CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to have a functional administration that enabled them ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to have a functional administration that enabled them to effectively and efficiently use their resources to maintain a safe environment. Facility staff failed to monitor blood pressure for one resident (#1) of three residents sampled taking blood pressure medication, the facility staff failed to carry out change of shift duties in manner to provide care and ensure nursing staff and equipment were available for residents on the 200, 400, and 800 halls including one resident (#1) that experienced respiratory distress. Staff failed to provide ADL (activities of daily living) care to three out of three residents (#1, 5, and 6) sampled out of 49 residents dependent on staff for showers.
Interviews with multiple staff members revealed on-going staffing issues. There is no staffing coordinator in the facility and the duties are being shared between the DON and the Central Supply Clerk. Scheduling errors were being made, staff were unaware of their schedules, and staff cancellations were not being covered. Interviews revealed staff members are unable to complete resident ADL care as expected due to having large resident assignments.
On 2/17/23 at 11:00 p.m. Staff A, Licensed Practical Nurse (LPN) was the only nurse working on the floor, with a census of 114 residents, for approximately three hours. Staff D, LPN was in the building until 1:46 a.m., however, she was only waiting and had no resident assignment. Staff A, LPN was assigned 57 residents total on the 500, 600, and 700 halls. The 57 residents total on the 200, 400, and 800 halls had no nurse assigned to them. Resident #1 resided on the 800 hall, with no nurse assigned to her. At approximately 1:45 a.m. Resident #1's CNA noticed the resident was not well and called for Staff A, LPN to come help. At that time Resident #1's blood pressure was 58/42, respirations 28, pulse 136, and oxygen saturation 71%. Staff A, LPN stated the resident had gurgling in her throat and she had to leave the resident to retrieve suctioning supplies, call 911 and call the doctor. There was no other nurse assisting with the resident or helping the nurse with these tasks. Resident #1 was transferred to the hospital via Emergency Medical Services. In the emergency department the resident was on 8 L (liters) of oxygen to keep her saturation at 94%. She was admitted with diagnoses including acute respiratory failure with hypoxia, aspiration pneumonia/healthcare-associated pneumonia, and severe sepsis requiring IV (intravenous) hydration.
Nurses from the 3:00 p.m. to 11:00 p.m. shift on Friday, 2/17/23 left the facility or their assignment without giving report or doing a narcotic count on the medication cart with a relieving nurse. The medication cart keys were left in the cart for the oncoming.
This failure created a situation that resulted in the likelihood of serious injury or harm to Resident #1 and abandonment of 57 residents and resulted in the determination of Immediate Jeopardy on 2/17/23. The findings of Immediate Jeopardy were determined to be removed on 2/23/23 at 11:45 a.m. and the scope and severity was reduced to a D.
Findings included:
Review of the Nursing Home Administrator Job Description provided by the facility revealed, Reports to: Regional [NAME] President, Summary of Position: The Nursing Home Administrator as a member of the Board of Managers of Operator is responsible for the Facility Quality Assurance Performance Improvement (QAPI) for all aspects of the Facility including but not limited to; establishing and implementing policies and procedures, quality of care, quality of life, regulatory compliance, compliance/ethics, business development and financial stewardship. Essential Duties and Responsibilities (To be completed without harming or injuring the resident/patient, co-worker, self, or others):
Leads the facility Ethics and Compliance Program, acting as the Ethics and Compliance officer.
Enacts, implements and enforces the facility policies regarding the management and operation of the facility.
Analyzes financial, quality of care, quality of life, business development, compliance, regulatory and other management reports to determine the appropriate management interventions needed then implements the interventions resulting in improved outcomes.
Implements facility communications to ensure that employees, residents and families are well informed regarding issues affecting them.
Acts as the facility Privacy Officer in evaluating and confirming HIPAA compliance activities.
Establishes a culture of resident choice and right to fair and equitable treatment, self-determination, individuality, privacy, property, and civil rights, including the right to lodge a complaint.
Provides supervision either directly or indirectly to all facility employees including the selection, hiring, orientation, training and coaching of employees.
Identifies facility needs or issues and obtains consulting assistance, as needed, in the root-cause analysis, recommendation for improvement, education assistance or monitoring.
Other duties as assigned.
Board of Managers
Responsible establishing and implementing policies regarding the operation of the facility.
Responsible and accountable for the QAPI program.
Responsible for reporting to the Board of Manages [sic] on a quarterly basis and as needed results of the operation including but not limited to Ethics, Survey and Certification, Financial, Staffing and Recognition.
Review of the Nursing Home Administrator Job Description provided by the facility revealed, Reports to: Nursing Home Administrator, Summary of Position: The Director of Nursing as a member of the Board of Managers of Operator is responsible for developing, organizing, evaluating and administering patient care programs and services of the Center. The DON has twenty-four (24) hour responsibility for the overall delivery of nursing services and ensures the implementation of all clinical policies and procedures.
Essential Duties and Responsibilities (To be completed without harming or injuring the resident/patient, co-worker, self, or others):
Leads, organizes, evaluates and manages nursing and clinical personnel through sound management practices and delegation.
Makes daily patient rounds with the appropriate manager/supervisor(s) to note resident/patient condition and to ensure nursing personnel are performing their work assignments in accordance with acceptable nursing standards.
Ensures that each resident's right to fair and equitable treatment, self-determination, individuality, privacy, property, and civil rights, including the right to lodge a complaint, are strictly enforced.
Ensures compliance with applicable local, state, federal and other regulatory agencies and quality assurance standards, certifications and licensure requirements.
Participates in the clinical admission process
Attends regularly conducted staff meetings and participates regularly in continuing education training programs.
Handles on-call responsibilities as required.
Accountable for adherence by staff to policies, procedures and standards; delivery and proper documentation of patient care. Leads and manages the General and Restorative Nursing Services on a 24 hour basis to ensure the delivery of high quality comprehensive patient care.
Assures directly or through delegation, the current licensure status and employee records of all RNs and LPNs and other licensed clinical personnel reporting to this position.
Continually works to assure compliance with all applicable State and Federal regulations.
Performs duties as defined by the State Nurse Practice Act and other regulatory agencies.
Assures adequate staffing of the facility on a 24-hour basis.
Leads and participates in Quality Improvement activities to improve facility services.
Other duties as assigned.
Review of the Staffing Coordinator Job Description provided by the facility revealed, reports to: (DON), Summary of Position: The Staffing Coordinator is responsible for maintain [sic] the daily scheduling and coordination of Facility Staff, as well as preparing reports and projects related to scheduling and staffing. Essential Duties and Responsibilities (To be completed without harming or injuring the resident/patient, co-worker, self, or others):
Confirms and verifies staffing schedules for the nursing departments.
Communicates and assists in resolving staffing concerns timely.
Maintain a current listing of current employee phone numbers.
Maintain daily tardies and absenteeism and communicates to the DON in accordance to the attendance policy.
Reviews staffing levels as needed on a daily basis.
Call staff to work open or available shifts as required.
Assists in completion and filing of designated reports in accordance with established policies and procedures.
Takes incoming facility staffing calls from employees.
Consults with leadership concerning the staffing needs.
Communicates written or verbal, reports to the DON and/or Administrator concerning staffing and schedules.
Develops and maintains a working relationship with employees and management.
May assist facility recruiting function.
Ensures administrative functions are carried out promptly.
Complies with all laws and regulations.
Other duties as assigned.
A review of physician orders for Resident #1 revealed the order: Midodrine HCL 15 mg (milligrams) by mouth three times a day for blood pressure. Hold for SBP (systolic blood pressure) above 140, dated 1/16/23.
A review of Resident #1's medical records revealed a care plan in place for Cardiovascular problem related to hypotension, revised on 7/8/22. Interventions included: administer medication as ordered, vital signs as ordered, observe for changes in heart rate, observe for signs and symptoms of hypotension, observe for changes in respiratory rate and pattern, and observe for presence or absence of chest pain, precipitating factors, level, method of relief and effectiveness.
A review of the electronic Medication Administration Record (eMAR) and Vital Sign section of the electronic record showed the following blood pressure readings:
2/1/23 at 6:51 a.m.- 111/54
2/2/23 to 2/10/23- no documented blood pressures
2/11/23 at 7:58 a.m.- 107/56
2/12/23 to 2/17/23 - no documented blood pressures
2/18/23 at 2:00 a.m.- 58/42
Resident #1 was administered Midodrine at 2:00 p.m. and 9:00 p.m. on 2/17/23.
An interview was conducted with Staff A, LPN on 2/20/23 at 7:20 a.m. Staff A, LPN stated a blood pressure should always be checked prior to administering Midodrine to a resident.
An interview was conducted with the DON on 2/20/23 at 8:12 a.m. regarding Midodrine administration. The DON stated blood pressure should be taken prior to each administration of Midodrine. She confirmed it would need to be taken to ensure the resident's blood pressure was in the parameters of the order. The DON was observed reviewing Resident #1's medical record and she confirmed no blood pressure had been documented under vital signs or on the eMAR since 2/11/23. Upon review of the order, the DON stated there was an error when the order was entered in the computer and the button was not selected to trigger the blood pressure to be entered.
An information sheet provided by the distributor of Midodrine HCL tablets, indicated, the supine and standing blood pressure should be monitored regularly, and the administration of midodrine hydrochloride tablets should be stopped if supine blood pressure increases excessively.
(https://www.parpharm.com/products/Midodrine-HCl-Tablets-2.5mg/)
An interview was conducted with Staff S, LPN. He stated Resident #1 had a suction machine in her room, but he did not know about supplies because he never had to use it with the resident. When asked to show where suction supplies, such as thin flexible suction catheters, yankauer suction tips, and suction tubing, were kept, he went first to the medication room and was unable to find them. He then went to the storage room and located a tracheostomy clean and care kit, tube holders and inner cannulas in an upper cabinet behind the door. On a shelf behind the door there was a bin labeled suction connecting and yankauer, containing suction cannisters but no yankauer suction tips. The shelf near the bin had suction connection tubing. Staff S, LPN said that is what connects to the suction machine and then the suction catheter that is being used. (Photographic evidence obtained.) He said he did not see any thin flexible suction tubing.
On 2/22/23 at 11:20 a.m. another tour was taken of the storage room on the 600 hall. A Suction Catheter Tray with Chimney Valve was found in the upper cabinet behind the door. (Photographic evidence obtained.)
An interview was conducted with Staff T, RN on 2/22/23 at 11:22 a.m. Staff T, RN observed the Suction Catheter Tray with Chimney Valve and confirmed that it was a thin flexible suction catheter. She said that or the yankauer can be used with the suction machines in the facility. She stated it can be used for any resident with or without a tracheostomy (an opening in the windpipe that provides an alternate airway) to suction secretions from a resident.
