was discharged from the facility. She clarified they received the lab results before resident #21 was discharged but were waiting for the sensitivity results. The UA report showed cloudy urine, and was positive for protein, blood, and bacteria. She indicated resident #21 knew she had an outstanding lab, so she had to follow up with her Primary Care Provider. She explained she did not know who reviewed the report but that person should have notified the physician and entered a progress note with the information. She indicated resident #21 would have needed antibiotics to treat her infection. The UM read the progress note entered on 2/21/24 which indicated the APRN was aware of the UA results and was waiting for the sensitivity results. UM stated she did not know if the sensitivity result was ever reported to the APRN.
On 4/03/24 at 1:19 PM, Occupational Therapy Assistant (OTA) F explained resident #21 worked with him to regain her independence with the activities of daily living (ADLs). He stated she was improved but a wound on her stump impeded the use of her prosthesis. He indicated as time progressed, she was allowed to use the prosthesis again, and got better standing up and performing her ADLs. He recalled about a week later she had another skin breakdown from wearing the prosthesis which did not fit perfectly as she had not used it while in the hospital. He explained staff from a prosthesis company visited resident #21, took measurements and mentioned not to use the prosthesis until the wound was completely healed. He stated they did not know the exact date she would be discharged , and learned resident #21 was going home one day in advance of her discharge. He stated he went over with resident #21 what she needed to do to be safe at home as she would not be able to transfer properly without her prosthesis. OTA F indicated he knew a wheelchair, slide board and home care services would be ordered. He stated resident #21 needed assistance from someone if the wheelchair and the slide board were not available. He indicated she would not be able to move safely without the assistance of another person. He recalled she was not comfortable going home and in his professional opinion, it would have been better if she stayed in the facility until her wound healed and the prosthesis was in place. OTA F stated his understanding of her discharge was the insurance was not going to pay past that day and she would have been financially responsible.
On 4/03/24 at 2:24 PM, PT G stated resident #21 had skin graft and a R BKA. She indicated resident #21 was initially non-weightbearing, and they worked on leg strengthening while she needed extensive assistance. PT G explained, on 2/08/24 resident #21 was given the approval to use the prosthesis by her surgeon and she was happy to use it again. PT G indicated this did not go well and resident #21 developed an open area soon after she used it. She explained resident #21 was seen by the prosthesis company staff and they agreed with their recommendation of not using the prosthetic leg until the new wound healed because it could lead to infection. She indicated after making progress they had to revert to practice bed-to-chair and chair-to-toilet transfers and simulate the movements because resident #21 was unable to use her prosthesis. She recalled resident #21 did not attempt to transfer by herself because she was afraid to fall, she knew she was weak, and she was working to build her strength. She stated resident #21 had fallen at home prior to being admitted to the facility. PT G explained resident #21 mentioned her understanding of the discharge was she would have a wheelchair at home readily available. PT G indicated resident #21 was not safe to be at home without a wheelchair and a slide board. She explained they had not performed gait training as that was not indicated with the wound. She stated she was under the impression the Discharge Planner was working on getting additional days approved from the insurance and she was very shocked to learn her insurance did not approve additional time. PT G explained she did not write an explicit recommendation for resident #21 to stay longer for additional therapy but it was implied and concluded when the insurance cuts a resident, that became the financial determination.
On 4/03/24 at 3:10 PM, the Rehabilitation Director indicated she did not know the OT recommendation was for resident #21 to continue with therapy. She stated he wrote the recommendation on the discharge note but did not tell her. She said she did not ask the Discharge Planner to file an appeal or request additional time from the insurance. She confirmed neither the PT nor the OT evaluation mentioned resident #21 had a wheelchair prior to her admission to the facility. She stated lending a wheelchair to resident #21 while she got one from the DME would not have been a problem.
On 4/03/24 at 3:42 PM, Registered Occupational Therapist (OTR) H confirmed he signed off the OT Discharge Summary note dated 2/20/24 which was completed by OTA F. He stated he had started working for the company a week or so prior to resident #21's discharge and had never seen her. He indicated resident #21 was discussed with the therapy team and everyone was aware, The patient would not be safe to go home. OTR H stated he agreed with their recommendation and signed off the note. He mentioned they needed to ensure residents were discharged to a safe environment with the required assistance and proper equipment. He mentioned that based on the OT notes he read about resident #21, she needed the assistance of a caregiver and the wheelchair at home.
