SMITH CROSSING




Inspected within the last 6 months. Data reflects current conditions.
Smith Crossing, located in Orland Park, Illinois, has a Trust Grade of F, indicating significant concerns about the care provided. With a state rank of #183 out of 665, they are in the top half of Illinois facilities, but their overall performance raises serious red flags. The facility is worsening, with the number of issues increasing from 9 in 2024 to 14 in 2025. Staffing is a strength, earning 5 out of 5 stars, though the turnover rate is 55%, which is average. However, there have been concerning incidents, such as residents suffering fractures due to improper transfer assistance and a failure to prevent the development of serious pressure ulcers, indicating potential risks to resident safety. While there is good RN coverage, the facility's overall trustworthiness is significantly undermined by these recent findings.
- Trust Score
- F
- In Illinois
- #183/665
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 55% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ⚠ Watch
- $95,193 in fines. Higher than 86% of Illinois facilities, suggesting repeated compliance issues.
- Skilled Nurses ✓ Good
- Each resident gets 86 minutes of Registered Nurse (RN) attention daily — more than 97% of Illinois nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 32 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Staffing Rating · Excellent nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, fire safety.
The Bad
Near Illinois avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Moderate penalties - review what triggered them
7 points above Illinois average of 48%
The Ugly 32 deficiencies on record
Jun 2025
10 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to prevent the development of an unstageable pressure ul...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide a dignified dining experience.
This applies to 1 resident (R26) reviewed for dignity in a sample of 21.
The findings...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident's medical records were in agreement with his wish...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide a safe and homelike environment.
This applies to 2 of 2 residents (R2, R22) reviewed for environment in a sample of 2...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide ADL (Activities of Daily Living) care to meet the needs of the residents.
This applies to 3 of 3 residents (R54, R59...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide peri-care in a manner that would prevent urinary tract infection, and failed to ensure that urinary catheter drainage...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to obtain orders for gastrostomy tube (g-tube) flushes.
This applies to 2 of 2 residents (R64, R70) reviewed for gastrostomy tu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure that medications were administered as prescribed by the physician. There were 26 medication opportunities with 5 error...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. R13's progress notes show the following:
On 12/30/24 at 9:14 PM at 6 PM, (R13) observed supine on floor near window. Limb sh...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
4. On 6/16/25, at 9:30 AM, R330 was resting on her bed and just had a bowel movement on the bed pan. V22 (CNA) provided peri-care with the assistance of V21 (Nurse). V22 cleaned R330's back perineum, ...
Read full inspector narrative →
May 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their policy to document complete assessments of pressure ul...
Read full inspector narrative →
Apr 2025
3 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure that a cognitively impaired resident received treatment and...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility failed to implement effective fall interventions to minimize t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to recognize an injury of unknown origin as a suspected allegation of abuse and failed to report an allegation of abuse to the administrator....
Read full inspector narrative →
Jun 2024
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to assess whether a resident was able to administer medications independently.
This applies to 1 of 1 resident (R419) reviewed f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide the facility's bed hold and bed payment policy in writing t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide wound dressing changes as per physician's orde...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On June 25, 2024 at 11:18 AM, V6 (CNA) assisted to transfer R418 from the wheelchair to the bed. V6 faced R418's wheelchair a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a resident received oxygen therapy consistent with how the device was designed to deliver it per physician orders.
Th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews the facility failed to provide privacy during personal cares.
This applie...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to appropriately store medications and biologicals sa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to post and follow isolation precautions for residents u...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure the kitchen staff performed hand hygiene before handling clean dishes, and failed to ensure staff contained their hair...
Read full inspector narrative →
Aug 2023
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to prevent, identify, and manage a residents facility ac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to ensure the correct placement of a gastrostomy tube before administering medication and fluids through it.
This applies to 1 of 1 (R58) reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide Peripherally Inserted Central Catheter (PICC) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview the facility failed to ensure that oxygen was delivered to a resident at the rate prescribed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to serve pureed diet with the consistency as per policy guidance. This applies to 2 of 2 residents (R224 and R225) reviewed for p...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to label and date medications after it was opened to determine expiration dates. This applies to 4 of 6 residents (R15, R57, R58,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to follow standard infection control practices regarding hand hygiene and changing of gloves during provisions of peri-care. Thi...
