AUSTIN OASIS, THE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Austin Oasis in Chicago has received a Trust Grade of F, indicating poor performance with significant concerns about the care provided. It ranks #451 out of 665 facilities in Illinois, placing it in the bottom half, and #149 out of 201 in Cook County, meaning there are only a few local options that are better. While the facility's trend is improving, with the number of issues decreasing from 27 to 17 between 2024 and 2025, it still faces serious challenges, including a concerning $532,728 in fines, which is higher than 92% of Illinois facilities. Staffing is a relative strength, with a 3/5 star rating and a turnover rate of 39%, below the state average, and the facility has more RN coverage than 79% of other facilities, providing better oversight. However, there have been serious incidents, including one resident being physically assaulted by another, resulting in injuries, and another resident sustaining an abrasion after being attacked, which raises serious safety concerns. Overall, while there are some strengths, the significant fines and incidents of abuse highlight serious issues that families should carefully consider.
- Trust Score
- F
- In Illinois
- #451/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 39% turnover. Near Illinois's 48% average. Typical for the industry.
- Penalties ○ Average
- $532,728 in fines. Higher than 56% of Illinois facilities. Some compliance issues.
- Skilled Nurses ✓ Good
- Each resident gets 54 minutes of Registered Nurse (RN) attention daily — more than average for Illinois. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 74 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (39%)
9 points below Illinois average of 48%
Facility shows strength in fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
Near Illinois avg (46%)
Typical for the industry
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 74 deficiencies on record
Mar 2025
16 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to protect one (R40) resident's right to be free from physical abuse...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure the residents were treated with respect and dignity by not passing out meals to all residents sitting at a table at the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure (A) The five administration rights were followe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to a.) ensure oxygen tubing and nebulizer mask were labeled and dated, b.) ensure nebulizer supplies were properly stored when no...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record reviews, the facility failed to document the information on the resident's (R332) COVID-19 vaccine...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0575
(Tag F0575)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to display, in a public and accessible location, post...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R63 has diagnosis not limited to Constipation, Schizophrenia, Cerebrovascular Disease, Essential Hypertension, Vitamin Deficienc...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to refer 9 (R1, R22, R35, R55, R59 R70, R83, R99, R136) residents to t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on interviews and record reviews, the facility failed to complete a quarterly smoking assessment for one resident (R1) and have individualized smoking care plans for independent smokers. This ha...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility failed to label open insulins for
4 [R36, R282, R283, R284] re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to prepare food items listed on menu for pureed diets and prepare adequate food portions as documented on the recipe. This failur...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to prepare ground/mechanical soft and pureed food in appropriate diet consistency form. This failure has the potential to affect ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0808
(Tag F0808)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record reviews, the facility failed to provide double portions as part of the therapeutic diet as prescribed by the physician for 19 (R9, R17, R18, R23, R47, R78...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to: (1) provide eligible residents and/or resident representatives edu...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to ensure a.) kitchen staff wearing appropriate hair covering, b.) hand washing was being done in between handling dirty and ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to follow their linen handling policy and procedure to ensure soiled linens are properly placed inside closed plastic bags with n...
Read full inspector narrative →
Feb 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, facility failed to protect a resident from physical abuse. This failure affec...
Read full inspector narrative →
Dec 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to protect one resident (R1) out of 9 from physical abuse. This failur...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to administer right dosage of a prescribed medication as ...
Read full inspector narrative →
Oct 2024
3 deficiencies
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to follow proper sanitation in the kitchen to prevent food-borne illnesses; and failed to ensure that staff store their food and ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure that the dumpster was closed and fee from overflowing trash. These failures have the potential to affect all 178 resid...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to maintain an effective pest control program to ensure that the facility's kitchen is free of insects. This failure has the pot...
Read full inspector narrative →
Jul 2024
2 deficiencies
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected most or all residents
Based on observation, interview and document review the facility failed to provide a safe, functional, sanitary and comfortable environment for residents and staff on 4 of 5 resident floors (2nd, 3rd,...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and document review the facility fails to maintain an effective pest control program so that the...
Read full inspector narrative →
May 2024
8 deficiencies
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure that 5 residents (R2, R5, R77, R114 and R137) h...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Findings include:
Census on the second floor is 40 residents.
On 5/13/24 at 11:40 am, Surveyor observed laundry/linen chute on the 2nd floor unlocked. Surveyor inquired to V23 CNA (Certified Nursing A...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0741
(Tag F0741)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to have sufficient Psychiatric Rehabilitation Services Coordinators/PRSC to meet the individualized psychosocial and mental heal...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to label an opened multi dose vial and discard an expired...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Findings include:
On 5/13/24 at 10:18am, this surveyor observed a droplet precautions sign on R8's bedroom door with PPE (Person...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Findings include:
On 5/13/2024 at 10:25am arrived on the fourth floor, observed the fourth-floor dayroom with chipped areas of paint on the walls in the dayroom.
