CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, review of facility's policies and procedures, and staff interview the facility failed to p...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, review of facility's policies and procedures, and staff interview the facility failed to protect residents' rights to be free from neglect.
The facility neglected to develop a care plan and ensure adequate supervision to prevent unsafe wandering and elopement for 1 (Resident #386) of 5 sampled cognitively impaired residents with active exit seeking behaviors.
On 4/1/23 at approximately 4:30 p.m., Resident #386 who was cognitively impaired, and wheelchair bound was not adequately supervised. The resident wheeled herself through an unsecured door of the skilled nursing facility into a hallway leading to the adjoining Assisted Living Facility.
Resident #386 left through the front door of the Assisted Living Facility, and traveled unsupervised in her wheelchair, approximately three tenths of a mile, and crossed two streets.
On 4/1/23 at 5:45 p.m., a staff member from a neighboring skilled nursing facility found Resident #386 wandering the streets.
Resident #386 had a likelihood for serious harm, injury, or death due to the risk for serious injury from a fall, getting lost or getting hit by a car.
The facility's failure to provide the necessary care and services to prevent neglect resulted in the determination of Immediate Jeopardy level at a scope and severity of isolated (J) starting on 4/1/23.
On 7/14/23 at 4:00 p.m., the facility's Administrator was informed of the determination of Immediate Jeopardy (IJ) and provided the IJ templates.
The facility census was 37 with five residents at risk for unsafe wandering and elopement.
The findings included:
Cross reference to F689, F835 and F867.
The facility's policy and procedure for abuse with a revised date of 10/23/22 noted, Neglect. Failure to provide goods or services necessary to avoid physical harm, mental anguish, or mental illness . Prevention. Identify, correct, and intervene in situations where . neglect, and/or mistreatment are more likely to occur. This includes, but is not limited to, identification/analysis of:
a.
Secluded areas of the facility.
b.
Sufficient staffing on each shift to meet the needs of the residents/patients.
c.
Assigned staff demonstrating knowledge of individual resident/patient needs.
d.
Sufficient and appropriate supervisory staff to identify inappropriate behaviors.
e.
Residents/patients with needs and behaviors which might lead to . neglect.
.The facility will take all necessary corrective actions depending on the results of the investigation . Occurrences will be analyzed to determine if any changes in policy and procedures should be implemented to prevent future occurrences .
Review of the clinical record revealed Resident #386 was an [AGE] year-old female admitted to the facility from an acute care hospital on 1/17/23 with diagnoses including Alzheimer's disease, history of intracranial hemorrhage (bleeding), visual loss in both eyes, traumatic brain injury, and seizures.
Review of the progress notes showed on 1/21/23 Resident #386 was up wandering in the hallway, attempting to go out exit door. The resident stated she was looking for the kitchen. The resident was reoriented and assisted back to her room and to bed.
The admission Minimum Data Set (MDS) Assessment with a target date of 1/23/23 noted the resident's cognition was severely impaired with a Brief Interview for Mental Status of 05. The MDS did not document Resident #386's wandering behaviors.
On 2/7/23 the physician ordered to apply a wanderguard (Brand name wander alert to notify staff when the resident leaves a safe area), and check the placement of the wanderguard every shift.
Resident #386 was discharged to an acute care hospital on 3/9/23 and returned to the facility on 3/20/23.
The elopement evaluation completed on 3/20/23 upon return to the facility noted Resident #386 was exhibiting exit-seeking searching behaviors such as standing by the exit door, looking for someone, asking to go home et cetera.
Review of the Medication Administration Record for 3/2023, and 4/2023 noted a physician's order dated 3/21/23 for a wanderguard.
The 5-Day Minimum Data Set (MDS) Assessment with a target date of 3/26/23 noted the resident's cognition was severely impaired with a Brief Interview for Mental Status of 01. The MDS noted Resident #386 exhibited wandering behaviors, one to three days. The MDS was inaccurate and did not reflect the use of the wander/elopement alarm. Resident #386 used a wheelchair and required extensive physical assistance of one person for locomotion off unit (How resident moves to and returns from off-unit locations), if in wheelchair, self-sufficiency once in a chair.
The care plan was not revised to reflect the risk for elopement and interventions to prevent unsafe wandering and elopement.
On 4/1/2023 at 6:56 p.m., a nursing progress note read, Resident was last seen during med pass by nurse in W/C (wheelchair) at nurses station at 1630 (4:30 p.m.). CNA (Certified Nursing Assistant) notified nurse as 1755 (5:55 p.m.) that resident was no longer in nurses station area nor in dining area. Head count completed and noticed that the resident was no longer on grounds. Absence of alarms did not notify facility that resident had exited the building. Found at near [sic] by facility . Family, MD, and DON (Director of Nursing) notified of elopement.
Review of the facility's investigation, and analysis of the incident revealed on 4/1/23 at 4:30 p.m., Resident #386 was seen at the nurses station. Upon investigation it was apparent she then traveled in her wheelchair down the back hallway where the wander guard was alarming outside room [ROOM NUMBER] outside door.
There was no documentation staff increased supervision when Resident #386 attempted to leave the facility and triggered the wander alarm.
The investigation noted after triggering the wander alarm to the outside door close to room [ROOM NUMBER], Resident #386 when through the double doors into the Assisted Living Facility (ALF), traveled that hallway until she made a right heading to the main entrance of the facility where the wander guard in that hallway was also triggered. She then exited the building through the main entrance and to the road where she turned left and proceeded down Pinebrook Avenue in her wheelchair. The elopement occurred during mealtime for both sides of the house and staff were either serving in their perspective dining rooms or on break in the ALF. Resident #386's family typically visit her daily between 4:00 p.m., and 5:00 p.m., and take her outside to visit and enjoy fresh air. On 4/1/23, Resident #386's family did not come. Upon interviewing staff who were on shift, they did not think her absence was unusual during this time because she is routinely outside at this time to visit with family.
The facility's immediate corrective action was to place the resident on one to one supervision to prevent further incidents of unsafe wandering and elopement.
On 4/4/23 Resident #386 was discharged to a secured memory care unit.
On 4/1/23 Registered Nurse Staff Y documented in a witness statement, On 4/1/23 I did not see (Resident #386) in the dining room or in the facility from the time I came on to the floor at 3:00 pm today. (Facility name) called Advinia Care at 6 pm asking if we were missing a resident. (Resident #386) was found at (facility name) and her nurse brought resident back. She was in her wheelchair.
The facility provided documentation on 4/3/23 (two days after the elopement) they educated staff for 10 minutes on responding to the wander alarm, including not turn off the alarm until all residents are accounted for.
There was no documentation five staff members on duty when Resident #386 eloped were educated.
There was no documentation the facility-initiated elopement drills on all shifts, including weekends to verify staff understood the education and responded appropriately to the wander alarm when activated.
On 7/11/23 the facility provided a list of current residents identified to be at risk for unsafe wandering and elopement, including Residents #8, #26, #11, #287, and #288.
On 7/11/23 at approximately 5:50 p.m., the door connecting the skilled nursing facility to the ALF remained unsecured. It was not equipped with an alarm to alert staff to unsafe wandering.
On 7/11/23 at 5:54 p.m., the surveyor used the fob provided by the facility to trigger the alarm of a door equipped with a wander alarm system at the skilled nursing facility to observe the staff response to the alarm.
On 7/11/23 at 5:57 p.m., CNA Staff AA started closing all residents' bedroom doors in response to the alarm. She said, I thought it was a fire alarm. Staff AA did not investigate or look around to see if Residents #8, #26, #11, #287, and #288 identified to be at risk for elopement and wore a wander alarm had left the facility.
Review of the Agency For Health Care Administration Background Screening Clearing house revealed Staff AA permanent hire date was 1/12/23.
Review of the in-service related to wanderguards dated 4/3/23 lacked documentation CNA AA attended the in-service which specified, If anyone hears this alarm they are to investigate it immediately. Look around do you see a resident with a white bracelet and alarm? Look outside, if there a resident outside who has on a white bracelet and alarm.
On 7/11/23 at 6:00 p.m., Licensed Practical Nurse (LPN) Staff P turned off the alarm, and said, The alarm means it is an elopement risk. She looked out the door and said she did not see anyone. She did not initiate a count of the residents to ensure all cognitively impaired residents at risk for elopement, including Residents #8, #26, #11, #287, and #288 were accounted for.
LPN Staff P attended the 10 minutes in-service on 4/3/23 and did not follow the procedure which specified, You can not [sic] turn off the alarm until you know that all residents are accounted for.
The facility's policy on Elopement Prevention effective 2/10/21 and revised on 6/22/23 noted when a resident is deemed to be an elopement risk, photos of the resident should be taken and placed in the elopement risk book. Documentation of the elopement risk should be made on the Facility elopement Book, placed at nursing station and front entry.
On 7/11/23 at approximately 3:00 p.m., the elopement book at the receptionist desk at the entrance of the skilled nursing facility, and the entrance of the adjoining Assisted Living Facility were reviewed. The elopement books did not include Resident #26, #288, and #287.
On 7/12/23 at 9:00 a.m., the Director of Nursing stated not all current employees had completed the Inservice. She verified the skilled nursing unit was not a secured unit. She stated the elopement book was updated with each resident added. The DON said she did not know what was going to be done about the unsecured door between the assisted living facility and the skilled unit.
On 7/14/23 at 10:30 a.m., the Administrator said he did not have any additional information related implementation of processes to ensure a safe environment, including adequate supervision of cognitively impaired residents with known exit seeking behaviors to prevent unsafe wandering and elopement.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and staff interviews, the facility failed to implement processes to ensure adequate supervi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and staff interviews, the facility failed to implement processes to ensure adequate supervision of 1 (Resident #386) of 5 cognitively impaired residents at risk for elopement to prevent unsafe wandering and elopement.
On 4/1/23 at approximately 4:30 p.m., Resident #386 who was a vulnerable cognitively impaired, wheelchair bound resident with known wandering behavior was not adequately supervised. The resident wheeled herself through an unsecured door of the skilled nursing facility into a hallway leading to the adjoining Assisted Living Facility. Resident #386 wore a wander alarm and triggered the alarm of two doors without staff response.
Resident #386 left through the front door of the Assisted Living Facility, and traveled in her wheelchair, approximately three tenths of a mile, and crossed two streets.
Resident #386 was missing for approximately one hour and 30 minutes without staff knowledge.
On 4/1/23 at 5:45 p.m., a staff member from a neighboring skilled nursing facility found Resident #386 wandering the streets.