A review of the 200, 400, and 800 hall medication cart Controlled Drug Shift Audit sheet (a record of narcotic counts completed and signed off by nurses at each shift change) revealed Staff F, LPN signed off her own narcotic audit without counting with a relieving nurse for the 400 hall medication cart on 2/17/2023 at 11: p.m. It showed the 200 and 800 hall medication cart narcotic audits were signed off by Staff B, RN/UM, who did not come in until approximately 2:00 a.m. on 2/18/23.
An interview was conducted with Staff B, RN/UM on 2/22/23 at 12:55 p.m. Staff B, RN/UM reviewed the Controlled Drug Shift Audit for the 200, 400, and 800 halls. She confirmed it was her signature signing off the narcotic audit for the Friday 2/17/23 11:00 p.m. to Saturday 2/18/23 7:00 a.m. shift. She said when she arrived at the facility just before 2:00 a.m. on 2/18/23, she did not complete a narcotic count or report with another nurse leaving their shift. Staff B, RN/UM said she counted the carts herself and the keys had been left by the previous nurse stuffed in the cart. Staff B, RN/UM said the 400 hall medication cart Controlled Drug Shift Audit was signed by Staff F, LPN coming on her shift at 3:00 p.m. on 2/17/23 and leaving her shift at 11:00 p.m. on 2/17/23. She confirmed there was not a second nurses' signature. Staff B, RN/UM confirmed medication cart keys should not be left in the medication carts, nurses should get report and keys from the previous nurse. She was unsure of who signed as the nurse leaving the shift on 2/17/23 at 11:00 p.m. due to the signatures being illegible.
The NHA and DON stated they were unsure who signed off the Controlled Drug Shift Audit sheets for the 200 and 800 hall leaving the 3:00 to 11:00 shift on 2/17/23, they could not read the signatures.
A review of the Nurse Daily Sign-in for 2/17/23 for the 3:00 p.m. to 11:00 p.m. shift showed Staff F, LPN was scheduled for the 400 hall, Staff D, LPN, was scheduled for the 600 hall and Staff E, LPN was scheduled for the 800 hall. Available was listed next to the 200 hall.
On 2/19/23 at 9:00 a.m. an interview was conducted with Staff E, LPN. He said he left the facility around 12:30 a.m. on 2/18/23. He said he was finishing his charting after his shift ended at 11:00 p.m. He said when he left Staff A, LPN was on the 500, 600, and 700 hall and Staff D, LPN and Staff F, LPN were still in the facility. He said Staff D, LPN was just charting and Staff F, LPN was just waiting.
An interview was conducted with the DON and the Regional [NAME] President at 2/22/23 at 1:23 p.m. When told staff have stated thin flexible suction catheters were used in the facility, one was found in the storage room, and the facility policy listed thin catheters as an option for suctioning, she said, I was just telling you what I would use. Regarding nurses leaving their shift, the DON said the nurses should be doing a narcotic count with an on-coming nurse and give medication cart keys directly to that person before leaving. The Regional [NAME] President said no nurse is allowed to leave until their replacement arrives, they should do a narcotic count, give report, and do walking rounds.
When asking if they considered it abandonment when the nurses from the 2/17/23 3:00 p.m. to 11:00 p.m. shift left without giving report and turning over their medication cart keys to another nurse, the Regional [NAME] President stated, yes, we were able to identify that as an issue in our investigation. He stated the facility would be reporting abandonment and neglect on at least one nurse and possibly more.
A review of Resident #1's SBAR (Situation Background Assessment Recommendation) Communication Form, dated 2/18/23 at 2:09 a.m. and signed by Staff A, LPN revealed that Resident #1's vital signs were: blood pressure 58/42, respirations 28, pulse 136, and oxygen saturation 71% and blood sugar 224. The Resident Evaluation showed the resident had swallowing difficulty, labored or rapid breathing, and a non-productive cough.
A review of the SNF/NF (Skilled Nursing Facility/Nursing Facility) to Hospital Transfer Form for Resident #1, dated 2/18/23 2:09 a.m., and signed by Staff A, LPN was reviewed. The form showed Staff A, LPN gave report by phone to the emergency room Charge Nurse on 2/18/23 at 2:43 a.m. The Hospital Transfer Form showed Resident #1 was totally dependent for bathing, dressing, toileting, transfers, and eating, incontinent of bowel and bladder, non-ambulatory, and had risk alerts for aspiration, high fall risk, needs medications crushed, pressure ulcers/injuries, seizures and swallowing precautions.
A review of the (local) County Fire Rescue run report showed the 911 call from the facility was received on 2/18/23 at 1:47 a.m. Emergency Medical Services (EMS) arrived on scene at 1:55 a.m. and departed the facility at 2:02 a.m. The run report revealed, Pt [patient] appears to be mentally disabled. Pt has audible congestion in her airway and staff stated that the pt does not have CHF [congestive heart failure], Pt was sheeted onto our stretcher and strapped on then loaded into R42[ambulance]. Pt vitals and info were gathered. Pt lung sounds are fairly clear on the right with some rhonchi, and pts lung sounds are diminished on the lefts side. Pts congestion sounds to be in the upper respiratory tract. Pt was sat up straight and was administered 10 LPM [liters per minute] of O2 [oxygen] via NRM [non re-breather mask], 4-lead EKG performed. IV was established in pts left hand. Pt BS [blood sugar] is 116. 12-Lead EKG performed. Pt O2 SAT [oxygen saturation] has improved. Pt was examined, no obvious injuries were noted. Pts mentation has remained the same. Pt was trans [transported] to the ER [emergency room] without incident, pt care and info turned over to ER staff.
A review of the Emergency Department Documents for Resident #1, dated 2/18/23, showed Patient is a 61 years [sic] old female presenting with a complaint of shortness of breath today with hypoxia. The patient has an extensive medical history and is at this skilled nursing facility mainly because she has Down Syndrome and developmental delay. The report was at baseline the patient has very limited verbal ability and cannot tell you how she is feeling if she feels sick. The EMS at the facility also noted that the patient had a fever. There is [sic] been no note vomiting or diarrhea, no rash, the patient has reportedly had a cough today. The documents noted: The patient is currently with continued hypoxia in the emergency department. The patient is now on 8 L (liters) of oxygen to keep her saturation at 94%. The patient remains with some tachycardia and some tachypnea due to the illness. The patient has been started on antibiotics with cefepime and vancomycin to cover for the urinary tract infection as well as healthcare acquired pneumonia. At this point the patient does not have clinical evidence of severe sepsis. Plan to have the patient admitted to [primary provider] service for continued evaluation and treatment.
A review of the hospital History and Physical (H & P) completed by Resident #1's physician on 2/18/23 at 11:26 a.m. revealed she was admitted to the hospital for shortness of breath and altered mental status. The H & P showed She was brought in yesterday as reported indicated that she was having worsening shortness of breath and hypoxia. The H & P Assessment showed the following:
1. Acute respiratory failure with hypoxia, present on admission.
2. Aspiration pneumonia/healthcare-associated pneumonia.
3. Severe sepsis requiring IV hydration.
5. Functional quadriplegia.
6. Dysphagia.
7. Down syndrome.
8. Coronavirus A infection.
An interview was conducted with Staff C, CNA on 2/21/23 at 7:25 a.m. Staff C, CNA confirmed she was the CNA taking care of Resident #1 on the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift. She stated there was no nurse assigned to the 800 hall, where Resident #1 resided, and there was only one nurse working on the floor in the facility. Staff C, CNA said she checked on Resident #1 and she did not look ok. She said she went out to the hall and yelled for Staff A, LPN, the only nurse working, to come help. Staff C, CNA said she took Resident #1's vital signs and they were not good. She stated Staff A, LPN came and quickly assessed the resident, then went to call 911 and get suction equipment while Staff C, CNA stayed with the resident. She stated Staff A, LPN returned to the room and couldn't find the thin suction tubing she needed to suction the resident. Staff C, CNA said she then went out and looked for the suction supplies. She said all they could find was a yankauer for the LPN to use. Staff C, CNA said the nurses had used the thin flexible suction in the facility before and she didn't understand why it wasn't replaced. She stated no one else came to assist her and Staff A, LPN with the resident. She added that Staff D, LPN who was in the building charting was going out the door. Staff C, CNA stated staffing is always an issue and it is concerning. She added there have been nights where there were only two CNAs for the entire facility (she was unable to recall dates.) Staff C, CNA said, something bad is going to happen.
An interview was conducted with Staff A, Licensed Practical Nurse (LPN) on 2/19/23 at 5:24 a.m. Staff A, LPN stated there are staffing and scheduling issues in the facility. She said sometimes people are on the schedule that are not supposed to be. She added there is no master schedule, staff do not get a copy of their schedules and they must come in to see when they are on the schedule to work. Staff A, LPN stated as an example this past Wednesday was her day off, but she was on the schedule to work. She said there have been various nights shifts in the facility when there are only three to four Certified Nursing Assistants (CNA) working. Staff A, LPN said when the census is 115 residents, there should be three nurses on the floor, but on Friday night, 2/17/23 11 p.m. to 2/18/23 7 a.m., she was the only nurse on the floor for a few hours. She stated one nurse on the schedule wasn't confirmed and the Director of Nursing (DON) cancelled two other nurses that were scheduled to work. Staff A, LPN reported when she saw texts the nurses were not coming in, she called the on-call nurse, Staff B, Registered Nurse (RN)/Unit Manager (UM,) and received no response. Staff A, LPN said one of the 3-11 p.m. nurses stayed over until that nurse completed her charting. She reiterated that she was left as the only nurse working in the facility for a few hours. She said she again contacted the on-call nurse, and that person contacted the DON. The on-call nurse, Staff B, RN/UM, came in to the facility at approximately 2:00 a.m. Staff A, LPN stated she was trying to send a resident out to the hospital due to respiratory distress while she was the only nurse covering residents. During the interview Staff A, LPN's text messages and call log were observed on her cell phone and showed she sent a text message to the on-call nurse at 11:32 p.m., a call to the on-call nurse at 11:42 p.m. and a call to the on-call nurse at midnight. The on-call nurse called Staff A, LPN's cell phone at 1:02 a.m. Staff A, LPN added there were only four CNAs in the facility that shift and some residents were unable to have their briefs changed and had to wait until the next morning.
A follow-up interview was conducted with Staff A, LPN on 2/19/23 at 7:23 a.m. regarding the resident she sent to the hospital on the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift. Staff A, LPN stated she had to send Resident #1 to the hospital via Emergency Medical Services (EMS) around 1:30 a.m. She stated the resident was gurgling in her throat, but she was unable to find the suction tubing she needed to suction the resident's throat area. Staff A, LPN said she had a suction canister but was unable to locate the larger tube that attached to the suction and could not find the small flexible tubing to suction the resident's throat. She said she was able to use a yankauer (a medical suction device that is a rigid plastic with a large opening for suctioning) to suction the resident's mouth. She said she was alone and did what she could.
