BUCKINGHAM PAVILION




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Buckingham Pavilion in Chicago has a Trust Grade of C+, indicating that it is slightly above average but not exceptional. It ranks #122 out of 665 facilities in Illinois, placing it in the top half, and #42 out of 201 in Cook County, meaning there are only a few local options that are better. The facility is showing improvement, as it reduced its issues from 20 in 2023 to 9 in 2024. However, staffing is a concern, rated at 2 out of 5 stars with a high turnover rate of 57%, which is above the state average. Recently, there were specific incidents noted during inspections, such as staff not using gloves while handling food and failing to properly store food items, which could pose health risks to residents. Additionally, expired food was found in the kitchen, which raises concerns about food safety practices. On a positive note, the facility provides more RN coverage than 80% of Illinois facilities, which can help catch potential problems early. Overall, while Buckingham Pavilion has some strengths, particularly in RN coverage, its staffing issues and recent inspection findings suggest that families should carefully consider these factors when researching care for their loved ones.
- Trust Score
- C+
- In Illinois
- #122/665
- Safety Record
- Low Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 57% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $9,750 in fines. Lower than most Illinois facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 42 minutes of Registered Nurse (RN) attention daily — more than average for Illinois. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 29 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
10pts above Illinois avg (46%)
Frequent staff changes - ask about care continuity
Below median ($33,413)
Minor penalties assessed
9 points above Illinois average of 48%
The Ugly 29 deficiencies on record
Nov 2024
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and review of records the facility failed to follow their policy in providing privacy to 1 out...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observations, interview and review of records, facility failed to follow a resident's care plan to ensure the call light was within reach for 1 (R98) out of three residents reviewed for call ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide privacy and confidentiality for three (R37, R44, R82) resident's personal medication administration record.
Finding in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, facility failed to follow their policy to ensure routine wellbeing checks are done for 1 (R45) out of three residents reviewed for activities of d...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews the facility failed to follow their enteral tube feeding via pump policy to ensure 1 (R21) resident's enteral nutrition bottles were labeled befor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and review of records the facility failed to provide dental services for a resident who has di...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on interview and record review, facility failed to follow their policy to provide influenza and pneumococcal vaccination and failed to document resident education for the vaccinations for 3 resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to refer residents with newly evident or possible serious mental disor...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Medical Records
(Tag F0842)
Minor procedural issue · This affected most or all residents
Based on observations, interviews, and record review the facility failed to grant access of the residents' electronic health records to the survey team timely. These failures have the potential to aff...
Read full inspector narrative →
Dec 2023
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews the facility failed to provide care in a manner to promote dignity for two residents (R31, R50) reviewed for dignity in a total sample of 18 resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to clarify a physician's order for one (R51) resident out of a total sample of 18 residents reviewed for medications.
Findings include:
R51...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to follow their policy to complete a nutritional assessmen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure respiratory care equipment was stored in a manner to prevent possible contamination from viral and/or bacterial pathog...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to label open insulins for 2 residents (R15, R54) on 1 of 6 medication carts reviewed for medication storage in a sample of 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to follow physician's orders for a specialized diet and update the resident's (R31) comprehensive care plan to correspond to ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to ensure standardized recipes were followed during pureed food preparation. This failure has the potential to affect 6 residents...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected most or all residents
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to use utensils or wear food handling gloves while handling a resident's (R31) food. The facility also failed to ensure food ...
Read full inspector narrative →
Feb 2023
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure that one resident's (R4) urinary catheter drainage bag was covered with a privacy cover. This failure affected one resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation and interviews, the facility failed to ensure that a call light was within reach for one resident (R40) from a sample of 45.
Findings include:
During patient rounds on 01/30/23 a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview, and record review, the facility failed to check placement of the gastrostomy tube before connecting the tube feeding after staff performed ADL (Activities of Daily Living) care for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure the low air loss mattress setting was based on resident's weight and/or mode for 1 (R52) resident reviewed for pressure...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record review, the facility failed to ensure that a staff member used personal protective equipment (PPE) and performed hand hygiene before entering and exiting a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to have an operational call light for one resident (R55)...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected multiple residents
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
Based on observation, interviews, and record review, the facility failed to ensure that oxygen tubing and humidifier bottle were changed and dated for 5 residents: R13, R46, R48, R52 and R74. These fa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to maintain shift change accountability records for controlled substances for residents' controlled medications. This failure has the potentia...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that residents' expired eye drops were discard...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure expired food was discarded on or before the expiration date in the walk-in cooler. This failure has the potential to a...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • 29 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • 57% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is Buckingham Pavilion's CMS Rating?
