LITTLE VILLAGE NRSG & RHB CTR
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Little Village Nursing and Rehabilitation Center has received a Trust Grade of F, indicating poor performance and significant concerns about the quality of care provided. Ranked #567 out of 665 facilities in Illinois, they are in the bottom half, and #178 out of 201 in Cook County, meaning there are very few local options that are worse. The facility is showing signs of improvement, as the number of issues decreased from 17 in 2024 to 8 in 2025, but they still face serious challenges. Staffing is relatively stable with a turnover rate of 33%, which is better than the state average, but they have only 1 out of 5 stars for staffing, suggesting a lack of adequate personnel. There are concerning financial fines totaling $252,644, which is higher than 91% of facilities in Illinois, indicating ongoing compliance issues. Specific incidents include a serious altercation between residents that resulted in one resident sustaining injuries requiring stitches, and reports of verbal abuse from staff members that left some residents feeling scared and anxious. While there are some strengths, such as a lower turnover rate, the overall atmosphere and safety concerns highlighted by these incidents suggest that families should approach this facility with caution.
- Trust Score
- F
- In Illinois
- #567/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 33% turnover. Near Illinois's 48% average. Typical for the industry.
- Penalties ○ Average
- $252,644 in fines. Higher than 75% of Illinois facilities. Some compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 14 minutes of Registered Nurse (RN) attention daily — below average for Illinois. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 46 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (33%)
15 points below Illinois average of 48%
Facility shows strength in fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
13pts below Illinois avg (46%)
Typical for the industry
Well above median ($33,413)
Significant penalties indicating serious issues
The Ugly 46 deficiencies on record
May 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to report an allegation of mental abuse (bullying) to the state survey agency. This failure affects 1 resident (R1) sampled for abuse reportin...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to complete a thorough investigation of verbal/mental abuse after an allegation of bullying was made. This failure affects 1 resident (R1) sam...
Read full inspector narrative →
Mar 2025
2 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure that 4 of 4 residents (R1, R2, R5, and R6) were free from phy...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to develop and implement appropriate measures to ensure adequate superv...
Read full inspector narrative →
Jan 2025
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
Based on interview and record review facility failed to document in the medical records the reason for one residents' (R1) transfer and discharge to the hospital out of three residents reviewed for tr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review facility failed to give a resident an involuntary discharge notice 30 days prior to the resident's discharge. This applies to one resident (R1) out of three reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review facility failed to follow their bed hold policy for one resident (R3) out of three resident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to let one resident (R1) return out of three residents reviewed transfers and discharges. This failure resulted in R1 not returning to the faci...
Read full inspector narrative →
Dec 2024
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of records and interviews the facility failed to provide the right of every resident to formulate advance direct...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to include urinary catheter use in R85's comprehensive care plan, have urinary catheter care orders, and maintain R85's dignity ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to transcribe hospital orders upon initial admission for one (R96) out of a total sample of 46 residents.
Findings include:
R96's Face Shee...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to a.) ensure the portable oxygen tank was on the correct setting, b.) ensure the oxygen tubing was stored to prevent contaminati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to have resident's medications readily available for administration, administer medications on time, and ensure accurate reco...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to obtain written informed consent prior to prescribing and administ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on review of records and interviews the facility failed to educate 2 residents (R73 and R250) on Covid- 19 vaccination per their policy on documentation of Covid-19 immunization. These failures ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and review of records the facility failed to ensure that resident room environment was in a sa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record reviews, the facility failed to discard medications not in their original packaging, label and date a used insulin pen, store unused insulin in the refrig...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on review of records and interviews the facility failed to educate 2 residents (R73 and R250) on influenza vaccination and 4 residents (R45, R73, R90 and R250) on pneumococcal immunization per t...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to provide Registered Nurse (RN) coverage for 8 consecutive hours in a 24-hour period on Mondays, Wednesdays, Thursdays, Fridays ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and review of records the facility failed to follow handling of clothes inside a net-like bag...
Read full inspector narrative →
Oct 2024
3 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0914
(Tag F0914)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure that residents have privacy curtains which extend around the bed. This failure affected Four residents (R8, R9, R10, a...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure that residents' call lights are functional and in good working order. This failure has the potential to affect 5 resid...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure that the large community shower room on the A-Wing is maintained in a sanitary manner free of patches black substance....
Read full inspector narrative →
Aug 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, facility failed to affirm the right of the resident to be free from verbal abuse. This def...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to revise a care plan for one (R1) of three residents reviewed for car...