On 4/03/24 at 4:22 PM, the Director of Nursing (DON) and Regional Nurse Consultant stated the facility should have contacted resident #21 and informed her of the lab results and potentially faxed the results to her PCP. The DON indicated the APRN did not order antibiotics after the resident was discharged . He mentioned there should have been a follow up regarding the lab results with the resident or her Primary Care Provider. The DON mentioned their former Administrator made the final decision to discharge residents even if the IDT disagreed with him.
On 4/03/24 at 4:59 PM, the Social Service Director reviewed resident #21's Psychosocial Evaluation she completed on 1/11/24. She indicated she learned resident #21's plan was to be a short-term resident and return home. The Social Service Director stated resident #21 lived independently in her own apartment and had a boyfriend that came over and helped her all the time. She indicated resident #21 had a wheelchair at home and told the Discharge Planner she wanted a larger one, Just as she was to leave the facility.
On 4/03/24 at 5:58 PM, Certified Nursing Assistant (CNA) I recalled resident #21 mentioned she was being discharged home. CNA I stated she asked the resident if she had any help at home and her response was she did not have anybody to help her. CNA I stated she asked her, How are you going home if you do not have anyone to help you? She stated her boyfriend did not help her. CNA I asked if she had any other relatives to help her and asked if she thought it was safe for her to go home. The resident responded she was not sure and said, It is what it is. CNA I stated resident #21 had mixed emotions about the discharge. When asked if she mentioned her conversation to the nurse or UM, she stated she did not and was not working when resident #21 was discharged .
On 4/05/24 at 11:27 AM, APRN D stated he visited the facility 3 days a week but was available on call every day. He explained he reviewed the lab results on the computer and nurses also called him with results. He indicated he did not recall if resident #21 had any signs or symptoms of a UTI when he ordered the UA with culture and sensitivity for her. He explained when a patient was asymptomatic, he preferred to wait for the sensitivity results to not impede antibiotic effectiveness. APRN D stated since she was discharged from the facility on 2/21/24, he would not, Typically be in her chart, so he would not have seen the UA culture and sensitivity results. He explained if he had been notified, his recommendation would be to notify the Primary Care Provider of the results. He indicated when a resident was discharged , they instructed them to follow up with their Primary Care Provider within 5-7 days. APRN D mentioned once she left the facility, resident #21 was under the care of her Primary Care Provider, but it did not mean they would not share the information they had. He said the potential outcome of an untreated UTI included the potential to become a bladder infection, which could progress to kidney infection, urosepsis, and ultimately septic shock. He explained a person with diabetes had a compromised immune system and she would have required antibiotics to treat the UTI.
2. Review of resident #29's medical record revealed she was admitted to the facility on [DATE] with diagnoses that included status post-surgery of the digestive system, rheumatoid arthritis, chronic obstructive pulmonary (lung) disease, and chronic pain syndrome.
Review of the MDS admission assessment with Assessment Reference Date of 3/20/24 revealed resident #29 had a Brief Interview for Mental Status score of 15 out of 15 which indicated she was cognitively intact. The MDS assessment showed resident #29 used a walker or wheelchair. She required setup or clean-up assistance for toileting hygiene and showers/bathe and supervision or touching assistance for lower body dressing and personal hygiene.
Review of resident #29's physician orders revealed an order dated 4/02/24 which read, Resident may d/c (discharge) home with meds, belonging, PT/OT/SN and wound care services, DME to include standard wheelchair.
Review of a Physician Progress Note dated 4/01/24 read, Patient seen and examined at bedside today. She says she was told she's going home tomorrow but no one has talked to her about it. She has been having dysuria for two days. A UA was collected last night after I was informed of this. Discussed starting empiric abx (antibiotic) today.
Review of a Progress Note dated 4/02/24 read, Resident discharged home this morning at 11:30 AM. Family accompanied her out. Medications with resident. Treatment to abdominal dressing completed before she went home. Education provided on how to wash surgical wound and the dressing that is needed to be put on. Dressing supplies sent home with resident. To follow up with her PCP 7-10 days. Antibiotic for her UTI called into her pharmacy by Dr. [name of physician]. Resident did get her dose this am (morning) before she left.
Review of a Progress Note dated 3/29/24 revealed a Weekly IDT utilization review meeting included the discharge date was planned for 4/02/24. The note listed financial concerns as of 3/31/24 and nursing concerns for a wound to the abdomen.
Review of a Discharge Plan and Instructions form dated 4/02/24 revealed resident #29 was discharged home with home health services, medical equipment and wound care services.
