Belhaven Nursing & Rehab Center



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Belhaven Nursing & Rehab Center has received a Trust Grade of F, indicating significant concerns about the quality of care, as it falls in the lowest category. It ranks #479 out of 665 facilities in Illinois, placing it in the bottom half of nursing homes in the state, and #156 out of 201 in Cook County, meaning there are only a handful of better local options. While the facility is showing improvement, reducing issues from 29 in 2024 to 17 in 2025, it still faces serious problems, including a concerning $413,912 in fines, which is higher than 85% of facilities in Illinois. Staffing is a relative strength with a lower turnover rate of 39%, compared to the state average of 46%, but the facility has less RN coverage than 95% of state facilities, meaning residents may not receive the best medical oversight. Specific incidents include one resident whose pressure ulcer worsened due to inadequate treatment, and instances of physical altercations between residents that resulted in injuries, highlighting both serious care lapses and the need for better supervision.
- Trust Score
- F
- In Illinois
- #479/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 39% turnover. Near Illinois's 48% average. Typical for the industry.
- Penalties ✓ Good
- $413,912 in fines. Lower than most Illinois facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 13 minutes of Registered Nurse (RN) attention daily — below average for Illinois. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 86 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (39%)
9 points below Illinois average of 48%
Facility shows strength in fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
Near Illinois avg (46%)
Typical for the industry
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 86 deficiencies on record
Aug 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record reviews, facility failed to administer resident's medications according to physicia...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
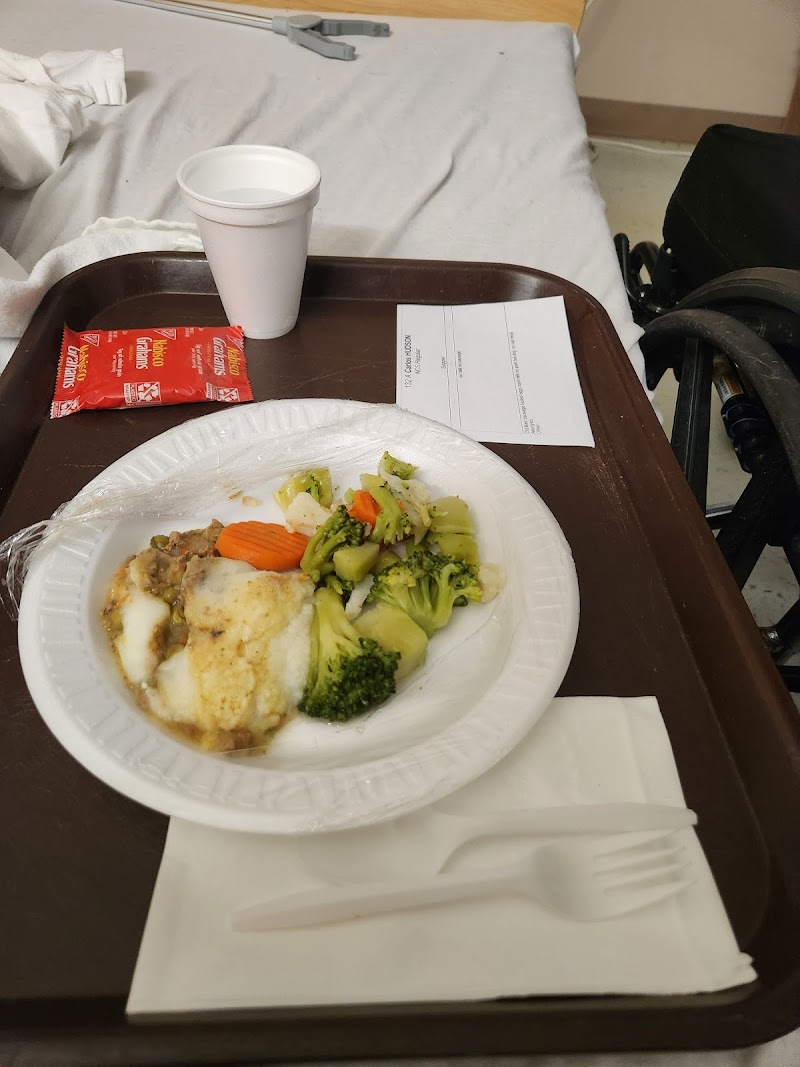
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure that residents were provided meals and snacks at appropriate times, in accordance with 42 CFRS483.60(f)(1) Each reside...
Read full inspector narrative →
Aug 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement resident-directed care consistent with the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0808
(Tag F0808)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to a.) ensure drinks consumed are in the appropriate form...
Read full inspector narrative →
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow a physician order and monitor a resident's vital signs for o...
Read full inspector narrative →
May 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
Based on observations, interview and record review, the facility failed to ensure that the resident's call light system was working properly. This failure has the potential to affect 64 residents that...
Read full inspector narrative →
May 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interviews, and record reviews the facility failed to maintain a safe, comfortable home like environment,[A] failed to maintain room temperatures for four [R4, R5, R6, R7] of sev...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure that resident's medications are administered as ordered by the physician. This failure affected three residents (R1, R2 and R3) of th...
