BRIA OF CHICAGO HEIGHTS



Inspected within the last 6 months. Data reflects current conditions.
Bria of Chicago Heights has received a Trust Grade of F, indicating poor quality and significant concerns with care. They rank #470 out of 665 facilities in Illinois, placing them in the bottom half, and #151 of 201 in Cook County, suggesting limited local options that are better. The facility is worsening, with issues increasing from 8 in 2024 to 13 in 2025. Staffing is a strength, with a turnover rate of 38%, which is better than the state average, but the overall staffing rating is poor at 1 out of 5 stars. However, the facility has faced serious incidents, including a resident leaving through a window without staff knowledge, raising serious safety concerns, and another resident suffering injuries of unknown origin, including bruising and swelling, which were not adequately addressed. There have also been reports of physical altercations between residents, highlighting issues with supervision and resident management. While there are some strengths in staffing retention, the serious safety violations and overall poor grades suggest families should carefully consider their options.
- Trust Score
- F
- In Illinois
- #470/665
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 38% turnover. Near Illinois's 48% average. Typical for the industry.
- Penalties ○ Average
- $22,084 in fines. Higher than 63% of Illinois facilities. Some compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 28 minutes of Registered Nurse (RN) attention daily — below average for Illinois. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 30 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (38%)
10 points below Illinois average of 48%
Facility shows strength in fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
Near Illinois avg (46%)
Typical for the industry
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 30 deficiencies on record
Jun 2025
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on interviews and record reviews, the facility failed to prevent a resident injury, and failed to determine the origin of the injury. This affected one of three residents (R1) reviewed for injur...
Read full inspector narrative →
May 2025
12 deficiencies
2 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on interview and record review the facility failed to prevent a resident to resident physical assault. This affected two of four (R48, R70) residents reviewed for physical abuse. This failure re...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R94 was admitted to the facility on [DATE] with a diagnosis of major depressive disorder, anxiety and conversion disorder with s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to follow their abuse policy and investigate an injury of unknown origin. This affected two of four residents (R48, R70) both reviewed for abus...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to follow the abuse policy and procedures and immediately report an injury of unknown origin. This affected two of four residents (R48, R70) re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, facility staff failed to accurately code a Minimum Data Set (MDS) for two of three reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to refer one resident who was later identified with serious mental ill...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interviews and records reviewed the facility failed to review and revise the resident's wound care interventions. This affected one of three residents (R42) reviewed for care plan review and ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to follow its medication regimen review policy to ensure the outside pharmacist identified and reported the absence or inadequate indication...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow their transmission-based isolation policy by not relocating ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to have an effective pest control policy/program, by not ensuring the facility was free of pest to include (rodents and flying insects). This a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on interviews and record reviews the facility failed to administer the influenza vaccine during influenza season, failed to screen residents for and offer the pneumococcal vaccine to residents. ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0565
(Tag F0565)
Minor procedural issue · This affected most or all residents
Based on interview and record review the facility failed to ensure that the assigned staff, thoroughly assisted and documented the resident concerns and grievances during the monthly resident council ...
Read full inspector narrative →
Jul 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to adequately monitor and supervise a newly admitted res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews the facility failed to follow their policy and procedures for protecting residents from a...
Read full inspector narrative →
May 2024
2 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and records reviews the facility failed to prevent a cognitively impaired resident who requires supervision ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record reviews, and observations the facility failed to have an effective pest control program to ensure th...
Read full inspector narrative →
Apr 2024
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to follow their hypoglycemia protocol by not administering glucagon to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow R44's Fall care plan by not placing the call light within reach. This failure affected 1 resident (R44) of 2 reviewed ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0577
(Tag F0577)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to have the State inspection survey results readily available and accessible to residents, family members and legal representativ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to label multi-dose medication for one of two medication...
Read full inspector narrative →
Oct 2023
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to maintain a clean, comfortable, and homelike environment in resident rooms and bathrooms. This failure applied to nine of 22 r...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to maintain air conditioners in resident rooms by not cleaning the filters prior to them becoming caked with dust and debris. This failure appli...
Read full inspector narrative →
Jan 2023
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to evaluate and modify the falls care plan of one resident (R73) out o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to maintain medication errors below 5% for one resident (R20) of four residents reviewed for medication review in the sample of 2...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to discard an inhaler more than thirty days after the opened date; and, the facility failed to discard single dose vials of medic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to follow Enhanced Barrier Precautions for one resident (R53) of one resident reviewed for gastric tube administration in the sam...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a resident's call light was accessible and functioning for 1 of 1 resident (R48) reviewed for call lights in a total sa...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to follow their policy and wear face masks properly in the kitchen and while preparing food. The facility also failed to wear fac...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observation, interview and record review, the facility failed to post the nursing staffing in a prominent place readily available to residents and visitors. This deficiency could potentially ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 38% turnover. Below Illinois's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: Federal abuse finding, 1 life-threatening violation(s), 4 harm violation(s). Review inspection reports carefully.
