BELLA TERRA LAGRANGE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Bella Terra LaGrange has a Trust Grade of C, which means it is average and sits in the middle of the pack for nursing homes. It ranks #224 out of 665 facilities in Illinois, placing it in the top half, and #70 out of 201 in Cook County, indicating only one local option is better. The facility's trend is stable, with 11 issues reported in both 2024 and 2025. Staffing is a relative strength, with a 3/5 star rating and a turnover rate of 39%, which is better than the state average of 46%. However, the facility has $18,005 in fines, which is concerning as it suggests some compliance problems. While the nursing home provides more RN coverage than 79% of Illinois facilities, there have been serious incidents, such as a resident experiencing sexual abuse by another resident, indicating significant safety concerns. Furthermore, the facility failed to offer staff the COVID-19 vaccine or document it properly, and it did not notify residents or their families about the reasons for hospital transfers, which raises issues about communication and resident rights. Overall, families should weigh these strengths and weaknesses carefully when considering this facility.
- Trust Score
- C
- In Illinois
- #224/665
- Safety Record
- Moderate
- Inspections
- Holding Steady
- Staff Stability ○ Average
- 39% turnover. Near Illinois's 48% average. Typical for the industry.
- Penalties ✓ Good
- $18,005 in fines. Lower than most Illinois facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 59 minutes of Registered Nurse (RN) attention daily — more than average for Illinois. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 30 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (39%)
9 points below Illinois average of 48%
Facility shows strength in fire safety.
The Bad
Near Illinois average (2.5)
Meets federal standards, typical of most facilities
Near Illinois avg (46%)
Typical for the industry
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 30 deficiencies on record
Mar 2025
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, the facility failed to ensure residents were treated with dignity while providing care.
This applies to 2 of 2 residents (R3 and R47) reviewed fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide the resident and/or their representative of the facility be...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
2. On 03/25/25 at 11:12 AM R14's nails were long, jagged, and with a brown substance under the nails. R14 said that her nails bothered her, and she wanted the staff to provide nail care for her.
R14'...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow physician's orders and subsequently a colonoscopy had to be ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. R46's 10/30/24 SBAR showed that on 10/30/24 R46's was transferred to the hospital and the form showed under Bed hold policy, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to conduct required care plan meetings and invite residents to partici...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure a resident's IV (intravenous) antibiotic therapy bag was labeled.
This applies to 1 of 1 resident (R81) reviewed for ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
9. On 03/25/25 10:22 AM, during initial tour, surveyor went to R81's room. R81 was lying in bed. There was a mediation cup with 5 chewable tablets of Tums on her bedside table. R81 stated, This is my ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
6. On 3/26/25 at 8:30 AM, soiled linen and a used resident gown were seen on the floor in R72's room.
On 3/26/25 at 8:35 AM, V10 (LPN-Licensed Practical Nurse) stated R72 was discharged the previous ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to offer staff the Covid-19 immunization vaccine and have written documentation of it.
This applies to all 97 residents in the facility revie...
Read full inspector narrative →
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to send a resident to the hospital emergency department via 911 after ...
Read full inspector narrative →
Jun 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to maintain resident room air temperatures at a comfortab...
Read full inspector narrative →
Apr 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents' call lights were within their reach...
Read full inspector narrative →
Feb 2024
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility also failed to ensure medication was not left at a resident's bedside for self-administration without a self-administration assessment ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure that one resident's ace wraps to his legs were applied according to doctor's order.
This applies to 1 of 20 residents...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the indwelling urinary catheter tube was secured to the resident to prevent potential tugging or pulling.
This applie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to check placement and flush a gastrostomy tube prior to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to administer medications as ordered. There were 25 oppo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide personal privacy during provisions of Activities of Daily (ADL) care.
This applies to 4 of 6 residents (R40, R11, R22...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to assist residents identified as needing assistance wit...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow their policy for Enhanced Barrier Precautions....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents were offered pneumococcal vaccination in accordanc...
Read full inspector narrative →
Apr 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident received medications as ordered by the physician....
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide care and services by not following physician ...
