WARREN BARR SOUTH LOOP




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Warren Barr South Loop has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #661 out of 665 in Illinois and #199 out of 201 in Cook County places this facility in the bottom tier for nursing homes in the area. While there is a slight improvement trend noted, with the number of issues decreasing from 21 to 17 over the past year, the overall picture remains troubling. Staffing is a major concern, with a low rating of 1 out of 5 stars and a high turnover rate of 62%, significantly above the state average. Additionally, the facility faced serious incidents, including a resident suffering a hematoma due to inadequate supervision and another resident who passed away after staff failed to monitor a tracheostomy properly. These findings highlight both the weaknesses in care and the critical need for families to weigh these factors carefully when considering this nursing home.
- Trust Score
- F
- In Illinois
- #661/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 62% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $237,213 in fines. Lower than most Illinois facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 35 minutes of Registered Nurse (RN) attention daily — about average for Illinois. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 73 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
16pts above Illinois avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
14 points above Illinois average of 48%
The Ugly 73 deficiencies on record
Sept 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observations interviews, and record reviews, facility failed to follow their policy to ensure residents have a homelike environment for 3 (R1, R8, R9) out 5 residents reviewed for homelike en...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure hemodialysis services were provided 3 times weekly as ordered by physician to a resident (R5). This failure has the potential to aff...
Read full inspector narrative →
Feb 2025
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to identify a resident's (R113) code status for one out of 35 reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record reviews, the facility failed to follow their policy and assess a resident's (R99) need for restraints at least quarterly for one resident out of a total sa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure low air loss mattress devices were on the corre...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow the smoking policy and smoking assessment to e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to follow their policies and procedures to ensure a resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a resident's food preference was followed for one (R81) out of 3 residents reviewed during dining observation in a fina...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to administer influenza and pneumococcal vaccines in a timely manner for three residents (R93, R118, R151) out of five residents reviewed fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to administer a COVID-19 vaccination in a timely manner for one resident (R118) out of five residents reviewed for immunizations.
Findings i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. R99's admission Record documents in part diagnoses of acute respiratory failure with hypoxia, stiffness of right hand, and co...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to safely secure medication in a locked storage area to l...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to prepare pureed food in appropriate diet consistency fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0808
(Tag F0808)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to provide therapeutic diets and dietary intervention...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed to ensure food items were properly labeled and dated, and failed to ensure kitchen staff wore appropriate hair covering. Thes...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record reviews, the facility failed to follow their infection control policies and procedu...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure residents who are unable to carry out ADLs (...
Read full inspector narrative →
Nov 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, facility failed to follow their policy to investigate an allegation of abuse for one of three residents (R4) in the sample of four.
Findings include:
On 11/17/...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to properly identify/assess a resident (R1) for the source of an injur...
Read full inspector narrative →
Oct 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to follow care plan interventions to provide adequate supervision as...
Read full inspector narrative →
Sept 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify resident's Responsible Party of pressure ulcer changes for 1...
Read full inspector narrative →
Aug 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Respiratory Care
(Tag F0695)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews, interviews, and observation the facility fails as follows:
to provide respiratory care as per physician...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records review and interview the facility failed to provide an individualized or person-centered care plan for a reside...
Read full inspector narrative →
Aug 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to follow policy procedures, failed to assess wounds time...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to review the risks and benefits of bed rails, failed to ...
Read full inspector narrative →
Jul 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews the facility failed as follows: failed to follow preventive measures in placing intervent...
Read full inspector narrative →
Apr 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a resident received enteral nutrition feedings via G-tube per physician orders for one (R2) resident out of three resi...
Read full inspector narrative →
Mar 2024
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide Notice of Medicare Non-Coverage for 3 (R387, R388, and R389) out of three residents reviewed for skilled nursing facility advance b...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and records review, the facility failed to provide proper medication by failing to administer medication as ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review the facility failed to get consent for psychotropic medication before starting to administ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews the facility failed to implement education and ensure that its visitor demonstrates proper use of transmission-based precautions to prevent the sp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and records review, the facility failed to administer/offer the pneumococcal vaccine to two (R30, R42) of fi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations, interviews and records review, the facility failed to label and store medications according to their policy for ten residents (R44, R49, R93, R98, R105, R110, R118, R158, R337, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected multiple residents
Based on observations, interviews and records review, the facility failed to perform refrigerator checks for four residents (R14, R54, R92, R336) in a sample of 36 according to facility policy.
