ACCOLADE HEALTHCARE OF SAVOY




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Accolade Healthcare of Savoy has a Trust Grade of F, indicating significant concerns about the quality of care provided. The facility ranks #422 out of 665 in Illinois, placing it in the bottom half of nursing homes in the state, and #3 out of 4 in Champaign County, meaning there is only one local option performing worse. While the facility is trending towards improvement with a reduction in issues from 24 in 2024 to 15 in 2025, it still faces serious challenges, including critical incidents of resident-to-resident abuse and inadequate supervision of residents, which raise major red flags. Staffing is rated 2 out of 5 stars, which is below average, and has a turnover rate of 46%, matching the state average, suggesting potential instability among caregivers. Additionally, the facility has incurred $179,055 in fines, which is concerning, and while RN coverage is average, it is essential to note that there have been serious failures in ensuring resident safety and managing behaviors that could lead to harm.
- Trust Score
- F
- In Illinois
- #422/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 46% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $179,055 in fines. Lower than most Illinois facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 32 minutes of Registered Nurse (RN) attention daily — about average for Illinois. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 109 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
Near Illinois avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 109 deficiencies on record
Sept 2025
6 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to monitor and report changes in condition, including monitoring and re...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to use foot pedals during wheelchair transportation for tw...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on Interview, Observation and Record Review the facility failed to notify the physician and power of attorney for an incident of elopement for one (R7) of three residents reviewed for elopement ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to transcribe physician's orders for one of four residents (R3) reviewed for accidents in the sample list of nine. On 8/27/25 at 9:30 AM, R3 wa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to administer medications as ordered resulting in significant medication errors for one of five residents (R2) reviewed for changes in conditio...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to ensure medical records are complete and accurate for four of seven residents (R1, R2, R3, R7) reviewed for changes in condition and elopemen...
Read full inspector narrative →
Aug 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to protect a resident's right to privacy. This failure affects one resident (R1) of three reviewed for privacy in the sample of ...
Read full inspector narrative →
Jul 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to report a resident fall to the licensed nurse, directly resulting in a lack notification of the residents physician and family...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility staff failed to report a resident fall to the licensed nurse, directly resulting in a lack of a licensed nurse completing a nursing ass...
Read full inspector narrative →
May 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to protect a resident right to be free from verbal abuse (R3) by anoth...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to report an injury of an unknown origin to the state survey agency for...
Read full inspector narrative →
May 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to implement Enhanced Barrier Precautions (EBP) for one (...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to timely report post fall pain and implement radiology orders timely, ...
Read full inspector narrative →
Feb 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to provide bathing, oral care, and toileting for three (R1...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to identify, assess, make the appropriate notifications, obtain treatments and interventions for three pressure wounds for one (R1...
Read full inspector narrative →
Dec 2024
2 deficiencies
2 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. R89's Facility Census dated 12/5/24 documents R89 has the following medical diagnoses: Acute on Chronic Systolic (Congestive)...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0698
(Tag F0698)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** -
Based on an interview and record review, the facility failed to communicate regularly with the dialysis center to coordinate c...
Read full inspector narrative →
Oct 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** --
Based on record review and interview, the facility failed to notify a resident's family representative of positive laboratory...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility repeatedly failed to maintain complete and accurate resident medical record, by failing to document the application of a physician ordered back brac...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility repeatedly failed to implement fall interventions for R1, R2...
Read full inspector narrative →
Oct 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to provide pain management by not having the correct pain medication av...
Read full inspector narrative →
Sept 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on the interview and record review, the facility failed to properly transfer one of two residents (R1) reviewed for periph...
Read full inspector narrative →
Sept 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to report an allegation of mental abuse to the state agency in the 2 hour required timeframe. This failure affects one resident (R1) out of tw...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to maintain residents' dignity by failing to answer call lights and respond to requests for assistance in a timely manner. This failure affect...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, the facility failed to maintain flooring in resident bathrooms in a clean, safe, and homelik...