A review of admission records showed Resident #1 was initially admitted on [DATE] and was re-admitted on [DATE] with diagnoses including pneumonitis due to inhalation of food and vomit, bronchiectasis, interstitial pulmonary disease, dysphagia, obstructive and reflux uropathy, epilepsy, down syndrome, and functional quadriplegia.
A review of Resident #1's care plan showed a care plan for Aspiration Risk, dated 5/18/22. The focus of the care plan The resident is at risk for aspiration related to difficulty swallowing because of: Diagnosis of dysphagia. History of aspiration pneumonia. Interventions included: observe for signs and symptoms of aspiration: coughing, tearing, runny nose, wet vocal tone, difficulty breathing, pocketing food. A care plan for Cognition, revised on 6/6/22, showed the resident has impaired cognitive function or impaired thought processes related to intellectual disability (Down syndrome.) The resident is not able to make concrete needs known and dose not follow commands. Interventions included: Report to nurse any changes in cognitive function, specifically changes in: decision making ability, memory, recall, awareness of surroundings and others, difficulty expressing self, difficulty understanding others, sleepiness/lethargy, confusion. A care plan, revised 1/16/23, in place for ADL (Activities of Daily Living) Self-care performance deficit due to impaired cognition, impaired mobility, and generalized weakness. Interventions included: Resident is totally dependent upon staff for ADLs. Encourage to participate at highest functional ability, anticipate needs, bathing: the resident requires the assist of two, and transfer is total mechanical lift to chair. A care plan in place for emphysema/COPD (Chronic obstructive pulmonary disease), dated 3/21/22. The interventions included: monitor for difficulty breathing (dyspnea) on exertion and remind resident not to push beyond endurance, monitor for signs and symptoms of acute respiratory insufficiency: anxiety, confusion, restlessness, shortness of breath (SOB) at rest, cyanosis, somnolence, monitor/document/report to doctor as needed any signs and symptoms of respiratory infection: fever, chills, increase in sputum, chest pain, increased difficulty breathing, increased coughing or wheezing.
A review of Resident #1's tasks show the resident was scheduled to receive showers every Tuesday and Friday on the 3:00-11:00 p.m. shift. From February 1st-Febuary 17th, the resident received five bed baths and no showers. From January 1st-January 31st (not counting days resident was out of the facility), the resident had eight scheduled shower days. Of those eight shower days, two were partial baths and six were bed baths. The resident had no showers from January 1-Febuary 17, 2023.
A review of progress notes showed Resident #1 was sent to the hospital on 1/11/23 and returned to the facility on 1/16/23 with a diagnosis of pneumonia and urinary tract infection (UTI.) A review of Resident #1's provider notes, dated 1/24/23, revealed she was seen at the facility to evaluate post hosp [hospital] PNA [pneumonia], UTI [urinary tract infection], g-tube accidently pulled ithout [sic] complication, will leave out per family request, complex UTI, siezure [sic] like activity hypotyriod [sic], PNA, and adjusting medication, anxiety, dermatitis, candida, around peg tube improving elevated ammonia level, BUN 45, UA [urinalysis] positive, hypotensive post hospitalization, monitoring of patient multiple comorbidities, evaluation of new developments medication reconciled and care coordination. The provider notes revealed the resident is at increase risk for rehospitalization, due to safety issues, infection, development of DVTs [Deep Vein thrombosis] and pulmonary embolism and the resident was needing frequent monitoring due to the complexity of chronic disease.
On 2/22/23 at 9:35 a.m. a family member/guardian for Resident #1 was interviewed. The family member stated sometimes there is only one CNA working two halls in the facility. She said you can press the call light and they don't answer. She said medications are late. She said she complains to administration all the time and nothing is done. The family member stated she was called at 2:00 a.m. Friday morning (2/18/23) and told Resident #1 was going to the hospital. She said she was told they couldn't suction the resident because there was no RN. She stated the resident had phlegm in her throat for the two days prior to going to the hospital. She felt like the resident needed suctioning during those two days.
On 2/17/23 at 11:00 p.m. the facility census was 114 according to the Director of Nursing (DON), on 2/19/23 the facility had a census of 113.
Review of the Facility Assessment, dated 9/30/22, indicated the following staffing patterns:
Night shift: 0 nurse leaders, 1 RN, 2 LPNs, 6 CNAs
The Facility Assessment does not relate the staffing patterns to the acuity level of the residents.
According to the Resident Census and Conditions of Residents, CMS (Centers for Medicare and Medicaid Services) - 672, completed and signed by the DON on 2/19/23, the following conditions represented the facility population on that day:
8 residents on Hospice Care
5 residents receiving Intravenous (IV) therapy, IV nutrition, and/or blood transfusion,
9 residents receiving respiratory treatment.
1 resident receiving ostomy care.
11 residents receiving tube feedings.
1 resident with an Intellectual and/or developmental disability.
50 residents with documented psychiatric diagnosis (exclude dementias and depression.)
43 residents with dementia
3 residents with behavioral healthcare needs
109 residents that are occasionally or frequently incontinent of bladder.
98 residents that are occasionally or frequently incontinent of bowel.
Of the current 113 residents 31 were dependent on staff for toilet use and 82 need one or two staff to assist.
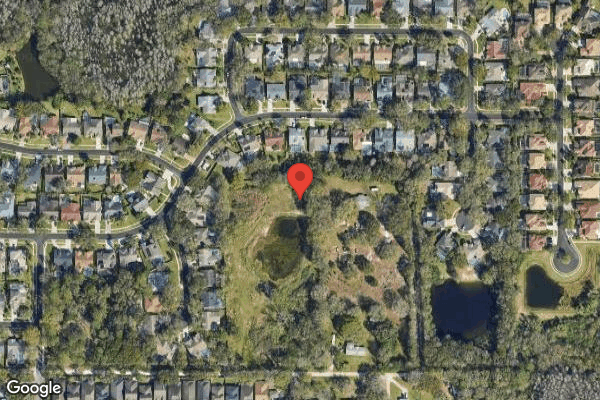
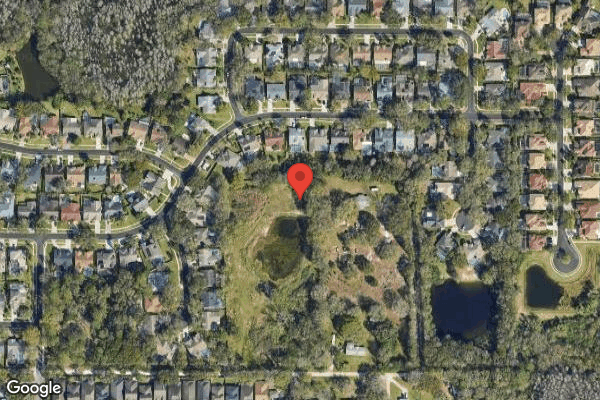
The facility consisted of a front and back unit with two nurses' stations in the middle. Six hallways join at the nurses' stations like the spokes of a wheel. The 200, 400, and 800 halls are the front unit, and the 500, 600 and 700 halls the back unit. Copy of facility floor plan obtained.
The facility used a Nurse Daily Sign-in sheet, located in a staffing book at the nurses' station; the sheet listed which RNs, LPNs, and CNAs were assigned to work each shift and what their assigned halls will be. Staff members initialed next to[TRUNCATED]
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility neglected to monitor blood pressure for one resident (#1) of ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility neglected to monitor blood pressure for one resident (#1) of three residents sampled taking blood pressure medication, the facility staff neglected to carry out change of shift duties in manner to provide care and ensure nursing staff and equipment were available for residents on the 200, 400, and 800 halls including one resident (#1) that experienced respiratory distress. They neglected to provide ADL (activities of daily living) care to three out of three residents (#1, 5, and 6) sampled out of 49 residents dependent on staff for showers.
On 2/17/23 at 11:00 p.m. Staff A, Licensed Practical Nurse (LPN) was the only nurse working on the floor, with a census of 114 residents, for approximately three hours. Staff D, LPN was in the building until 1:46 a.m., however, she was only waiting and had no resident assignment. Staff A, LPN was assigned 57 residents total on the 500, 600, and 700 halls. The 57 residents total on the 200, 400, and 800 halls had no nurse assigned to them. Resident #1 resided on the 800 hall, with no nurse assigned to her. At approximately 1:45 a.m. Resident #1's CNA noticed the resident was not well and called for Staff A, LPN to come help. At that time Resident #1's blood pressure was 58/42, respirations 28, pulse 136, and oxygen saturation 71%. Staff A, LPN stated the resident had gurgling in her throat and she had to leave the resident to retrieve suctioning supplies, call 911 and call the doctor. There was no other nurse assisting with the resident or help the nurse with these tasks. Resident #1 was transferred to the hospital via Emergency Medical Services. In the emergency department the resident was on 8 L (liters) of oxygen to keep her saturation at 94%. She was admitted with diagnoses including acute respiratory failure with hypoxia, aspiration pneumonia/healthcare-associated pneumonia, and severe sepsis requiring IV (intravenous) hydration.
Nurses from the 3:00 p.m. to 11:00 p.m. shift on Friday, 2/17/23 left the facility and/or their assignment without giving report or doing a narcotic count on the medication cart with a relieving nurse. The medication cart keys were left in the cart for the oncoming nurse.
These failures created a situation that resulted in the likelihood of serious injury or harm to Resident #1 and abandonment of 57 resident and resulted in the determination of Immediate Jeopardy on 2/17/23. The findings of Immediate Jeopardy were determined to be removed on 2/23/23 at 11:45 a.m. and the scope and severity was reduced to a E.
Findings included:
A review of physician orders for Resident #1 revealed the order: Midodrine HCL 15 mg (milligrams) by mouth three times a day for blood pressure. Hold for SBP (systolic blood pressure) above 140, dated 1/16/23.
A review of Resident #1's medical records revealed a care plan in place for Cardiovascular problem related to hypotension, revised on 7/8/22. Interventions included: administer medication as ordered, vital signs as ordered, observe for changes in heart rate, observe for signs and symptoms of hypotension, observe for changes in respiratory rate and pattern, and observe for presence or absence of chest pain, precipitating factors, level, method of relief and effectiveness.
A review of the electronic Medication Administration Record (eMAR) and Vital Sign section of the electronic record showed the following blood pressure readings:
2/1/23 at 6:51 a.m.- 111/54
2/2/23 to 2/10/23- no documented blood pressures
2/11/23 at 7:58 a.m.- 107/56
2/12/23 to 2/17/23 - no documented blood pressures
2/18/23 at 2:00 a.m.- 58/42
Resident #1 was administered Midodrine at 2:00 p.m. and 9:00 p.m. on 2/17/23.