Resident #386 had a likelihood for serious harm, injury, or death due to the risk for serious injury from a fall, getting lost or getting hit by a car.
The failure to ensure adequate supervision to protect vulnerable residents from unsafe wandering and elopement resulted in a determination of Immediate Jeopardy (IJ) at a scope and severity of isolated (J) starting on 4/1/23 when Resident #386 left the building without staff knowledge.
On 7/14/23 at 4:00 p.m., the facility Administrator was notified of the Immediate Jeopardy and provided the IJ templates.
The immediate Jeopardy was ongoing.
The facility census was 37 with five residents at risk for elopement.
The findings included:
Cross reference to F600, F835 and F867
The facility's policy for Elopement Prevention with a revised date of 6/22/2021 noted, When a resident is deemed to be an elopement risk the following measures should be put in place:
Residents should be placed in a secured unit.
A wander guard bracelet should be placed on the resident.
A Physicians order should be written to check placement of the wander guard every shift and function of bracelet daily.
Photos should be taken of the resident to be placed in the Elopement Risk book.
Communication to all staff on duty should be completed and carried on from shift to shift.
Documentation of the Elopement Risk should be made . facility Elopement Book, placed at nursing station and front entry . Elopement concerns and resident at risk should be reviewed monthly and discussed at the facility QAPI (Quality Assurance and Performance Improvement) meeting to discuss trends and concerns.
Elopement Risk Book should be reviewed daily and discussed at change of shift. Photos should be current with description of resident along with any other pertinent information that may help with locating the resident in an elopement situation.
The Elopement-Missing Resident Policy CE-2, Revised 10/2022 noted the facility administration should complete a thorough investigation including the wanderguard (wander alarm to alert staff when a resident leaves a safe area) system and evaluating any preventative measure that may have been in place.
Resident #386 was an [AGE] year-old female admitted to the facility from an acute care hospital on 1/17/23 with diagnoses including Alzheimer's disease, history of intracranial hemorrhage (bleeding), visual loss in both eyes, traumatic brain injury, and seizures.
The elopement evaluation completed on 3/20/23 noted Resident #386 was exhibiting exit-seeking searching behaviors such as standing by the exit door, looking for someone, asking to go home et cetera.
The physicians orders dated 3/21/23 included the use of a wander guard for Resident #386.
The care plan was not revised to reflect the risk for elopement and interventions to prevent unsafe wandering and elopement.
The 5-Day Minimum Data Set (MDS) Assessment with a target date of 3/26/23 noted the resident's cognition was severely impaired with a Brief Interview for Mental Status of 01. The MDS noted Resident #386 exhibited wandering behaviors, one to three days. The MDS was inaccurate and did not reflect the use of the wander/elopement alarm that was used during the assessment observation period.
A nursing progress note dated 4/1/23 (Saturday) read, Resident (Resident #383) was last seen during med pass by nurse in W/C (wheelchair) at nurses station at 1630 (4:30 p.m.). CNA (Certified Nursing Assistant) notified nurse as 1755 (5:55 p.m.) that resident was no longer in nurses station area nor in dining area. Head count completed and noticed that the resident was no longer on grounds. Absence of alarms did not notify facility that resident had exited the building. Found at near [sic] by facility . Family, MD, and DON (Director of Nursing) notified of elopement.
Review of the facility's investigation, and analysis of the incident revealed on 4/1/23 at 4:30 p.m., Resident #386 was seen at the nurses station. Upon investigation it was apparent she then traveled in her wheelchair down the back hallway where the wander guard was alarming outside room [ROOM NUMBER] outside door.
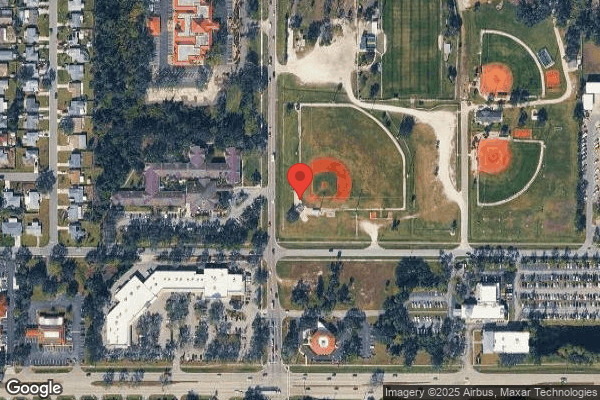
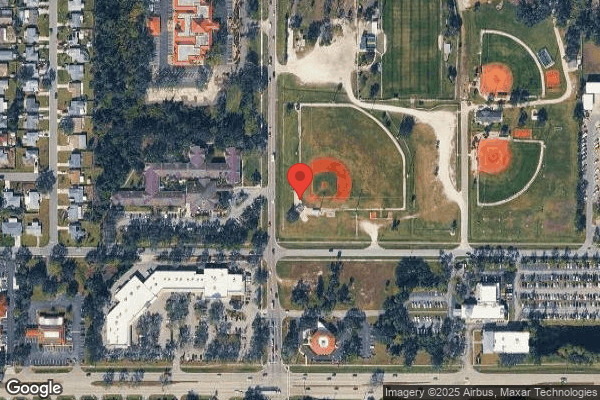
The investigation noted after triggering the wander alarm to the outside door, close to room [ROOM NUMBER], Resident #386 went through the double door into the Assisted Living Facility (ALF), traveled that hallway until she made a right heading to the main entrance of the facility where the wander guard in that hallway was also triggered. She then left the facility through the main entrance where that alarm was also triggered. She then exited the building through the main entrance and to the road where she turned left and proceeded down Pinebrook Avenue in her wheelchair.
All wander guard checks have shown no fault in the system alerting when triggered. The elopement occurred during mealtime for both sides of the house and staff were either serving in their perspective dining rooms or on break in the ALF.
Resident #386's family typically visited her daily between 4:00 p.m., and 5:00 p.m. and took her outside to visit and enjoy fresh air. On 4/1/23 the family did not come. Upon staff interview, staff who were on shift and knew Resident #386 said they did not think the resident's absence was unusual during this time since she was routinely outside at that time of the day to visit with family.
Resident #386 was discovered down Pinebrook Avenue on 4/1/23 at approximately 6:00 p.m., by a member of a nearby skilled nursing facility who contacted the facility and asked if they were missing a resident.
There was no documentation staff increased supervision after Resident #386's first attempt to leave the facility when she triggered the wander alarm of the door leading to the outside near room [ROOM NUMBER].
The facility's immediate corrective action was to place Resident #386 on one-to-one supervision to prevent further incidents of unsafe wandering and elopement.
On 4/4/23 Resident #386 was discharged to a secured memory care unit.
Resident #386's care plan was not updated with interventions to prevent further incidents of unsafe wandering and elopement until 4/6/23, two days after discharge.
On 4/1/23 Registered Nurse Staff Y documented in a witness statement, On 4/1/23 I did not see (Resident #386) in the dining room or in the facility from the time I came on to the floor at 3:00 pm today. [Facility name] called Advinia Care at 6 pm asking if we were missing a resident. (Resident #386) was found at Orchid Cove and she was brought back to the facility.
The facility provided documentation on 4/3/23 (two days after the elopement) they educated staff for 10 minutes. The topic of the education was Wanderguards, and included responding to the wander alarm, including not turning off the alarm until all residents are accounted for.
There was no documentation Licensed Practical Nurse Staff X, Certified Nursing Assistants (CNAs) Staff CC, DD, EE, and FF who were on duty when Resident #386 eloped were educated.
There was no documentation the facility-initiated elopement drills on all shifts, including weekends to verify staff understood the education and responded appropriately to the wander alarm when activated.
On 7/11/23 the facility provided a list of current residents identified to be at risk for unsafe wandering and elopement, including Residents #8, #26, #11, #287, and #288. Residents #11, #287, and #288 wore a wander alert bracelet.
On 7/11/23 at 5:00 p.m., the Administrator in training provided the surveyor a fob to trigger the wander alarm from front entrance door of the Assisted Living Facility to observe staff response. The Administrator in training was present when the alarm was triggered.
The ALF receptionist and business office manager said they were new employees and had completed their orientation. Both staff members said they did not receive education about the wander alarm system.
A staff member from the skilled nursing facility started educating the receptionist and the business office manager on response when the wander alarm is triggered.
On 7/11/23 at approximately 5:50 p.m., the door connecting the skilled nursing facility to the ALF remained unsecured. It was not equipped with an alarm to alert staff to unsafe wandering.
On 7/11/23 at 5:54 p.m., the surveyor used the fob to trigger the alarm of a door equipped with a wander alarm system at the skilled nursing facility to observe the staff response to the alarm.
On 7/11/23 at 5:57 p.m., CNA Staff AA started closing all residents' bedroom doors in response to the alarm. She said, I thought it was a fire alarm. Staff AA did not investigate or look around to see if Residents #11, #287, and #288 identified to be at risk for elopement and wore a wander alarm had left the facility.
Review of the Agency For Health Care Administration Background Screening Clearing House website revealed Staff AA's permanent hire date was 1/12/23.
Review of the in-service related to Wanderguards dated 4/3/23 lacked documentation CNA AA attended the in-service which specified, If anyone hears this alarm they are to investigate it immediately.
On 7/11/23 at 6:00 p.m., Licensed Practical Nurse (LPN) Staff P turned off the alarm, and said, The alarm means it is an elopement risk. She looked out the door and said she did not see anyone. She did not initiate a count of the residents to ensure all cognitively impaired residents including Residents #8, #26, #11, #287, and #288 were accounted for.
On 7/12/23 at approximately 4:00 p.m., Resident #288 was observed on the unit. He did not have a wander alert bracelet.
LPN Staff P verified Resident #288 was not wearing a wander alert bracelet as ordered. She said the resident had removed the wander alert bracelet.
Review of the clinical record for Resident #288 revealed a physician's order dated 7/11/23. Resident #288's diagnoses included Alzheimer's, and Dementia. Resident #288 did not have a care plan alerting the staff of the risk for elopement.
Review of the clinical record for Resident #26 revealed an admission date of 6/15/23 with diagnoses including Dementia. There was no care plan alerting the staff of the risk for elopement. On 7/11/23 at approximately 4:30 p.m., Resident #26 was observed in a wheelchair wandering in the hallways.
On 7/11/23 at approximately 3:00 p.m., the elopement book at the receptionist desk at the entrance of the skilled nursing facility, and the entrance of the adjoining Assisted Living Facility were reviewed. The elopement books did not include Resident #26, #288, and #287.
