HALE MALAMALAMA




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Hale Malamalama has received a Trust Grade of F, indicating significant concerns about the quality of care provided. They rank #32 out of 41 nursing homes in Hawaii, placing them in the bottom half of facilities in the state, and #18 of 26 in Honolulu County, meaning only a handful of local options perform better. The facility is trending towards improvement, with issues decreasing from 6 in 2024 to 5 in 2025, but still has a long way to go. Staffing is a strength, with a rating of 4 out of 5 stars, though turnover is at 43%, which is average for Hawaii. The facility has accumulated $87,032 in fines, which is concerning as it is higher than all other facilities in the state, indicating ongoing compliance problems. Additionally, while RN coverage is average, there are serious deficiencies. Incidents include staff making inappropriate comments and neglecting to assist a resident with toileting, leading to emotional harm. Another serious issue involved failing to provide proper care for a resident allergic to iodine, which could cause pain. Lastly, a resident experienced avoidable falls due to inadequate safety measures and care plan oversight, resulting in visible bruises. Overall, while there are some strengths, the significant issues and poor trust grade warrant caution for families considering this facility.
- Trust Score
- F
- In Hawaii
- #32/41
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 43% turnover. Near Hawaii's 48% average. Typical for the industry.
- Penalties ○ Average
- $87,032 in fines. Higher than 64% of Hawaii facilities. Some compliance issues.
- Skilled Nurses ✓ Good
- Each resident gets 64 minutes of Registered Nurse (RN) attention daily — more than 97% of Hawaii nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 43 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (43%)
5 points below Hawaii average of 48%
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Below Hawaii average (3.4)
Below average - review inspection findings carefully
Near Hawaii avg (46%)
Typical for the industry
Well above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 43 deficiencies on record
Jan 2025
5 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record and document review, the facility failed to protect one resident (R)1 of two investigated for staff a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to report two of a sample size of two allegations of Resident (R)1 an...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and document review, the facility failed to provide evidence they conducted thorough investigations of two R...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to timely update one Resident's(R)1 care plan. R1 initially required ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review (RR) and interviews, the facility failed to provide the needed incontinence care and standar...
Read full inspector narrative →
Sept 2024
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review, the facility failed to treat one of 13 sampled residents (Resident (R) 4) with respect and dignity while assisting with R4's meal. This deficient ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to revise one of the 13 sampled residents (Resident (R) 18) care plan after R18 had a fall with injury. This deficient practice has the potent...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, interview, and facility policy review, the facility failed to ensure drugs and biologicals are stored in a locked compartment. Proper storage of medications is necessary to prom...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review. The facility failed to provide an orderly and comfortable home for the residents residing in the facility, due to the following:
Resident care equi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, interview and review of policy, the facility failed to ensure housekeeping services were being provided to the residents in a manner that was safe. Housekeeping staff were cleani...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on interviews and record review, the facility failed to create an annual Performance Improvement Project (PIP) that focuses on high risk or problem prone areas identified through the data collec...
Read full inspector narrative →
Sept 2023
23 deficiencies
2 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to provide care to residents in accordance with profes...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review (RR), interview with family and staff, the facility failed to ensure one of two residents sampled were fr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record reviews, and interview, the facility failed to ensure that one resident (R), R28, out of two reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on record review and interview with staff member, the facility failed to ensure one (Resident 7) of three residents selected for liability notice review received Notice of Medicare Non-Coverage ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interview, the facility failed to ensure that a complete medical summary documented by the physician...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on record review and staff interview the facility failed to develop and implement a baseline care plan within 48 hours for two sampled residents upon admission, Residents (R)6 and R7. The facili...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview with staff members, the facility failed to assure discharge planning was done prior to resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview with staff member, the facility did not ensure one (Resident 38) of one residents reviewed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to assure one of two residents sampled had an effective pain manageme...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview with staff, the facility failed to assure 2 (Residents 31 and 23) of 5 residents had the op...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected multiple residents
Based on record review (RR) and staff interview the facility failed to inform three of three residents reviewed for the use of psychotropic medications, Resident (R)7, R9 and R25, or the residents' re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Based on interview, the facility failed to ensure the residents of the facility exercised their right to organize and participate in a resident group.
Findings include:
On 09/14/23 at 07:58 AM, an Ent...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation and interviews, the facility failed to provide a sanitary and comfortable environment as evidenced by a damaged closet shelf and the lack of monitoring the water system to ensure ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on record review and interview with staff, the facility failed to implement a grievance system to assure residents exercised their right to file a grievance. The facility did not have an identif...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0563
(Tag F0563)
Could have caused harm · This affected most or all residents
Based on complaint report and interview, the facility failed to ensure residents of the facility had the right to receive visitors.
Findings include:
On 11/28/22, the Office of Health Care Assurance (...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected most or all residents
Based on record review (RR), interviews with family and staff, the facility failed to involve and notify resident's representative(s) of scheduled care plan meetings for Resident (R)6, R7 and R29. The...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
Based on interview with staff, the facility did not assure a system was in place to review the performance/competency of certified nurse aides (CNA) at least once every 12 months. This systemic defici...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to provide safe storage for foods in the kitchen refrigerators and freezer and failed to develop a process to ensure that the...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
Based on observations, record review, and interviews the facility's nursing administration did not assure the facility was administered in a manner that enabled it to develop and maintain systems for ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0837
(Tag F0837)
Could have caused harm · This affected most or all residents
Based on interview with the Administrator, the facility did not assure the governing body oversees the Administrator's management and operations of the facility.