Read full inspector narrative →
Aug 2023
1 deficiency
1 Harm
SERIOUS
(H)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to provide safe transfer assistance. This applies to 5 of ...
Read full inspector narrative →
Nov 2022
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident's bed alarm was enabled for a resident who was at high risk for falls.
This applies to 1 of 3 residents (R1) reviewed fo...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 4 harm violation(s), $95,193 in fines, Payment denial on record. Review inspection reports carefully.
- • 32 deficiencies on record, including 4 serious (caused harm) violations. Ask about corrective actions taken.
- • $95,193 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (35/100). Below average facility with significant concerns.
About This Facility
What is Smith Crossing's CMS Rating?
CMS assigns SMITH CROSSING an overall rating of 4 out of 5 stars, which is considered above average nationally. Within Illinois, this rating places the facility higher than 99% of the state's 100 nursing homes. This rating reflects solid performance across the metrics CMS uses to evaluate nursing home quality.
How is Smith Crossing Staffed?
CMS rates SMITH CROSSING's staffing level at 5 out of 5 stars, which is much above average compared to other nursing homes. Staff turnover is 55%, which is 9 percentage points above the Illinois average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at Smith Crossing?
State health inspectors documented 32 deficiencies at SMITH CROSSING during 2022 to 2025. These included: 4 that caused actual resident harm and 28 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
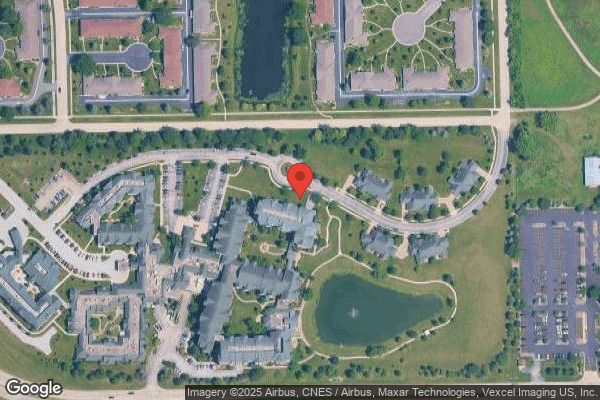
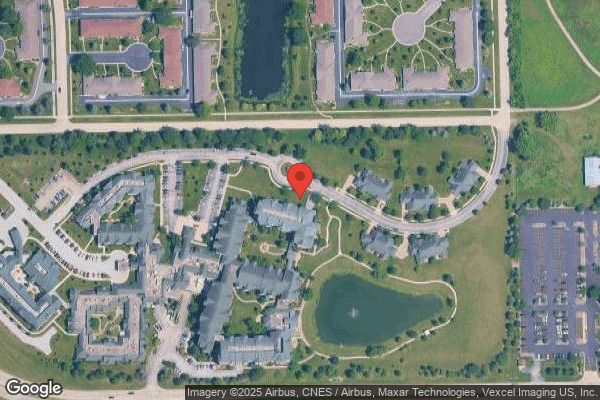
Who Owns and Operates Smith Crossing?
SMITH CROSSING is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 92 certified beds and approximately 77 residents (about 84% occupancy), it is a smaller facility located in ORLAND PARK, Illinois.
How Does Smith Crossing Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, SMITH CROSSING's overall rating (4 stars) is above the state average of 2.5, staff turnover (55%) is near the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Smith Crossing?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's high staff turnover rate.
Is Smith Crossing Safe?
Based on CMS inspection data, SMITH CROSSING has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 4-star overall rating and ranks #1 of 100 nursing homes in Illinois. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Smith Crossing Stick Around?
Staff turnover at SMITH CROSSING is high. At 55%, the facility is 9 percentage points above the Illinois average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Smith Crossing Ever Fined?
SMITH CROSSING has been fined $95,193 across 1 penalty action. This is above the Illinois average of $34,031. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Smith Crossing on Any Federal Watch List?
SMITH CROSSING is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.