On 7/12/23 at 9:00 a.m., the Director of Nursing said she recommended installing a wander alert system which would automatically lock the doors when a resident with a wander alert bracelet came near an exit door. She said she did not know what the plan was for the unsecured door between the skilled nursing facility and the ALF.
On 7/12/23 at 10:30 a.m., the Director of Nursing verified the elopement books were not updated. She said Resident #26 was at risk for unsafe wandering and elopement and should have been in the book. She said the Activities Staff was responsible to update the elopement book and ensuring all residents identified to be at risk for elopement were in the books.
On 7/12/23 at 10:50 a.m., the Activities Director said she did not know her responsibilities included updating the elopement books.
On 7/14/23 at 10:30 a.m., the Administrator said he did not have any additional information related implementation of processes to ensure a safe environment, including adequate supervision of cognitively impaired residents with known exit seeking behaviors to prevent unsafe wandering and elopement.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility's administration failed to utilize its resources effectively t...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility's administration failed to utilize its resources effectively to ensure a safe environment, including adequate supervision of cognitively impaired residents with known exit seeking behaviors to prevent unsafe wandering and elopement.
On 4/1/23 at approximately 4:30 p.m., Resident #386 who was cognitively impaired, and wheelchair bound was not adequately supervised. The resident wheeled herself through an unsecured door of the skilled nursing facility into a hallway leading to the adjoining Assisted Living Facility.
Resident #386 left through the front door of the Assisted Living Facility, and traveled unsupervised in her wheelchair, approximately three tenths of a mile, and crossed two streets.
On 4/1/23 at 5:45 p.m., a staff member from a neighboring skilled nursing facility found Resident #386 wandering the streets.
Resident #386 had a likelihood for serious harm, injury, or death due to the risk for serious injury from a fall, getting lost or getting hit by a car.
The failure of the facility's Administration to provide the necessary care and services to prevent neglect, unsafe wandering, and elopement of cognitively impaired residents at risk for elopement resulted in the determination of Immediate Jeopardy at a scope and severity of isolated (J) starting on 4/1/23.
On 7/14/23 at 4:00 p.m., the facility's Administrator was informed of the determination of Immediate Jeopardy (IJ) and provided the IJ templates.
The facility census was 37 with five residents at risk for unsafe wandering and elopement.
The findings included:
Cross reference to F600, F689, and F867.
The Executive Director's job description signed on 3/31/23 specified the Executive Director is totally responsible for the management of the skilled nursing facility, ensures high quality resident care services. The job description read, . Monitor resident care on a daily basis; conduct daily rounds . Directs community safety and loss prevention program; monitors adherence to safety rules and regulations and takes remedial action when necessary .
Review of signed, not dated Director of Nursing responsibilities revealed the Director of Nursing is responsible for managing the care of residents from admission through discharge and for maintaining the delivery of quality care. Direct nursing department in the delivery of the individual patient's plan of care as well as identifying interdisciplinary needs and coordination of health care clinicians. The Director of Nursing, Understands and implements rules and regulations under Medicare . understands and implements adequate clinical patient assessments identifying specific needs of residents in the facility . Demonstrates sound, logical and timely decision making skills . Oversees incidents/accident of patients. Provides in-services as needed in areas of expertise . Scheduling ongoing training of employees .
The facility's policy for Elopement Prevention with a revised date of 6/22/2021 noted, When a resident is deemed to be an elopement risk the following measures should be put in place:
Resident should be placed in a secured unit.
A wander guard bracelet should be placed on the resident.
A Physicians order should be written to check placement of the wander guard every shift and function of bracelet daily.
Photos should be taken of the resident to be placed in the Elopement Risk book.
Communication to all staff on duty should be completed and carried on from shift to shift.
Documentation of the Elopement Risk should be made . facility Elopement Book, placed at nursing station and front entry . Elopement concerns and resident at risk should be reviewed monthly and discussed at the facility QAPI (Quality Assurance and Performance Improvement) meeting to discuss trends and concerns.
Elopement Risk Book should be reviewed daily and discusses at change of shift. Photos should be current with description of resident along with any other pertinent information that may help with locating the resident in an elopement situation.
Review of the facility's incident investigations revealed on 4/1/23 Resident #386 who was cognitively impaired, and wheelchair bound, wheeled herself through an unsecured door into a hallway leading to the adjoining Assisted Living Facility (ALF). Resident #386 left through the front door of the ALF.
The resident was last seen at the nurse's station of the skilled nursing facility at approximately 4:30 p.m.
Resident #386 traveled alone, and unsupervised in a wheelchair three tenths of a mile and crossed two streets. On 4/1/23 at 6:00 p.m., a staff member from a neighboring facility found the resident wandering the streets. Resident #1 was returned unharmed to the skilled nursing facility.
Review of the facility's investigation, and analysis of the incident revealed documentation, Upon investigation it was apparent that she (Resident #386) traveled in her wheelchair down the back hallway where the wander guard was alarming outside room [ROOM NUMBER] outside door, she then went through the double doors into the ALF. She then exited the building through the main entrance and to the road where she turned left and proceeded down Pinebrook Ave (Avenue) in her wheelchair .
Resident #386 was placed on one to one supervision and discharged to a secured unit ALF on 4/4/23.
Review of the corrective actions implemented by the facility revealed on 4/3/23 (two days after the elopement) the Regional Director of Clinical Operations educated staff for 10 minutes on responding to the wander alarm, including not turn off the alarm until all residents are accounted for.
There was no documentation Licensed Practical Nurse Staff X, Certified Nursing Assistants (CNAs) Staff CC, DD, EE, and FF who were on duty when Resident #386 eloped were educated.
On 7/11/23 the Director of Nursing provided a handwritten list of current residents identified to be at risk for unsafe wandering and elopement and wore wander guards including Residents #8, #26, #11, #287, and #288.
On 7/11/23 at approximately 3:00 p.m., the elopement book at the receptionist desk at the entrance of the skilled nursing facility, and the entrance of the adjoining Assisted Living Facility were reviewed.
The elopement books did not include Resident #26, #288, and #287.
On 7/12/23 at 11:11 a.m., CNA Staff K said she would refer to the elopement risk book at the nurse's station to identify residents at risk for unsafe wandering and elopement. She said Residents #26, #11, and #287 had wandering behaviors.
On 7/12/23 at 11:21 a.m., CNA Staff L said Residents #26, #11, and #287 had wandering behaviors. She the nurses would tell them if someone has a potential for elopement and they would have a wander guard on.
On 7/12/23 at approximately 4:00 p.m., Resident #288 was observed on the unit. He did not have a wander alert bracelet.
LPN Staff P verified Resident #288 was not wearing a wander alert bracelet as ordered. She said the resident had removed the wander alert bracelet.
Review of the clinical record for Resident #288 revealed a physician's order dated 7/11/23. Resident #288's diagnoses included Alzheimer's, and Dementia. Resident #288 did not have a care plan alerting the staff of the risk for elopement.
Review of the clinical record for Resident #26 revealed an admission date of 6/15/23 with diagnoses including Dementia. There was no care plan alerting the staff of the risk for elopement.
On 7/11/23 at approximately 4:30 p.m., the resident was observed in a wheelchair wandering in the hallways.
On 7/12/23 at 9:00 a.m., the Director of Nursing (DON) said she recommended installing a wander alert system which would automatically lock the doors when a resident with a wander alert bracelet came near an exit door. She said she did not know what the plan was for the unsecured door between the skilled nursing facility and the ALF. The DON said although she has been employed at the facility for over a year, she was not the DON at the time of the incident. She said on 5/1/23 she became the DON at the facility.
On 7/12/23 at 10:30 a.m., the Director of Nursing verified Resident #26 was at risk for unsafe wandering and elopement. She said the Activities Staff was responsible to update the elopement book and ensure all residents identified to be at risk for elopement were in the books.
Review of the Agency For Health Care Administration Background Screening Clearing House revealed the Activities Director had a date of hire of 5/8/23.
On 7/12/23 at 10:50 a.m., the Activities Director said she did not know her responsibilities included updating the elopement books.
On 7/14/23 at 10:30 a.m., the Director of Nursing verified no one ensured the elopement book risk was updated.
Review of the facility's policy and procedure for Elopement-Missing Resident revised on 10/22 noted if an employee discovers that a resident is missing from the facility, he/she should announce on the overhead paging system, Code Orange three times, the unit/area involved or the room number of the missing resident, the time the resident was determined missing.
On 7/14/23 at 10:57 a.m. Staff Q, Transporter said he did not know the overhead code for elopement.
On 7/14/23 at 11:00 a.m. Staff R, Activities Assistant said Code Orange was an emergency, You make sure everyone is in their rooms and shut the doors.
On 7/14/23 at 10:30 a.m., during a review of the facility's Quality Assurance and Performance Improvement process review, the Administrator said he did not have any additional information related implementation of processes to ensure a safe environment, including adequate supervision of cognitively impaired residents with known exit seeking behaviors to prevent unsafe wandering and elopement.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
QAPI Program
(Tag F0867)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, review of the facility's policies and procedures, and staff interviews the facility failed to develop an...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, review of the facility's policies and procedures, and staff interviews the facility failed to develop and implement appropriate corrective actions related to adequate supervision of cognitively impaired residents at risk for unsafe wandering, elopement and exit seeking behaviors.
On 4/1/23 at approximately 4:30 p.m., Resident #386 who was vulnerable, cognitively impaired, and wheelchair bound was not adequately supervised. The resident wheeled herself through an unsecured door of the skilled nursing facility into a hallway leading to the adjoining Assisted Living Facility.
Resident #386 left through the front door of the Assisted Living Facility, setting off a wander alarm, and traveled unsupervised in her wheelchair, approximately three tenths of a mile, and crossed two streets.
On 4/1/23 at 6:00 p.m., a staff member from a neighboring skilled nursing facility found Resident #386 wandering the streets.
Resident #386 had a likelihood for serious harm, injury, or death due to the risk for serious injury from a fall, getting lost or getting hit by a car.
The facility failure to implement appropriate corrective actions to prevent further incidents of unsafe wandering and elopement of cognitively impaired residents identified at risk for elopement and unsafe wandering resulted in the determination of Immediate Jeopardy (IJ) at a scope and severity of isolated (J) beginning on 4/1/23.
The Immediate Jeopardy was ongoing.
On 7/14/23 at 4:00 p.m., the facility's Administrator was informed of the determination of Immediate Jeopardy (IJ) and provided the IJ templates.
The facility census was 37 with five residents at risk for unsafe wandering and elopement.