On 4/04/24 at 12:26 PM, during a telephone interview, resident #29 stated she learned she was discharged from the facility on the day she was sent home by her ex-husband who went to pick her up to bring her to a doctor's appointment. She explained on 4/02/24 her ex-husband got to her room and asked her, Did you know you are discharged today? Well you are. She stated she told him she did not know so he left the room and found out she was scheduled to be discharged at 1:30 PM. She indicated the facility knew she was going to a doctor's appointment that afternoon. She explained she had an abdominal surgical wound and had been lying on her couch since Tuesday waiting for someone to change her dressing. She stated she had not received a call or services from a home health agency as she was told she would. She mentioned she had macular degeneration, was blind and was unable to change the wound dressing by herself. She stated her ex-husband did not live with her and only assisted with medical appointments. She said, My ex-husband stuck stuff he got from the nursing home on my coffee table, but I cannot see, and I do not know what medications or paperwork he received from them. She added, I cannot speak any longer because I am in a lot of pain, and hung up.
On 4/04/24 at 12:38 PM, during a telephone interview, a representative from the Home Health Agency stated they received the referral for services for resident #29 on 4/03/24. She indicated their liaison spoke with the facility's Discharge Planner and told her they were unable to accept the patient because they did not take her insurance.
On 4/04/24 at 3:38 PM, the Social Service Director stated she recalled resident #29 went home with her ex-husband. She stated she lived independently, received assistance whenever needed, and her vision was good. The Social Service Director indicated the Discharge Planner was not in today and she was not aware the Home Health Agency did not accept resident #29.
On 4/05/24 at 1:17 PM, the Administrator stated her expectation was the Discharge Planner faxed and confirmed DME and HHC orders with the appropriate agency to ensure they were providing the services as ordered to the discharged residents.
Review of the job description for the Discharge Planner signed on 5/09/23 revealed job functions included planning and coordinating activities related to discharge planning. The duties and responsibilities included assessing patients and families for post discharge needs and informing patients and families on discharge planning options based on diagnoses, prognoses, resources, and preferences related to home care services.
Review of the job description for the Director of Social Services signed by the SSD on 3/21/23 revealed duties and responsibilities included to keep abreast of current federal and state regulations and participate in discharge planning.
Review of the facility policy and procedure titled Transfer/Discharge Notification & Right to Appeal revised on 10/24/22 read, Transfer and discharges of residents, initiated by the center (facility initiated) will be conducted according to Federal and/or State regulatory requirements. The policy included the facility would provide and document sufficient preparation and orientation, In a form and manner that the resident understands, to ensure safe and orderly transfer or discharge.
Review of the facility policy and procedure titled Discharge Planning dated 11/30/14 revealed after a resident was discharged home or to other facility, a follow-up call or if necessary, a home visit would be performed within 24 to 48 hours, To ascertain that community services/referrals are indeed being provided according to the discharge plan. The policy directed staff to document the after-discharge contact on a social service progress note. The form read, Should pre-scheduled services not be provided or arranged, the social worker will make every attempt to coordinate services and follow-up again.
Review of the facility policy and procedure titled Interdisciplinary Discharge Planning dated 11/30/14 read, If the interdisciplinary team determines the resident is at risk regarding discharge, Social Services is to notify a local agency for at risk persons in the community.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to obtain written authorization to manage personal funds for 1 of 3 r...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to obtain written authorization to manage personal funds for 1 of 3 residents reviewed for personal funds, of a total sample of 23 residents, (#23).
Findings:
Review of resident #23's medical record revealed she was admitted to the facility on [DATE]. Her diagnoses included history of falls, pathological fracture of right humerus, osteoporosis, and muscle weakness. Resident #23 was discharged from the facility on 1/16/23.
Review of the Minimum Data Set admission Assessment with Assessment Reference Date of 12/13/22 revealed resident #23 had a Brief Interview for Mental Status score of 13 which indicated she was cognitively intact. Resident #23's medical record revealed she made all decisions for her care.
On 4/02/24 at 8:23 AM, during a telephone interview, resident #23 explained she lived at the facility for a couple of months and received therapy services. She indicated months after she was discharged , the facility in error received her alimony payments which totaled $1500.00. She said the facility cashed the check without her consent. The resident stated after several calls, the facility returned the money minus $116.18, a balance they said she owed them. She stated she spoke with the facility's billing staff and was told this amount would be refunded, but to this date she had not received the money. She shared she lived on a limited income, and this had created a hardship for her.