Read full inspector narrative →
Nov 2023
9 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to follow their policy to protect the resident's right to be free fr...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0745
(Tag F0745)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews the facility social service staff failed to assist one resident[R83] in maintaining their...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to accurately document advanced directives code status for 1 residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure that medications were given as ordered by the physician for 2...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain a medication error rate below 5% as evidenced by 3 medication errors out of 28 opportunities, resulting in a medicat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility (a.) failed to properly discard a multi-dose insulin 28 days af...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to follow their policy and procedure to ensure that resid...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to a.) ensure food items were properly labeled, dated, and stored, b.) air dry the blender after being washed in the three-co...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to ensure dumpster was covered to prevent the harborage and feeding of pests, insects, and rodents. This deficient sanitation pra...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to serve food as planned on the cycle menu, and failed to ensure standardized recipes were followed during food preparation. This...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure the residents right to be free of verbal abuse in 1 (R1) of 3...
Read full inspector narrative →
Apr 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on interview and record review, facility failed to follow their policy to ensure resident had the right in receiving assistance in obtaining transportation when necessary for services outside th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, facility failed to follow their policy to ensure inital fall care plan interventions are in place for one (R3) of 3 resident reviewed for falls. This failure resu...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to follow their policy on medication administration for o...
Read full inspector narrative →
Jan 2023
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to ensure the call light for one resident (R69) was within reach. This failure affected one resident (R69) in a sample of 37 resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to have a doctor's order prior to administering a medicati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to dispose of loose pills in the bottom of medication cart A on the first floor, date opened multi-dose insulin Kwikpens for 2 res...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to ensure the bedroom bathroom toilet was properly working for four residents (R3, R27, R57 and R44) in a sample of 37 residents r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to don proper personal protective equipment (PPE) prior t...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure the Kitchen's main exhaust hood, exhaust fan, and wall fan were free of accumulation of grayish blackish material to p...
Read full inspector narrative →
Dec 2022
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement their abuse policy and conduct a pre-employment screening...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 33% turnover. Below Illinois's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: Federal abuse finding, 4 harm violation(s), $252,644 in fines. Review inspection reports carefully.
- • 46 deficiencies on record, including 4 serious (caused harm) violations. Ask about corrective actions taken.
- • $252,644 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Little Village Nrsg & Rhb Ctr's CMS Rating?
CMS assigns LITTLE VILLAGE NRSG & RHB CTR an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Little Village Nrsg & Rhb Ctr Staffed?
CMS rates LITTLE VILLAGE NRSG & RHB CTR's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 33%, compared to the Illinois average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Little Village Nrsg & Rhb Ctr?
State health inspectors documented 46 deficiencies at LITTLE VILLAGE NRSG & RHB CTR during 2022 to 2025. These included: 4 that caused actual resident harm and 42 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Little Village Nrsg & Rhb Ctr?
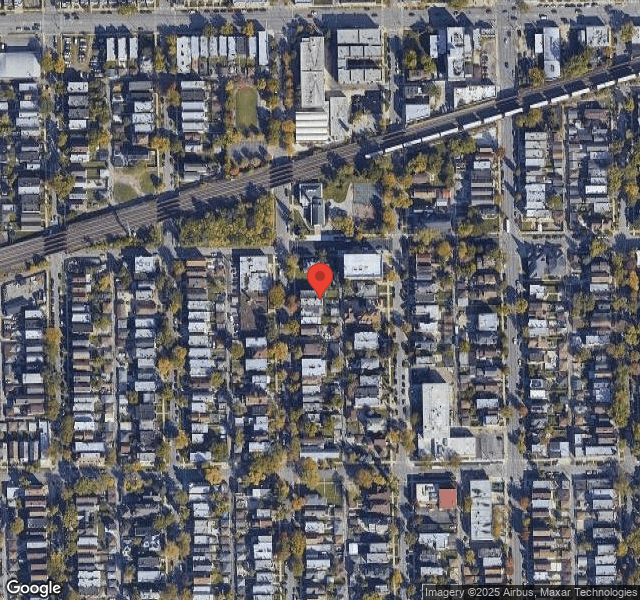
LITTLE VILLAGE NRSG & RHB CTR is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 106 certified beds and approximately 98 residents (about 92% occupancy), it is a mid-sized facility located in CHICAGO, Illinois.
How Does Little Village Nrsg & Rhb Ctr Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, LITTLE VILLAGE NRSG & RHB CTR's overall rating (1 stars) is below the state average of 2.5, staff turnover (33%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Little Village Nrsg & Rhb Ctr?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the below-average staffing rating.
Is Little Village Nrsg & Rhb Ctr Safe?
Based on CMS inspection data, LITTLE VILLAGE NRSG & RHB CTR has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Little Village Nrsg & Rhb Ctr Stick Around?
LITTLE VILLAGE NRSG & RHB CTR has a staff turnover rate of 33%, which is about average for Illinois nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Little Village Nrsg & Rhb Ctr Ever Fined?
LITTLE VILLAGE NRSG & RHB CTR has been fined $252,644 across 3 penalty actions. This is 7.1x the Illinois average of $35,605. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Little Village Nrsg & Rhb Ctr on Any Federal Watch List?
LITTLE VILLAGE NRSG & RHB CTR is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.