The findings included:
Cross reference to F600, F689, and F835
The facility's Quality Assurance and Performance Improvement (QAPI) plan reviewed 2/7/2021 noted, The organizational program, established by the Medical Director and Director of Nursing and interdisciplinary Performance Improvement Committee, with support and approval from the Governing Body, shall have the responsibility for monitoring every aspect of resident care and service (including contracted services) from the time the resident enters the facility through diagnosis, treatment, recovery and discharge in order to identify and resolve any breakdowns that may result in suboptimal resident care and safety, while striving to continuously improve and facilitate positive resident outcomes . The committee shall identify quality deficiencies and develop and implement plans of action to correct these quality deficiencies, including monitoring the effect of implemented changes and making needed revisions to the action plans .
The Executive Director's job description signed by the Administrator on 3/31/23 noted the Executive Director (Administrator) oversees and monitors nursing services to ensure high quality nursing delivery systems.
The Director of Nursing Job Performance, signed (undated) noted the Director of Nursing participates in quality assurance performance improvement set and meet department goals to meet expectations of quality. Maintains knowledge and skills required to perform job.
Review of the facility's incident investigations revealed on 4/1/23 Resident #386 who was cognitively impaired, and wheelchair bound, wheeled herself through an unsecured door into a hallway leading to the adjoining Assisted Living Facility (ALF). Resident #386 left through the front door of the ALF. The resident was last seen at the nurse's station of the skilled nursing facility at approximately 4:30 p.m. Resident #386 traveled alone, and unsupervised in a wheelchair three tenths of a mile and crossed two streets. On 4/1/23 at 6:00 p.m., a staff member from a neighboring facility found the resident wandering the streets. Resident #1 was returned unharmed to the skilled nursing facility.
Review of the analysis of the incident revealed documentation, Upon investigation it was apparent that she (Resident #386) traveled in her wheelchair down the back hallway where the wander guard was alarming outside room [ROOM NUMBER] outside door, she then went through the double doors into the ALF. She then exited the building through the main entrance and to the road where she turned left and proceeded down Pinebrook Ave (Avenue) in her wheelchair.
Review of the corrective actions implemented by the facility to prevent recurrence of unsafe wandering and elopement revealed:
Resident #386 was placed on one to one supervision and discharged to a secured unit ALF on 4/4/23.
On 4/3/23 (two days after the elopement) the Regional Director of Clinical Operations educated staff for 10 minutes on responding to the wander alarm, including not turn off the alarm until all residents are accounted for. There was no documentation Licensed Practical Nurse Staff X, Certified Nursing Assistants (CNAs) Staff CC, DD, EE, and FF who were on duty when Resident #386 eloped were educated.
There was no documentation the facility-initiated elopement drills on all shifts, including weekends to verify staff understood the education and responded appropriately to the wander alarm when activated.
On 7/11/23 at approximately 5:50 p.m., the door connecting the skilled nursing facility to the ALF remained unsecured. It was not equipped with an alarm to alert staff to unsafe wandering.
On 7/11/23 at approximately 10:35 a.m., the Director of Nursing provided a handwritten list of current residents identified to be at risk for unsafe wandering and elopement, including Residents #8, #26, #11, #287, and #288. She said residents #8, #26, #11, #287, and #288 wore a wander alert bracelet to alert staff of unsafe wandering and attempt at elopement.
Review of the clinical record for Resident #26 revealed an admission date of 6/15/23 with diagnoses including Dementia. There was no care plan alerting the staff of the risk for elopement. On 7/11/23 at approximately 4:30 p.m., the resident was observed in a wheelchair wandering in the hallways.
On 7/11/23 at 5:54 p.m., the alarm of a door equipped with a wander alarm system was triggered to observe the staff response to the alarm.
On 7/11/23 at 5:57 p.m., CNA Staff AA started closing all residents' bedroom doors in response to the alarm. She said, I thought it was a fire alarm. Staff AA did not investigate or look around to see if Residents #11, #287, and #288 identified to be at risk for elopement and wore a wander alarm had left the facility.
Review of the 10 minutes in-service related to wanderguards dated 4/3/23 lacked documentation CNA AA with a date of hire of 1/12/23 attended the in-service which specified, If anyone hears this alarm they are to investigate it immediately. Look around do you see a resident with a white bracelet and alarm? Look outside, if there is a resident outside who has on a white bracelet and alarm.
On 7/11/23 at 6:00 p.m., five minutes after the alarm was triggered, Licensed Practical Nurse (LPN) Staff P turned off the alarm, and said, The alarm means it is an elopement risk. She looked out the door and said she did not see anyone. She did not initiate a count of the residents to ensure all cognitively impaired residents including Residents #8, #26, #11, #287, and #288 were accounted for. Staff P said she did not respond to the alarm quickly because she could barely hear anything, especially in the dining room with the clanking of the dishes.
LPN Staff P attended the in-service on 4/3/23 and did not follow the procedure outlined in the in-service which specified, You can not turn [sic] off the alarm until you know that all residents are accounted for.
No staff present on the unit looked at the unsecured double door leading to the ALF where Resident #386 eloped from.
Review of the facility's policy for Elopement Prevention with a revised date of 6/22/2021 noted photos of residents at risk for elopement should be taken and placed in the Elopement Risk book.
On 7/11/23 at approximately 3:00 p.m., the elopement book at the receptionist desk at the entrance of the skilled nursing facility, and the entrance of the adjoining Assisted Living Facility were reviewed. The elopement books did not include Resident #26, #288, and #287.
On 7/12/23 at 9:00 a.m., the Director of Nursing said she recommended installing a wander alert system which would automatically lock the doors when a resident with a wander alert bracelet came near an exit door. She said she did not know what the plan was for the unsecured door between the skilled nursing facility and the ALF.
On 7/12/23 at 9:31 a.m., the DON said she was the designated Risk Manager. She said she was not involved in developing a performance improvement plan for elopement. She said, The Administrator would know that. She said, I told them I thought the doors were the cause of the elopement in the QAPI (Quality Assurance and Performance Improvement) meetings.
On 7/12/23 at 10:30 a.m., the Director of Nursing said the Activities Staff was responsible to update the elopement book and ensure all residents identified to be at risk for elopement were in the books.
On 7/12/23 at 10:50 a.m., the Activities Director who had a date of hire of 5/8/23 said she did not know her responsibilities included updating the elopement books.
On 7/12/23 at approximately 4:00 p.m., Resident #288 who had a physician's order for a wander alert bracelet was observed on the unit. He did not have a wander alert bracelet.
On 7/14/23 at 10:30 a.m., during a review of the facility's Quality Assurance and Performance Improvement (QAPI) process review, the Administrator presented an elopement drill QAPI worksheet dated 4/1/23 which noted, Time in: 6:00 p.m. There was no Time out noted on the worksheet. The comment noted Education on door alarms for all SNF (Skilled Nursing Facility), ALF (Assisted Living Facility) and entire building staff and elopement
At the time of the survey there were 39 active nursing staff (Licensed Nurses and Certified Nursing Assistants) employed at the facility. There was no documentation 24 of the 39 had received elopement prevention training since the elopement incident of 4/1/23.
An elopement Drill QAPI worksheet dated 5/23/23 at 11:20 a.m. to 11:32 a.m. consisted of a check mark placed next to each item on the list. The form noted after the drill is completed, review drill with staff, provide feedback and answer questions, staff to sign in-service sheet. There was no documentation the drill was reviewed, who participated and feedback.
Review of the QAPI minutes for the May 2023 meeting noted an elopement drill was held on 5/23/23 on the day shift with 100% accuracy in action and response time. There was no discussion of the unsecured SNF door to prevent further incidents of unsafe wandering into the ALF and elopement.
The Administrator presented an undated document titled, Performance Improvement Plan-Life Safety and Clinical Operations
The document listed the following Issues:
Elopement Drills and Process. Solution: Life Safety Director and Clinical Director will work together in submitting Elopement audits to QAPI Committee monthly. The project was ongoing and X entered on the Completed column.
Monitoring. Monthly education will be provided to staff on the elopement procedures with an X entered in the column, indicating the monthly education was completed.
QAPI. Audit results will be brought to QAPI had an X entered indicating the audit results were brought to QAPI. The Administrator only had documentation of the check off Elopement drill QAPI worksheet completed on 5/23/23. There was no sign in sheet making it impossible to determine who participated in the drill.
On 7/14/23 at 10:30 a.m., the Administrator said he did not have any additional information related implementation of processes to ensure a safe environment, including adequate supervision of cognitively impaired residents with known exit seeking behaviors to prevent unsafe wandering and elopement.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on record review, review of the facility's policies and procedure, and staff interviews the facility failed to submit an immediate report for an elopement, which could be considered neglect, to ...
Read full inspector narrative →
Based on record review, review of the facility's policies and procedure, and staff interviews the facility failed to submit an immediate report for an elopement, which could be considered neglect, to the State Survey Agency and adult protective services in accordance with State law for 1 (Resident #386) of 3 incidents reviewed.
The findings included:
Cross reference to F600 and F689
The facility's abuse policy, section resident rights, revised 10/23/22 noted, The facility has designed and implemented processes, which strive to ensure the prevention and reporting of suspected or alleged resident/patient . neglect . Neglect. Failure to provide goods or services necessary to avoid physical harm, mental anguish, or mental abuse . Reporting . Notify the local law enforcement and appropriate State Agency(s) immediately (no later than 2 hours after allegation/identification of allegation) by Agency's designated process after identification of alleged/suspected incident .
Review of the facility's incidents investigations on 4/1/23 at approximately 4:30 p.m., revealed Resident #386, who was cognitively impaired, identified to be at risk for unsafe wandering and elopement, and wheelchair bound was not adequately supervised.
The resident wheeled herself through an unsecured door of the skilled nursing facility into a hallway leading to the adjoining Assisted Living Facility.
Resident #386 left through the front door of the Assisted Living Facility, and traveled unsupervised in her wheelchair, approximately three tenths of a mile, and crossed two streets.
Staff was not aware the resident was missing for approximately one hour and 45 minutes.
On 4/1/23 at 5:45 p.m., a staff member from a neighboring skilled nursing facility found Resident #386 wandering the streets.
There was no documentation the facility reported the neglect to the State Survey Agency within 24 hours as required, or Adult Protective Services.
On 7/12/23 at 10:30 a.m., the Director of Nursing said she had no idea why Adult Protective Services was not notified of the elopement incident.