Findin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure bedtime snacks were offered to two of five residents (R158, R97) reviewed for bedtime snacks in the sample of 36.
Findings include:...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record reviews, the facility failed the following practices related to the kitchen: failed to follow the policy on maintaining a clean kitchen environment; faile...
Read full inspector narrative →
Jan 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure that two (R1, R2) residents remain free from ab...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected multiple residents
Based on observations, interviews and record review the facility failed to provide reasonable access to the use of a telephone to five (R7, R8, R9, R10, R11) residents reviewed for phone access. This ...
Read full inspector narrative →
Dec 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, the facility failed to properly reconcile medication for a resident to the physician or ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record reviews and interviews the facility failed to provide accurate progress notes, created new notes by separating single notes with different dates and putting additional notes after disc...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to follow their policy to reposition a dependent resident in a timely manner to prevent worsening of a pressure ulcer for 1 (R20)...
Read full inspector narrative →
Sept 2023
9 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review the facility failed to ensure that staff knocks before entering the room of o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to ensure the call device is within reach for 1 (R12) resident reviewed for call device in a total sample of 23 residents.
F...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to notify a family representative of a change in condition which affected one (R13) resident reviewed for policy and procedure in a total samp...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure that 1 resident was given scheduled medication. This defici...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the Low Air Loss Mattress was not set to Static Mode and failed to ensure the Low Air Loss Mattress was layered per fa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0691
(Tag F0691)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to prevent a colostomy bag from overflowing and spilling...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review the facility failed to ensure that one resident's (R8) humidifier bottle had...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure resident's allergies and intolerance were recorded on the resident electronic health record. This failure affected 1 (R3) resident r...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R14 is [AGE] year old with diagnosis including but not limited to: Hypertension, Lack of Coordination, Obesity, Paraplegia and N...
Read full inspector narrative →
Aug 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to supervise one cognitively impaired resident (R2) who i...
Read full inspector narrative →
Aug 2023
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on record review and interview the facility failed to implement appropriate care plan interventions to prevent serious injury for one of five residents (R5) reviewed for injury of unknown origin...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide incontinence care for two resident R20 and R22 in a timely manner. This failure affected 2 out of 2 residents (R20, R2...
Read full inspector narrative →
Apr 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide residents who depend on staff assistance for their ADL (Activities of Daily Living) care and grooming receive skin ca...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow physician orders to hold gastrostomy(G-Tube) feedings for a resident that was scheduled for a surgical procedure. This failure affec...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement fall interventions for one (R1) of three re...
Read full inspector narrative →
Jan 2023
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to provide privacy to one of 58 residents (R124) in the sample.
Findings include:
On 1/23/23 at 10:50am, V43 (Caregiver) was at R1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to provide a means of communication to two of 58 residents (R48, R205) in the sample.
Findings include:
1. On 1/23/23 at 9:50am, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to follow physician orders for monitoring and recording of indwelling catheter output for two residents (R127 and R135) out of 5 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow their policy for administering medications via...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to have a five percent (5%) or lower medication error rat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. On 1/23/23 at 10:10 am during room rounds, R117 was observed sitting in a chair at the bedside. R117's call light was observe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
4. On 01/23/23 at 11:33 AM, surveyor observed R9 with white facial hair approximately a quarter-inch long creating a goatee appearance on R9's face. The surveyor inquired if R9 would like to be shaved...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
5. On 01/23/2023 at 10:10am, R405 was lying on a LALM. The setting of R405's LALM was at 550lbs. Surveyor inquired about R405's weight. R405 stated, I weigh 260lbs.
On 01/23/2023 at 10:20am, V7 (Infec...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
2. On 01/23/23 at 10:26 AM, R110's oxygen tracheostomy collar and humidifier bottle were labeled with the date of 1/12/23. At 10:30 AM, this observation was brought to the attention of V13 (Respirator...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review the facility failed to follow proper food storage practices and label/date food to prevent food-borne illnesses; failed to maintain daily refrigerator...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to perform indwelling catheter care as ordered by the physician. This f...