Read full inspector narrative →
Jul 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on record review and interviews the facility failed to protect two residents from misappropriation of property by facility staff. This failure caused R1 to have 11 transactions totaling $1515.96...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to protect the residents' right to be free from misappropriation of property by failing to follow the facility's Abuse Prevention Program by st...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure fall interventions were in place, safely positi...
Read full inspector narrative →
May 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to ensure a resident right to dignified care and treatment. This failur...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to protect a residents' right to be free from verbal/ment...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to ensure an allegation of physical and verbal abuse by R2 towards R1, was reported to the Administrator/Abuse Prevention Coordinator. This fai...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure two staff were assisting during a mechanical lift transfer fo...
Read full inspector narrative →
Mar 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed notify the physician of a resident refusal of catheterization for one (R1) of three residents reviewed for physician notification on the sample...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to administer narcotic medications safely to one (R1) of three residents reviewed for narcotic administration on the sample list of three.
Find...
Read full inspector narrative →
Feb 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to revise and update a resident's (R1) Plan of Care to include Gastrostomy Residual Volume checks before each enteral feeding. R1 is one of th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to have physician orders in place regarding Gastrostomy Residual Volum...
Read full inspector narrative →
Jan 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to thoroughly investigate an injury of unknown origin for one of four residents (R6) reviewed for injuries in the sample list of 33.
Findings ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0659
(Tag F0659)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to administer medications in accordance with physician's orders for two...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to implement its policies to accurately record and account for controlled medications for 28 of 28 residents (R1, R2, R3, R9-R33)...
Read full inspector narrative →
Nov 2023
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to provide Advance Beneficiary Notices (ABN) to three of three residents (R264, R146, and R6) reviewed for Beneficiary Protection Notifications...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to provide nail care to one of 31 residents (R56) reviewed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to have fall prevention interventions in place on admission for one of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to perform hand hygiene before or after administering medications and obtaining a blood glucose level for five (R52, R119, R64, R4...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4.) R63's Medication Administration Record dated 10/1/23 to 10/31/23 documents an order dated 10/04/23 for Hydroxyzine (antihist...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to dispose of undated insulin for seven (R104, R51, R68, R1, R134, R119, R64) of seven residents reviewed for medication storage f...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to complete performance reviews to identify training needs and provide training for CNAs (Certified Nursing Assistants). This failure has the p...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected most or all residents
Based on interview, and record review the facility failed to ensure all Certified Nurse's Aide's (CNA) received twelve hours of annual training including required subjects. This failure has the potent...
Read full inspector narrative →
Sept 2023
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to prevent the worsening of a resident's facility acquired...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure the dignity of residents. This failure affects t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure a resident (R2) who had previously been placed on continual m...
Read full inspector narrative →
Sept 2023
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to notify a resident's Family Member and provide a written Notice of Tr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure pressure ulcer risk assessments, wound assessme...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to complete pressure ulcer risk assessments for (R3), mon...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed repeatedly to ensure gastrostomy tube (G-tube) feeding vo...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to maintain resident bedroom, bathroom and shower room call lights in operable condition on the second floor of the facility. This...
Read full inspector narrative →
Jun 2023
13 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to supervise a resident (R1) with a known history of wand...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
Based on observation, interview and record review, the facility failed to update resident plans of care for pressure ulcers, failed to document measurements/assessments of pressure ulcers, and failed ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to obtain informed consent from the resident's representative prior to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide advance and written notification of a room change and reason for the room change for one resident (R3). R1 and R3 are ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to report allegations of sexual abuse to law enforcement for three of f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to implement interventions to prevent further sexual abus...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0659
(Tag F0659)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident was scheduled for and/or was taken to physician o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement hospital physician's orders for Diabetic Foot Care. The facility also failed to document completion of treatments to a resident's...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident attended a podiatrist appointment as ordered. This failure affects one of three residents (R4) reviewed for physician's v...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to implement behavior monitoring, develop/implement nonpharmacological ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to have a policy to determine a resident's ability or capacity to conse...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to employ a full-time Director of Nursing. This failure affects all 143 residents residing in the facility.
