ASCENSION RESURRECTION LIFE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Ascension Resurrection Life has a Trust Grade of D, indicating below-average performance with some concerning issues. Ranked #216 out of 665 facilities in Illinois, they fall in the top half of the state, while standing #67 out of 201 in Cook County, meaning there are only a few local options that are better. The facility is improving, with a decrease in reported issues from 12 in 2024 to just 3 in 2025. Staffing is a strength, rated 4 out of 5 stars, with turnover at 53%, which is around the state average, and they have more RN coverage than 99% of Illinois facilities, ensuring better care. However, the facility has faced serious incidents, including a resident developing a pressure ulcer due to a failure in wound prevention and another resident not receiving necessary medications upon admission, leading to significant pain. Overall, while there are notable improvements and staffing strengths, families should consider these past incidents when evaluating care quality.
- Trust Score
- D
- In Illinois
- #216/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 53% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Illinois facilities.
- Skilled Nurses ✓ Good
- Each resident gets 94 minutes of Registered Nurse (RN) attention daily — more than 97% of Illinois nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 41 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, fire safety.
The Bad
Near Illinois average (2.5)
Meets federal standards, typical of most facilities
Near Illinois avg (46%)
Higher turnover may affect care consistency
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 41 deficiencies on record
Sept 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to clean and empty a resident's ileostomy bag in a timely manner. The ...
Read full inspector narrative →
Aug 2025
1 deficiency
MINOR
(B)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Deficiency F0628
(Tag F0628)
Minor procedural issue · This affected multiple residents
Based on interview and record review, the facility failed to notify the Office of the State Long-Term Care Ombudsman of residents who were transferred or discharged back to the community or to another...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide person-centered discharge plan of care for 5 out 5 resident...
Read full inspector narrative →
Oct 2024
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure call light was within reach for one (R32) out of eight residents reviewed in a total sample of 26 for call lights.
Fin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to follow their discharge against medical advice policy for 1 (R120) re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident's initial preadmission screening was completed prior to admission to the nursing facility for 1 (R40) out of 2 sampled re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to follow a resident's (R64's) and their representative's wishes for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record reviews, the facility failed to correctly set an air loss mattress based on weight ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and records reviews, the facility failed to follow the fall care plan intervention for one resident (R98) of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to follow their policy and procedure to ensure a.) oxygen ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to ensure that a resident (R221) was free of any significant medication errors for one out of five residents reviewed for med...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to serve mechanical soft food to a resident on mechanical soft diet order. This failure affected 1 (R19) of 4 residents reviewed ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record reviews, the facility failed to dispose eye drops after the discard date, refrigerate an unopened insulin pen, and lock a medication cart when not in use ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
3.) On 10/1/24 at 11:14 AM, R8 was lying in bed and noted an Enhanced Barrier Precautions signage posted on R8's door. V5 (CNA) was interviewed and stated V5 was assigned to R8 and was about to dress ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to a.) ensure all food items were labeled with an opened and use by date, b.) discard expired food based on use by date docum...
Read full inspector narrative →
Dec 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that a resident remain free from abuse, for one of three (R1...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interviews and records review, the facility failed to ensure a Certified Nursing Assistant/CNA possessed the competencies and skill sets necessary to provide nursing and related services in a...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and records review, the facility failed to follow their Discarding and Destroying Medications policy, and failed to assure that medications to be disposed were secur...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and records review, the facility failed to follow infection control policy by failing to properly dispose of used needles, contaminated blood draw equipment, failed to...
Read full inspector narrative →
Nov 2023
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0558
(Tag F0558)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record reviews the facility failed to make reasonable accommodations for two (R1, R2) of fo...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record reviews the facility failed to follow their wound prevention policy for two residen...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to provide group activities to meet the needs and interests of 1 resident (R1) out of 3 reviewed for resident rights. This failure...
Read full inspector narrative →
Sept 2023
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to ensure that the call light was within reach for R14 and failed to respond to R34's needs for two out of a total sample of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to ensure that residents' code statuses were consistent with their P...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to revise the care plan for 1 (R72) resident reviewed for wound preventive measures in a sample of 25.
Findings Include:
R72 has...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure the physician order for wound preventive measures were followed for 1 (R72) resident review for wound prevention in a s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record reviews, the facility failed to ensure a resident received the correct oxygen flow ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a medication error rate was less than 5% for 2 (R67 and R229) of 6 residents reviewed for medication administration. T...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews the facility failed to ensure that resident is free of any significant medication errors. This failure applies to 1 (R67) of 6 residents reviewed for medication ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to discard outdated medications for 2 (R9 and R16) residents. The facility failed to properly store medications requiring refrig...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
2.) On 9/5/23 9:56 am Medication administration conducted with V10 (Agency Registered Nurse). Observed R229 lying in bed, alert and verbally responsive, with Oxygen at 3L/min via nasal cannula. Observ...