On 7/14/23 at 3:24 p.m., the Director of Nursing said, a federal report for elopement should have been done.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, resident and staff interviews, the facility failed to ensure resident care plan meeting/conference was c...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, resident and staff interviews, the facility failed to ensure resident care plan meeting/conference was conducted with the resident and/or their representative after completion of the comprehensive admission Minimum Data Set (MDS) assessment for 2 (Resident #29 and #25) of 5 sampled residents. This did not allow the resident and/or their representative to participate in decision-making related to their plan of care and ensure the resident's care plan had the required information.
The findings included:
1. On 7/10/23 at 10:26 a.m., during an interview with Resident #29, he said he was not invited to his care plan meeting. Resident #29 said because he was not invited to his plan of care meeting, he did not know what the Interdisciplinary Team (IDT) had determined his plan of care would be while he is at the facility.
On 7/12/23 a review of Resident #29's medical records revealed he was admitted to the facility on [DATE] with a diagnosis of pathological left femur fracture, and abnormalities of gait and mobility. The Comprehensive admission Assessment was completed and finalized on 6/28/23. A review of Resident #29's plan of care revealed they were completed by 7/6/23. Further review of Resident #29's medical records revealed no documentation Resident #29 had attended or was invited to participate in decision-making related to the completion of his plan of care.
2. On 7/10/23 at 11:01 a.m., during an interview with Resident #25's husband, he said since his wife's admission to the facility, he had asked multiple staff members about the plan of care related to his wife's stay at the facility. He said no one had kept them updated about the plan of care for his wife and he told them he wanted to meet with the case manager and the IDT related to his concerns about his wife's care at the facility.
On 7/12/23 a review of Resident #25's medical records revealed she was admitted to the facility on [DATE] with a diagnosis of fracture to left hip, joint replacement surgery, infection of the left hip, Hypertension, abnormalities of gait and mobility, altered mental status and unspecified dementia. An Attestation of Incapacity form was completed and signed by the physician on 6/19/23 for Resident #25.
Further review of Resident #25's plan of care revealed they were reviewed and initiated by the IDT on 6/20/23 and 6/26/23. Resident #25's medical records revealed no documentation Resident #25 and/or Resident #25's husband had attended or were invited to attend Resident #25's IDT care plan meeting on 6/26/23.
3. On 7/13/23 review of the Clinical Operations for Care Plans, policy #CC-21 created 7/2018 and last revised 1/2023 stated each resident of the facility shall be involved in the development and review of their plan of care along with their family member. Residents, family members or other responsible people should be invited to attend the interdisciplinary conference.
4. On 7/13/23 at 9:44 a.m., in an interview with the Minimum Data Set (MDS)/Care Plan Coordinator, she said she liked to complete the resident's baseline care plan within 48 hours of admission and tried to meet with the IDT to finalize the resident's full care plan within 7 to 10 business days of the resident's admission to the facility. The MDS Coordinator said the comprehensive plan of care is required to be developed within 7 days after the completion of the comprehensive assessment. The MDS Coordinator confirmed the facility's Care Plans policy stated each resident or family member or responsible people should be invited to attend the development and review of the resident's plan of care while at the facility.
On 7/13/23 at 9:50 a.m., the MDS Coordinator reviewed Resident #25's medical record and confirmed Resident #29's last admission to the facility was on 6/09/23. She said Resident #25's baseline care plan was completed on 6/12/23 and the full care plan was finalized by the IDT on 6/26/23. She said she was unable to find documentation Resident #25 and/or her husband were invited and participated in the development of the plan of care for Resident #25 on 6/26/23 as required.
On 7/13/23 at 10:08 a.m., the MDS Coordinator, after she reviewed Resident #29's medical record, confirmed the resident was admitted to the facility on [DATE]. She said Resident #29's baseline care plan was completed on 6/22/23 and she completed the Comprehensive admission Assessment on 6/28/23. The MDS Coordinator said Resident #29's plan of care was completed within seven days of the Comprehensive admission Assessment, but she was unable to find documentation Resident #29 was invited and/or participated in the development of his plan of care as required.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to implement individualized, care planned interventions ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to implement individualized, care planned interventions to prevent the decline in range of motion for 2 (Resident #15, and #21) of 2 sampled residents with limited range of motion.
The findings included:
1. Resident #15 was admitted to the facility on [DATE]. Diagnoses included as of 8/11/22 hemiplegia (Paralysis on one side of the body) related to a cerebral vascular accident (stroke), and Parkinson's disease as of 2/22/19.
Observation on 7/11/23 at 12:15 p.m., showed Resident #15's fourth and fifth fingers of both hand were contracted, pointing downwards toward the palm of his hands.
Resident #15 said he did not have any splints or other device to keep his hands open.
Clinical Record review showed the admission Minimum data Set (MDS) assessment dated [DATE] noted Resident #15 was admitted from an acute care hospital. Resident #15's cognition was moderately impaired with a Brief Interview of Mental Status (BIMS) score of 11. The MDS noted Resident #15 had no functional limitation in Range of Motion to his upper extremities and started physical therapy on 5/1/23.
Review of Resident #15's care plan initiated on 5/5/23 showed Resident #15 has a deficit in his activities of daily living self-care with performance deficit related to limited mobility. Interventions as of 6/9/23 included applying a palm roll in the left hand to prevent contractures.
On 7/12/23 at 11:48 a.m., the Director of Physical Therapy (PT) said she started employment at the facility a month ago. She verified Resident #15's hands were both contracted. The Director of Physical Therapy said Resident #15 was supposed to wear an orthotic device (An artificial appliance that supports the body part for the purpose of stabilization, support, or movement reminder) to both hands.
On 7/12/23 at 11:55 a.m., The PT director said Resident #15's orthotic devices were shaped and looked like carrots. The PT director searched the resident's room and was not able to locate the orthotic devices.
On 7/13/23 at 1:00 p.m., Resident #15's nephew said he was concerned because the facility was not doing anything to keep his hands functioning. The nephew said Resident #15 used to have splints for his hands when he resided at an Assisted Living Facility. He said since his admission to the nursing home, he has not been wearing any splints.
On 7/14/23 at 10:00 a.m., the Medical Director verified Resident #15 had contractures in both his hands and he should be receiving services to prevent further decline to his hands.
On 7/14/23 at 3:00 p.m., the MDS Coordinator verified Resident #15 had not been assessed and care planned appropriately for the contractures of his hands.
On 7/14/23 at 4:00 p.m., the Restorative Aide said she had seen the resident with carrots (orthotic device) in his hands a month ago.
2. Resident #21 was admitted to the facility from the hospital on [DATE]. Resident #21 has a history of Cerebral vascular Accident (Stroke), hypertension, Diabetes Mellitus, depression and anxiety.
The Quarterly MDS dated [DATE] showed Resident #21 has a BIMS of 13 which show intact cognition. Resident #21 had no rejection of care behaviors. Resident #21 had function limitations in range of motion on one side on both his upper and lower extremities.
On 7/10/23 at 4:12 p.m., Resident #21 was observed in his bed. The resident was observed to have contractures to his right hand. Resident #21 was not to able to straighten the fourth and fifth finger of his right hand. The resident had some movement observed on the first and second fingers of the right hand. The resident stated his right leg was contracted. The resident said he did not get assistance from staff with range of motion exercises. The resident stated he did not have a splint for his hand. The resident stated if he had a splint he would wear it.
Resident #21's Care plan read, The resident has limited physical mobility r/t [related to] Stroke. Has right sided weakness. Receives restorative nursing to maintain abilities. Res [Resident] has refused restorative program DC'd [discontinued] Date initiated:11/21/20 Revision on:10/16/22.
The last intervention listed in the care plan was to report any decline or pain which was initiated on 4/27/21. The care plan did not list any orthotics to the resident's right hand or leg. There was no revision to the interventions since 5/20/21. The goal listed in the care plan was, The resident will demonstrate improved performance ADL (activities of daily living) ability as he regains strength. This goal was initiated on 11/21/20 and was revised on 4/14/23 with a target date of 7/10/23.
On 7/12/23 at 12:20 p.m., the Director of PT said Resident #21 should be receiving restorative. The PT director stated the resident should have a splint for his hand and a brace for leg in place. She stated Occupational Therapy was going to pick up the resident for services and they would be assessing the resident's mobility needs.
An active physician's order dated 12/28/20 reads, apply right wrist brace No directions were specified in the order.
Documentation provided by the facility listed as Nursing Rehab/Restorative Program Record showed the restorative program was discontinued on 5/3/21 due to resident refusal of care.
Further documentation showed Restorative continued from 1/12/22 through 7/21/22. The documentation showed the resident was declining to participate in restorative and to wear wrist splint and leg brace. There was no nursing assessment related to the resident's refusal of care.
On 7/14/23 at approximately 10:00 a.m., Resident #21 was observed coming out of the therapy room in his wheelchair. He was wearing a right leg brace. The resident appeared comfortable and compliant with the brace.
On 7/14/23 at 2:45 p.m., the PT director said staff found the resident's wrist brace, but it was not unusable, and another brace had been ordered.
On 7/14/23 at 4:00 p.m., the Restorative Aide said she knew Resident #21, and he was compliant with restorative, but he got to where he would not let her touch him. She stated the resident would be in pain with any movements. She stated she reported this to the nursing staff. They finally ended up discontinuing restorative. The Restorative Aide said she did not know if nursing put any interventions in place to reduce the resident pain during restorative.
On 7/14/23 at 4:30 p.m., the Director of Nursing (DON) said the resident's restorative had been stopped due to noncompliance. She was not the DON at the time the restorative was stopped, and she could not say if nursing assessed the reason for refusal of restorative services.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, staff, resident, and family interview, the facility failed to provide nutritional ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, staff, resident, and family interview, the facility failed to provide nutritional interventions and physician's orders to prevent weight loss for 1 (Resident #7) of 1 resident identified at risk for compromised nutrition and weight loss.
The findings included:
Clinical record review revealed Resident #7 was admitted to the facility on [DATE]. The admission Minimum Data Set (MDS) assessment dated [DATE] noted diagnoses of non-Alzheimer's dementia, hypertension, Parkinson's Disease, Dysphagia (swallowing difficulties), and cognitive communication deficit. The MDS noted the resident was receiving a mechanically altered diet (change in texture of food and/or liquids).
The clinical record noted Resident #7 had an allergy to shellfish which was not listed on the meal ticket.
The Care area assessment dated [DATE] indicated Resident #7's BMI (Body Mass Index) was too low (17) (Body Mass Index less than 18.5 indicates the resident is at nutritional risk), and the resident required a therapeutic diet.