An interview was conducted with Staff A, LPN on 2/20/23 at 7:20 a.m. Staff A, LPN stated a blood pressure should always be checked prior to administering Midodrine to a resident.
An interview was conducted with the Director of Nurses (DON) on 2/20/23 at 8:12 a.m. regarding Midodrine administration. The DON stated blood pressure should be taken prior to each administration of Midodrine. She confirmed it would need to be taken to ensure the resident's blood pressure was in the parameters of the order. The DON was observed reviewing Resident #1's medical record and she confirmed no blood pressure had been documented under vital signs or on the eMAR since 2/11/23. Upon review of the order, the DON stated there was an error when the order was entered in the computer and the button was not selected to trigger the blood pressure to be entered.
An information sheet provided by the distributor of Midodrine HCL tablets, indicated, the supine and standing blood pressure should be monitored regularly, and the administration of midodrine hydrochloride tablets should be stopped if supine blood pressure increases excessively.
(https://www.parpharm.com/products/Midodrine-HCl-Tablets-2.5mg/)
An interview was conducted with Staff S, LPN. He stated Resident #1 had a suction machine in her room, but he did not know about supplies because he never had to use it with the resident. When asked to show where suction supplies, such as thin flexible suction catheters, yankauer suction tips, and suction tubing, were kept, he went first to the medication room and was unable to find them. He then went to the storage room and located a tracheostomy clean and care kit, tube holders and inner cannulas in an upper cabinet behind the door. On a shelf behind the door there was a bin labeled suction connecting and yankauer, containing suction cannisters but no yankauer suction tips. The shelf near the bin had suction connection tubing. Staff S, LPN said that is what connects to the suction machine and then the suction catheter that is being used. (Photographic evidence obtained.) He said he did not see any thin flexible suction tubing.
On 2/22/23 at 11:20 a.m. another tour was taken of the storage room on the 600 hall. A Suction Catheter Tray with Chimney Valve was found in the upper cabinet behind the door. (Photographic evidence obtained.)
An interview was conducted with Staff T, RN on 2/22/23 at 11:22 a.m. Staff T, RN observed the Suction Catheter Tray with Chimney Valve and confirmed that it was a thin flexible suction catheter. She said that or the yankauer can be used with the suction machines in the facility. She stated it can be used for any resident with or without a tracheostomy (an opening in the windpipe that provides an alternate airway) to suction secretions from a resident.
A review of the 200, 400, and 800 hall medication cart Controlled Drug Shift Audit sheet (a record of narcotic counts completed and signed off by nurses at each shift change) revealed Staff F, LPN signed off her own narcotic audit without counting with a relieving nurse for the 400 hall medication cart on 2/17/2023 at 11: p.m. It showed the 200 and 800 hall medication cart narcotic audits were signed off by Staff B, RN/UM, who did not come in until approximately 2:00 a.m. on 2/18/23.
An interview was conducted with Staff B, RN/UM on 2/22/23 at 12:55 p.m. Staff B, RN/UM reviewed the Controlled Drug Shift Audit for the 200, 400, and 800 halls. She confirmed it was her signature signing off the narcotic audit for the Friday 2/17/23 11:00 p.m. to Saturday 2/18/23 7:00 a.m. shift. She said when she arrived at the facility just before 2:00 a.m. on 2/18/23, she did not complete a narcotic count or report with another nurse leaving their shift. Staff B, RN/UM said she counted the carts herself and the keys had been left by the previous nurse stuffed in the cart. Staff B, RN/UM said the 400 hall medication cart Controlled Drug Shift Audit was signed by Staff F, LPN coming on her shift at 3:00 p.m. on 2/17/23 and leaving her shift at 11:00 p.m. on 2/17/23. She confirmed there was not a second nurses' signature. Staff B, RN/UM confirmed medication cart keys should not be left in the medication carts, nurses should get report and keys from the previous nurse. She was unsure of who signed as the nurse leaving the shift on 2/17/23 at 11:00 p.m. due to the signatures being illegible.
The NHA and DON stated they were unsure who signed off the Controlled Drug Shift Audit sheets for the 200 and 800 hall leaving the 3:00 to 11:00 shift on 2/17/23, they could not read the signatures.
A review of the Nurse Daily Sign-in for 2/17/23 for the 3:00 p.m. to 11:00 p.m. shift showed Staff F, LPN was scheduled for the 400 hall, Staff D, LPN, was scheduled for the 600 hall and Staff E, LPN was scheduled for the 800 hall. Available was listed next to the 200 hall.
On 2/19/23 at 9:00 a.m. an interview was conducted with Staff E, LPN. He said he left the facility around 12:30 a.m. on 2/18/23. He said he was finishing his charting after his shift ended at 11:00 p.m. He said when he left Staff A, LPN was on the 500, 600, and 700 hall and Staff D, LPN and Staff F, LPN were still in the facility. He said Staff D, LPN was just charting and Staff F, LPN was just waiting.
An interview was conducted with the DON and the Regional [NAME] President at 2/22/23 at 1:23 p.m. When told staff have stated thin flexible suction catheters were used in the facility, one was found in the storage room, and the facility policy listed thin catheters as an option for suctioning, she said, I was just telling you what I would use. Regarding nurses leaving their shift, the DON said the nurses should be doing a narcotic count with an on-coming nurse and give medication cart keys directly to that person before leaving. The Regional [NAME] President said no nurse is allowed to leave until their replacement arrives, they should do a narcotic count, give report, and do walking rounds.
When asking if they considered it abandonment when the nurses from the 2/17/23 3:00 p.m. to 11:00 p.m. shift left without giving report and turning over their medication cart keys to another nurse, the Regional [NAME] President stated, yes, we were able to identify that as an issue in our investigation. He stated the facility would be reporting abandonment and neglect on at least one nurse and possibly more.
1.
A review of Resident #1's SBAR (Situation Background Assessment Recommendation) Communication Form, dated 2/18/23 at 2:09 a.m. and signed by Staff A, LPN revealed that Resident #1's vital signs were: blood pressure 58/42, respirations 28, pulse 136, and oxygen saturation 71% and blood sugar 224. The Resident Evaluation showed the resident had swallowing difficulty, labored or rapid breathing, and a non-productive cough.
A review of the SNF/NF (Skilled Nursing Facility/Nursing Facility) to Hospital Transfer Form for Resident #1, dated 2/18/23 2:09 a.m., and signed by Staff A, LPN was reviewed. The form showed Staff A, LPN gave report by phone to the emergency room Charge Nurse on 2/18/23 at 2:43 a.m. The Hospital Transfer Form showed Resident #1 was totally dependent for bathing, dressing, toileting, transfers, and eating, incontinent of bowel and bladder, non-ambulatory, and had risk alerts for aspiration, high fall risk, needs medications crushed, pressure ulcers/injuries, seizures and swallowing precautions.
A review of the (local) County Fire Rescue run report showed the 911 call from the facility was received on 2/18/23 at 1:47 a.m. Emergency Medical Services (EMS) arrived on scene at 1:55 a.m. and departed the facility at 2:02 a.m. The run report revealed, Pt [patient] appears to be mentally disabled. Pt has audible congestion in her airway and staff stated that the pt does not have CHF [congestive heart failure], Pt was sheeted onto our stretcher and strapped on then loaded into R42 [ambulance]. Pt vitals and info were gathered. Pt lung sounds are fairly clear on the right with some rhonchi, and pts lung sounds are diminished on the lefts side. Pts congestion sounds to be in the upper respiratory tract. Pt was sat up straight and was administered 10 LPM [liters per minute] of O2 [oxygen] via NRM [non re-breather mask], 4-lead EKG performed. IV was established in pts left hand. Pt BS [blood sugar] is 116. 12-Lead EKG performed. Pt O2 SAT [oxygen saturation] has improved. Pt was examined, no obvious injuries were noted. Pts mentation has remained the same. Pt was trans [transported] to the ER [emergency room] without incident, pt care and info turned over to ER staff.
A review of the Emergency Department Documents for Resident #1, dated 2/18/23, showed Patient is a 61 years [sic] old female presenting with a complaint of shortness of breath today with hypoxia. The patient has an extensive medical history and is at this skilled nursing facility mainly because she has Down Syndrome and developmental delay. The report was at baseline the patient has very limited verbal ability and cannot tell you how she is feeling if she feels sick. The EMS at the facility also noted that the patient had a fever. There is [sic] been no note vomiting or diarrhea, no rash, the patient has reportedly had a cough today. The documents noted: The patient is currently with continued hypoxia in the emergency department. The patient is now on 8 L (liters) of oxygen to keep her saturation at 94%. The patient remains with some tachycardia and some tachypnea due to the illness. The patient has been started on antibiotics with cefepime and vancomycin to cover for the urinary tract infection as well as healthcare acquired pneumonia. At this point the patient does not have clinical evidence of severe sepsis. Plan to have the patient admitted to [primary provider] service for continued evaluation and treatment.
A review of the hospital History and Physical (H & P) completed by Resident #1's physician on 2/18/23 at 11:26 a.m. revealed she was admitted to the hospital for shortness of breath and altered mental status. The H & P showed She was brought in yesterday as reported indicated that she was having worsening shortness of breath and hypoxia. The H & P Assessment showed the following:
1. Acute respiratory failure with hypoxia, present on admission.
2. Aspiration pneumonia/healthcare-associated pneumonia.
3. Severe sepsis requiring IV hydration.
5. Functional quadriplegia.
6. Dysphagia.
7. Down syndrome.
8. Coronavirus A infection.
An interview was conducted with Staff C, CNA on 2/21/23 at 7:25 a.m. Staff C, CNA confirmed she was the CNA taking care of Resident #1 on the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift. She stated there was no nurse assigned to the 800 hall, where Resident #1 resided, and there was only one nurse working on the floor in the facility. Staff C, CNA said she checked on Resident #1 and she did not look ok. She said she went out to the hall and yelled for Staff A, LPN, the only nurse working, to come help. Staff C, CNA said she took Resident #1's vital signs and they were not good. She stated Staff A, LPN came and quickly assessed the resident, then went to call 911 and get suction equipment while Staff C, CNA stayed with the resident. She stated Staff A, LPN returned to the room and couldn't find the thin suction tubing she needed to suction the resident. Staff C, CNA said she then went out and looked for the suction supplies. She said all they could find was a yankauer for the LPN to use. Staff C, CNA said the nurses had used the thin flexible suction in the facility before and she didn't understand why it wasn't replaced. She stated no one else came to assist her and Staff A, LPN with the resident. She added that Staff D, LPN who was in the building charting was going out the door. Staff C, CNA stated staffing is always an issue and it is concerning. She added there have been nights where there were only two CNAs for the entire facility (she was unable to recall dates.) Staff C, CNA said, something bad is going to happen.