On 5/13/2024 at 10:59am observed the...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review the facility failed to ensure food in the refrigerator and freezer was labeled with a date indicating when the item was placed into the refrigerator/f...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review the facility failed to ensure the outside dumpster lid was closed and garbage bags were placed into the dumpster to prevent pests and rodents from ent...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on Observation, interview and record review the facility failed to administer scheduled medications in the schedule time frame. This failure affected 4 residents (R1, R2, R3, and R4) reviewed fo...
Read full inspector narrative →
Apr 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that a resident was free from physical abuse. This failure a...
Read full inspector narrative →
Feb 2024
8 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure that adequate supervision was provided for five...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide privacy during glucose monitoring and insulin administration for one resident (R23) reviewed for resident rights in th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to report to IDPH (Illinois Department of Public Health) within the required regulation time, unwitnessed fall with injury for one resident (R1...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure that physician order on medication administrations was followed, failed to document insulin administration and blood gl...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure that privacy was afforded to one of four residents (R14) with urine collection bag in the sample reviewed for privacy. ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to ensure that call light is within the reach for four residents (R1, R4, R15 and R16) reviewed for call lights.
Findings include...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
Based on observation, interview, record review the facility failed to ensure that the call light system was in a working condition for residents to call for staff assistance. This failure has the pote...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to provide a safe and functional environment in regard call light for resident's staff assistance. This failure affected all the ...
Read full inspector narrative →
Jan 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one resident (R2) remained free from verbal abuse. This failure affected one resident (R2) out of three residents reviewed for abuse...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to ensure that a resident (R1) who depend on staff's assistance for their ADL (Activities of Daily Living) care received showers, ...
Read full inspector narrative →
Dec 2023
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected most or all residents
Based on observation and document review the facility failed to provide a clean homelike environment, this failure has the potential to affect all residents
Finding include:
On 12/15/23, 12/16/23 an...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that residents remain free from staff to resident physical a...
Read full inspector narrative →
Oct 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 10/24/2023 at 1:47pm, R1 said on that day (09/18/2023) during dinner, she did not get her dinner tray and she informed sta...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to protect the resident's right to be free from physical abuse by other residents for two (R1 and R4) out of four residents reviewed for abuse...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and review of records the facility failed to provide residents comfortable environment due to insufficient and inefficient air conditioning system. And failed to fol...
Read full inspector narrative →
May 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, facility failed to affirm the right of the resident to be free from verbal abuse. This def...
Read full inspector narrative →
May 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to submit the final facility-reported incident report to the state agency within 5 working days as per facility policy for one resident (R1). ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure that one resident (R5) who is dependent on staff for bed mobility and who has a stage III pressure ulcer to the sacrum ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure that fall prevention interventions were in place as care planned for one resident (R3) who is a high risk for falls out...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure a safe and sanitary environment in the hallway ...
Read full inspector narrative →
Apr 2023
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that residents were free of abuse/physical assault. This fai...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide appropriate person-centered and individualized psychosocial and mental health services to meet the assessed needs of ...
Read full inspector narrative →
Apr 2023
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to provide wheelchair arm rest for 1 (R4) and arm rest pads for 2 (R12, R15) of seven residents reviewed for accommodation of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Interviews and records review, the facility failed to address advance directives with residents and ensure documentatio...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, facility failed to follow their policy to ensure residents are free from physical abuse by providing necessary care in services thus resulting in a female residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide an environment free from accident hazards by a.) having an exposed light bulb without a cover and no ability for one r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews. The facility failed to A) follow their infection prevention and control policy when staff entered a room of one [R61] resident on transmission-ba...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observations, interviews and records review, the facility failed to ensure a safe system of narcotic storage/disposition for four (R26, R50, R22, R57) residents, failed to accurately reconcil...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to follow their recipes and give adequate portion sizes. This failure has the potential to affect all 163 residents receiving foo...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to a.) ensure food items were properly labeled and dated; b.) the facility failed to clean ice machine; c.) the facility failed t...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to ensure garbage and refuse were disposed of properly by not closing the lids of the dumpsters outside the facility. This defici...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to follow their abuse policy for one resident (R1) out of four residents reviewed abuse. This failure resulted in a staff member being verbally...
Read full inspector narrative →
Feb 2023
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
Based upon observation, interview and record review the facility failed to ensure accuracy of assessment (re: risk for pressure ulcer) and failed to provide timely incontinence care for one of three r...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based upon record review and interview the facility failed to ensure accuracy of (risk for skin breakdown) assessment for one of three residents (R1) reviewed for pressure ulcer.
Findings include:
R1'...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based upon observation, interview and record review the facility failed to provide ADL (Activities of Daily Living) care to two ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based upon observation, interview and record review, the facility failed to follow policies & procedures and failed to ensure that sufficient nursing staff were available to meet the needs for two of ...