Review of a voided check image showed a check dated 10/02/23 in the amount of $1,383.82 payable and mailed to the original sender and not resident #23.
On 4/03/24 at 12:14 PM, the Business Office Manager (BOM) stated she was responsible for posting money received to residents' accounts for patient liability. The BOM recalled resident #23 had spoken to her regarding the checks received by the facility in error. The BOM explained those checks were deposited into their operating account, and she understood they needed to issue a refund. She explained a refund check was made for $1,380.82 and not the $1500.00 they had received because resident #23 owed them money. She said their refund policy included they would deduct any amount owed to the facility. She confirmed resident #23 did not open a trust account and did not consent for them to keep the $116.18.
On 4/04/24 at 12:00 PM, the BOM's assistant explained they usually knew what the checks were for when they came in the mail. She stated they did not deposit checks that were not payable to the facility, but the envelope containing the checks payable to resident #23 must have been addressed to the facility, otherwise they would not have opened it. She indicated since checks were not payable to the facility, they should not have cashed them. She explained when an envelope was addressed to a resident, they gave it back to the receptionist to rescind and send back to her since resident #23 was no longer a resident of the facility. She stated their Corporate office made the decision to issue a refund minus the amount she owed. She confirmed the facility did not obtain a written consent from resident #23 to manage her personal funds.
On 4/04/24 at 1:18 PM, the BOM explained resident #23's alimony checks had never been received by the facility previously. She stated the facility had no idea the checks were alimony checks. The BOM indicated the facility did not get checks payable to residents and the checks they handled were all payable to the facility. She acknowledged the checks in question were payable to resident #23 but stated a message on top of the check read, Please post this payment for our mutual customer. She indicated they assumed that was a payment for her account since she had a balance. The BOM explained if the envelope was addressed to the resident, they would not have opened it. She indicated once they spoke with resident #23, they understood the checks were sent to the facility in error and did not accept any more checks. She indicated they submitted a refund request for $1500.00 through a refund portal but the refund was processed by their Corporate office.
On 4/05/24 at 1:17 PM, the Administrator stated her understanding was any checks that came to the facility were deposited into their operating account and applied to the resident's balance. She stated at the time they received resident #23's alimony checks, she had an outstanding balance, and it was their policy to cover that before processing a refund.
Review of the admission Agreement signed by resident #23 on 12/23/22 read, The Center will refund any overpayment due to the Patient within state and or federal guideline. In the event of the Patient's death or discharge, refunds and any of the Patient's personal property remaining in the center will be returned to the Patient, Patient's estate, or other personal authorized by law pursuant to state and federal law. The Patient may, but is not required, to deposit personal spending money to be maintained in accordance with state and federal laws, when necessary, by the Center. The Patient must sign an authorization form, and the Center will not charge additional fee for this service.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify the residents or their representatives of a facility-initiat...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify the residents or their representatives of a facility-initiated discharge in a timely manner and in writing and failed to submit a copy of the notice to the State Long-Term Care (LTC) Ombudsman for 3 of 3 residents reviewed for discharge status out of a total sample of 23 residents, (#21, #28 and #29).
Findings:
1. Resident #21 was readmitted to the facility on [DATE] with diagnoses including type 2 diabetes, right below the knee amputation, absence of left toes, anxiety, anemia, chronic heart failure and mood disorder. She was discharged home on 2/21/24.
On 4/04/24 at 7:28 AM, resident #21 stated she was verbally informed she would be discharged the day before she went home. She indicated she asked the facility how to appeal her insurance's decision for discharge and was told it only applied to Medicare patients. She asked for the Ombudsman's information but did not receive it and was told if she wanted to stay it would cost her about $371.00 a day. She stated she signed a discharge form as she was wheeled out of the facility and did not receive any copies of the documents she signed.
2. Resident #28 was admitted to the facility on [DATE] with diagnoses including urinary tract infection, muscle weakness, difficulty in walking, Parkinsonism, and dementia. She was discharged home on 4/03/24.
On 4/04/24 at 2:52 PM, during a telephone interview with resident #28's son, he stated he thought she was going to be in the facility longer. He explained he was told the insurance did not approve her to stay longer. He indicated a second appeal was not an option mentioned by the facility. He stated he was told you either come pick her up or you need to pay the $1,400.00 for the 4 days since the insurance coverage ended when your appeal was lost. The son explained his mother was by herself during the day while he worked and he was afraid for her as she was still weak, a fall risk and could hurt herself. He stated he felt pressured to take her home and did not have any other option. He said he was not aware of the services of the LTC Ombudsman's office.