An interview was conducted with Staff A, Licensed Practical Nurse (LPN) on 2/19/23 at 5:24 a.m. Staff A, LPN stated there are staffing and scheduling issues in the facility. She said sometimes people are on the schedule that are not supposed to be. She added there is no master schedule, staff do not get a copy of their schedules and they must come in to see when they are on the schedule to work. Staff A, LPN stated as an example this past Wednesday was her day off, but she was on the schedule to work. She said there have been various nights shifts in the facility when there are only three to four Certified Nursing Assistants (CNA) working. Staff A, LPN said when the census is 115 residents, there should be three nurses on the floor, but on Friday night, 2/17/23 11 p.m. to 2/18/23 7 a.m., she was the only nurse on the floor for a few hours. She stated one nurse on the schedule wasn't confirmed and the Director of Nursing (DON) cancelled two other nurses that were scheduled to work. Staff A, LPN reported when she saw texts the nurses were not coming in, she called the on-call nurse, Staff B, Registered Nurse (RN)/Unit Manager (UM,) and received no response. Staff A, LPN said one of the 3-11 p.m. nurses stayed over until that nurse completed her charting. She reiterated that she was left as the only nurse working in the facility for a few hours. She said she again contacted the on-call nurse, and that person contacted the DON. The on-call nurse, Staff B, RN/UM, came in to the facility at approximately 2:00 a.m. Staff A, LPN stated she was trying to send a resident out to the hospital due to respiratory distress while she was the only nurse covering residents. During the interview Staff A, LPN's text messages and call log were observed on her cell phone and showed she sent a text message to the on-call nurse at 11:32 p.m., a call to the on-call nurse at 11:42 p.m. and a call to the on-call nurse at midnight. The on-call nurse called Staff A, LPN's cell phone at 1:02 a.m. Staff A, LPN added there were only four CNAs in the facility that shift and some residents were unable to have their briefs changed and had to wait until the next morning.
A follow-up interview was conducted with Staff A, LPN on 2/19/23 at 7:23 a.m. regarding the resident she sent to the hospital on the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift. Staff A, LPN stated she had to send Resident #1 to the hospital via Emergency Medical Services (EMS) around 1:30 a.m. She stated the resident was gurgling in her throat, but she was unable to find the suction tubing she needed to suction the resident's throat area. Staff A, LPN said she had a suction canister but was unable to locate the larger tube that attached to the suction and could not find the small flexible tubing to suction the resident's throat. She said she was able to use a yankauer (a medical suction device that is a rigid plastic with a large opening for suctioning) to suction the resident's mouth. She said she was alone and did what she could.
A review of admission records showed Resident #1 was initially admitted on [DATE] and was re-admitted on [DATE] with diagnoses including pneumonitis due to inhalation of food and vomit, bronchiectasis, interstitial pulmonary disease, dysphagia, obstructive and reflux uropathy, epilepsy, down syndrome, and functional quadriplegia.
A review of Resident #1's care plan showed a care plan for Aspiration Risk, dated 5/18/22. The focus of the care plan The resident is at risk for aspiration related to difficulty swallowing because of: Diagnosis of dysphagia. History of aspiration pneumonia. Interventions included: observe for signs and symptoms of aspiration: coughing, tearing, runny nose, wet vocal tone, difficulty breathing, pocketing food. A care plan for Cognition, revised on 6/6/22, showed the resident has impaired cognitive function or impaired thought processes related to intellectual disability (Down syndrome.) The resident is not able to make concrete needs known and does not follow commands. Interventions included: Report to nurse any changes in cognitive function, specifically changes in: decision making ability, memory, recall, awareness of surroundings and others, difficulty expressing self, difficulty understanding others, sleepiness/lethargy, confusion. A care plan, revised 1/16/23, in place for ADL (Activities of Daily Living) Self-care performance deficit due to impaired cognition, impaired mobility, and generalized weakness. Interventions included: Resident is totally dependent upon staff for ADLs. Encourage to participate at highest functional ability, anticipate needs, bathing: the resident requires the assist of two, and transfer is total mechanical lift to chair. A care plan in place for emphysema/COPD (Chronic obstructive pulmonary disease), dated 3/21/22. The interventions included: monitor for difficulty breathing (dyspnea) on exertion and remind resident not to push beyond endurance, monitor for signs and symptoms of acute respiratory insufficiency: anxiety, confusion, restlessness, shortness of breath (SOB) at rest, cyanosis, somnolence, monitor/document/report to doctor as needed any signs and symptoms of respiratory infection: fever, chills, increase in sputum, chest pain, increased difficulty breathing, increased coughing or wheezing.
A review of Resident #1's tasks show the resident was scheduled to receive showers every Tuesday and Friday on the 3:00-11:00 p.m. shift. From February 1st-Febuary 17th, the resident received five bed baths and no showers. From January 1st-January 31st (not counting days resident was out of the facility), the resident had eight scheduled shower days. Of those eight shower days, two were partial baths and six were bed baths. The resident had no showers from January 1-Febuary 17, 2023.
A review of progress notes showed Resident #1 was sent to the hospital on 1/11/23 and returned to the facility on 1/16/23 with a diagnosis of pneumonia and urinary tract infection (UTI.) A review of Resident #1's provider notes, dated 1/24/23, revealed she was seen at the facility to evaluate post hosp [hospital] PNA [pneumonia], UTI [urinary tract infection], g-tube accidently pulled ithout [sic] complication, will leave out per family request, complex UTI, siezure [sic] like activity hypotyriod [sic], PNA, and adjusting medication, anxiety, dermatitis, candida, around peg tube improving elevated ammonia level, BUN 45, UA [urinalysis] positive, hypotensive post hospitalization, monitoring of patient multiple comorbidities, evaluation of new developments medication reconciled and care coordination. The provider notes revealed the resident is at increase risk for rehospitalization, due to safety issues, infection, development of DVTs [Deep Vein thrombosis] and pulmonary embolism and the resident was needing frequent monitoring due to the complexity of chronic disease.
On 2/22/23 at 9:35 a.m. a family member/guardian for Resident #1 was interviewed. The family member stated sometimes there is only one CNA working two halls in the facility. She said you can press the call light and they don't answer. She said medications are late. She said she complains to administration all the time and nothing is done. The family member stated she was called at 2:00 a.m. Friday morning (2/18/23) and told Resident #1 was going to the hospital. She said she was told they couldn't suction the resident because there was no RN. She stated the resident had phlegm in her throat for the two days prior to going to the hospital. She felt like the resident needed suctioning during those two days.
On 2/17/23 at 11:00 p.m. the facility census was 114 according to the Director of Nursing (DON), on 2/19/23 the facility had a census of 113.
Review of the Facility Assessment, dated 9/30/22, indicated the following staffing patterns:
Night shift: 0 nurse leaders, 1 RN, 2 LPNs, 6 CNAs
The Facility Assessment does not relate the staffing patterns to the acuity level of the residents.
According to the Resident Census and Conditions of Residents, CMS (Centers for Medicare and Medicaid Services) - 672, completed and signed by the DON on 2/19/23, the following conditions represented the facility population on that day:
8 residents on Hospice Care
5 residents receiving Intravenous (IV) therapy, IV nutrition, and/or blood transfusion,
9 residents receiving respiratory treatment.
1 resident receiving ostomy care.
11 residents receiving tube feedings.
1 resident with an Intellectual and/or developmental disability.
50 residents with documented psychiatric diagnosis (exclude dementias and depression.)
43 residents with dementia
3 residents with behavioral healthcare needs
109 residents that are occasionally or frequently incontinent of bladder.
98 residents that are occasionally or frequently incontinent of bowel.
Of the current 113 residents 31 were dependent on staff for toilet use and 82 need one or two staff to assist.
The facility consisted of a front and back unit with two nurses' stations in the middle. Six hallways join at the nurses' stations like the spokes of a wheel. The 200, 400, and 800 halls are the front unit, and the 500, 600 and 700 halls the back unit. Copy of facility Floor Plan obtained.
The facility used a Nurse Daily Sign-in sheet, located in a staffing book at the nurses' station; the sheet listed which RNs, LPNs, and CNAs were assigned to work each shift and what their assigned halls will be. Staff members initialed next to their name when they came in for each shift. A review of the Nurse Daily Sign-in Sheet for the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift, showed the following nurses were scheduled: Staff A, LPN, Staff, I, RN, and Staff J, LPN. Written beside Staff J, LPN was a note, said he doesn't work wkends [sic]. The following CNAs were scheduled to work: Staff N, CNA, Staff O, CNA, Staff P, CNA, Staff C, CNA, and Staff Q, CNA. Staff Q, CNA had a line through her name with off written next to it, leaving only four CNAs working that shift. In the daily staffing book a loose sheet of paper was observed with a note, dated 2/17/23, from Staff M, CNA, tomorrow Sat. [DATE] is my regular day off. (W/E off) [weekends off] I never agreed to work. Staff M, CNA was scheduled to work from 3:00 p.m. to 11:00 p.m. on 2/18/23.
Review of the Nurse Daily Sign-in Sheet for Saturday, February 18, 2023, showed the resident census of 114 and four CNAs working on the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift, they were assigned on average 28 residents each.
Review of the Punch Detail Report for the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift revealed the time each staff member clocked in and out of the facility. Staff A, LPN clocked in at 11:04 p.m. on 2/17/23 and clocked out at 7:48 a.m. on 2/18/23, Staff F, LPN clocked out at 12:41 a.m. and Staff D, LPN clocked out at 1:46 a.m. Staff I, RN clocked in at 2:10 a.m. Staff B, RN/UM came in at approximately 1:45 a.m. to 2:00 a.m. (management does not clock-in).
Review of the Nurse Daily Sign-in sheet for Sunday February 19, 2023, revealed six CNAs scheduled to work the Saturday 2/18/23 11:00 p.m. to 2/19/23 7:00 a.m. shift. Two of the scheduled CNAs did not work that shift and one additional was added, leaving five CNAs working. With a resident census of 114; this gave each CNA on average 22 residents each. Being down one CNA, this left the available CNAs splitting the extra hallway. The assignments for that shift were as follows:
Staff N, CNA -one full hall plus rooms [ROOM NUMBERS]
Staff O, CNA- one full hall plus rooms [ROOM NUMBERS]
Staff R, CNA- one full hall plus room [ROOM NUMBER]
Staff G, CNA- one full hall plus rooms [ROOM NUMBERS]
Staff H, CNA- one full hall plus rooms [ROOM NUMBERS]
An interview was conducted with Staff I, RN on 2/19/23 at 5:50 a.m. Staff I, RN said she was scheduled to work the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift, but there was a miscommunication because she had requested off. She stated she came in around 2:00 a.m. She said there were two nurses in the building when she arrived. She also confirmed there were only four CNAs working that shift.
