CLARK MANOR




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Clark Manor in Chicago has a Trust Grade of F, indicating significant concerns about the quality of care provided. It ranks #346 out of 665 facilities in Illinois, placing it in the bottom half, and #111 out of 201 in Cook County, meaning there are better local options available. While the overall trend shows improvement, dropping from 12 issues in 2024 to 4 in 2025, the facility still has serious challenges, including a past incident where a resident was physically abused by another resident, which resulted in hospitalization for injuries. Staffing is a relative strength, with a low turnover rate of 26%, compared to the state average, and good RN coverage that exceeds 80% of Illinois facilities. However, the facility has faced fines totaling $55,796, which is average but still concerning, and specific deficiencies included inadequate food safety practices and insufficient weekend staffing, affecting the care of all residents.
- Trust Score
- F
- In Illinois
- #346/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ✓ Good
- 26% annual turnover. Excellent stability, 22 points below Illinois's 48% average. Staff who stay learn residents' needs.
- Penalties ✓ Good
- $55,796 in fines. Lower than most Illinois facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 39 minutes of Registered Nurse (RN) attention daily — about average for Illinois. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 37 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Low Staff Turnover (26%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (26%)
22 points below Illinois average of 48%
Facility shows strength in staff retention, fire safety.
The Bad
Below Illinois average (2.5)
Below average - review inspection findings carefully
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 37 deficiencies on record
Jul 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected multiple residents
Based on observation, interview and document review the facility failed to maintain an effective pest control program so that the facility is free of rodents on 3 of 4 resident floors.
Findings inclu...
Read full inspector narrative →
Jun 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that residents are free from abuse for one of three resident...
Read full inspector narrative →
Mar 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and document review the facility failed to ensure the rights of residents to be free from abuse in one of fou...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to a) ensure a residents' self-releasing seat belts (used...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based upon observation, interview, and record review the facility failed to ensure accuracy of wound location, failed to documen...
Read full inspector narrative →
May 2024
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure one (R221) resident had access to call light of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observations, interviews and records review, the facility failed to protect one (R101) resident's personal and confidential information of 6 residents reviewed for patient information protect...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to initiate a new Level I screen for a resident with a known mental il...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to follow physician order policy for prescribed gastrosto...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and records review, the facility failed to follow their policy on controlled drug count by fai...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to ensure the residents were treated with respect and dignity by not passing out meals to all residents sitting at a table at the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** On 5/14/24 at 8:11 PM R44 was observed sleeping on a specialty bed. R44 heel protectors were observed off of the resident and on...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to have sufficient staffing on the weekend. This failure affects all 245 residents residing in the facility reviewed for lack of staff.
Findin...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to a.) ensure food items were labeled and dated per facility policy, b.) keep food storage areas clean, c.) conduct hand wash...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to ensure dumpster was covered to prevent the harborage and feeding of pests, insects, and rodents. This deficient sanitation pra...
Read full inspector narrative →
Mar 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to prevent and protect residents from resident-to-resident physical ab...
Read full inspector narrative →
Nov 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and review of records, the facility failed to protect a resident's right (R15) to be free from...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interviews and records reviewed, the facility failed to report and initiate an investigation of an injury of unknown source in the time frame required resulting in the delay of the investigat...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and review of records, the facility failed to follow policy in discarding expired medications ...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the call light was within reach for 1 resident (R1) out of 4 residents reviewed for call lights.
Findings include:
R1'...
Read full inspector narrative →
Jun 2023
6 deficiencies
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure two medication carts were free of expired medications. This failure has the potential to effect 25 residents receiving ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observations, interviews and records review, the facility failed to ensure food served was palatable, attractive, and appetizing for four (R164, R145, R57, R155) residents reviewed for food q...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and review of records the facility failed to follow multiple policies related to the following: Failed to maintain ice free from outside leaks coming from sanitary s...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and review of records the facility failed to remove garbage in a safe and efficient manner per policy to prevent garbage from overflowing with lids to contain garbag...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and review of records the facility failed to place signs per policy for two residents (R168 and R176) who are in contact precautions for diagnosis of infectious dise...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and review of records the facility failed to address maintenance issues with the ice machine that was exposed to leakage from an unclean source.
These failures have ...
Read full inspector narrative →
Apr 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and document review the facility failed to maintain an effective pest control program so that th...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based upon observation, interview and record review the facility failed to ensure that the menu was followed for 4 of 4 (R1, R2,...
