TAYLORVILLE CARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Taylorville Care Center has received a Trust Grade of F, indicating significant concerns regarding the quality of care provided. It ranks #645 out of 665 nursing homes in Illinois, placing it in the bottom half of facilities in the state, and is the lowest-ranked facility in Christian County. While the facility shows signs of improvement, having reduced issues from 22 in 2024 to 7 in 2025, the overall situation remains troubling, with 55 serious deficiencies noted, including two critical incidents where residents were unsupervised and left the facility. Staffing is a major concern, with only 1 out of 5 stars and a RN coverage level lower than 95% of Illinois facilities, meaning they may not have enough registered nurses to catch issues that other staff might miss. Additionally, the facility has incurred $216,034 in fines, which is higher than 89% of Illinois nursing homes, suggesting ongoing compliance problems. Specific incidents include a resident leaving the facility unsupervised and being found by police, and another resident suffering a fractured arm due to improper use of bed rails, highlighting significant safety risks.
- Trust Score
- F
- In Illinois
- #645/665
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 50% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $216,034 in fines. Lower than most Illinois facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 14 minutes of Registered Nurse (RN) attention daily — below average for Illinois. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 55 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
Near Illinois avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 55 deficiencies on record
Aug 2025
3 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on interview, observation, and record review, the Facility failed to provide residents with palatable and safe temperature meals for 8 of 8 residents (R4, R20, R24, R27, R28, R43, R45, R46) revi...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the Facility failed to employ a Director of Food and Nutrition. This has the potential to affect all 67 residents living in the Facility. Findings in...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the Facility failed to ensure foods were stored and prepared in a manner that prevents foodborne illness. This has the potential to affect all 67 res...
Read full inspector narrative →
May 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to promote dignity and to treat residents in a respectful manner during...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to report an allegation of verbal and physical abuse to the State Agency for 1 (R2) of 3 residents reviewed for abuse in the sample of 10.
Fin...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to operationalize their policy to conduct an investigation of allegatio...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to report injury of unknown origin for one of four (R2) residents, rev...
Read full inspector narrative →
Jun 2024
11 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, observation and record review, the Facility failed to prevent, identify, obtain orders and monitor pressure ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. R14's Braden Score for predicting Pressure Sore Risk, dated 5/9/2024, documents that R14 is constantly moist, chairfast, and ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to prevent verbal abuse for 1 of 17 residents (R51) reviewed for abuse...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the Facility failed to ensure their Abuse Prevention Policy was followed/implemented for 2...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure standards of care were implemented for a resident with a dia...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, observation, and record review, the facility failed to provide timely and complete incontinent care for 2 of...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review, the Facility failed to ensure physician's orders were accurately completed and implemented for 1 of 3 residents (R50) reviewed for significant medication error in...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure wheelchair brakes were locked,a gait belt was u...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
4. On 06/04/24 at 08:16 AM, V8, Licensed Practical Nurse (LPN) did not perform any hand hygiene prior to getting R14's medications ready to give. V8 then gave R14 her medications she went back to the ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to remove expired medication and glucose control solution from refrigerator and medication cart and date multi dose insulin pens...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to properly store and label foods with open dates, secure hair during meal preparation and service, and utilize hand hygiene to ...
Read full inspector narrative →
May 2024
11 deficiencies
2 IJ (1 facility-wide)
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0700
(Tag F0700)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to use alternatives to bed rails, and assess and monitor ...
Read full inspector narrative →
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide supervision for residents who require supervis...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Notification of Changes
(Tag F0580)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify the Physician of a change of condition and delay in diagnost...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based interview and record review, the facility failed to timely treat an injury of unknown origin for 1 of 1 resident (R6) revi...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, observation, and record review, the facility failed to assess, measure, document, obtain orders for, prevent...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide pain management for 1 of 3 residents (R6) in the sample of ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interviews, and observations the facility failed to answer call lights in a timely manner to meet reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide complete incontinence care for one of three r...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interviews and observations the facility failed to provide sufficient nursing staff to ensure resident s...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on record review, interviews, and observations the facility failed to provide the services of a Director of Nursing on a full-time basis. This failure has the potential to affect all residents r...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
Based on record review and interviews the facility failed to implement and maintain an affective Quality Assurance program. This has the potential to affect all 71 residents residing in the facility. ...
Read full inspector narrative →
Jul 2023
7 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on interview and record review, the Facility failed to provide an Advanced Beneficiary Notice of Non-Coverage (ABN) to residents being discharged from Medicare part A with benefit days remaining...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide residents privacy during transferring and wound care for 2 of 4 residents (R27 and R42) reviewed for privacy in a samp...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the Facility failed to follow physician's orders for the treatment of pressur...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the Facility failed to ensure residents have water available for hydration pu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to perform appropriate hand hygiene while passing out and setting up meal trays for residents and providing care to prevent the s...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on record review and interview, the facility failed to provide a registered nurse (RN) for at least 8 consecutive hours a day, 7 days a week on the dates. This has the potential to affect all th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the Facility failed to ensure mediations that require refrigeration were monitored for the correct/current temperature for storage as well as ensure ...
Read full inspector narrative →
Jun 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident is free from employee-to-resident verbal abuse fo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to immediately report an allegation of abuse and injury ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to investigate an allegation of employee to resident physical abuse and injury of unknown origin and failed to remove an alleged ...