A Review of the Nurse Daily Sign-in for Saturday February 18, 2023, confirmed there were five CNAs scheduled for the Friday 2/17/23 11:00 p.m. to Saturday 2/18/23 7:00 a.m. shift and one of them was crossed out with off written by their name.
An interview was conducted with Staff I, RN on 2/19/23 at 5:52 a.m. Staff I, RN said one CNA did not show up for the current shift (2/18/23 11:00 p.m. to 2/19/23 7:00 a.m.) leaving them short one CNA. Staff I, RN said the facility does not have a Staffing Coordinator; the one they had left over a month ago with no notice. She said the DON has been doing staffing for nurses and the supply person has been doing the CNA staffing. Staff I, RN stated she was scheduled to work a double shift Friday, 2/17/23 from 3:00-11:00 p.m. and then 11:00 p.m. to 7:00 a.m. on 2/18/23. She said she requested off, but was only taken off one shift, not both. Staff I, RN did not realize she was still on the schedule to work from 11:00 p.m. to 7:00 a.m.
An interview was conducted with Staff F, LPN on 2/19/23 at 9:08 a.m. Staff F, LPN said she worked Friday 2/17/23 from 3-11 p.m. She said she stayed over after her shift due to staffing issues. She stated there was no nurse to relieve her. Staff F, LPN said she clocked out at 12:41 a.m. on Saturday 2/18/23. She stated her shift had four nurses working, but the 11p.m. to 7 a.m. shift only had one nurse and two no shows. Staff F, LPN confirmed Staff A, LPN was the only nurse working and Staff B, RN/UM was the on-call nurse. Staff F, LPN said Staff D, LPN was staying until the on-call nurse arrived. The on-call nurse is a nurse that has the on-call phone. Staff call that phone if they are not going to be at work or if they are late. The on-call nurse either finds someone to cover or goes in to work. Staff F, LPN said the facility used to staff four nurses at night and now they only staff three. She also added they do not have enough CNAs either. She said CNAs are always having to split an extra hall and she had noticed residents are not getting showers because of the CNA shortage.
An interview was conducted with Staff D, LPN on 2/19/23 at 9:27 a.m. Staff D, LPN said she worked Friday 2/17/23 from 3-11 p.m. She said she stayed over to just before 2:00 a.m. when the on-call nurse, Staff B, RN/UM, came in. Staff, D, LPN said Staff A, LPN was the only nurse there and she was waiting with her. Staff D, LPN said she did not have any residents assigned to her, but she was keeping an eye out. She said there were only the two of them in the building and she waited for the second nurse to arrive before she left. Staff D, LPN said no resident had to go to the hospital while she was there. A follow-up interview was conducted with Staff D, LPN on 2/21/23 at 4:17 p.m. She stated if another nurse is late, it is normal for the nurse that is waiting to not pick up an assignment. She said the expectation is they are actively waiting and assist if needed. Staff D, LPN said normally a nurse leaving her shift waits and does their narcotic counts with the on-coming nurse or the unit manager.
A follow-up interview was conducted with Staff A, LPN on 2/20/23 at 7:20 a.m. regarding the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift. Staff A, LPN confirmed Staff D, LPN was in the facility but she was just waiting. She added Staff D, LPN was not answering call lights or helping with anything. Staff A, LPN said she did narcotic counts and took keys for three medication carts and took report for the residents on the 500, 600, and 700 halls. She said she told the nurses she was not doing counts and taking any more medication cart keys or residents than that. She added that when Staff B, RN/UM arrived, she took the key to the front medication carts, for the 200, 400, and 800 halls. Staff A, LPN said by the time Staff B, RN/UM arrived, she had already completed the paperwork for Resident #1 to go to the hospital and EMS had already been initiated. Staff A, LPN stat[TRUNCATED]
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0725
(Tag F0725)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure sufficient staffing in order to provide care...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure sufficient staffing in order to provide care and services to 57 residents on the 200, 400, and 800 halls including one resident (#1) that experienced respiratory distress. They failed to ensure sufficient staffing to provide ADL (Activity of Daily Living) care to three out of three residents (#1, 5, and 6) sampled out of 49 residents dependent on staff for showers.
On 2/17/23 at 11:00 p.m. three nurses and five Certified Nursing Assistants (CNA) were scheduled to begin their shift. Of the three nurses, one clocked-in for her shift, one was scheduled in error, and one did not realize she was scheduled to work that shift. For approximately three hours Staff A, Licensed Practical Nurse (LPN) was the only nurse working on the floor, with a census of 114 residents. Staff D, LPN was in the building until 1:46 a.m., however, she was only waiting and had no resident assignment. Staff A, LPN was assigned 57 residents total on the 500, 600, and 700 halls. The 57 residents total on the 200, 400, and 800 halls had no nurse assigned to them. Resident #1 resided on the 800 hall, with no nurse assigned to her. At approximately 1:45 a.m. Resident #1's CNA noticed the resident was not well and called for Staff A, LPN to come help. At that time Resident #1's blood pressure was 58/42, respirations 28, pulse 136, and oxygen saturation 71%. Staff A, LPN stated the resident had gurgling in her throat and she had to leave the resident to retrieve suctioning supplies, call 911 and call the doctor. There was no other nurse available to assist with the resident or help the nurse with these tasks. Resident #1 was transferred to the hospital via Emergency Medical Services. In the emergency department the resident was on 8 L (liters) of oxygen to keep her saturation at 94%. She was admitted with diagnoses including acute respiratory failure with hypoxia, aspiration pneumonia/healthcare-associated pneumonia, and severe sepsis requiring IV (intravenous) hydration. Staff B, Registered Nurse (RN)/Unit Manager (UM) arrived at the facility at approximately 1:45-2:00 a.m. and Staff I, RN arrived at 2:10 a.m. Of the five scheduled CNAs only four clocked-in to work. During the Friday 2/17/23 11:00 p.m. to Saturday 2/18/23 7:00 a.m. shift CNAs were assigned to 28 residents on average.
Interviews with multiple staff members revealed on-going staffing issues. There was no staffing coordinator in the facility and the staffing duties were being shared between the DON and the Central Supply Clerk. Scheduling errors were being made, staff were unaware of their schedules, and staff cancellations were not being covered. Interviews revealed staff members are unable to complete resident ADL care as expected due to having large resident assignments.
This failure created a situation that resulted in the likelihood of serious injury or harm to Resident #1 and other residents in the facility and resulted in the determination of Immediate Jeopardy on 2/17/23. The findings of Immediate Jeopardy were determined to be removed on 2/23/23 at 11:45 a.m. and the scope and severity was reduced to a E.
Findings included:
1.
A review of Resident #1's SBAR (Situation Background Assessment Recommendation) Communication Form, dated 2/18/23 at 2:09 a.m. and signed by Staff A, LPN revealed that Resident #1's vital signs were: blood pressure 58/42, respirations 28, pulse 136, and oxygen saturation 71% and blood sugar 224. The Resident Evaluation showed the resident had swallowing difficulty, labored or rapid breathing, and a non-productive cough.
A review of the SNF/NF (Skilled Nursing Facility/Nursing Facility) to Hospital Transfer Form for Resident #1, dated 2/18/23 2:09 a.m., and signed by Staff A, LPN was reviewed. The form showed Staff A, LPN gave report by phone to the emergency room Charge Nurse on 2/18/23 at 2:43 a.m. The Hospital Transfer Form showed Resident #1 was totally dependent for bathing, dressing, toileting, transfers, and eating, incontinent of bowel and bladder, non-ambulatory, and had risk alerts for aspiration, high fall risk, needs medications crushed, pressure ulcers/injuries, seizures and swallowing precautions.
A review of the (local) County Fire Rescue run report showed the 911 call from the facility was received on 2/18/23 at 1:47 a.m. Emergency Medical Services (EMS) arrived on scene at 1:55 a.m. and departed the facility at 2:02 a.m. The run report revealed, Pt [patient] appears to be mentally disabled. Pt has audible congestion in her airway and staff stated that the pt does not have CHF [congestive heart failure], Pt was sheeted onto our stretcher and strapped on then loaded into R42 [ambulance]. Pt vitals and info were gathered. Pt lung sounds are fairly clear on the right with some rhonchi, and pts lung sounds are diminished on the lefts side. Pts congestion sounds to be in the upper respiratory tract. Pt was sat up straight and was administered 10 LPM [liters per minute] of O2 [oxygen] via NRM [non re-breather mask], 4-lead EKG performed. IV was established in pts left hand. Pt BS [blood sugar] is 116. 12-Lead EKG performed. Pt O2 SAT [oxygen saturation] has improved. Pt was examined, no obvious injuries were noted. Pts mentation has remained the same. Pt was trans [transported] to the ER [emergency room] without incident, pt care and info turned over to ER staff.
A review of the Emergency Department Documents for Resident #1, dated 2/18/23, showed Patient is a 61 years [sic] old female presenting with a complaint of shortness of breath today with hypoxia. The patient has an extensive medical history and is at this skilled nursing facility mainly because she has Down Syndrome and developmental delay. The report was at baseline the patient has very limited verbal ability and cannot tell you how she is feeling if she feels sick. The EMS at the facility also noted that the patient had a fever. There is [sic] been no note vomiting or diarrhea, no rash, the patient has reportedly had a cough today. The documents noted: The patient is currently with continued hypoxia in the emergency department. The patient is now on 8 L (liters) of oxygen to keep her saturation at 94%. The patient remains with some tachycardia and some tachypnea due to the illness. The patient has been started on antibiotics with cefepime and vancomycin to cover for the urinary tract infection as well as healthcare acquired pneumonia. At this point the patient does not have clinical evidence of severe sepsis. Plan to have the patient admitted to [primary provider] service for continued evaluation and treatment.
A review of the hospital History and Physical (H & P) completed by Resident #1's physician on 2/18/23 at 11:26 a.m. revealed she was admitted to the hospital for shortness of breath and altered mental status. The H & P showed She was brought in yesterday as reported indicated that she was having worsening shortness of breath and hypoxia. The H & P Assessment showed the following:
1. Acute respiratory failure with hypoxia, present on admission.
2. Aspiration pneumonia/healthcare-associated pneumonia.
3. Severe sepsis requiring IV hydration.
5. Functional quadriplegia.
6. Dysphagia.
7. Down syndrome.
8. Coronavirus A infection.
An interview was conducted with Staff C, CNA on 2/21/23 at 7:25 a.m. Staff C, CNA confirmed she was the CNA taking care of Resident #1 on the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift. She stated there was no nurse assigned to the 800 hall, where Resident #1 resided, and there was only one nurse working on the floor in the facility. Staff C, CNA said she checked on Resident #1 and she did not look ok. She said she went out to the hall and yelled for Staff A, LPN, the only nurse working, to come help. Staff C, CNA said she took Resident #1's vital signs and they were not good. She stated Staff A, LPN came and quickly assessed the resident, then went to call 911 and get suction equipment while Staff C, CNA stayed with the resident. She stated Staff A, LPN returned to the room and couldn't find the thin suction tubing she needed to suction the resident. Staff C, CNA said she then went out and looked for the suction supplies. She said all they could find was a yankauer for the LPN to use. Staff C, CNA said the nurses had used the thin flexible suction in the facility before and she didn't understand why it wasn't replaced. She stated no one else came to assist her and Staff A, LPN with the resident. She added that Staff D, LPN who was in the building charting was going out the door. Staff C, CNA stated staffing is always an issue and it is concerning. She added there have been nights where there were only two CNAs for the entire facility (she was unable to recall dates.) Staff C, CNA said, something bad is going to happen.