CMS assigns BUCKINGHAM PAVILION an overall rating of 4 out of 5 stars, which is considered above average nationally. Within Illinois, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Buckingham Pavilion Staffed?
CMS rates BUCKINGHAM PAVILION's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 57%, which is 10 percentage points above the Illinois average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at Buckingham Pavilion?
State health inspectors documented 29 deficiencies at BUCKINGHAM PAVILION during 2023 to 2024. These included: 28 with potential for harm and 1 minor or isolated issues.
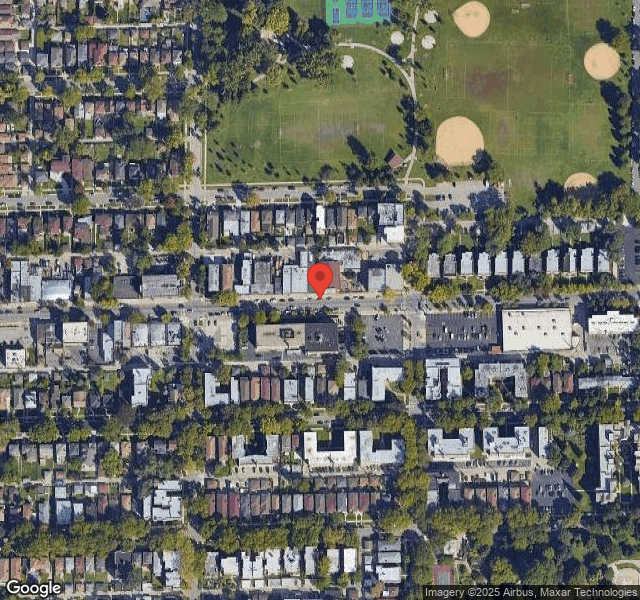
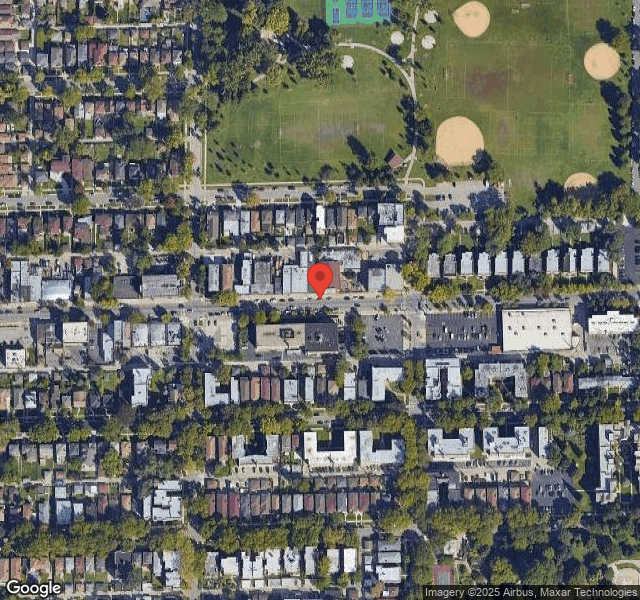
Who Owns and Operates Buckingham Pavilion?
BUCKINGHAM PAVILION is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 235 certified beds and approximately 105 residents (about 45% occupancy), it is a large facility located in CHICAGO, Illinois.
How Does Buckingham Pavilion Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, BUCKINGHAM PAVILION's overall rating (4 stars) is above the state average of 2.5, staff turnover (57%) is significantly higher than the state average of 46%, and health inspection rating (4 stars) is above the national benchmark.
What Should Families Ask When Visiting Buckingham Pavilion?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is Buckingham Pavilion Safe?
Based on CMS inspection data, BUCKINGHAM PAVILION has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 4-star overall rating and ranks #1 of 100 nursing homes in Illinois. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Buckingham Pavilion Stick Around?
Staff turnover at BUCKINGHAM PAVILION is high. At 57%, the facility is 10 percentage points above the Illinois average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Buckingham Pavilion Ever Fined?
BUCKINGHAM PAVILION has been fined $9,750 across 1 penalty action. This is below the Illinois average of $33,176. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Buckingham Pavilion on Any Federal Watch List?
BUCKINGHAM PAVILION is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.