Read full inspector narrative →
Dec 2022
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to follow their policy by failing to respond to a resident's call light promptly. This failure affected one resident (R12) and ha...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that medications were documented in the MAR (Medication Admi...
Read full inspector narrative →
Dec 2022
3 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to a) follow facility policy to notify the physician of ...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and review of records, the facility failed to follow It's policy ensuring prompt identification...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to provide a person-centered care plan for 2 of 2 resi...
Read full inspector narrative →
Nov 2022
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record review, the facility failed to prevent, assess, provide timely care, and update resi...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 10 harm violation(s), $237,213 in fines, Payment denial on record. Review inspection reports carefully.
- • 73 deficiencies on record, including 10 serious (caused harm) violations. Ask about corrective actions taken.
- • $237,213 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Warren Barr South Loop's CMS Rating?
CMS assigns WARREN BARR SOUTH LOOP an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Warren Barr South Loop Staffed?
CMS rates WARREN BARR SOUTH LOOP's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 62%, which is 16 percentage points above the Illinois average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 67%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Warren Barr South Loop?
State health inspectors documented 73 deficiencies at WARREN BARR SOUTH LOOP during 2022 to 2025. These included: 10 that caused actual resident harm and 63 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Warren Barr South Loop?
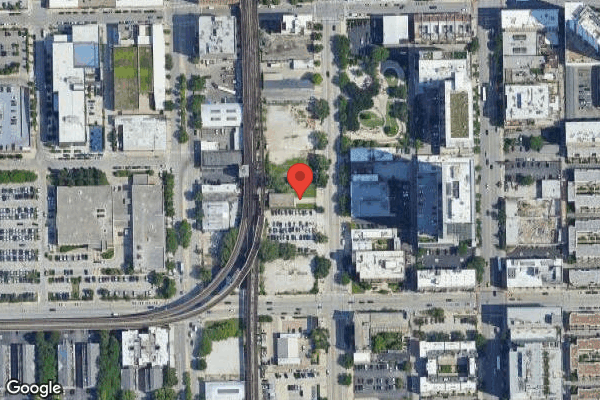
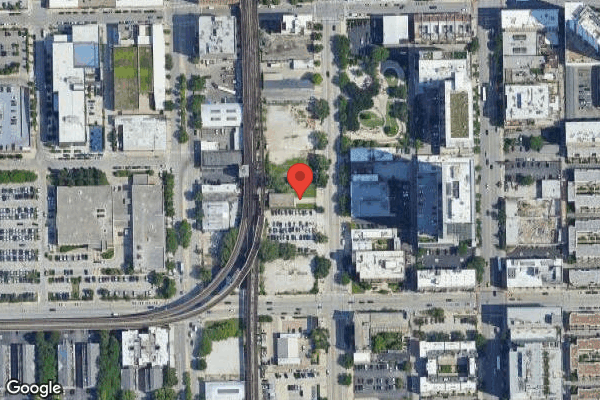
WARREN BARR SOUTH LOOP is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by LEGACY HEALTHCARE, a chain that manages multiple nursing homes. With 210 certified beds and approximately 189 residents (about 90% occupancy), it is a large facility located in CHICAGO, Illinois.
How Does Warren Barr South Loop Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, WARREN BARR SOUTH LOOP's overall rating (1 stars) is below the state average of 2.5, staff turnover (62%) is significantly higher than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Warren Barr South Loop?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is Warren Barr South Loop Safe?
Based on CMS inspection data, WARREN BARR SOUTH LOOP has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Warren Barr South Loop Stick Around?
Staff turnover at WARREN BARR SOUTH LOOP is high. At 62%, the facility is 16 percentage points above the Illinois average of 46%. Registered Nurse turnover is particularly concerning at 67%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Warren Barr South Loop Ever Fined?
WARREN BARR SOUTH LOOP has been fined $237,213 across 5 penalty actions. This is 6.7x the Illinois average of $35,451. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Warren Barr South Loop on Any Federal Watch List?
WARREN BARR SOUTH LOOP is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.