An interview was conducted with Staff A, Licensed Practical Nurse (LPN) on 2/19/23 at 5:24 a.m. Staff A, LPN stated there are staffing and scheduling issues in the facility. She said sometimes people are on the schedule that are not supposed to be. She added there is no master schedule, staff do not get a copy of their schedules and they must come in to see when they are on the schedule to work. Staff A, LPN stated as an example this past Wednesday was her day off, but she was on the schedule to work. She said there have been various nights shifts in the facility when there are only three to four Certified Nursing Assistants (CNA) working. Staff A, LPN said when the census is 115 residents, there should be three nurses on the floor, but on Friday night, 2/17/23 11 p.m. to 2/18/23 7 a.m., she was the only nurse on the floor for a few hours. She stated one nurse on the schedule wasn't confirmed and the Director of Nursing (DON) cancelled two other nurses that were scheduled to work. Staff A, LPN reported when she saw texts the nurses were not coming in, she called the on-call nurse, Staff B, Registered Nurse (RN)/Unit Manager (UM,) and received no response. Staff A, LPN said one of the 3-11 p.m. nurses stayed over until that nurse completed her charting. She reiterated that she was left as the only nurse working in the facility for a few hours. She said she again contacted the on-call nurse, and that person contacted the DON. The on-call nurse, Staff B, RN/UM, came in to the facility at approximately 2:00 a.m. Staff A, LPN stated she was trying to send a resident out to the hospital due to respiratory distress while she was the only nurse covering residents. During the interview Staff A, LPN's text messages and call log were observed on her cell phone and showed she sent a text message to the on-call nurse at 11:32 p.m., a call to the on-call nurse at 11:42 p.m. and a call to the on-call nurse at midnight. The on-call nurse called Staff A, LPN's cell phone at 1:02 a.m. Staff A, LPN also added there were only four CNAs in the facility that shift and some residents were unable to have their briefs changed and had to wait until the next morning.
A follow-up interview was conducted with Staff A, LPN on 2/19/23 at 7:23 a.m. regarding the resident she sent to the hospital on the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift. Staff A, LPN stated she had to send Resident #1 to the hospital via Emergency Medical Services (EMS) around 1:30 a.m. She stated the resident was gurgling in her throat, but she was unable to find the suction tubing she needed to suction the resident's throat area. Staff A, LPN said she had a suction canister but was unable to locate the larger tube that attached to the suction and could not find the small flexible tubing to suction the resident's throat. She said she was able to use a yankauer (a medical suction device that is a rigid plastic with a large opening for suctioning) to suction the resident's mouth. She said she was alone and did what she could.
A review of Resident #1's care plan showed a care plan for Aspiration Risk, dated 5/18/22. The focus of the care plan The resident is at risk for aspiration related to difficulty swallowing because of: Diagnosis of dysphagia. History of aspiration pneumonia. Interventions included: observe for signs and symptoms of aspiration: coughing, tearing, runny nose, wet vocal tone, difficulty breathing, pocketing food. A care plan for Cognition, revised on 6/6/22, showed the resident has impaired cognitive function or impaired thought processes related to intellectual disability (Down syndrome.) The resident is not able to make concrete needs known and dose not follow commands. Interventions included: Report to nurse any changes in cognitive function, specifically changes in: decision making ability, memory, recall, awareness of surroundings and others, difficulty expressing self, difficulty understanding others, sleepiness/lethargy, confusion. A care plan, revised 1/16/23, in place for ADL (Activities of Daily Living) Self-care performance deficit due to impaired cognition, impaired mobility, and generalized weakness. Interventions included: Resident is totally dependent upon staff for ADLs. Encourage to participate at highest functional ability, anticipate needs, bathing: the resident requires the assist of two, and transfer is total mechanical lift to chair. A care plan in place for emphysema/COPD (Chronic obstructive pulmonary disease), dated 3/21/22. The interventions included: monitor for difficulty breathing (dyspnea) on exertion and remind resident not to push beyond endurance, monitor for signs and symptoms of acute respiratory insufficiency: anxiety, confusion, restlessness, shortness of breath (SOB) at rest, cyanosis, somnolence, monitor/document/report to doctor as needed any signs and symptoms of respiratory infection: fever, chills, increase in sputum, chest pain, increased difficulty breathing, increased coughing or wheezing.
A review of Resident #1's tasks show the resident was scheduled to receive showers every Tuesday and Friday on the 3:00-11:00 p.m. shift. From February 1st-Febuary 17th, the resident received five bed baths and no showers. From January 1st-January 31st (not counting days resident was out of the facility), the resident had eight scheduled shower days. Of those eight shower days, two were partial baths and six were bed baths. The resident had no showers from January 1-Febuary 17, 2023.
A review of progress notes showed Resident #1 was sent to the hospital on 1/11/23 and returned to the facility on 1/16/23 with a diagnosis of pneumonia and urinary tract infection (UTI.) A review of Resident #1's provider notes, dated 1/24/23, revealed she was seen at the facility to evaluate post hosp (hospital) PNA [pneumonia], UTI [urinary tract infection], g-tube accidently pulled ithout [sic] complication, will leave out per family request, complex UTI, siezure [sic] like activity hypotyriod [sic], PNA, and adjusting medication, anxiety, dermatitis, candida, around peg tube improving elevated ammonia level, BUN 45, UA [urinalysis] positive, hypotensive post hospitalization, monitoring of patient multiple comorbidities, evaluation of new developments medication reconciled and care coordination. The provider notes revealed the resident is at increase risk for rehospitalization, due to safety issues, infection, development of DVTs [Deep Vein thrombosis] and pulmonary embolism and the resident was needing frequent monitoring due to the complexity of chronic disease.
On 2/22/23 at 9:35 a.m. a family member/guardian for Resident #1 was interviewed. The family member stated sometimes there is only one CNA working two halls in the facility. She said you can press the call light and they don't answer. She said medications are late. She said she complains to administration all the time and nothing is done. The family member stated she was called at 2:00 a.m. Friday morning (2/18/23) and told Resident #1 was going to the hospital. She said she was told they couldn't suction the resident because there was no RN. She stated the resident had phlegm in her throat for the two days prior to going to the hospital. She felt like the resident needed suctioning during those two days.
On 2/17/23 at 11:00 p.m. the facility census was 114 according to the Director of Nursing (DON), on 2/19/23 the facility had a census of 113.
Review of the Facility Assessment, dated 9/30/22, indicated the following staffing patterns:
Night shift: 0 nurse leaders, 1 RN, 2 LPNs, 6 CNAs
The Facility Assessment does not relate the staffing patterns to the acuity level of the residents.
According to the Resident Census and Conditions of Residents, CMS (Centers for Medicare and Medicaid Services) - 672, completed and signed by the DON on 2/19/23, the following conditions represented the facility population on that day:
8 residents on Hospice Care
5 residents receiving Intravenous (IV) therapy, IV nutrition, and/or blood transfusion,
9 residents receiving respiratory treatment.
1 resident receiving ostomy care.
11 residents receiving tube feedings.
1 resident with an Intellectual and/or developmental disability.
50 residents with documented psychiatric diagnosis (exclude dementias and depression.)
43 residents with dementia
3 residents with behavioral healthcare needs
109 residents that are occasionally or frequently incontinent of bladder.
98 residents that are occasionally or frequently incontinent of bowel.
Of the current 113 residents 31 were dependent on staff for toilet use and 82 need one or two staff to assist.
The facility consisted of a front and back unit with two nurses' stations in the middle. Six hallways join at the nurses' stations like the spokes of a wheel. The 200, 400, and 800 halls are the front unit, and the 500, 600 and 700 halls the back unit. Copy of facility floor plan obtained.
The facility used a Nurse Daily Sign-in sheet, located in a staffing book at the nurses' station; the sheet listed which RNs, LPNs, and CNAs were assigned to work each shift and what their assigned halls will be. Staff members initialed next to their name when they came in for each shift. A review of the Nurse Daily Sign-in Sheet for the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift, showed the following nurses were scheduled: Staff A, LPN, Staff, I, RN, and Staff J, LPN. Written beside Staff J, LPN was a note, said he doesn't work wkends [sic]. The following CNAs were scheduled to work: Staff N, CNA, Staff O, CNA, Staff P, CNA, Staff C, CNA, and Staff Q, CNA. Staff Q, CNA had a line through her name with off written next to it, leaving only four CNAs working that shift. In the daily staffing book a loose sheet of paper was observed with a note, dated 2/17/23, from Staff M, CNA, tomorrow Sat. [DATE] is my regular day off. (W/E off) [weekends off] I never agreed to work. Staff M, CNA was scheduled to work from 3:00 p.m. to 11:00 p.m. on 2/18/23.
Review of the Nurse Daily Sign-in Sheet for Saturday, February 18, 2023, showed the resident census of 114 and four CNAs working on the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift, they were assigned on average 28 residents each.
Review of the Punch Detail Report for the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift revealed the time each staff member clocked in and out of the facility. Staff A, LPN clocked in at 11:04 p.m. on 2/17/23 and clocked out at 7:48 a.m. on 2/18/23, Staff F, LPN clocked out at 12:41 a.m. and Staff D, LPN clocked out at 1:46 a.m. Staff I, RN clocked in at 2:10 a.m. Staff B, RN/UM came in at approximately 1:45 a.m. to 2:00 a.m. (management does not clock-in).
Review of the Nurse Daily Sign-in sheet for Sunday February 19, 2023, revealed six CNAs scheduled to work the Saturday 2/18/23 11:00 p.m. to 2/19/23 7:00 a.m. shift. Two of the scheduled CNAs did not work that shift and one additional was added, leaving five CNAs working. With a resident census of 114; this gave each CNA on average 22 residents each. Being down one CNA, this left the available CNAs splitting the extra hallway. The assignments for that shift were as follows:
Staff N, CNA -one full hall plus rooms [ROOM NUMBERS]
Staff O, CNA- one full hall plus rooms [ROOM NUMBERS]
Staff R, CNA- one full hall plus room [ROOM NUMBER]
Staff G, CNA- one full hall plus rooms [ROOM NUMBERS]
Staff H, CNA- one full hall plus rooms [ROOM NUMBERS]
An interview was conducted with Staff I, RN on 2/19/23 at 5:50 a.m. Staff I, RN said she was scheduled to work the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift, but there was a miscommunication because she had requested off. She stated she came in around 2:00 a.m. She said there were two nurses in the building when she arrived. She confirmed there were only four CNAs working that shift.
