ALIYA OF HOMEWOOD



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Aliya of Homewood currently holds a Trust Grade of F, indicating significant concerns about the quality of care provided. With a state rank of #98 out of 665 facilities in Illinois, they are in the top half, but that ranking does not mitigate the serious issues reported. The facility is improving, having reduced its number of issues from 8 in 2024 to just 2 in 2025, but it still has a long way to go. Staffing is a noted weakness with a rating of 2 out of 5 stars and a turnover rate of 38%, which is below the Illinois average but still concerning. Specific incidents highlight serious lapses in care, such as a resident suffering an undetermined injury and another falling off the bed during a transfer, resulting in hospitalization for a head injury. While the facility has some positive aspects, including good quality measures and a majority of non-critical issues, the overall picture remains troubling for prospective families.
- Trust Score
- F
- In Illinois
- #98/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 38% turnover. Near Illinois's 48% average. Typical for the industry.
- Penalties ✓ Good
- $64,180 in fines. Lower than most Illinois facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 50 minutes of Registered Nurse (RN) attention daily — more than average for Illinois. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 31 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (38%)
10 points below Illinois average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Near Illinois avg (46%)
Typical for the industry
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 31 deficiencies on record
Jul 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on interviews and record review, the facility failed to prevent an injury of unknown origin which occurred for one resident. This affected one of three residents (R1) reviewed for injury of unkn...
Read full inspector narrative →
May 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to monitor a resident (R2) sitting on the side of the bed when prepari...
Read full inspector narrative →
Nov 2024
2 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure the antibiotic prescribed include duration, care plan, and documentation of long term used. This deficiency has the pot...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to implement ongoing monitoring of antibiotics. This defi...
Read full inspector narrative →
Aug 2024
4 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** B. On 7/25/24 at 3:13PM V10 (Nurse) said, R3 was wheelchair bound, very weak and could not articulate well. V10 said, V13 (CNA) ...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R8 admitted in the facility on [DATE] under hospice care and expired in the facility on [DATE].
R8 has diagnoses of Metabolic En...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to notify their physician of an acute change in condition as noted in their change in condition policy. This failure affected one of three res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their internal refund process policy by not providing a refu...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow their policy to ensure housekeeping staff inspected the privacy curtains in resident rooms and removed visibly soiled ...
Read full inspector narrative →
Mar 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to have effective fall interventions in place for a resident assessed ...
Read full inspector narrative →
Dec 2023
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents were able to engage in the Activity ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** On 12/11/23 at 10:55AM, R28 was observed to be in bed in their room. R28 said I have expressed concern to the staff that I am al...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected most or all residents
Based on observation, interviews, and record reviews, the facility failed to follow manufacturer's guidelines for dating a multidose vial when opened. This deficiency has the potential to affect all 1...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
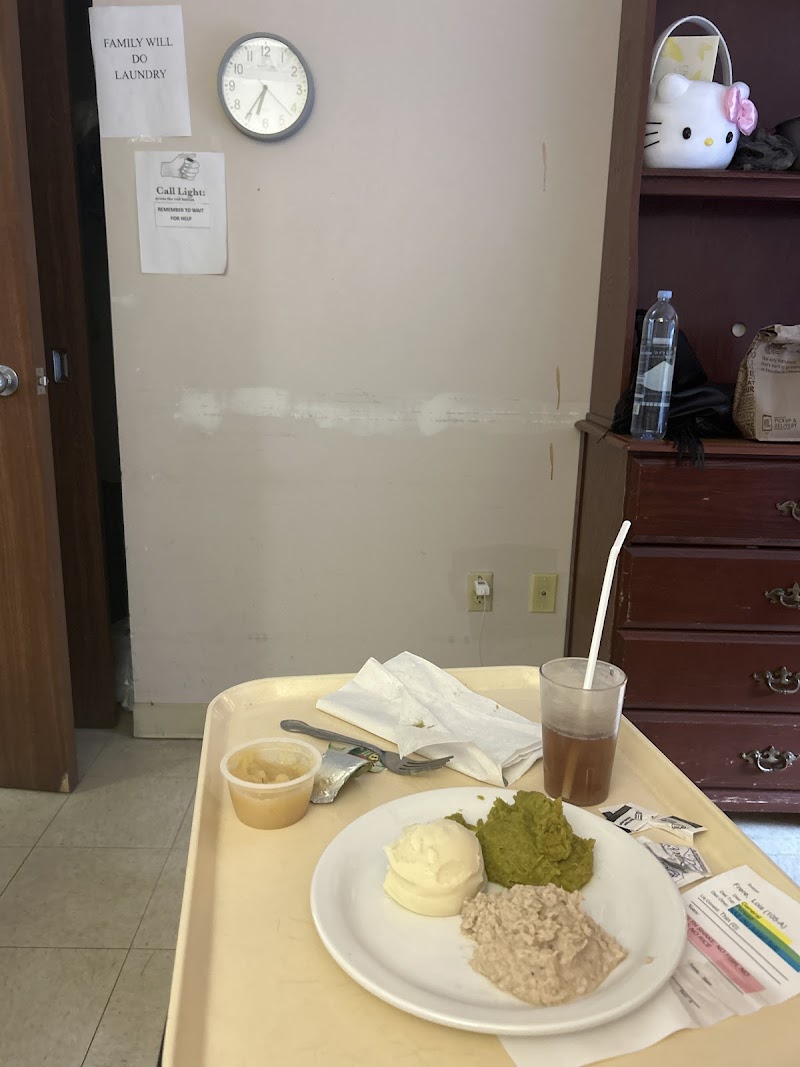
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to follow their menu and failed to provide appropriate and approved menu changes and substitutions. This failure has the potenti...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to follow their policies on food service sanitation and storage by not taking temperatures prior to the start of meal service; f...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
B. 12/11/23 12:35 PM, observed medication administration with V5 (LPN) who was administering insulin to R39. V5 finished administering insulin to resident, removed her gloves and disposed it in a garb...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to follow its fall prevention and management policy and accurately assess a resident's fall risk and implement high fall risk interventions ...