Read full inspector narrative →
Jan 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow physician's orders to administer medication in accordance to acceptable clinical practice for 2 (R5, R7) of 4 resident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a medication pass error rate of <5% for 2 (R5, R7) of 4 residents observed for medication administration. There wer...
Read full inspector narrative →
Sept 2022
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record reviews, the facility failed to maintain accurate code status orders that follow a ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, the facility failed to (a) assess the removal of a resident's (R219) urinary catheter as soon as possible, (b) provide a dignity bag for a residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to properly label an opened insulin vial for 1 (R166) ou...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and records review, the facility failed to provide dental services for one resident (R171) revi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to follow their menu and provide a nutritionally equivalent product (due to making a food substitution change) for residents on me...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations, interviews and record review the facility failed to ensure food was served in a sanitary manner for 5 residents (R7, R25, R36, R84, R176) receiving dessert served from the kitch...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to properly store the ice scoop and wash the portable ice coolers for the residents residing on floors 2 through 5. This deficien...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 26% annual turnover. Excellent stability, 22 points below Illinois's 48% average. Staff who stay learn residents' needs.
- • Multiple safety concerns identified: Federal abuse finding, 1 harm violation(s), $55,796 in fines, Payment denial on record. Review inspection reports carefully.
- • 37 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $55,796 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (23/100). Below average facility with significant concerns.
About This Facility
What is Clark Manor's CMS Rating?
CMS assigns CLARK MANOR an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Clark Manor Staffed?
CMS rates CLARK MANOR's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 26%, compared to the Illinois average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Clark Manor?
State health inspectors documented 37 deficiencies at CLARK MANOR during 2022 to 2025. These included: 1 that caused actual resident harm and 36 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
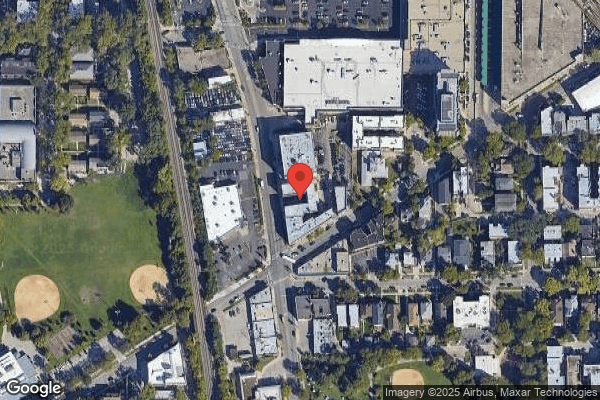
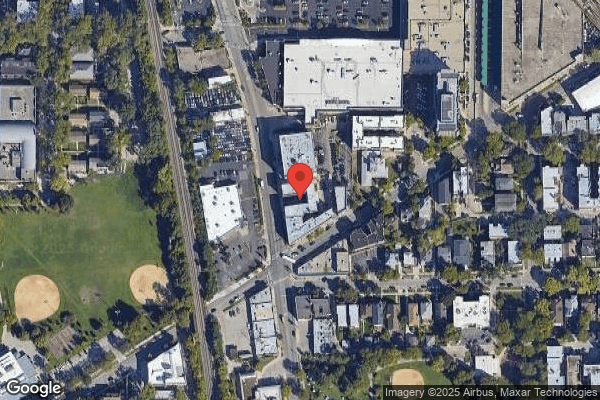
Who Owns and Operates Clark Manor?
CLARK MANOR is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by LEGACY HEALTHCARE, a chain that manages multiple nursing homes. With 267 certified beds and approximately 241 residents (about 90% occupancy), it is a large facility located in CHICAGO, Illinois.
How Does Clark Manor Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, CLARK MANOR's overall rating (2 stars) is below the state average of 2.5, staff turnover (26%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Clark Manor?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the below-average staffing rating.
Is Clark Manor Safe?
Based on CMS inspection data, CLARK MANOR has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Illinois. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Clark Manor Stick Around?
Staff at CLARK MANOR tend to stick around. With a turnover rate of 26%, the facility is 20 percentage points below the Illinois average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly. Registered Nurse turnover is also low at 13%, meaning experienced RNs are available to handle complex medical needs.
Was Clark Manor Ever Fined?
CLARK MANOR has been fined $55,796 across 1 penalty action. This is above the Illinois average of $33,637. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Clark Manor on Any Federal Watch List?
CLARK MANOR is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.