Read full inspector narrative →
Mar 2023
5 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure that expired medications are removed from use.
This applies to 1 of 5 residents (R55) reviewed for insulin storage, l...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to apply splint/rolled towel and heel protectors to prevent further decrease in range of motion.
This applies to 2 of 2 resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to monitor and maintain PICC (Peripherally Inserted Cent...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow physician orders for pain management and assessment. This ap...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. R49's face sheet documents diagnoses including cerebral infarction, attention-deficit hyperactivity disorder, paranoid person...
Read full inspector narrative →
Jan 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to protect a resident's right to be from sexual abuse by another resid...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 39% turnover. Below Illinois's 48% average. Good staff retention means consistent care.
- • 30 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $18,005 in fines. Above average for Illinois. Some compliance problems on record.
- • Grade C (53/100). Below average facility with significant concerns.
About This Facility
What is Bella Terra Lagrange's CMS Rating?
CMS assigns BELLA TERRA LAGRANGE an overall rating of 3 out of 5 stars, which is considered average nationally. Within Illinois, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Bella Terra Lagrange Staffed?
CMS rates BELLA TERRA LAGRANGE's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 39%, compared to the Illinois average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Bella Terra Lagrange?
State health inspectors documented 30 deficiencies at BELLA TERRA LAGRANGE during 2023 to 2025. These included: 1 that caused actual resident harm and 29 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Bella Terra Lagrange?
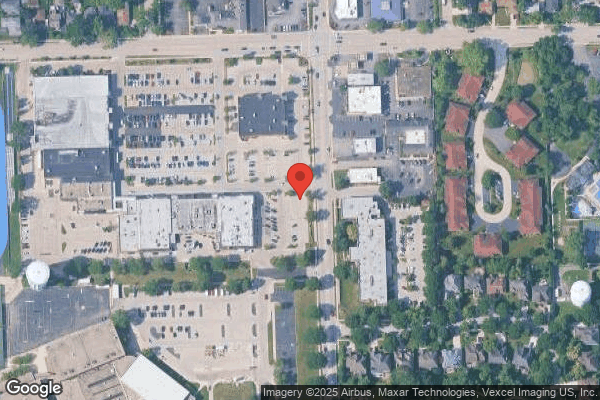
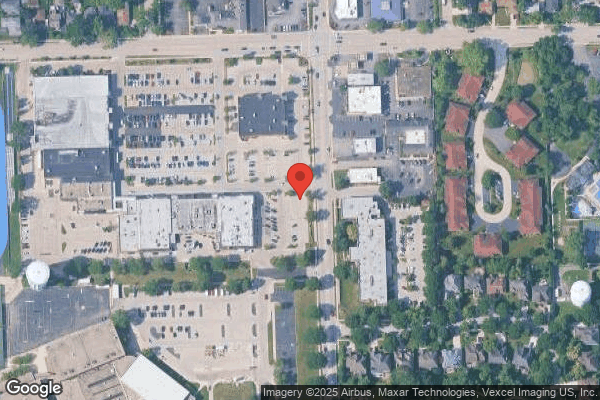
BELLA TERRA LAGRANGE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by LEGACY HEALTHCARE, a chain that manages multiple nursing homes. With 120 certified beds and approximately 97 residents (about 81% occupancy), it is a mid-sized facility located in LA GRANGE, Illinois.
How Does Bella Terra Lagrange Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, BELLA TERRA LAGRANGE's overall rating (3 stars) is above the state average of 2.5, staff turnover (39%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Bella Terra Lagrange?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Bella Terra Lagrange Safe?
Based on CMS inspection data, BELLA TERRA LAGRANGE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Illinois. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Bella Terra Lagrange Stick Around?
BELLA TERRA LAGRANGE has a staff turnover rate of 39%, which is about average for Illinois nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Bella Terra Lagrange Ever Fined?
BELLA TERRA LAGRANGE has been fined $18,005 across 1 penalty action. This is below the Illinois average of $33,259. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Bella Terra Lagrange on Any Federal Watch List?
BELLA TERRA LAGRANGE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.