Islands Skilled Nursing & Rehabilitation
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Islands Skilled Nursing & Rehabilitation has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #34 out of 41 facilities in Hawaii places it in the bottom half, and #20 out of 26 in Honolulu County means that there are only a few local options that are better. Although the facility is improving, having reduced issues from 27 in 2024 to 14 in 2025, it still faces serious challenges, including $89,206 in fines, which is higher than 97% of Hawaii facilities. Staffing is a relative strength, with a 0% turnover rate, but the overall staffing rating is only 2 out of 5 stars. There were concerning incidents noted, such as a resident suffering hallucinations and increased heart rate due to improper medication application, and failures to maintain proper documentation for staffing, which could indicate underlying issues with care quality.
- Trust Score
- F
- In Hawaii
- #34/41
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ⚠ Watch
- $89,206 in fines. Higher than 98% of Hawaii facilities. Major compliance failures.
- Skilled Nurses ✓ Good
- Each resident gets 163 minutes of Registered Nurse (RN) attention daily — more than 97% of Hawaii nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 64 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Hawaii average (3.4)
Below average - review inspection findings carefully
Well above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 64 deficiencies on record
Apr 2025
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to provide a clean and homelike environment. Observed a buildup of dus...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to accurately assess one (Resident 18) of four residents reviewed for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to develop and implement a baseline care plan for Resident (R)33's hype...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to follow Resident (R) 22's care plan and facility policies/protocols for the prevention/treatment of skin breakdown for one resident of three ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview the facility failed to provide an environment free of accident hazards for one of one residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on staff interviews, record review and review of policy, the facility failed to act on a Pharmacist Medication Regimen Review (MRR) recommendation for one resident (R) 2 of five residents sample...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
2) On 04/29/25 at 08:13 AM observed medication cart two near nurse's station with keys left unattended in a disposable cup on top of the medication cart. Inquired of Registered Nurse (RN) 7 if the med...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure the ice machine was kept in clean and sanitary condition in accordance with professional standards for food service safety. This defic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to correctly fill out an accurate Physician Orders for Life Sustaining ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5) On 04/27/25 at 11:10 AM observed R31 resting in his bed. At this time observed R31's indwelling urinary catheter tubing and u...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure the right to a dignified existence for four ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview the facility failed to develop and implement comprehensive person-centered care plan (CP) for two of 20 residents sampled for care plan review, Reside...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Data
(Tag F0851)
Could have caused harm · This affected most or all residents
Based on record review and interview the facility failed to submit their staffing information based on payroll data for direct care staffing (including information for agency and contract staff) for f...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected most or all residents
Based on observation, staff interview and policy review, the facility failed to keep record of dryer lint removal and cleaning. As a result of this deficient practice, the facility did not show that t...
Read full inspector narrative →
Jul 2024
6 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0726
(Tag F0726)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, document and record review, the facility nursing staff did not demonstrate the competency and skill set to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record and document reviews, the facility violated federal regulations when they initiated a discharge that...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record and document reviews, the facility did not provide the required notification of transfer/discharge t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, document review and record review, the facility had an established transfer/discharge policy, but failed to...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to update one Resident's (R)1 care plan (CP) of a sample size of four...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0713
(Tag F0713)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, document review and medical record review, the facility failed to provide availability of physician service...
Read full inspector narrative →
May 2024
21 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
3) On 05/13/24 at 09:52 AM, observed from outside of R4's room, his urinary catheter bag hanging from the bottom of his bed, uncovered.
On 05/13/24 at 09:53 AM, an interview with CNA17 was done. Inqu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0551
(Tag F0551)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the rights of a resident's representative in a ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to ensure written copy of the Notice of Medicare Non-Coverage (NOMNC)...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to report an allegation of abuse immediately but no later than two hours after the allegation was made or allegation of mistreatment and an i...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to prevent further potential abuse or mistreatment while the investigation was in progress for Resident (R) 34. The facility did not remove C...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to ensure written notification of transfer/discharge was provided to the resident or resident's representative, as soon as practicable, befor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to re-assess Resident (R) 15 for falls quarterly. The deficient practice puts all residents who are at risk for falls or have had a change in t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to include Resident (R) 35's daily preferences to her baseline care pla...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
4) During review of the facility's Resident Council Minutes for February, March, and April 2024 monthly meetings, on 04/29/24 the minutes documented R4 inquiring What's going on regarding have the sup...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to change a suction cannister half full of red-brown secr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
2) On 05/13/24 at 11:42 AM, during observation and interview with R4, RN74 walked in R4's room placed a small clear plastic cup on his bedside table and informed R4 it was his pain medication, oxycodo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
2) Cross reference to F761. The facility failed to ensure medications were not left unattended by authorized staff and stored in locked compartments.
On 05/14/24 at 09:53 AM, observed R14 in her bed ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to develop and implement a comprehensive person-centered care plan (C...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to update the care plan for one Resident (R) 27 with treatment plans and recommendations. R27 has a tracheostomy and wears a Passy Muir valve (...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure a resident received treatment and care in accordance with pr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure the attending physician documented in the residents' medical record that a review of the medication regimen review (MMR) recommendat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to specify and monitor behaviors related to psychotropic and sedative...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) On 05/15/24 at 08:28 AM medication administration observation with RN79 in the front unit on second floor. The following medi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interview and policy review, the facility failed to ensure it established and maintained an infection pre...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected most or all residents
Based on observation and interview the facility failed to provide Nursing Staffing Information to include hours worked by Registered Nurses (RNs), Certified Nurse Aides (CNAs) and resident census each...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
Based on review of the Facility Assesment (FA), the facility failed to conduct, document, and annually review its facility-wide assessment. The facility used a facility assessment tool as a template i...