Read full inspector narrative →
May 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to obtain medications and insulin from the facility's emergency disp...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure that two staff members were utilized when using the mechanical lift to transfer a resident that was assessed to require two persons ...
Read full inspector narrative →
Jul 2022
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to assess one resident (R82) for the ability to safely self-administer medications in the sample of 49 residents reviewed for med...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure personal information remained confidential for 1 (R72) resident reviewed for confidentiality of record in the sample o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure that a resident who depends on staff's assistance for ADL (Activities of Daily Living) care receives incontinence care...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that a resident receives adequate supervision ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to properly store respiratory supplies to prevent contamination for 2 (R42, R70) out of 6 residents reviewed for respiratory care...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the topical pain patch is dated for 1 (R72) resident reviewed for pain management in the sample of 49 residents.
Find...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. On 7/25/22 at 10:32 AM, the surveyor observed R40 lying in bed on a Low Air Loss Mattress. R40 observed lying on top of 1 fla...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the medication cart is locked when unattended. This failure has the potential to affect all 18 residents residing in 2...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Illinois facilities.
- • Multiple safety concerns identified: 3 harm violation(s), Payment denial on record. Review inspection reports carefully.
- • 41 deficiencies on record, including 3 serious (caused harm) violations. Ask about corrective actions taken.
- • Grade D (45/100). Below average facility with significant concerns.
About This Facility
What is Ascension Resurrection Life's CMS Rating?
CMS assigns ASCENSION RESURRECTION LIFE an overall rating of 3 out of 5 stars, which is considered average nationally. Within Illinois, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Ascension Resurrection Life Staffed?
CMS rates ASCENSION RESURRECTION LIFE's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 53%, compared to the Illinois average of 46%.
What Have Inspectors Found at Ascension Resurrection Life?
State health inspectors documented 41 deficiencies at ASCENSION RESURRECTION LIFE during 2022 to 2025. These included: 3 that caused actual resident harm, 37 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Ascension Resurrection Life?
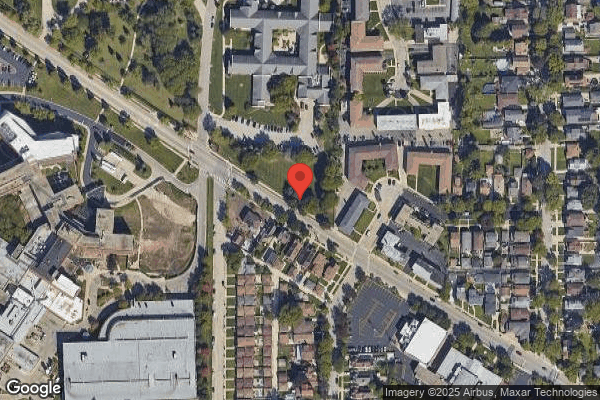
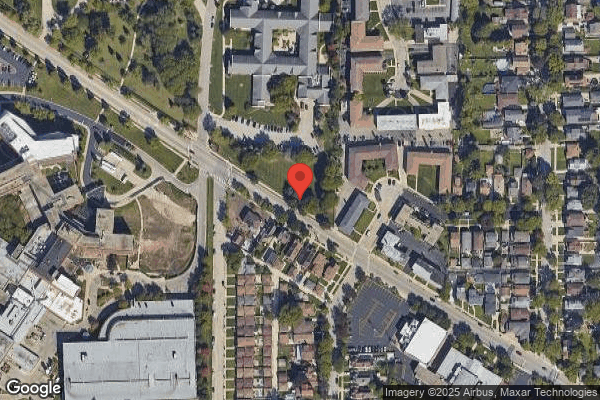
ASCENSION RESURRECTION LIFE is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility is operated by ASCENSION LIVING, a chain that manages multiple nursing homes. With 162 certified beds and approximately 124 residents (about 77% occupancy), it is a mid-sized facility located in CHICAGO, Illinois.
How Does Ascension Resurrection Life Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, ASCENSION RESURRECTION LIFE's overall rating (3 stars) is above the state average of 2.5, staff turnover (53%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Ascension Resurrection Life?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Ascension Resurrection Life Safe?
Based on CMS inspection data, ASCENSION RESURRECTION LIFE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Illinois. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Ascension Resurrection Life Stick Around?
ASCENSION RESURRECTION LIFE has a staff turnover rate of 53%, which is 7 percentage points above the Illinois average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Ascension Resurrection Life Ever Fined?
ASCENSION RESURRECTION LIFE has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Ascension Resurrection Life on Any Federal Watch List?
ASCENSION RESURRECTION LIFE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.