FOSTER HEALTH & REHAB CENTER



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
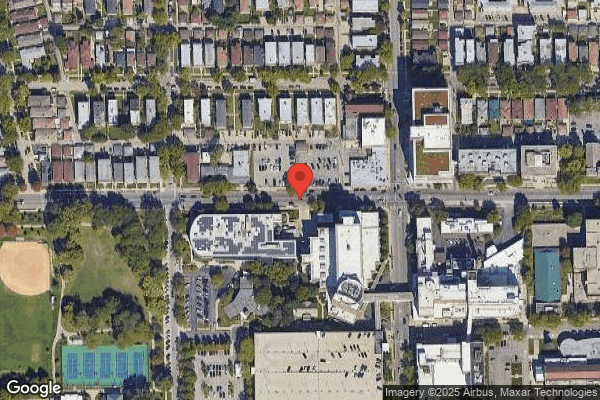
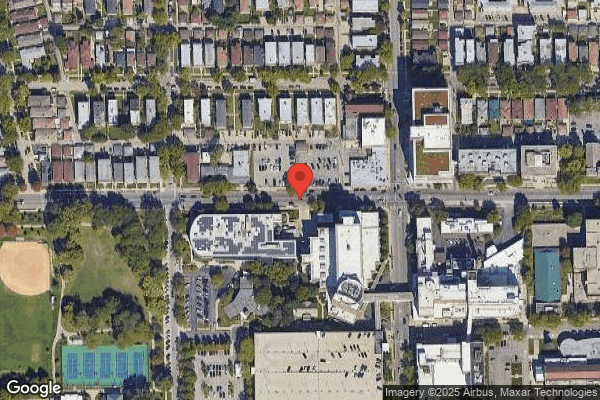
Foster Health & Rehab Center has received a Trust Grade of F, indicating significant concerns regarding its operations and care quality. It ranks #526 out of 665 facilities in Illinois, placing it in the bottom half, and #171 out of 201 in Cook County, meaning there are only a few local options that perform better. Fortunately, the facility is trending towards improvement, reducing its reported issues from 23 in 2024 to just 1 in 2025. Staffing is a relative strength, with 2 out of 5 stars and a turnover rate of 54%, which is close to the state average. However, the facility has faced serious fines totaling $151,119, indicating compliance problems, and specific incidents include a critical failure to administer essential medications to 37 residents on two consecutive days and a serious incident where one resident was subjected to hair-pulling by another, raising concerns about resident safety and care standards.
- Trust Score
- F
- In Illinois
- #526/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ⚠ Watch
- $151,119 in fines. Higher than 93% of Illinois facilities. Major compliance failures.
- Skilled Nurses ✓ Good
- Each resident gets 59 minutes of Registered Nurse (RN) attention daily — more than average for Illinois. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 58 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
Near Illinois avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
The Ugly 58 deficiencies on record
May 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to update a resident care plan as exacerbation of neurological symptoms began to occur. This failure affected 1 (R3) resident reviewed for car...
Read full inspector narrative →
Dec 2024
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to protect residents' rights to be free from mental and p...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow its abuse policy of reporting incidents and/or allegations o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow its abuse policy on investigating incidents and/or allegatio...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and review of records the facility failed to identify and provide behavioral services to 1 (R1)...
Read full inspector narrative →
Oct 2024
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure the call light was within reach for one (R12) out of four residents reviewed in a total sample of 14 for call lights.
...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to accurately document advanced directives code status for 1 residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policies and procedures for the Preadmission Screening...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to maintain a medication error rate of less than 5% for 3 (R6, R22, R27) of 11 residents reviewed for medication administrati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to ensure that two residents (R6, R27) were free of any significant medication errors out of eleven residents reviewed for me...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide and follow menus and recipes to ensure menu variety for three (R2, R5, R15) out of three residents reviewed for pureed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to label and date food items in resident personal refrigerators and failed to discard unlabeled/undated spoiled foods in resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected multiple residents
Based on interview and record reviews, the facility failed to complete the comprehensive Minimum Data Set (MDS) assessments using the CMS-specified Resident Assessment Instrument (RAI) process within ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete MDS (Minimum Data Set) assessments using CMS - specified R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0642
(Tag F0642)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that each Minimum Data Set (MDS) assessment was certified as...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policy to develop a comprehensive, person-centered car...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record reviews, the facility failed to follow their policy and procedure to ensure emergency supplies in the crash cart were securely locked at all times when no...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to perform monthly medication regimen review (MRR) for 4...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to properly date opened multi-dose inhalers for 4 residents (R2, R23, R28, R31) and to dispose a house stock medication after th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0808
(Tag F0808)
Could have caused harm · This affected multiple residents
R1's admission record showed initial admission date on 1/24/2022 with diagnoses not limited to Chronic obstructive pulmonary disease, Essential (primary) hypertension, Alzheimer's disease, Epilepsy, G...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure food items were properly labeled, dated, and stored, failed to properly rotate food using First In, First Out (FIFO) g...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to handle linen in a manner to prevent cross contamination, failed to conduct an annual review of its infection control policy an...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to investigate and report an allegation of abuse for one of three resi...