Read full inspector narrative →
Sept 2023
2 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interviews, the facility failed to ensure pneumococcal vaccination was offered to one of the si...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to ensure that one resident (R), R28, out of the six residents sampled, had the appropriate documentation for the administration or refusal o...
Read full inspector narrative →
May 2023
21 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on observations and interview, the facility failed to identify and support one resident's (R)17 preference to not be placed in a yellow gown. As a result of this deficient practice, R17 did not ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and staff interview, the facility failed to provide safe, clean, and homelike environment for the resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to develop and implement person-centered Comprehensiv...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews with staff members, the facility failed to revise the care plan for 2 (Residents 33 and 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews with staff, residents, and resident representatives, the facility failed to ensure residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews with resident and staff member, the facility failed to assure a resident who is incontinen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, and record review, the facility failed to provide nutritional care and services to addr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interview with staff member, the facility failed to use infection control precautions ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interviews and record reviews, the facility failed to ensure two (Residents 20 and 17) of five residents sampled ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, the facility failed to provide food that accommodates a resident's food allergies. Resident (R)190 was served food that contained an ingredient th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on resident interviews and record reviews, the facility failed to ensure the resident's right to an environment that promotes enhancement of his or her quality of life, as evidenced by staff spe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0577
(Tag F0577)
Could have caused harm · This affected multiple residents
Based on observations and interviews, the facility failed to post the results of the facility's most recent State survey, that is easily accessible to residents, legal representatives, and family memb...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) R22 was admitted to the facility on [DATE]. A review of the EHR was conducted on 05/24/23 at 10:00 AM. The EHR indicated that...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and staff interview, the facility failed to provide written notice of the facility's bed-hold policy for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) On 05/22/23 at 09:18 AM during the initial observations in room [ROOM NUMBER], Registered Nurse (RN) 22 entered room and stat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on interview and record review (RR), the facility failed to ensure there was enough staff to provide services and respond to each resident's needs in a timely manner, as evidenced by a complaint...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interviews and record reviews, the facility failed to ensure that the drug regimen of each resident was reviewed ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) On 05/24/23 at 09:20 AM, an unlocked medication cart was observed on the second-floor unit hallway. An interview was conducte...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations and staff interview, the facility failed to provide a clean area to prepare food for the residents. This deficient practice has the potential to affect all residents, visitors an...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
2) On 05/24/23 at 11:13 AM, conducted a review of R20's EHR. Under Progress Notes, noted an entry from the attending physician done on 05/23/23 at 07:55 AM. Entry contained the name and medical inform...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews and record reviews, the facility failed to prevent the possible spread of infectious ill...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • 64 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $89,206 in fines. Extremely high, among the most fined facilities in Hawaii. Major compliance failures.
- • Grade F (35/100). Below average facility with significant concerns.
About This Facility
What is Islands Skilled Nursing & Rehabilitation's CMS Rating?
CMS assigns Islands Skilled Nursing & Rehabilitation an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Hawaii, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Islands Skilled Nursing & Rehabilitation Staffed?
CMS rates Islands Skilled Nursing & Rehabilitation's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes.
What Have Inspectors Found at Islands Skilled Nursing & Rehabilitation?
State health inspectors documented 64 deficiencies at Islands Skilled Nursing & Rehabilitation during 2023 to 2025. These included: 1 that caused actual resident harm and 63 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Islands Skilled Nursing & Rehabilitation?
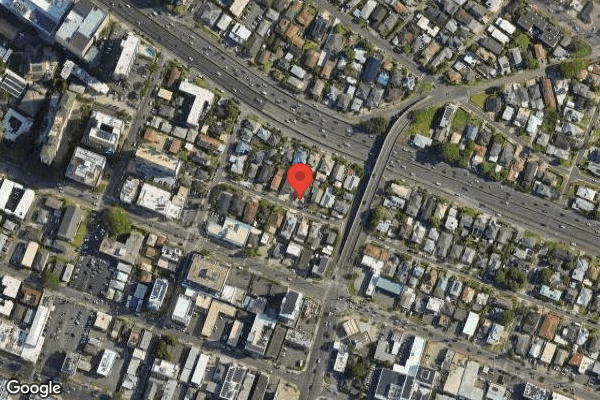
Islands Skilled Nursing & Rehabilitation is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 42 certified beds and approximately 31 residents (about 74% occupancy), it is a smaller facility located in Honolulu, Hawaii.
How Does Islands Skilled Nursing & Rehabilitation Compare to Other Hawaii Nursing Homes?
Compared to the 100 nursing homes in Hawaii, Islands Skilled Nursing & Rehabilitation's overall rating (2 stars) is below the state average of 3.4 and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Islands Skilled Nursing & Rehabilitation?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Islands Skilled Nursing & Rehabilitation Safe?
Based on CMS inspection data, Islands Skilled Nursing & Rehabilitation has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Hawaii. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Islands Skilled Nursing & Rehabilitation Stick Around?
Islands Skilled Nursing & Rehabilitation has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Islands Skilled Nursing & Rehabilitation Ever Fined?
Islands Skilled Nursing & Rehabilitation has been fined $89,206 across 1 penalty action. This is above the Hawaii average of $33,971. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Islands Skilled Nursing & Rehabilitation on Any Federal Watch List?
Islands Skilled Nursing & Rehabilitation is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.