Read full inspector narrative →
Mar 2023
4 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R5 was admitted with Vascular Dementia, Metabolic Encephalopathy, Hypertension and a history of falls. Brief interview for menta...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
Based on interview and record review, the facility failed to effectively monitor and ensure adequate hydration was provided to prevent dehydration. This affected 2 of 3 (R5 and R1) residents reviewed ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to follow their skin assessment policy by not identifying and providing a treatment/dressing of a draining arterial wound to the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on interview and record review, facility failed to provide a clean dressing after an episode of incontinence care for a stage 3 pressure ulcer. This affected 1 of 3 (R1) residents reviewed for w...
Read full inspector narrative →
Dec 2022
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop a plan to prevent or reduce the risk of falling for a high ...
Read full inspector narrative →
Nov 2022
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and records reviewed the facility failed to follow and implement their abuse policy to ensure that employees...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and records reviewed the facility failed to follow their policy to by allowing the accused staff member to c...
Read full inspector narrative →
Sept 2022
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews the facility failed to follow their policy and procedures for providing se...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews the facility failed to follow their policy and procedures for providing se...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide ADL (Activities of Daily Living) care by fail...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R54 is a [AGE] year-old woman who was originally admitted to the facility January 13, 2020, for primary concerns related to adva...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to have a five percent (5%) or lower medication error rate. There were nine medication errors out of 30 observed opportunities, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to date opened insulin; failed to dispose of narcotic me...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R42 was originally admitted to the facility on [DATE] with multiple diagnoses including but not limited to the following: dyspha...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 38% turnover. Below Illinois's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 8 harm violation(s), $64,180 in fines. Review inspection reports carefully.
- • 31 deficiencies on record, including 8 serious (caused harm) violations. Ask about corrective actions taken.
- • $64,180 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (20/100). Below average facility with significant concerns.
About This Facility
What is Aliya Of Homewood's CMS Rating?
CMS assigns ALIYA OF HOMEWOOD an overall rating of 4 out of 5 stars, which is considered above average nationally. Within Illinois, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Aliya Of Homewood Staffed?
CMS rates ALIYA OF HOMEWOOD's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 38%, compared to the Illinois average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Aliya Of Homewood?
State health inspectors documented 31 deficiencies at ALIYA OF HOMEWOOD during 2022 to 2025. These included: 8 that caused actual resident harm and 23 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Aliya Of Homewood?
ALIYA OF HOMEWOOD is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by ALIYA HEALTHCARE, a chain that manages multiple nursing homes. With 132 certified beds and approximately 103 residents (about 78% occupancy), it is a mid-sized facility located in HOMEWOOD, Illinois.
How Does Aliya Of Homewood Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, ALIYA OF HOMEWOOD's overall rating (4 stars) is above the state average of 2.5, staff turnover (38%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Aliya Of Homewood?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Aliya Of Homewood Safe?
Based on CMS inspection data, ALIYA OF HOMEWOOD has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 4-star overall rating and ranks #1 of 100 nursing homes in Illinois. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Aliya Of Homewood Stick Around?
ALIYA OF HOMEWOOD has a staff turnover rate of 38%, which is about average for Illinois nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Aliya Of Homewood Ever Fined?
ALIYA OF HOMEWOOD has been fined $64,180 across 2 penalty actions. This is above the Illinois average of $33,721. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Aliya Of Homewood on Any Federal Watch List?
ALIYA OF HOMEWOOD is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.