A Review of the Nurse Daily Sign-in for Saturday February 18, 2023, confirmed there were five CNAs scheduled for the Friday 2/17/23 11:00 p.m. to Saturday 2/18/23 7:00 a.m. shift and one of them was crossed out with off written by their name.
An interview was conducted with Staff I, RN on 2/19/23 at 5:52 a.m. Staff I, RN said one CNA did not show up for the current shift (2/18/23 11:00 p.m. to 2/19/23 7:00 a.m.) leaving them short one CNA. Staff I, RN said the facility does not have a Staffing Coordinator; the one they had left over a month ago with no notice. She said the DON has been doing staffing for nurses and the supply person has been doing the CNA staffing. Staff I, RN stated she was scheduled to work a double shift Friday, 2/17/23 from 3:00-11:00 p.m. and then 11:00 p.m. to 7:00 a.m. on 2/18/23. She said she requested off, but was only taken off one shift, not both. Staff I, RN did not realize she was still on the schedule to work from 11:00 p.m. to 7:00 a.m.
An interview was conducted with Staff F, LPN on 2/19/23 at 9:08 a.m. Staff F, LPN said she worked Friday 2/17/23 from 3-11 p.m. She said she stayed over after her shift due to staffing issues. She stated there was no nurse to relieve her. Staff F, LPN said she clocked out at 12:41 a.m. on Saturday 2/18/23. She stated her shift had four nurses working, but the 11p.m. to 7 a.m. shift only had one nurse and two no shows. Staff F, LPN confirmed Staff A, LPN was the only nurse working and Staff B, RN/UM was the on-call nurse. Staff F, LPN said Staff D, LPN was staying until the on-call nurse arrived. The on-call nurse is a nurse that has the on-call phone. Staff call that phone if they are not going to be at work or if they are late. The on-call nurse either finds someone to cover or goes in to work. Staff F, LPN said the facility used to staff four nurses at night and now they only staff three. She added they do not have enough CNAs either. She said CNAs are always having to split an extra hall and she had noticed residents are not getting showers because of the CNA shortage.
An interview was conducted with Staff D, LPN on 2/19/23 at 9:27 a.m. Staff D, LPN said she worked Friday 2/17/23 from 3-11 p.m. She said she stayed over to just before 2:00 a.m. when the on-call nurse, Staff B, RN/UM, came in. Staff, D, LPN said Staff A, LPN was the only nurse there and she was waiting with her. Staff D, LPN said she did not have any residents assigned to her, but she was keeping an eye out. She said there were only the two of them in the building and she waited for the second nurse to arrive before she left. Staff D, LPN said no resident had to go to the hospital while she was there. A follow-up interview was conducted with Staff D, LPN on 2/21/23 at 4:17 p.m. She stated if another nurse is late, it is normal for the nurse that is waiting to not pick up an assignment. She said the expectation is they are actively waiting and assist if needed. Staff D, LPN said normally a nurse leaving her shift waits and does their narcotic counts with the on-coming nurse or the unit manager.
A follow-up interview was conducted with Staff A, LPN on 2/20/23 at 7:20 a.m. regarding the Friday 2/17/23 11 p.m. to Saturday 2/18/23 7 a.m. shift. Staff A, LPN confirmed Staff D, LPN was in the facility but she was just waiting. She added Staff D, LPN was not answering call lights or helping with anything. Staff A, LPN said she did narcotic counts and took keys for three medication carts and took report for the residents on the 500, 600, and 700 halls. She said she told the nurses she was not doing counts and taking any more medication cart keys or residents than that. She added that when Staff B, RN/UM arrived, she took the key to the front medication carts, for the 200, 400, and 800 halls. Staff A, LPN said by the time Staff B, RN/UM arrived, she had already completed the paperwork for Resident #1 to go to the hospital and EMS had already been initiated. Staff A, LPN stated when EMS arrived, they were asking about the resident's normal state. She said she told them she honestly didn't know, but fortunately the CNA knew the resident and was able to answer their questions. Staff A, LPN said when Resident #1 was in respiratory distress the CNA came to get her and the CNA took the resident's vital signs. Staff A, LPN said she had to leave the resident with the CNA to get suction equipment, call the doctor, and call 911. She said she was unable to find thin flexible suction catheter, but she did get a yankauer. She said when she returned to the room, the CNA left and got the larger tubing off the crash cart to connect the suction to the machine. Staff A, LPN said she was not able to get much with the yankauer suction and she felt if she had the thin flexible suction catheter it would have helped the resident. Staff A, LPN was asked where Staff D, LPN was during this time. She stated Staff D, LPN was leaving and she stated, she just needs to get suctioned. Staff A, LPN reiterated there have been on-going staffing issues. She stated for the Sunday 2/19/23 11:00 p.m. to 2/20/23 7:00 a.m. shift the DON cancelled a CNA and a RN. She said a CNA didn't show up, so an RN had to work as a CNA all night. Staff A, LPN said when they are short a CNA, the aides split the extra hall and those call lights do not get answered quickly. She said for the Saturday 2/18/23 11:00 p.m. to Sunday 2/19/23 7:00 a.m. shift the 500 hall was the one that was split between the CNAs.
An observation was made on 2/19/23 at 5:58 a.m. of Resident #2's call light activated on the 500 hall. The light outside the resident's room was on and the call bell was beeping at the nurses' station. The call light was observed continuously until it was answered at 6:18 a.m. At 10:32 a.m. an interview was conducted with Resident #2. The resident confirmed he was the one that had his call light on early this morning. When asked about waiting 20 minutes for his call light to be answered, he said, sometimes it takes that long. He added it takes longer for call bells to be answered around sunrise and just before.
A review of Resident #2's Minimum Data Set (MDS,) dated 11/22/22 was conducted. Section C, Cognitive Patterns showed Resident #1's Brief Interview for Mental Status (BIMS) score is 14, indicating he is cognitively intact. Section G, Functional Status, shows the resident needs extensive assistance with bed mobility, transfers, and toilet use.
An interview was conducted with Staff H, CNA on 2/19/23 at 5:28 a.m. He stated they are short a CNA on the current shift and each CNA has around 24 residents each. He stated it is harder to answer call lights with this many residents because he must start his final rounds early.
An interview was conducted with Staff G, CNA on 2/19/23 at 5:37 a.m. Staff G, CNA stated she has 26 residents assigned to her for the current shift. She said, it is too much, it is too much. Staff G, CNA said they are short staffed every night with nurses and CNAs. She said Friday night (2/17/23) the 11:00 p.m. to 7:00 a.m. shift only had one nurse until a second one eventually came in. She stated some nights there are only three to four CNAs working. Staff G, CNA said it is a lot of residents and she cannot do everything she needs to get done and answer call lights too.
On the Friday night (2/17/23) the 11:00 p.m. to 7:00 a.m. shift Staff A, LPN had taken over the medication cart and residents on the back unit, (the 500, 700, and 700 halls). This left 57 residents, including Resident #1, that resided on the front unit, (the 200, 400, and 800 halls), with no nurse assigned to them. The total census in the facility was 114 residents, according to the Nurse Daily Sign-in Sheet.
An interview was conducted with Staff B, RN/UM on 2/19/23 at 9:54 a.m. Staff B, RN/UM confirmed she was the on-call nurse for the Friday 2/17/23 11:00 p.m. to Saturday 2/18/23 7:00 a.m. shift. She stated Staff A, LPN called her early Saturday morning (2/18/23) and told her they were down nurses. Staff B, RN/UM told Staff A, LPN she was going to try to find someone to cover. Staff B, RN/UM came in to work; she said when she arrived Staff A, LPN was on the back halls (500, 600, and 700) and Staff D, LPN was still in the building. Staff B, RN/UM stated Staff D, LPN, did not have an assignment she was just waiting on me. Staff B RN/UM stated she worked on the front halls (200, 400, 800) once she arrived. She said when she arrived at the facility Staff A, LPN was working on a resident that was going to the hospital due to respiratory distress. She stated Staff A, LPN was unable to suction the resident. When asked if Staff A, LPN had the supplies she need to suction Resident #1 she stated, I couldn't tell you. I was doing vitals and other stuff. Staff B, RN/UM said she hasn't noticed staffing issues, but she is the UM for the day shift. Staff B, RN/UM confirmed there were only four CNAs working the Friday 2/17/23 11:00 p.m. to Saturday 2/18/23 7:00 a.m. shift.
An interview was conducted with the DON on 2/19/23 at 9:32 a.m. The DON stated she had inadvertently placed Staff J, LPN on the schedule for the Friday 2/17/23 11:00 p.m. to Saturday 2/18/23 7:00 a.m. shift. She said when she found out he wasn't at work she told the on-call nurse she would need to go in and work. The DON said Staff D, LPN stayed over until around 12:45 a.m. She stated there were only about 30 minutes with only two nurses in the building. She said Staff I, RN was late because she requested off from 3-11 on Friday 2/17/23, but was still supposed to from work 11:00 p.m. to 3 a.m. She said Staff I, RN assumed she had the whole night off, but she did not. The DON was asked about being short a CNA on the Saturday 2/18/23 11:00 p.m. to 2/19/23 7:00 a.m. shift. She said she didn't know off the top of her head how many CNAs were working. She stated there should have been six and she wasn't told anyone didn't come in. The DON stated the Staffing Coordinator quit on December 22, 2023 without giving notice. She confirmed herself and Staff K, Central Supply Clerk were doing staffing.
An interview was conducted on 2/20/23 at 8:19 a.m. with the DON. She stated Resident #1 has a history of aspiration pneumonia. She said they do not keep suctioning supplies in the resident's room, but the suctioning machine is on the crash cart. The DON stated they have the suctioning machine and a yankauer. She said they do not do deep suctioning or use the thin flexible catheter for suctioning; that is beyond our scope. We are not experienced in that She said they use the yankauer and suction the mouth. She added the nurse can also take their finger and swipe to clear the airway. The DON said for a resident in respiratory distress someone needs to be with the resident at all times. She said a staff member should stay with the resident until the nurse arrives, then the nurse can leave the room if there is another nurse with the resident. Regarding the shift going from Friday 2/17/23 11:00 p.m. to Saturday 2/18/23 7:00 a.m.; she said she cancelled two nurses prior to the shift because they were over their PPD (per patient day: the minimum required staffing per patient in the facility per day.) She said they should have three nurses with their current census. She said one of the nurses (Staff J, LPN) was on the schedule due to a scheduling error. She said when she found out he didn't