On 4/04/24 at 3:41 PM, the Social Services Director (SSD) stated resident #28 went home yesterday, and the discharge paperwork was completed by the Discharge Planner. She indicated she had verified the discharge plans upon admission and did not have any information about the discharge.
3. Resident #29 was admitted to the facility on [DATE] with diagnoses including status post-surgery of digestive system, rheumatoid arthritis, and chronic pain syndrome. She was discharged home on 4/02/24.
On 4/04/24 at 12:26 PM, resident #29 stated she learned she was going home the same day she was discharged . She explained her ex-husband came to the facility to take her to a doctor's appointment, and he was told she would be discharged with him that day.
Review of the medical records revealed no evidence of notification to the LTC Ombudsman's Office for residents #21, #28, or #29. There was no evidence of a written notification of discharge given to residents #28 and #29. Review of a Nursing Home Transfer and Discharge Notice for resident #21 was signed by the resident on 2/21/24, the same day she was sent home.
On 4/03/24 at 4:22 PM, the Regional Nurse Consultant stated she had not seen the Agency for Healthcare Administration (AHCA) Nursing Home Transfer and Discharge Notice used for the discharges of non-Medicare residents. She indicated she was not sure of the appeal processes for commercial insurance.
On 4/04/24 at 3:20 PM, the SSD stated the Medical Records Coordinator was responsible for sending transfer and discharge notifications to the LTC Ombudsman. She indicated residents #28 and #29 did not receive the AHCA Nursing Home Transfer and Discharge Notice because their payors were not Medicare.
On 4/05/24 at 9:13 AM, the Medical Records Coordinator explained she did not send any documents to the Ombudsman, as that was done by the Discharge Coordinator or the SSD. She explained she uploaded the forms to the residents' medical records when she received them. The Medical Records Coordinator indicated the SSD told her she could not find evidence of the Ombudsman notification for discharges in 2024. She explained she was asked to handle the bed hold and transfer to hospital forms in March 2024, but not the discharges.
On 4/05/24 at 1:17 PM, the Administrator stated the SSD was responsible for all notifications to the Ombudsman.
Review of the facility policy and procedure titled Transfer/Discharge Notification & Right to Appeal revised on 10/24/22 read, Transfer and discharges of residents, initiated by the center (facility initiated) will be conducted according to Federal and/or State regulatory requirements. The policy disclosed, Before a center transfers or discharges a resident the center must: Notify the resident and resident representative(s) of the transfer or discharge and the reasons for the move in writing (in a language and manner they understand). The Center must send a copy of the notice to a representative of the Office of the State Long-Term Care Ombudsman. Record the reasons for the transfer or discharge in the resident's medical record.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure implementation of policies to include thorough monitoring of previously identified areas of concern and adequately track performance...
Read full inspector narrative →
Based on interview and record review, the facility failed to ensure implementation of policies to include thorough monitoring of previously identified areas of concern and adequately track performance to ensure prior improvement measures for discharge notifications were realized and sustained.
Findings:
Cross reference F623
Review of the facility's policy, Quality Assurance and Performance Improvement (QAPI) revised 10/24/22 read, The center will monitor department performance systems to identify issues or adverse events. Center will review department system data. If a quality deficiency is identified, the committee will oversee the development of corrective action(s).
The facility was cited at F623, Notice Requirements Before Transfer/Discharge
, §483.15(c)(3) (6)(8), Code of Federal Regulations, during the last complaint survey conducted 6/07/23.
Review of the Plan of Correction (POC) which served as the facility's allegation of compliance with the alleged citations, approved by the QAPI committee on 7/06/23 read, SSD (Social Services Director) was re-educated by the regional nurse on 6/15/23 regarding the components of this regulation with emphasis on appropriate notification of discharges to the Ombudsman. The POC included the Executive Director or designee would conduct quality monitoring of discharges through morning meeting to ensure appropriate notification to the Ombudsman was completed weekly for four weeks then biweekly and PRN (as needed). The POC revealed the findings were reported to the QAPI committee monthly.
During the current survey, F623 was again identified with no continued oversight of the before mentioned citation.
On 4/05/24 at 1:17 PM, the Administrator stated she was ultimately responsible for overseeing the operation of the facility. She explained they performed audits and monitored processes to remain in compliance. She stated the SSD was responsible for the Ombudsman notification and she was unaware this was not being done as required.