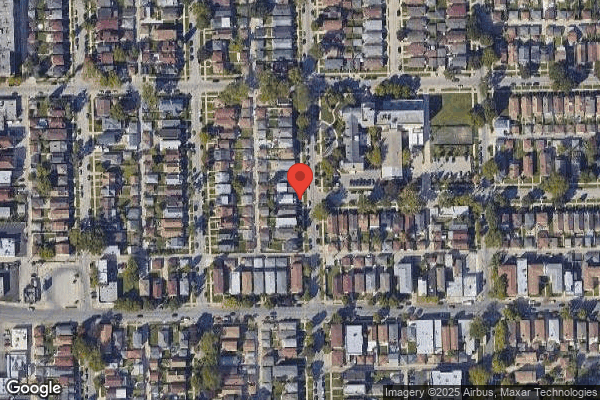
PEARL OF MONTCLARE, THE
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
The Pearl of Montclare has a Trust Grade of F, which indicates significant concerns and poor performance. Ranking #391 out of 665 facilities in Illinois places it in the bottom half, while its county rank of #126 out of 201 suggests limited local options that are better. The facility's trend is improving slightly, having reduced issues from 18 to 16 over the past year. Staffing is average with a turnover rate of 52%, and while RN coverage is also average, it does not stand out as a strength. Notably, the facility has concerning fines totaling $132,091, higher than 77% of Illinois facilities. There have been serious incidents, including a resident who fell and sustained a head injury because the facility failed to apply a protective helmet as required, and another resident who fractured a femur due to improper transfer techniques without a gait belt. Additionally, a resident fell and sustained a leg laceration, requiring stitches after safety measures were overlooked. Overall, while there are some improvements, the facility faces critical concerns that families should consider.
- Trust Score
- F
- In Illinois
- #391/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 52% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $132,091 in fines. Higher than 58% of Illinois facilities. Some compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 37 minutes of Registered Nurse (RN) attention daily — about average for Illinois. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 54 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Illinois average (2.5)
Below average - review inspection findings carefully
Near Illinois avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 54 deficiencies on record
May 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to ensure a medication administration error rate of <5% for 2 (R2 and R5) residents of 4 (R2, R4, R5, and R6) residents re...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to report an abuse allegation to Illinois Department of Public Health ...
Read full inspector narrative →
Mar 2025
14 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and records reviews, the facility failed to follow a resident's (R95) fall care plan intervention and physic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews the facility failed to obtain a physician order and to determine if self-a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to refer a resident (R67) to the appropriate state-designated author...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews the facility failed to ensure nail care was provided for three (R14, R27, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Resident #92
Unnecessary Meds, Psychotropic Meds, and Med Regimen Review
Based on observations, interviews, and record reviews, the facility failed to update a resident's (R92) comprehensive care pla...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
FACILITY
Medication Administration
F759
Based on observations, interviews, and record reviews, the facility failed to maintain a medication error rate of less than 5% for 1 (R51) of 3 residents review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to follow their menu and failed to follow cooking instructions. This affected all 108 residents receiving nutrition from the ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to follow physician orders for nectar-thick liquids for one resident (R40) out of a total sample of 22 residents.
Findings in...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure low air loss mattress devices were on the corre...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** On 3/11/25 at 9:36 AM, R48's resting in bed alert and able to verbalize needs. Surveyor noted R48's BiPAP mask on the floor conn...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident #37
Accidents
PLEASE SEE F700 CITATION FOR DETAILS.
Resident #41
Accidents
F700
Based on observation, interview and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0808
(Tag F0808)
Could have caused harm · This affected multiple residents
Findings include:
On 3/11/2025 at 12:15 PM, V15 (Certified Nurse Aide) assisted R40 with lunch meal. V15 stated R40 did not get a high calorie frozen dessert with the meal. V15 stated [V15] hasn't se...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
R16's Order Summary Report documents in part an active order for Enhance Barrier Precaution due to: wound every shift (order date 1/29/2025).
R16's Care Plan Report documents in part that R16 is on En...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to follow their policies and dispose of food items past their expiration/best buy/use by dates, label opened food item, store...
Read full inspector narrative →
Aug 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to utilize a gait belt during resident transfer, from toilet to wheelc...
Read full inspector narrative →
Jun 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to a.) monitor call light system and answer call lights ...
Read full inspector narrative →
Apr 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure residents who depend on staff assistance for th...