Read full inspector narrative →
Mar 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, and record review, the facility failed to provide necessary treatment and services to promote healing of ex...
Read full inspector narrative →
Mar 2025
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that one resident (R1) with a pressure ulcer, received the n...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to respond to call lights used for staff assistance f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to follow their policy for scheduled medication administration time frame. This failure affected one resident (R2) reviewed for m...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide a functioning call device for a dependent res...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure that a resident is free from physical assault from another resident. This failure affected one resident (R2) who was physically assa...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to a.) provide adequate supervision and monitoring for r...
Read full inspector narrative →
Jan 2025
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policy on abuse to protect residents' rights to be fre...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on interview and record review, the facility failed to provide appropriate supervision to four (R2, R3, R4, and R5) residents while in the dining room out of four residents reviewed for supervis...
Read full inspector narrative →
Oct 2024
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to obtain and document the code status in the resident's ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to ensure that one resident's (R115) privacy curtain in ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to provide Activity of Daily Living (ADL) care to one resident seeking assistance with care (R109) in a total sample size of 74 re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement pressure ulcer prevention interventions for residents at risk for pressure ulcers. This failure has the potential t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide the fall prevention interventions as stated i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure that the urinary drainage bag was hanging below...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure that the nebulizer mask was contained and faile...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record review, the facility failed to ensure incoming and outgoing nurses counted the controlled medications/substances during shift change. This failure affecte...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review the facility failed to ensure that four residents (R55, R104, R116 and R118) ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure multidose medications have open and discard dates and failed to ensure a multidose medication of a discharged resident ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure that the two wall heating unit vents in dining room and the hallway on the third floor are maintained in good repair a...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interviews and record review the facility failed to accurately log dish machine temperatures and failed to ensure that that the dish machine was functioning properly. This failur...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Findings include:
On 10/28/24 at 11:13am, V32 (Certified Nursing Assistant/CNA) observed cleaning R148 with no PPE (Personal Protective Equipment) gown on. EBP (Enhance Barrier Precaution) sign on the...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to follow policies and procedures for immunization of residents against pneumococcal disease in accordance with national standards of practice...
Read full inspector narrative →
Oct 2024
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure that the medications were safely locked up in t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to report to IDPH (Illinois Department of Public Health) within require...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to ensure that call lights are within reach for 7 of 7 residents reviewed for call lights in the sample. This failure affected R5...
Read full inspector narrative →
Sept 2024
3 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review the facility failed to follow Medical Doctor's orders for PRN (as needed) wou...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review the facility failed to ensure that one patient's (R6) pain was managed with p...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review the facility failed to ensure that four patients (R2, R5, R6 and R8) were pro...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure that resident's medications are administered as ordered by the physician. This failure affected three residents (R1, R2, and R3) out ...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
The facility failed to follow provider orders and change the wound treatment plan for one resident (R4) out of a total sample of three residents (R4, R10, R11) for review.
Findings include:
7/11/2024 ...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents were free from physical restraints i...
Read full inspector narrative →
Mar 2024
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure that residents were free of abuse/physical assa...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to: adequately supervise and monitor a resident(R2) who has a history ...
Read full inspector narrative →
Mar 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to recognize, evaluate, and address weight loss; and the facility faile...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0776
(Tag F0776)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure radiological services were provided, as indicated by the phy...
Read full inspector narrative →
Jan 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure that a resident (R7) remained free from abuse, in a sample of three residents reviewed. This failure resulted in R7 being verbally a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to ensure the proper amount of fabric layers were used for one resident (R1) using a low air loss mattress out of three depen...
Read full inspector narrative →
Dec 2023
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure that Nurses documented weekly skin checks in the...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to follow policy/procedures and failed to ensure that ADL (Activities of Daily Living) care was provided to three of four dependen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to follow physician orders, failed to ensure that medications were administered as ordered, failed to notify the physician regardi...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to ensure that sufficient nursing staff were available to meet the needs for three of four dependent residents (R1, R3, R4) review...
Read full inspector narrative →
Nov 2023
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to follow their policy to ensure call lights are within reach for 1 resident (R373) out of three residents reviewed for call ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to follow their Guidelines for Cardiopulmonary Resuscitation-CPR by ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to administer medications as ordered by the physician for 1 (R43) of 2 (R105) residents reviewed for providing care according to p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, the facility failed to follow their policy and procedure on use of linen with an air loss mattress for 3 residents (R10, R87, and R104) of 8 resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to follow their Urinary Catheters policy by not placing a resident's (R38) urinary drainage bag in a privacy bag for 1 of 3 r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review the facility failed to follow their midline intravenous catheter and periphe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to follow their Oxygen Administration Guidelines by not following physician orders and changing oxygen tubing weekly for 1 (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to ensure that a resident (R15) was free from unnecessary anti-psychotic medications for 1 out of 5 residents reviewed for un...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to ensure a medication error rate of less than 5% for 1 (R43) of 2 (R43, R105) residents observed during medication administration...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure a resident was free from a significant medication error related to anticonvulsant medication administration for 1 (R43)...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to ensure food trays and beverages were covered during transportation to residents' rooms to prevent contamination; failed to...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure a Registered Nurse was on duty 8 consecutive hours 7 days a w...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to ensure food trays and beverages were covered during transportation to residents' rooms to prevent contamination; failed to...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to follow their Garbage and Refuse policy by not disposing garbage in a sanitary manner. This has the potential to affect all...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review the facility failed to follow their policy to ensure proper infection control protocols are followed such as performing hand hygiene while distributin...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to have an effective pest control program. This has the potential to affect all 171 residents residing at the facility.