The Care plan initiated 6/9/2023 indicated the resident has a nutritional problem related to diagnoses of dementia, altered mental status, Parkinson's disease, required a therapeutic diet, history of weight loss. The goal initiated 6/9/2023 was The resident will maintain adequate nutritional status as evidenced by maintaining weight without significant weight changes.
Interventions included to record/report signs or symptoms of malnutrition, significant weight loss: 3 pounds (lbs.) in 1 week, greater than 5% in 1 month, greater than 7.5% in 3 months, greater than 10% in 6 months; Provide and serve supplements as ordered; Provide, serve diet as ordered; Monitor intake and record every meal; RD (Registered Dietitian) to evaluate and make diet change recommendations.
The resident weight flow sheet revealed on 5/2/23 Resident #7 weight was 97.0 lbs.
The admission Minimum Data Set (MDS) assessment dated [DATE] noted the resident's height to be 5 feet, 3 inches.
On 5/5/23 the physician ordered a house shake supplement, 90 milliliters (ml's.) three times daily.
On 6/4/23 the resident's weight was documented to be 90.0 lbs. which indicated a significant weight loss of 7.2 % in 30 days.
The Registered Dietitian (RD) documented in a progress note date 6/9/23, Resident #7 weight triggered for loss for 1 week, 1 month. RD to increase house shake from three times daily to four times daily and discuss potential for appetite stimulant with physician.
On 6/10/23 the house shake was increased to four times a day.
On 7/5/23, the resident's weight was documented as 88.5 lbs.
The RD quarterly evaluation dated 7/7/23 noted resident remained underweight and triggered for significant weight loss x 3 months. Resident #7 was dependent on staff for meals.
On 7/11/23 at 1030 a.m., Resident #7's private duty Certified Nursing Assistant (CNA) stated she works with the resident two days a week. She feeds Resident #7, offers food, and fluids. Resident #7 will eat at least half of what the facility provides for meals and is offered extra fruits and vegetables that she likes and eats all of. The CNA said, I used to see the supplement on her tray but have not seen it for a couple of months. She's lost a lot of weight.
On 7/12/23 at 11:44 a.m., Resident #7 was observed in bed, dressed in a hospital gown. There was no food or drink at the bedside. The resident looked thin.
On 7/12/23 at 3:11 p.m., Licensed Practical Nurse (LPN) Staff P stated we have been out of the house shake for about three weeks. She stated she has been documenting it in the records but has not had any for some time.
On 7/12/23 at 3:29 p.m., the Director of Food and Nutrition Services said no one had provided house shakes to the nursing unit. Anyone can take them, but no one has for a while.
On 7/13/23 at 11:16 a.m., the physician stated he had not been informed the resident was not receiving the supplements and would have liked to have known.
On 7/13/23 at 11:20 a.m. during a telephone interview, the RD stated she works remotely one day per week, she does not physically come to the facility. The RD verified Resident #7 had lost weight. She confirmed resident #7 had lost 9.5 pounds or 8.76 percent. The RD stated, I let the Director of Nursing know on 6/28/23, last week, and on July 7th, the nurses were charting the supplement was not available, or on order, so the resident was not getting it.
On 7/13/23 5:55 p.m., CNA Staff T was observed feeding the resident while in bed. There was no house shake on the tray, as listed on the meal ticket. Staff T, CNA stated she just gets it at lunch not dinner.
On 7/13/23 at 5:58 p.m., Dietary Aide staff V said she didn't know what the house shakes were. She opened the pantry refrigerator, held a house shake container and asked, this is it? while holding the house shake container. She stated she did not put house shakes on any trays.
On 7/13/23 at 6:00 p.m., the DON was observed checking trays and tickets and stated she has not put any house shakes on trays. She stated she did not see it on the meal ticket and did not realize it had been added to the meal tickets.
On 7/14/23 at 9:38 a.m., the physician stated during a follow up telephone interview the lack of shakes may not have caused the weight loss, but it definitely did not help that she did not receive the shakes.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, resident and staff interviews, the facility failed to ensure ongoing communication between the nursing f...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, resident and staff interviews, the facility failed to ensure ongoing communication between the nursing facility and the dialysis center related to the phyiscal assessment of a dialysis resident before, during, and after each dialysis treatment for 1 (Resident #17) of 1 resident receiving dialysis.
The findings included:
The facility policy CD-3, Dialysis Management revised 10/2022 stated Residents receiving hemodialysis treatments [a procedure whree a dialysis macing and a special filter called an artificial kidney, or a dialyzer, are used to clean the blood] will be assessed and monitored to ensure quality of life and well-being.
The procedure included the following information. On admission the resident will be assessed to determine [hemodialysis] access type. The site will be observed for function and signs and symptoms of infection.
The nurse will obtain orders for monitoring of site, and interventions as appropriate.
Facility will establish open communication with the Residents Dialysis center utilizing a Dialysis Communication Book completing the Dialysis Communication form CD-3A.
The nurse will establish pre-dialysis vital signs (Blood pressure, pulse, temp, respirations).
On return from the Dialysis Center, the nurse will review the communication returning from the Dialysis Center. The nurse should review specifically, pre and post vital signs, treatment tolerance, any medications given and any new orders for resident care.
The nurse will evaluate the resident post dialysis for mental status, pain, access site condition and response to treatment.
The nurse will document findings in the nurses note.
The facility policy CW-3, Weight assessment and interventions revised 5/2019 stated Residents receiving Hemodialysis treatment should be weighed pre and post treatment at dialysis. Post weights should be recorded in the Residents' medical record (Electronic Health Record) upon return from hemodialysis by their licensed nurse.
On 7/11/23, clinical record review noted Resident #17 was admitted to the facility on [DATE]. The diagnoses included End Stage Renal (kidney) Disease and required Hemodialysis, Anemia, Stroke, Stage 4 pressure ulcer of the sacrum.
The admission Minimum Data Set with a target date of 6/18/23 noted the resident's cognition was intact with a Brief Interview for Mental Status of 15. Resident #17 required the assistance of one person for transfer and mobility.
The Physician order with an effective date of 6/13/23 noted the resident required Dialysis every Tuesday, Thursday, and Saturday (the resident received dialysis at a dialysis center).
Resident #17's care plan initiated on 6/13/23 for hemodialysis included the following interventions to be completed by nursing staff.
Potential for complications related to hemodialysis for diagnosis of End Stage Renal Failure.
Coordinate resident's care in collaboration with dialysis center.
Observe and report to physician complications related to renal failure: Edema/fluid overload; Respiratory difficulty/shortness of breath; Increased weakness, changes in mental status; changes in vital signs.
Weigh resident as ordered and notify physician of significant weight changes.
The Electronic Health Record review revealed Hemodialysis Communication Forms were not completed for the resident on 6/13/23, 6/15/23, 6/20/23,6/22/23,6/24/23 and 6/29/23. The dialysis center did not document Resident #17's pre and post dialysis vital signs, any resident complications during dialysis, nutritional concerns, medication given during dialysis treatment, laboratory values, post-dialysis instructions and any new physician orders for those treatment days.
On 7/10/22 at 4:54 p.m., Resident #17 said she goes to the dialysis center on Tuesday, Thursday, and Saturday. She said the nursing facility and dialysis center do not always communicate with each other. She said she did not carry a dialysis binder or bring any hemodialysis communication form from the dialysis center and back to the nursing facility after dialysis.
On 7/12/23 at 12:00 p.m., Staff P, Licensed Practical Nurse (LPN) stated Resident #17 goes to dialysis on Tuesday, Thursday, and Saturday. She did not know about a dialysis book but does send the resident to dialysis with a face sheet. She verified the resident had not returned with any communication forms from the dialysis center.
On 7/12/23 at 12:01 p.m., Staff W, Registered Nurse (RN) stated she was not sure but there should be a dialysis book, every facility has one.
On 7/12/23 at 4:50 p.m., the Director of Nursing (DON) stated there was no contract between the facility and the dialysis center. Dialysis is coordinated by nephrologist, dialysis, and patient. We are not involved in it. The care coordination with dialysis is confirmed prior to admission and transportation is arranged by us for Tuesday and Thursday and she takes the public bus on Saturdays. There is a dialysis hand off sheet that is done during the week but there is no copy retained for the record and it is not completed on Saturdays. Dialysis does not send any updates back. The DON said she has not done any training with the nurses regarding dialysis access site assessment, dressing removal, assessing for bruit or thrill [a whooshing or swishing sound caused by turbulent blood flow through an artery], it is not part of a competency assessment or skills check. If the dressing is soiled or saturated, we call 911. I've never checked to see if nurses have documented they assessed the access site for bleeding or complications after dialysis. The DON stated Resident #17 does not have a book to take back and forth to dialysis for communication. The DON verified the Dialysis center has not called to give any updates on resident #17 since admission to the facility.
On 7/13/23 at 11:34 a.m., The Registered Dietitian (RD) stated she left a message for the Dialysis Dietitian on 6/30/23. The RD stated there was no communication with the dialysis center between 6/12/23 to 6/30/23 when the first message was left. I was not working because dietary services had been stopped at the nursing facility.
On 7/13/23 at 2:08 p.m., Resident #17 stated she had been back from dialysis since 12:30 p.m. The resident stated her vitals and dressing were not checked prior to going to dialysis and since being back no one had checked her vital signs or dressing.
On 7/14/23 at 11:50 a.m., The DON stated no specific order had been entered for the dialysis access site monitoring and assessment. The DON stated her expectation was that vital signs be checked for a resident both pre and post dialysis visits and confirmed the nurses have not checked the vital signs for this resident both prior to and following dialysis. The DON confirmed post dialysis weights have not been recorded in the electronic health record. The DON verified these items are listed in the dialysis management and weights policy.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview, and record review the facility failed to complete performance reviews for 3 (Certified Nursing Assistants Staff G, Staff E, and Staff F) of 3 Certified Nursing Assistants (CNAs) su...
Read full inspector narrative →
Based on interview, and record review the facility failed to complete performance reviews for 3 (Certified Nursing Assistants Staff G, Staff E, and Staff F) of 3 Certified Nursing Assistants (CNAs) surveyed for performance review.
The findings included:
Review of the current staff list provided by the facility revealed CNA Staff G had a date of hire of 9/16/21, CNA Staff E had a date of hire of 5/6/21, and CNA Staff F had a date of hire of 5/20/21.
On 7/14/23 at 12:00 p.m., 2:00 p.m., a request was made to the Administrator for documentation of the annual performance review for CNAs Staff G, E, and F.
On 7/14/23 at 4:00 p.m., an additional request was made to the Administrator in training for documentation of the annual performance review for CNAs. Staff G, E, and F.