Read full inspector narrative →
Apr 2024
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide needed care or services by not ensuring compre...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to ensure the low air loss mattress was in the correc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure a resident receiving enteral feeding received ap...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** On 04/10/24 at 10:56 AM R106 was in bed without oxygen on. No tracheostomy in place. Oxygen tubing was noted to be in lying in a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record reviews, the facility failed to treat five residents (R4, R37, R53, R65, R91) with respect and dignity by not serving all the residents sitting at the sam...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to provide language support to non-English-speaking residents in accordance with professional standards of practice and facility ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record reviews, the facility failed to ensure that a staff member supervised residents (R4, R7, R12, R26, R37, R53, R60, R63, R65, R86, R90, R91) sitting in the ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to a.) provide thickened liquids as prescribed by physicia...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
On 4/10/24 at 12:45 PM, R13 stated that last Monday and Sunday 11-7 shift, R13 stated R13 rang R13's call button at 12 midnight and asked for pain medications but did not receive. R13 stated R13 was u...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R76's health record documented admission date on 5/18/2023 with diagnoses with not limited to Chronic obstructive pulmonary dise...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations, interviews and record reviews, the facility (a) failed to properly discard multi-dose inhaler and insulins on expiration dates for 6 residents (R68, R362, R8, R56, R1, R89), (b)...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to a.) ensure resident menus, individual food plan and preferences were followed affecting four residents (R29, R56, R75, R87), b...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review the facility failed to ensure food was served at a palatable temperature, and an appetizing appearance and taste. This deficient practice has the pote...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to a.) ensure food items were labeled and dated per facility policy, b.) discard expired and/or rotten foods, c.) follow manu...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to follow standards of professional practice and facility policy relative to infection prevention and control. This failure has t...
Read full inspector narrative →
Nov 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and records review, the facility failed to ensure resident safety for one resident (R2) of three residents r...
Read full inspector narrative →
Sept 2023
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement their Involuntary Transfer and Discharge Process policy a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide their bed hold policy, upon discharge to hospital, for one ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to permit a resident to return to the facility after hospitalization f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow its policy on infection control and prevention to prevent th...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to assert the rights of the residents by not ensuring residents were afforded the opportunity to choose their own food menu items. This failur...
Read full inspector narrative →
May 2023
12 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** On 05/02/2023 at 10:29 AM, surveyor observed R24 and V39 (Son/POA for R24) sitting in R24's room. R24 stated that she is blind a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and review or records, facility failed to follow their policy to report to Illinois Department of Public Health, the abuse incident for two residents (R42, R24) out of three residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and review or records, facility failed to follow their policy to conduct a thorough investigation of an abuse allegation for two residents (R42, R24) out of three residents reviewed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, the facility failed to ensure oxygen nasal cannula tubing and humidifier bottle was labelled with date for one resident (R55) reviewed for respira...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and records review, failed to discontinue a PRN (As Needed) psychotropic medication after 14 ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on interviews and review of records the facility failed to follow policy in offering, educating and documenting influenza and pneumococcal to 4 of 5 residents (R129, R54, R128, and R45) about th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
Based on interviews and review of records the facility failed to offer, provide education and documentation of Covid-19 to 4 of 5 residents (R129, R24, R128, and R45) about the benefits and risks of C...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure disposal of expired food items and follow prope...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed dispose of garbage and refuse properly. This failure has the potential to affect 80 residents residing in the facility.
Findings ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
On 05/04/2023 at 10:00 AM, surveyor observed V33 (Licensed Practical Nurse) pass medication to residents on the 2nd floor.
On 05/04/2023 at 10:12 AM, surveyor observed V33 go into R32's room with the...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and review of records the facility failed to follow Covid-19 testing policy during an outbreak to test residents and staffs exposed to a resident positive of Covid-1...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0888
(Tag F0888)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and review of records the facility failed to monitor Covid-19 vaccinations status of healthcare workers (employed and contracted) performing direct care to residents...
Read full inspector narrative →
Jan 2023
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to use a gait belt and or walker during transfer from wheelchair to be...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow a physician's order to change an indwelling urinary catheter...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 5 harm violation(s), $132,091 in fines, Payment denial on record. Review inspection reports carefully.
- • 54 deficiencies on record, including 5 serious (caused harm) violations. Ask about corrective actions taken.
- • $132,091 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (10/100). Below average facility with significant concerns.
About This Facility
What is Pearl Of Montclare, The's CMS Rating?
CMS assigns PEARL OF MONTCLARE, THE an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Pearl Of Montclare, The Staffed?
CMS rates PEARL OF MONTCLARE, THE's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 52%, compared to the Illinois average of 46%.
What Have Inspectors Found at Pearl Of Montclare, The?
State health inspectors documented 54 deficiencies at PEARL OF MONTCLARE, THE during 2023 to 2025. These included: 5 that caused actual resident harm and 49 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Pearl Of Montclare, The?
PEARL OF MONTCLARE, THE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PEARL HEALTHCARE, a chain that manages multiple nursing homes. With 96 certified beds and approximately 105 residents (about 109% occupancy), it is a smaller facility located in CHICAGO, Illinois.
How Does Pearl Of Montclare, The Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, PEARL OF MONTCLARE, THE's overall rating (2 stars) is below the state average of 2.5, staff turnover (52%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Pearl Of Montclare, The?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Pearl Of Montclare, The Safe?
Based on CMS inspection data, PEARL OF MONTCLARE, THE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Illinois. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Pearl Of Montclare, The Stick Around?
PEARL OF MONTCLARE, THE has a staff turnover rate of 52%, which is 6 percentage points above the Illinois average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Pearl Of Montclare, The Ever Fined?
PEARL OF MONTCLARE, THE has been fined $132,091 across 3 penalty actions. This is 3.8x the Illinois average of $34,400. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Pearl Of Montclare, The on Any Federal Watch List?
PEARL OF MONTCLARE, THE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.