Findings include:
The facility's F...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Social Worker
(Tag F0850)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to have a qualified social worker on staff. This failure has the potent...
Read full inspector narrative →
Apr 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide foot care for two (R2, R3) of four residents r...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to maintain safe food temperature and storage to prevent ...
Read full inspector narrative →
Apr 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide feeding assistance to residents according to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to implement measures to help prevent the development of infections according to facility policy. This failure affects one resid...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure a current copy of a resident's advance directive was in the r...
Read full inspector narrative →
Mar 2023
2 deficiencies
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to follow the Centers for Disease Control and Local Health Department r...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to ensure that all employees were tested twice weekly during a Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) outbreak. This fail...
Read full inspector narrative →
Sept 2022
34 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** B.) Based on interview and record review the facility failed to prevent a resident-to-resident altercation for two (R89, R95) of...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to timely identify and address significant weight loss, c...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
Based on observation, interview and record review the facility failed to provide residents with pain control and pain assessments. The facility also failed to provide timely treatment of pain for a re...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0919
(Tag F0919)
A resident was harmed · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure the emergency nurse call system had a functioning light for R214 and a properly functioning emergency nurse call device...
Read full inspector narrative →
SERIOUS
(H)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0740
(Tag F0740)
A resident was harmed · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to comprehensively assess a resident's aggressive behaviors upon admiss...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure medications were consumed during medication administration for one of one resident (R215) reviewed for self-administrat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to notify the resident's physician and family of significant weight los...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure a Preadmission Screening and Resident Review (PASARR) level I...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to develop an initial baseline care plan for one of 24 residents (R74) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide assistance with showers, nail care, shaving an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) R17's undated diagnosis list documents the following diagnoses including Neuromuscular Dysfunction of Bladder, Generalized An...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to implement physician's orders for a urinary catheter, f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a resident had physician's orders for use of a Continuous Positive Airway Pressure (CPAP) device. The facility also fai...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0696
(Tag F0696)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident received orders for care of/maintenance for a resident's artificial eyes. This failure affects one of one resident (R101)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to complete psychological medication assessments, complete Abnormal Inv...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) R80's undated diagnosis sheet documents the following diagnoses including Metabolic Encephalopathy, Catatonic Schizophrenia, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to offer COVID-19 (Human Coronavirus Infection) immunizations for three...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to promote residents' dignity by failing to ensure residents were served meals at the same time, ensure staff did not stand over ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to keep residents' emergency nurse call light devices with...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2.) The facility's abuse allegation investigative files from March 2022-August 2022 were reviewed. The only documented abuse all...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. R70's Minimum Data Set (MDS) dated [DATE] documents R13 has severe cognitive impairment, is not on a prescribed weight loss r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. R13's Minimum Data Set (MDS) dated [DATE] documents R13 has severe cognitive impairment, R13 is not on a prescribed weight lo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4.) R372's Orthopedic after care notes document a post operative appointment on 5/18/22. The post operative visit notes dated 5/...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to provide meals that met dietary needs and preferences for four (R14, R215, R106, and R214) of 24 residents reviewed for meals o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to prepare and serve meat that was easily cut and chewed for five (R214, R113, R67, R70, and R13) of 24 residents reviewed for me...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to disinfect scissors after a wound treatment, change gloves, perform hand hygiene during incontinence care, implement isolation ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to address/provide response for concerns voiced during resident council meetings. These failures have the potential to affect all 122 resident...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review the facility failed to provide a full time Director of Nursing (DON) since January 1, 2022. These failures have the potential to affect all 122 reside...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to maintain sanitary food preparation and storage areas. These failures have the potential to affect all 122 residents in the fa...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0837
(Tag F0837)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to designate and operationalize an effective governing body, impacting ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to implement a quality assurance program within the facility. This failure has the potential to affect all 122 residents residing in the facili...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to hold quarterly quality meetings. This failure has the potential to affect all 122 residents residing in the facility.