Findings include:
On 09/15/23 at 01:1...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
Based on record review and interview, the facility failed to develop, implement, and maintain an effective, comprehensive, data-driven Quality Assurance and Performance Improvement (QAPI) program that...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
3) On 09/14/23 at 09:21 AM, conducted a concurrent observation and interview with Licensed Practical Nurse (LPN)2 during R3's dressing change to her right heel and right toe. LPN2 used the same gloves...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected most or all residents
Based on observations, interview, and record review, the facility failed to ensure the safety of their residents and staff by not providing accessible means to trigger the call light system should the...
Read full inspector narrative →
Oct 2022
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, interviews, and facility policy review, the facility failed to ensure a dependent resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, interviews, and facility policy review, the facility failed to provide a homelike environm...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interviews, the facility failed to develop a care plan to address hand contractures for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews, the facility failed to ensure nursing care was provided in accordance with...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews, the facility failed to ensure care and services were provided to prevent f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0728
(Tag F0728)
Could have caused harm · This affected 1 resident
Based on document review, interviews, and facility policy review, the facility failed to ensure a nursing assistant (NA) who was a full-time employee completed the required competency exam for certifi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0811
(Tag F0811)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, interviews, and document review, the facility failed to ensure a paid feeding assistant pr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected multiple residents
Based on observations, record review, interviews, and document review, the facility's nursing administration failed to ensure processes were in place to promptly identify resident-specific care needs ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observations and interviews, the facility failed to ensure staff implemented appropriate infection control practices during 3 of 3 meals observed. Specifically, staff opened and handled resid...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 43% turnover. Below Hawaii's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: Federal abuse finding, Special Focus Facility, 3 harm violation(s), $87,032 in fines. Review inspection reports carefully.
- • 43 deficiencies on record, including 3 serious (caused harm) violations. Ask about corrective actions taken.
- • $87,032 in fines. Extremely high, among the most fined facilities in Hawaii. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Hale Malamalama's CMS Rating?
CMS assigns HALE MALAMALAMA an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Hawaii, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Hale Malamalama Staffed?
CMS rates HALE MALAMALAMA's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 43%, compared to the Hawaii average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Hale Malamalama?
State health inspectors documented 43 deficiencies at HALE MALAMALAMA during 2022 to 2025. These included: 3 that caused actual resident harm and 40 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
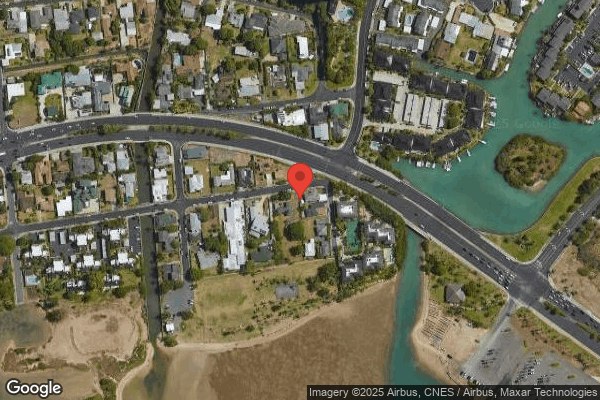
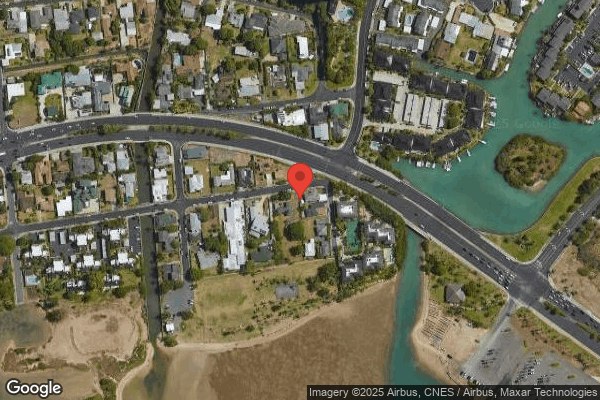
Who Owns and Operates Hale Malamalama?
HALE MALAMALAMA is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 40 certified beds and approximately 39 residents (about 98% occupancy), it is a smaller facility located in HONOLULU, Hawaii.
How Does Hale Malamalama Compare to Other Hawaii Nursing Homes?
Compared to the 100 nursing homes in Hawaii, HALE MALAMALAMA's overall rating (2 stars) is below the state average of 3.4, staff turnover (43%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Hale Malamalama?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the substantiated abuse finding on record.
Is Hale Malamalama Safe?
Based on CMS inspection data, HALE MALAMALAMA has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Hawaii. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Hale Malamalama Stick Around?
HALE MALAMALAMA has a staff turnover rate of 43%, which is about average for Hawaii nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Hale Malamalama Ever Fined?
HALE MALAMALAMA has been fined $87,032 across 2 penalty actions. This is above the Hawaii average of $33,949. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Hale Malamalama on Any Federal Watch List?
HALE MALAMALAMA is currently an SFF Candidate, meaning CMS has identified it as potentially qualifying for the Special Focus Facility watch list. SFF Candidates have a history of serious deficiencies but haven't yet reached the threshold for full SFF designation. The facility is being monitored more closely — if problems continue, it may be added to the official watch list. Families should ask what the facility is doing to address the issues that led to this status.