As of the exit date of 7/16/23, the facility's administration did not provide documentation verifying CNAs. Staff G, E, and F had an annual performance review completed.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
5. On 7/12/23 a review of the Medication Regimen Review for Resident #13 revealed a consultant pharmacist's recommendation dated 6/13/23 that read, The resident is receiving both Escitalopram and Bupr...
Read full inspector narrative →
5. On 7/12/23 a review of the Medication Regimen Review for Resident #13 revealed a consultant pharmacist's recommendation dated 6/13/23 that read, The resident is receiving both Escitalopram and Bupropion for depression. Could you please consider a gradual dose reduction of Bupropion with the hopeful possibility of eventually eliminating this drug?
On 6/30/23 the APRN agreed with the recommendation.
On 7/12/23, a review of Resident #13's medical record revealed the resident was still receiving Bupropion 75 mg once daily.
On 7/12/23 at 10:18 a.m., the DON confirmed the APRN agreed to the dose reduction of the Bupropion recommended by the consultant pharmacist, but it had not been changed in the Resident #13's medical record.
Based on record review, policy review, and staff interviews, the facility failed to ensure medication irregularities and/or concerns were addressed in a timely manner when the consultant pharmacist identified irregularities and/or medication concerns, for 3 (Residents #11, #13 and #25) of 5 resident's medication regimens which were reviewed.
The findings included:
1. On 7/12/23 a review of the consultant pharmacist's monthly medication review for Resident #25 revealed on 5/16/23 he recommended a GDR (gradual dose reduction) be attempted for Buspirone 10 milligrams (mg) once daily for anxiety to Buspirone 7.5 mg once daily for anxiety.
On 6/13/23 the consultant pharmacist recommended a GDR be attempted for Escitalopram 10 mg once daily for depression to Escitalopram 5 mg once daily for depression for Resident #25.
On 6/30/23 Resident #25's Advanced Practice Registered Nurse (APRN) agreed with the consultant pharmacist's recommendation to lower the Escitalopram to 5 mg daily for depression.
A review of Resident #25's medical record revealed Resident #25 was currently receiving Buspirone 10 mg once daily for anxiety and Escitalopram 10 mg once daily for anxiety.
Further review of Resident #25's medical record revealed no documentation Resident #25's primary care physician (PCP) had reviewed and acted upon the consultant pharmacist's recommendation for a GDR of Buspirone 10 mg on 5/16/23. The facility did not decrease Escitalopram to 5 mg as recommended by the consultant pharmacist and agreed upon by the APRN on 6/30/23.
2. On 7/12/23 a review of the consultant pharmacist's monthly medication review for Resident #11 revealed on 2/14/23 he recommended a GDR be attempted for Sertraline 100 mg in the afternoon for depression once daily to Sertraline 75 mg in the afternoon for depression.
On 3/14/23 the consultant pharmacist recommended the Benzonatate Pearls 100 mg by mouth every 8 hours, as needed for cough be discontinued to minimize the potential of unwanted side effects which could be severe drowsiness or dizziness, confusion, hallucinations, ongoing numbness or tingling in your mouth, throat, or face, numbness in your chest or a choking feeling.
Further review of Resident #11's medical record revealed Resident #25 was currently receiving Sertraline 100 mg for depression and Benzonatate Pearls 100 mg as needed for cough. There was no documentation Resident #11's PCP (Primary Care Physician) had reviewed the consultant pharmacist's recommendations for a GDR for the Sertraline 100 mg on 2/14/23 and the discontinuation of the Benzonatate Pearls on 3/14/23 as required.
3. Review of the Pharmacy Consultant Medication Review, Policy # C_MED_27 created on 7/2018 and revised 1/2023 stated a licensed pharmacist (pharmacy consultant), would review the medication regimen review (MRR) for each resident at least monthly and more frequently, as needed. The consultant pharmacist would review each medication regimen of all residents in the facility once per month for supporting diagnosis, allergy conflicts, pertinent orders, contraindications between medications, identifying adverse consequences . and gradual dose reductions attempted. The Pharmacy Consultant should report irregularities to the attending physician, medical director, and Director of Nursing (DON) with the resident's medication regimen review. The DON would give the Unit Manager/designee a copy of the monthly pharmacy consultant reports. The Unit Manager/designee was responsible to ensure all recommendations are acted upon, all recommendations are reported to the resident physicians, there was documentation in the resident medical record that notification and follow-up occurred, notify the resident's physician of the pharmacy consultant's recommendations and document in the resident's medical record that the recommendation was completed, and remind the resident's physician to sign the resident's consultant report that was filed in the resident's medical record. The Unit Manager/designee would return the copy of the consultant's report to the DON when notifications, follow-ups, and documentation had been completed. The DON would notify the facility's medical director if the resident physician did not follow through on the consultant's recommendations.
4. On 7/11/23 at 4:10 p.m., the Director of Nursing (DON) said she was responsible to print all the monthly consultant pharmacist recommendations and give them to the residents' PCP for their review and ensure any physician orders related to the consultant pharmacist recommendations were implemented timely.
On 7/12/23 at 10:12 a.m., the DON confirmed, after reviewing Resident #11's medical record, the consultant pharmacist had recommended on 2/14/23 for a GDR be attempted for Sertraline 100 mg for depression and on 3/14/23 the discontinuation of Benzonatate Pearls 100 mg as needed for cough. The DON confirmed Resident #11 was currently receiving those medications and the GDR was not done for the Sertraline 100 mg and the Benzonatate Pears 100 mg was not discontinued as requested.
The DON said she was unable to find documentation the consultant pharmacist recommendations on 2/14/23 and 3/14/23 were reviewed by Resident #11's physician, the pharmacy consultant report was signed by the physician as reviewed, and a copy of the signed report was placed in the resident's medical record as required.
The DON confirmed the consultant pharmacist had written on 5/16/23 for a GDR to be attempted for Buspirone 10 mg once daily for anxiety to Buspirone 7.5 mg once daily for anxiety.
On 7/12/23 at 10:18 a.m., the DON confirmed, after a review of Resident #25's medical record, the consultant pharmacist had recommended on 6/13/23 for a GDR to be attempted for Escitalopram 10 mg once daily for depression to Escitalopram 5 mg once daily for depression, which the APRN confirmed and wrote to lower the Escitalopram to 5 mg on 6/30/23.
The DON said she was unable to find documentation the consultant pharmacist recommendations on 5/16/23 were reviewed by Resident #25's physician, the pharmacy consultant report was signed by the physician as reviewed, and a copy of the signed report was placed in the resident's medical record as required. The DON said the pharmacist consultant's recommendation to lower the Escitalopram to 5 mg and signed by the APRN on 6/30/23 to lower the Escitalopram to 5 mg was not implemented on 6/30/23 as ordered by the APRN.
On 7/12/23 at 11:18 a.m., during an interview with the Consultant Pharmacist, he said he reviewed all facility resident's medication regimes at least every month to include supporting diagnoses for each medication, allergy conflicts, pertinent orders, contraindications between medications, identifying adverse consequences . and request for a gradual dose reduction as per federal and state guidelines. He said he met with the DON every month and she was responsible to ensure each resident's primary care physician reviewed all recommendations, ensured the physician signed the recommendations, and placed the physician signed review of the recommendation into the resident's medical record. He said if there were any physician orders and/or recommendations, the DON was responsible to ensure they were acted upon in a timely manner.
The consultant pharmacist confirmed he had recommended a GDR for Resident #25 on 5/16/23 and 6/13/23, and he had recommended a GDR for Resident #11 on 2/14/23 and a recommendation to discontinue medication on 3/14/23. He said he was not informed by the DON that his recommendations for Residents #11 and #25 were not reviewed by their physician and/or implemented as ordered by their physician.
On 7/14/23 at 9:40 a.m., in an interview with the facility's Medical Director, he said the DON was responsible to ensure all consultant pharmacy medication review recommendations were given to the resident's primary care physician for review and to ensure all physician orders and/or physician request were implemented in a timely manner as required in their Pharmacy Consultant Medication Review, policy #C-Med-27.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observations, record review, and staff interviews, the facility failed to ensure no greater than 5% medication error rate. 38 opportunities with 5 errors were observed resulting in a 13.16% m...
Read full inspector narrative →
Based on observations, record review, and staff interviews, the facility failed to ensure no greater than 5% medication error rate. 38 opportunities with 5 errors were observed resulting in a 13.16% medication error rate.
The findings included:
On 7/14/23 at 8:15 a.m., Licensed Practical Nurse (LPN) Staff P was observed administering 13 different medications to Resident #16.
Upon reconciliation of the observation with the physician's orders, it was revealed in addition to the 13 medications administered, an order to administer Lorazepam (medication used for anxiety) 0.5 milligram (mg) one tablet by mouth two times a day, hold for sedation.
The morning Lorazepam was scheduled for 9:00 a.m. Staff P was not observed administering the Lorazepam to Resident #16 as ordered.
The physician's orders also included Cyanocobalamin (Vitamin B12) 1000 micrograms (mcg) one tablet by mouth one time a day for supplement. Staff P was not observed administering the Cyanocobalamin to Resident #16.
On 7/14/23 at 8:26 a.m., LPN Staff P documented in a progress note she held the Lorazepam since, Daughter prefers that patient not have it in the morning.
On 7/14/23 at 8:30 a.m., LPN Staff P verified she did not administer the Cyanocobalamin as ordered to Resident #16. She said the Cyanocobalamin has not been available for two months, and Administration said, It's on order.
On 7/14/23 at 2:00 p.m., LPN Staff P verified she held the Lorazepam at the daughter's request but had not notified the Advanced Practice Registered Nurse who ordered the medication.
On 7/15/23 review of the Medication Administration Record (MAR) showed Resident #16 did not receive the Cyanocobalamin on 7/14/23.
2. On 7/14/23 at 9:15 a.m., LPN Staff U was observed administering medications to Resident #85, including two tablets of Magnesium Oxide 400 mg for a total of 800 mg.
LPN Staff U said Resident #85 had an order for Co Q-10 (supplement)100 mg, but she was not able to locate the medication. She did not administer the Co Q-10.
Reconciliation of the observation of the medication administration with the physician's orders revealed an order for Co Q-10 oral capsule 100 mg by mouth daily for supplement and Magnesium Oxide 250 mg, give two tablets (500 mg) one time a day.
LPN Staff U documented on the MAR she administered Magnesium Oxide 500 mg as per the physician's order, and the Co Q-10 was not available.