Findings include:
On 9...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to include the Director of Nursing in quality assurance meetings. This failure has the potential to affect all 122 residents residing in the fa...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0888
(Tag F0888)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to ensure a licensed nurse was vaccinated for COVID-19. This failure has the potential to affect all 122 residents residing in th...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 2 life-threatening violation(s), 11 harm violation(s), $179,055 in fines, Payment denial on record. Review inspection reports carefully.
- • 109 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $179,055 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
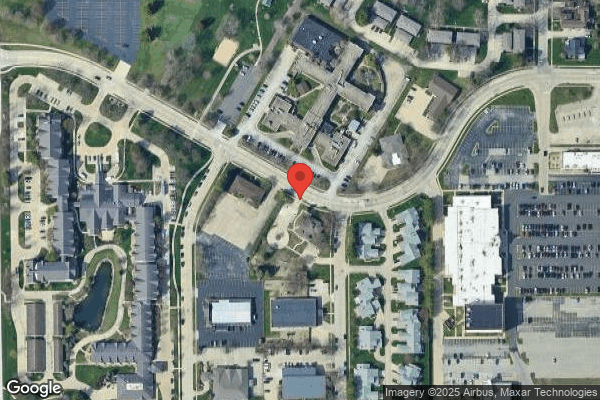
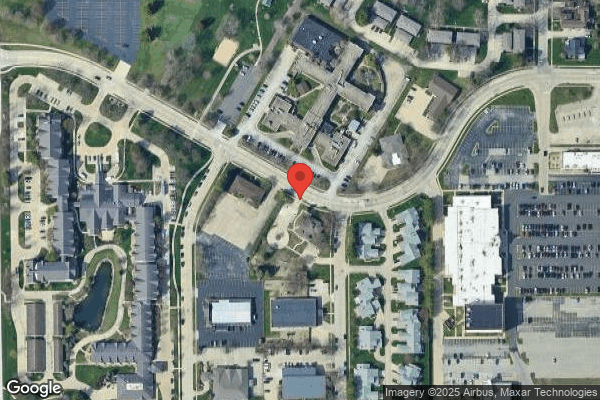
About This Facility
What is Accolade Healthcare Of Savoy's CMS Rating?
CMS assigns ACCOLADE HEALTHCARE OF SAVOY an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Accolade Healthcare Of Savoy Staffed?
CMS rates ACCOLADE HEALTHCARE OF SAVOY's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 46%, compared to the Illinois average of 46%.
What Have Inspectors Found at Accolade Healthcare Of Savoy?
State health inspectors documented 109 deficiencies at ACCOLADE HEALTHCARE OF SAVOY during 2022 to 2025. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 11 that caused actual resident harm, and 96 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Accolade Healthcare Of Savoy?
ACCOLADE HEALTHCARE OF SAVOY is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by ACCOLADE HEALTHCARE, a chain that manages multiple nursing homes. With 213 certified beds and approximately 178 residents (about 84% occupancy), it is a large facility located in SAVOY, Illinois.
How Does Accolade Healthcare Of Savoy Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, ACCOLADE HEALTHCARE OF SAVOY's overall rating (1 stars) is below the state average of 2.5, staff turnover (46%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Accolade Healthcare Of Savoy?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the substantiated abuse finding on record, and the below-average staffing rating.
Is Accolade Healthcare Of Savoy Safe?
Based on CMS inspection data, ACCOLADE HEALTHCARE OF SAVOY has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Accolade Healthcare Of Savoy Stick Around?
ACCOLADE HEALTHCARE OF SAVOY has a staff turnover rate of 46%, which is about average for Illinois nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Accolade Healthcare Of Savoy Ever Fined?
ACCOLADE HEALTHCARE OF SAVOY has been fined $179,055 across 5 penalty actions. This is 5.1x the Illinois average of $34,869. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Accolade Healthcare Of Savoy on Any Federal Watch List?
ACCOLADE HEALTHCARE OF SAVOY is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.