- • 30 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $22,084 in fines. Higher than 94% of Illinois facilities, suggesting repeated compliance issues.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Bria Of Chicago Heights's CMS Rating?
CMS assigns BRIA OF CHICAGO HEIGHTS an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Bria Of Chicago Heights Staffed?
CMS rates BRIA OF CHICAGO HEIGHTS's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 38%, compared to the Illinois average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Bria Of Chicago Heights?
State health inspectors documented 30 deficiencies at BRIA OF CHICAGO HEIGHTS during 2023 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 4 that caused actual resident harm, 23 with potential for harm, and 2 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
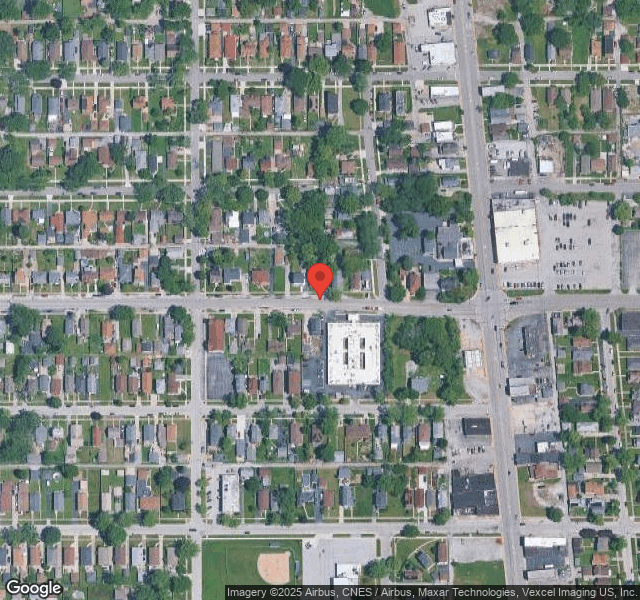
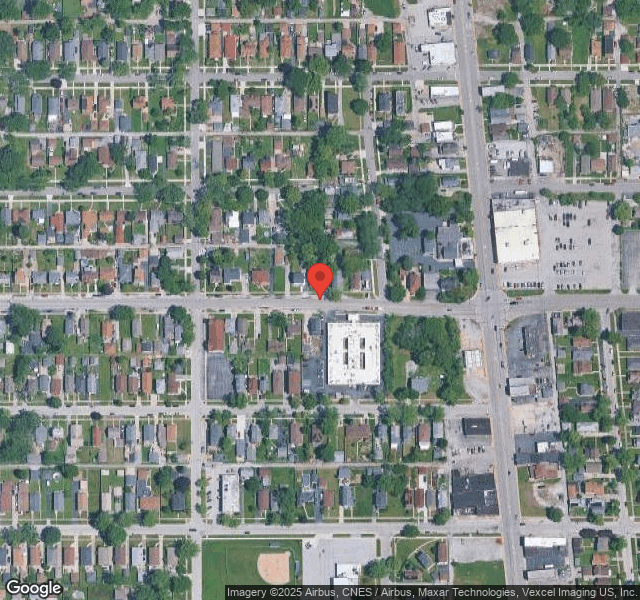
Who Owns and Operates Bria Of Chicago Heights?
BRIA OF CHICAGO HEIGHTS is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by BRIA HEALTH SERVICES, a chain that manages multiple nursing homes. With 112 certified beds and approximately 96 residents (about 86% occupancy), it is a mid-sized facility located in SOUTH CHICAGO HEIGHT, Illinois.
How Does Bria Of Chicago Heights Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, BRIA OF CHICAGO HEIGHTS's overall rating (1 stars) is below the state average of 2.5, staff turnover (38%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Bria Of Chicago Heights?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the substantiated abuse finding on record, and the below-average staffing rating.
Is Bria Of Chicago Heights Safe?
Based on CMS inspection data, BRIA OF CHICAGO HEIGHTS has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Bria Of Chicago Heights Stick Around?
BRIA OF CHICAGO HEIGHTS has a staff turnover rate of 38%, which is about average for Illinois nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Bria Of Chicago Heights Ever Fined?
BRIA OF CHICAGO HEIGHTS has been fined $22,084 across 2 penalty actions. This is below the Illinois average of $33,300. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Bria Of Chicago Heights on Any Federal Watch List?
BRIA OF CHICAGO HEIGHTS is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.