On 7/14/23 at 5:10 p.m. The Director of Nursing (DON) said CO Q-10 was on order and not available.
On 7/14/23 at 12:00 p.m., LPN Staff U verified she administered 800 mg of Magnesium Oxide to Resident #85 instead of Magnesium Oxide 500 mg as per the physician's order.
On 7/14/23 at 4:35 p.m., the DON said the facility did not have Magnesium Oxide 250 mg. She said the nurse who took the verbal order on 7/5/23 for the Magnesium Oxide should have informed the practitioner the Magnesium Oxide was not available in that strength.
5. On 7/14/23 at 2:00 p.m., LPN Staff P was observed administering four different medications to Resident #24.
Reconciliation of the observation with the physician's orders revealed an order to administer Miralax (laxative) 17 grams mixed in eight ounces of water once a day for constipation.
LPN Staff P was not observed to offer or administer the Miralax. She documented on the MAR Resident #24 refused the Miralax.
On 7/14/23 at 3:30 p.m., LPN Staff P verified she did not offer or administer the Miralax to Resident #24 and documented the resident refused the medication.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0810
(Tag F0810)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure 2 (Residents #15, and #21) of 2 sampled residen...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure 2 (Residents #15, and #21) of 2 sampled residents of 25 residents requiring assistance with eating received the necessary assistive devices during dining.
The findings included:
1. Resident #15 was admitted to the facility on [DATE] with diagnoses including hemiplegia (Paralysis on one side of the body), and Parkinson's disease. Resident #15 had contractures (deformity) of both hands. Resident #15 received a pureed diet.
On 7/11/23 at 12:30 p.m., Resident #15 was observed eating a pureed lunch in the dining room with a regular spoon. The resident had difficulty getting the food to his mouth, spilling the content of the spoon on the plate.
On 7/12/23 at 11:48 p.m., the Director of Physical Therapy stated Resident #15 should have a weighted utensil when he was eating his meals.
Review of the care plans for activities of daily living and nutrition showed no intervention to provide the resident with weighted utensils for meals.
On 7/12/23 at 12:45, Resident #15 was observed eating in the dining room. No weighted utensils were provided for him during his meal.
On 7/14/23 at 4:00 p.m., the Restorative Aide said Resident #15 uses three weighted utensils and she keeps them rolled up in a towel in the skilled nursing kitchen. She stated she made sure when she was working the resident had the utensils. She stated she was not sure how the resident got the utensils when she was not working.
On 7/14/23 at 4:30 p.m., the Director of Nursing said the weighted utensils should be listed on the meal ticket to alert the staff assisting with the meals.
On 7/14/23 Resident #15's lunch meal ticket was observed. It did not list the weighted utensils.
2. Resident #21 was admitted to the facility from the hospital on [DATE]. Diagnoses included Cerebral vascular Accident (Stroke), hypertension, Diabetes Mellitus, depression and anxiety.
The Quarterly Minimum Data Set (MDS) assessment dated [DATE] noted Resident #21's cognition was intact with a Brief Interview for Mental Status (BIMS) of 13. Section E of the assessment shows Resident #21 had no rejection of care behaviors. Section G showed Resident #21 had function limitations on one side on both his upper and lower extremities.
On 7/10/23 at 12:30 p.m., Resident #21 was observed in bed eating a peanut butter and jelly sandwich. The resident also had a regular small bowl of pudding.
The meal ticked for the lunch meal of 7/10/23 noted the use of a divided plate (keeps food separated).
Review of Resident #21's care plans showed no intervention listed for a divided plate.
On 7/12/23 at 11:50 a.m., the Director of Physical Therapy (PT) said she will provide the kitchen with a divided plate. The Director of Physical Therapy opened a cabinet in her office which contained a supply of divided plates.
On 7/13/23 at 12:40 a.m., Resident #21 was observed in bed. The resident's lunch was on his bedside table, it was not on a divided plate.
On 7/14/23 at 12:30 p.m., Resident #21 was observed in the dining room having lunch. The meal was not served on a divided plate.
On 7/14/213 at 2:20 p.m., the Director of PT verified she had not yet provided the kitchen with a divided plate for Resident #21.
On 7/14/23 at 4:30 p.m., the Director of Nursing said the adaptive equipment, including divided plates should be listed on each resident's meal ticket.
Resident #21's meal ticket for 7/14/23 was observed. It did not list the divided plate.
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on staff interviews, and record reviews, the facility failed to ensure the Dietary Manager possessed the necessary qualifications and to ensure frequently scheduled consultation by a qualified d...
Read full inspector narrative →
Based on staff interviews, and record reviews, the facility failed to ensure the Dietary Manager possessed the necessary qualifications and to ensure frequently scheduled consultation by a qualified dietitian.
The findings included:
On 7/11/23 at 11:45 a.m., the Director of Food and Nutrition Services said she had completed a course work on June 28, 2019, at a university for Nutrition and Food service Professional training.
She said the completed course allowed her to take the certification exam but has not done so yet. She stated the Registered Dietician (RD) worked offsite but came in once a month.
The Director of Food and Nutrition Services provided a certificate of completion dated June 28, 2019 which noted she had, Satisfactorily completed the requirement for the Professional Development pre-certification course. Nutrition and foodservice [sic] Professional Training.
On 7/12/23 at 4:13 p.m., the regional RD said he visits the facility monthly to monitor the food and nutrition services. He said the facility RD normally does the clinical part of the assessments, including readmissions, quarterly, Minimum Data Set assessments, care plan and addresses any weight loss.
He said the current Director of Food and Nutrition Services started in April 2023, and he was aware the Directof of Food and Nutrition Services was not qualified and verbalized concerns about changes in the regulations she may not be aware of which could impact her ability to pass the certification exam.
On 7/12/23 at 3:13 p.m., the Human Resources Assistant said the Director of Food and Nutrition Services was hired in January 2023 as a cook. She was promoted to Director of Food and Nutrition Services on April 3, 2023. She verified the employment application was incomplete and did not list dates of prior work experience, employment title or documented references. She stated she was not aware of the regulations required for a Director of Food and Nutrition Services.
On 7/13/23 at 11:20 a.m., during a telephone interview the RD stated she was contracted by the facility to work remotely one day per week.
On 7/13/23 11:34 a.m., the RD stated she did not work from 5/30/23 until 6/29/23.
On 7/13/23 at 5:18 p.m., the administrator stated he was not aware of the regulatory requirement for Director of Food and Nutrition Services qualifications.
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
Based on resident and staff interview, record review, and observation, the facility failed to provide palatable food at appropriate temperatures for 3 (Residents #7, #17 and #385) of 4 residents inter...
Read full inspector narrative →
Based on resident and staff interview, record review, and observation, the facility failed to provide palatable food at appropriate temperatures for 3 (Residents #7, #17 and #385) of 4 residents interviewed for food palatability. Poor food quality may cause resident to eat less of their food or not at all, which can lead to weight loss and impaired nutrition.
The findings included:
On 7/10/23 at 9:55 a.m., Resident #385 stated the food is cold. She said, the vegetables don't have any seasoning, are over cooked, no fruit, no soda. The oatmeal is dried and hard, no sugar or milk in it and the eggs are cold.
On 7/11/23 at 10:30 a.m. Resident #7's private duty Certified Nursing Assistant (CNA) was interviewed. She stated she worked with Resident #7 two days a week. She stated, The food is often cold or just lukewarm. The staff will warm it if someone is here to ask them.
On 7/11/23 10:55 a.m., Resident #385 stated she just can't eat cold eggs, the food is cold no matter what they bring.
On 7/11/23 at 12:15 p.m., food was observed being delivered from the main kitchen to the satellite kitchen and placed on the steam table.
The assistant kitchen manager was observed plating the food on room temperature plates. She stated the plate warmer had not been in service for a couple of weeks.
Tray line was stopped after serving four bowls of soup for a staff member to go to the main kitchen and return with enough bowls to serve everyone in the dining area.
On 7/11/23 at 1:10 p.m., tray line was paused again when staff ran out of plates. Staff returned to the kitchen to obtain additional plates for the residents. The assistant kitchen manager stated the area was not stocked with dishes for lunch service.
On 7/11/23 at 1:19 p.m., a test tray was requested for the back hall.
The test tray was done after the last tray was distributed in the back hall. The turkey was barely warm when tasted, and the temperature was 109 degrees Fahrenheit. The green beans and sweet potato were warm when tasted, not hot.
On 7/12/23 at 1:30 p.m., Resident #17 stated the food does not have much taste, at best, the hot food is only lukewarm. It's just not hot.
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
Based on interview, and record review the facility failed to have documentation of a comprehensive facility-wide assessment, including an evaluation of the resident population and resources needed to ...
Read full inspector narrative →
Based on interview, and record review the facility failed to have documentation of a comprehensive facility-wide assessment, including an evaluation of the resident population and resources needed to provide the necessary care and services.
The findings included:
On 7/10/23 at 9:20 a.m., and on 7/14/23 at 12:00 p.m., a request was made to the administrator to provide documentation of a facility assessment.
On 7/14/23 at 2:00 p.m., the Administrator provided an 18 page document titled, Facility's Quality Assessment and Assurance which he said was the facility assessment.
The document a clinical systems scorecard summary, and a long term care essentials clinical assessment test which noted individuals scoring less than a 70 on assessments will be given the opportunity to retest at a later time and/or date.
The document did not include an evaluation of the resident population, including diseases, conditions, physical, functional or cognitive status, acuity of the resident population, and any other pertinent information about the residents that may affect and plan for the services the facility must provided. and resources needed to provide the necessary care and services the residents require.
The form did not list the facilities resources and daily needs to ensure the care of the residents.
On 7/14/23 at 12:01 p.m., the Administrator said this document was all he could provide as a facility assessment.
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0843
(Tag F0843)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure they had an updated transfer agreement with one or more hospi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure they had an updated transfer agreement with one or more hospitals approved for participation under the Medicare and Medicaid programs. The transfer agreement was to be used to ensure a safe and appropriate transfer of a resident between the facilities.
The findings included:
A review of the Facility Transfer Agreement (Revised on 01-2009) between the long-term care facility/nursing home and the hospital revealed it was signed on [DATE] with an end date of [DATE]. Further review of the Facility Transfer Agreement noted it was not renewed after the [DATE] end date.
On [DATE] at 1:50 p.m., in an interview with the Administrator, he said the current transfer agreement between the nursing home and the hospital expired on [DATE]. He said he was unable to find documentation the facility had renewed the transfer agreement with the hospital or had attempted to secure a new transfer agreement with a hospital as required per federal regulation.