Findi...
Read full inspector narrative →
Oct 2023
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide a shower chair to accommodate a resident's need due to physical limitations. This affected one resident (R4) out of 2...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure that residents who depend on staff's assistance for their ADL (Activities of Daily Living) care receive showers. This ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to administer medications as ordered by the physician and failed to document the reasons for not administering medications as ordered. This fa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0917
(Tag F0917)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide dressers for residents to keep personal cloth...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure that the two community shower rooms on the first floor and the only available shower room on the third floor were in a...
Read full inspector narrative →
Jun 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0573
(Tag F0573)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to provide requested medical records for one resident (R3) out of three...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to provide daily Registered Nurse (RN) coverage. This failure has the p...
Read full inspector narrative →
May 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record review, the facility failed to follow their call lights policy by failing to place ...
Read full inspector narrative →
Feb 2023
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R12 is a [AGE] year-old male who has a diagnosis of but not limited to Covid-19, Type 2 Diabetes Mellitus with Ketoacidosis with...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide housekeeping services necessary to maintain a sanitary and comfortable environment. This failure affected one residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to obtain a physician's order for one resident (R3) on G-tube feeding;...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
On 2/14/23 at 10:30 am, surveyor observed first floor dining room with dried food and crumbs on floor and base of tables dirty with dust, stains, and dried food.
On 2/14/23 at 11:00 am on the third fl...
Read full inspector narrative →
Dec 2022
8 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** On [DATE] at 11:45 AM Surveyor observed a free- standing oxygen tank at the bedside in R146's room.
V16 (Licensed Practical Nurs...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to have a doctor's order for one resident (R146) who had...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
On 12/05/22 at 12:32 PM observed lunch tray pass in the third-floor dining room. Surveyor observed staff person passing lunch trays, staff person did not use alcohol-based hand sanitizer or wash their...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0924
(Tag F0924)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure that the handrail on the 2nd floor is firmly secured to the wall. This failure has the potential to affect all 59 resi...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to follow their policy for conducting healthcare worker background checks on all staff. This failure has the potential to affect all 163 resid...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review the facility failed to ensure expired food was discarded on or before the expiration date in the walk-in refrigerator. This failure has the potential ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0888
(Tag F0888)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to follow their policy to ensure that all facility employees have received a dose of a single-dose Covid-19 vaccine or all doses of a multiple...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to maintain an effective pest control program to ensure that the facility is free of roaches. This failure has the potential to a...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 39% turnover. Below Illinois's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: Federal abuse finding, 12 harm violation(s), $413,912 in fines, Payment denial on record. Review inspection reports carefully.
- • 86 deficiencies on record, including 12 serious (caused harm) violations. Ask about corrective actions taken.
- • $413,912 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Belhaven Nursing & Rehab Center's CMS Rating?
CMS assigns Belhaven Nursing & Rehab Center an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Belhaven Nursing & Rehab Center Staffed?
CMS rates Belhaven Nursing & Rehab Center's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 39%, compared to the Illinois average of 46%. This relatively stable workforce can support continuity of care. RN turnover specifically is 62%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Belhaven Nursing & Rehab Center?
State health inspectors documented 86 deficiencies at Belhaven Nursing & Rehab Center during 2022 to 2025. These included: 12 that caused actual resident harm and 74 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Belhaven Nursing & Rehab Center?
Belhaven Nursing & Rehab Center is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by INFINITY HEALTHCARE CONSULTING, a chain that manages multiple nursing homes. With 221 certified beds and approximately 173 residents (about 78% occupancy), it is a large facility located in CHICAGO, Illinois.
How Does Belhaven Nursing & Rehab Center Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, Belhaven Nursing & Rehab Center's overall rating (1 stars) is below the state average of 2.5, staff turnover (39%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Belhaven Nursing & Rehab Center?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the below-average staffing rating.
Is Belhaven Nursing & Rehab Center Safe?
Based on CMS inspection data, Belhaven Nursing & Rehab Center has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Belhaven Nursing & Rehab Center Stick Around?
Belhaven Nursing & Rehab Center has a staff turnover rate of 39%, which is about average for Illinois nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Belhaven Nursing & Rehab Center Ever Fined?
Belhaven Nursing & Rehab Center has been fined $413,912 across 9 penalty actions. This is 11.1x the Illinois average of $37,218. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Belhaven Nursing & Rehab Center on Any Federal Watch List?
Belhaven Nursing & Rehab Center is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.