Read full inspector narrative →
Mar 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to implement fall interventions and provide supervision t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide sufficient nursing staff to address resident's...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to wear required Personal Protective Equipment (PPE) and perform hand hygiene to prevent the spread of COVID-19 for 2 of 7 reside...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to provide a Registered Nurse (RN) 8 hours a day 7 days a week. This has the potential to affect all 59 residents living in the f...
Read full inspector narrative →
Mar 2023
6 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
Based on interview, observation, and record review the facility failed to have sufficient activities on the evening shift, and weekend for 7 of 10 residents (R1, R2, R3, R4, R5, R6, R9) reviewed for a...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
Based on interview, observation, and record review the facility failed to provide sufficient nursing staff to provide for the needs of the residents. This has the potential to affect all 59 residents ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review the facility failed to provide a Registered Nurse (RN) for at least 8 consecutive hours a day 7 days a week. This failure has the potential to affect ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review the facility failed to have a qualified cook with skill sets to carry out food and nutrition services and serve the correct amounts to each resident. ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected most or all residents
Based on interview, observation and record review the Facility failed to follow the monthly scheduled Menu and failed to provide nutritional bedtime snacks. This has the potential to affect all 59 res...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected most or all residents
Based on interviews, observations, and record review the facility failed to serve a nourishing bedtime snack. This failure has the potential to affect all 59 residents residing at the facility.
Findin...
Read full inspector narrative →
Jan 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review, the Facility failed to follow their policy regarding re-ordering of medications to ensure medications were available for administration per Physician's Orders for...
Read full inspector narrative →
May 2022
5 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. R11's May 2022 Physician Order Sheet (POS) documents R11 has a diagnosis of pain in left hip, orthostatic hypotension, repeat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to discard insulin within an appropriate timeframe after opening to maintain the integrity of the insulin for 3 of 12 residents (...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to implement an Antibiotic Stewardship Program to ensure the appropriate use of antibiotics for 4 of 4 residents (R1, R7, R8 and R19) reviewed...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the Facility failed to store food in accordance with professional standards for food service safety. This has the potential to affect all 63 residen...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on interview, observation, and record review the facility failed to require staff to wear the proper PPE (personal protective equipment) and follow the guidelines of the county's transmission ra...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 2 life-threatening violation(s), 6 harm violation(s), $216,034 in fines. Review inspection reports carefully.
- • 55 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $216,034 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Taylorville's CMS Rating?
CMS assigns TAYLORVILLE CARE CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Taylorville Staffed?
CMS rates TAYLORVILLE CARE CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 50%, compared to the Illinois average of 46%.
What Have Inspectors Found at Taylorville?
State health inspectors documented 55 deficiencies at TAYLORVILLE CARE CENTER during 2022 to 2025. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 6 that caused actual resident harm, and 47 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Taylorville?
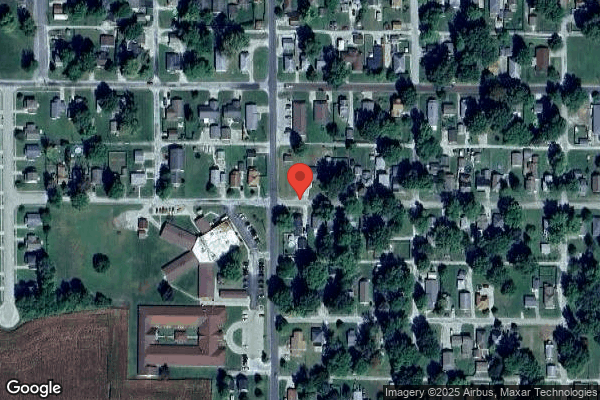
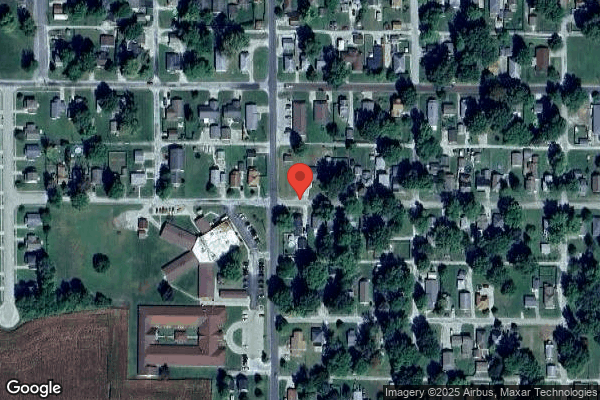
TAYLORVILLE CARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PALLADIAN HEALTHCARE, a chain that manages multiple nursing homes. With 98 certified beds and approximately 66 residents (about 67% occupancy), it is a smaller facility located in TAYLORVILLE, Illinois.
How Does Taylorville Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, TAYLORVILLE CARE CENTER's overall rating (1 stars) is below the state average of 2.5, staff turnover (50%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Taylorville?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Taylorville Safe?
Based on CMS inspection data, TAYLORVILLE CARE CENTER has documented safety concerns. Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Taylorville Stick Around?
TAYLORVILLE CARE CENTER has a staff turnover rate of 50%, which is about average for Illinois nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Taylorville Ever Fined?
TAYLORVILLE CARE CENTER has been fined $216,034 across 3 penalty actions. This is 6.1x the Illinois average of $35,239. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Taylorville on Any Federal Watch List?
TAYLORVILLE CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.