Read full inspector narrative →
Feb 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on interview and record review, failed to follow their policy to be free from physical abuse by providing necessary care in services thus resulting in a male resident (R2) physically assaulting ...
Read full inspector narrative →
Nov 2022
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure two residents (R4 and R5) were free from resident-to-resident physical assault. This failure resulted in R5 sustaining a scratch to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to ensure one resident (R2) was free from misappropriation of resident property by a staff member.
Findings include:
On 11/07/22 at 10:30 AM...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to report an allegation of resident-to-resident (R4 and R5) physical assault.
Findings include:
On 11/09/2022 at 9:33 AM, R5 (R4's roommate)...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 39% turnover. Below Illinois's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: Federal abuse finding, 8 harm violation(s), $532,728 in fines, Payment denial on record. Review inspection reports carefully.
- • 74 deficiencies on record, including 8 serious (caused harm) violations. Ask about corrective actions taken.
- • $532,728 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Austin Oasis, The's CMS Rating?
CMS assigns AUSTIN OASIS, THE an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Austin Oasis, The Staffed?
CMS rates AUSTIN OASIS, THE's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 39%, compared to the Illinois average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Austin Oasis, The?
State health inspectors documented 74 deficiencies at AUSTIN OASIS, THE during 2022 to 2025. These included: 8 that caused actual resident harm and 66 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Austin Oasis, The?
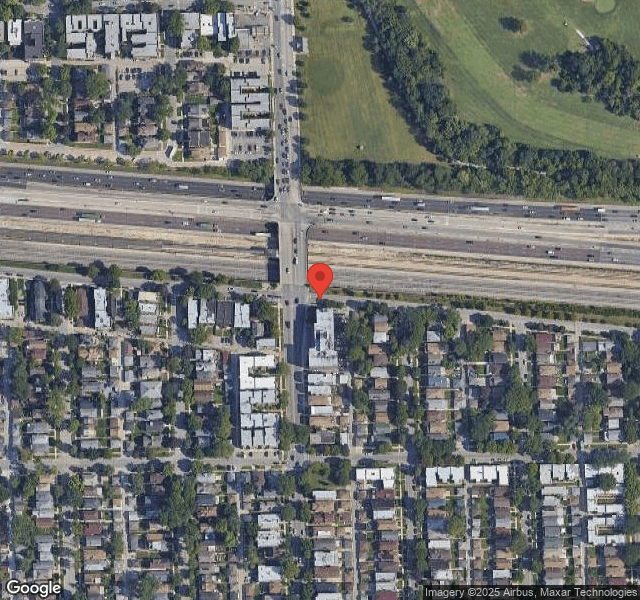
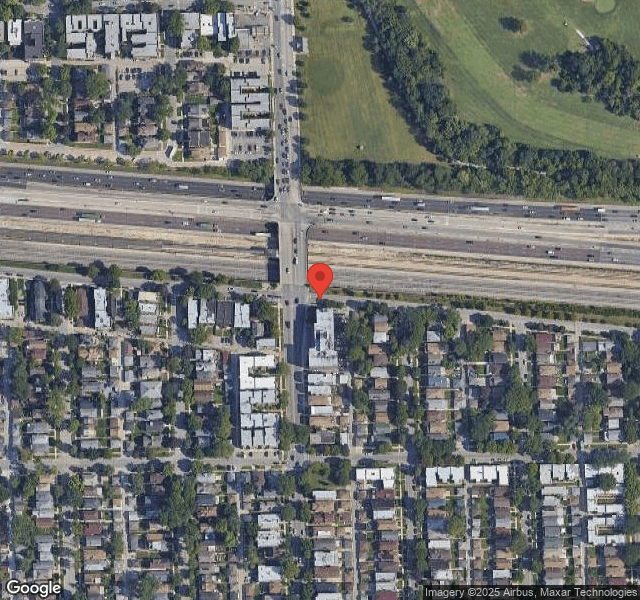
AUSTIN OASIS, THE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by ICARE CONSULTING SERVICES, a chain that manages multiple nursing homes. With 216 certified beds and approximately 174 residents (about 81% occupancy), it is a large facility located in CHICAGO, Illinois.
How Does Austin Oasis, The Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, AUSTIN OASIS, THE's overall rating (1 stars) is below the state average of 2.5, staff turnover (39%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Austin Oasis, The?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the substantiated abuse finding on record.
Is Austin Oasis, The Safe?
Based on CMS inspection data, AUSTIN OASIS, THE has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Austin Oasis, The Stick Around?
AUSTIN OASIS, THE has a staff turnover rate of 39%, which is about average for Illinois nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Austin Oasis, The Ever Fined?
AUSTIN OASIS, THE has been fined $532,728 across 6 penalty actions. This is 13.9x the Illinois average of $38,406. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Austin Oasis, The on Any Federal Watch List?
AUSTIN OASIS, THE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.