Read full inspector narrative →
Feb 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain dignity for three (R1, R2, R3) residents rev...
Read full inspector narrative →
Nov 2023
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one resident's (R2) indwelling catheter drainage bag was covered. This failure affected one resident (R2) reviewed for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a resident's call light was accessible within ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to obtain a doctor's order and document the code status in one residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that a resident's low air loss (LAL) mattress ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure an extra tracheostomy (trach) tube was stored ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0813
(Tag F0813)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide a thermometer for four resident (R10, R30, R3...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to store biologicals in a safe manner, and failed to label opened multi dose vials. These failures have the potential to affect ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 7. R29 has diagnoses which includes iron deficiency anemia, repeated falls, lymphedema, difficulty in walking, essential hyperte...
Read full inspector narrative →
Aug 2023
6 deficiencies
1 IJ (1 facility-wide)
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0725
(Tag F0725)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
Based on observation, interview, and record review, the facility failed to provide sufficient nursing staff and failed to follow their medication policy to ensure residents received essential medicati...
Read full inspector narrative →
SERIOUS
(H)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure resident medications were administered according to physicia...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to perform wound care treatment as ordered by physician on 06/05/2023 ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to complete grievance forms to document and explain in detail the nature of resident concerns from August 2022 utill July 2023, ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, facility failed to have the services of a full time Director of Nursing. This failure has the potential to affect all 37 residents residing in the f...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policy to administer medications in accordance with th...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide daily treatment as ordered, and failed to ens...
Read full inspector narrative →
Dec 2022
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure call lights were within reach for 1 (R5) out of 6 residents reviewed in a total sample of 12 for call lights.
Findings...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on Observations, interviews and records review, the facility failed to follow their medication administration policy for o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement adequate fall prevention precautions during...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to date and prevent nasal cannula from touching the floor for 1 (R20) out of 1 resident reviewed for oxygen usage in a sample of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a medication error rate was less than 5% for 3 of 4 residents (R183, R86, R27) in the sample reviewed. There were 35 o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure 1 (R27) of 4 residents observed for medication...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their policy and procedure to ensure antibiotic use is monitored and to determine if antibiotics are ordered accordingly based on ap...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide non-disposable cutlery and dishware including cups, bowls, and plates at all meals. These failures affected 4 (R3, R5...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete the quarterly Minimum Data Set (MDS) assessments using the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide restorative treatment services to prevent the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record reviews, the facility failed to follow policy on Influenza and Pneumococcal Vaccine for 4 (R25, R1...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete the annual Minimum Data Set (MDS) assessments using the CM...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to develop and implement a baseline care plan for each resident that includes the instructions needed to provide effective and person-centered...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure food stored in the freezer was stored in a sanitary manner. This failure has the potential to affect 35 residents who ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
R2 has diagnosis not limited Urinary Calculus, Urogenital Implants, Hydronephrosis with Renal & Ureteral Calculous Obstruction, Urinary Tract Infection, Dementia, Type 2 Diabetes Mellitus, Parkinson '...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to designate at least one qualified Infection Preventionist (IP) who is responsible for the facility's Infection Prevention and Control Progra...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected most or all residents
Based on interview and record reviews, the facility (a) failed to develop policies and procedures of COVID-19 immunizations for the residents; (b) failed to provide education regarding the benefits an...
Read full inspector narrative →
Nov 2022
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to implement adequate fall prevention and monitoring for one resident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policy to assure the social work staff assessed 3 (R2,...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 1 life-threatening violation(s), 3 harm violation(s), $151,119 in fines, Payment denial on record. Review inspection reports carefully.
- • 58 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $151,119 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Foster Health & Rehab Center's CMS Rating?
CMS assigns FOSTER HEALTH & REHAB CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Foster Health & Rehab Center Staffed?
CMS rates FOSTER HEALTH & REHAB CENTER's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 54%, compared to the Illinois average of 46%. RN turnover specifically is 77%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Foster Health & Rehab Center?
State health inspectors documented 58 deficiencies at FOSTER HEALTH & REHAB CENTER during 2022 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 3 that caused actual resident harm, and 54 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Foster Health & Rehab Center?
FOSTER HEALTH & REHAB CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 46 certified beds and approximately 37 residents (about 80% occupancy), it is a smaller facility located in CHICAGO, Illinois.
How Does Foster Health & Rehab Center Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, FOSTER HEALTH & REHAB CENTER's overall rating (1 stars) is below the state average of 2.5, staff turnover (54%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Foster Health & Rehab Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the substantiated abuse finding on record, and the below-average staffing rating.
Is Foster Health & Rehab Center Safe?
Based on CMS inspection data, FOSTER HEALTH & REHAB CENTER has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Foster Health & Rehab Center Stick Around?
FOSTER HEALTH & REHAB CENTER has a staff turnover rate of 54%, which is 8 percentage points above the Illinois average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Foster Health & Rehab Center Ever Fined?
FOSTER HEALTH & REHAB CENTER has been fined $151,119 across 1 penalty action. This is 4.4x the Illinois average of $34,590. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Foster Health & Rehab Center on Any Federal Watch List?
FOSTER HEALTH & REHAB CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.