BRICKYARD HEALTHCARE -SYCAMORE VILLAGE CARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Brickyard Healthcare - Sycamore Village Care Center has a trust grade of D, indicating below-average performance and some significant concerns. It ranks #435 out of 505 nursing homes in Indiana, placing it in the bottom half of facilities in the state, and #7 out of 7 in Howard County, meaning there is only one other local option that performs better. The facility is currently improving, with the number of issues identified decreasing from 14 in 2023 to 9 in 2024. Staffing is an average concern with a turnover rate of 50%, similar to the state average, and they have no fines on record, which is a positive aspect. However, there have been notable incidents, such as staff improperly using residents' personal funds without consent and failing to securely store controlled substances, highlighting serious issues with resident safety and financial management. Overall, while there are some strengths, families should weigh these concerns carefully when considering this facility for their loved ones.
- Trust Score
- D
- In Indiana
- #435/505
- Safety Record
- Low Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 50% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Indiana facilities.
- Skilled Nurses ○ Average
- Each resident gets 32 minutes of Registered Nurse (RN) attention daily — about average for Indiana. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 36 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Indiana average (3.1)
Significant quality concerns identified by CMS
Near Indiana avg (46%)
Higher turnover may affect care consistency
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 36 deficiencies on record
Dec 2024
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the SNF-ABN (Skilled Nursing Facility-Advanced Beneficiary Notice) forms were accurately completed for 2 of 3 residents discharged f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure Preadmission Screening and Record Review (PASARR) evaluations were updated and accurate for 2 of 4 residents reviewed for PASARR. (R...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the physician ordered parameters to hold blood pressure medications were followed for 1 of 1 resident reviewed for quality of care. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure an admission weight was obtained for 2 of 5 residents review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure policy and procedures were followed for medications administered through a gastrostomy tube (g-tube) for 1 of 1 residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a physician's order, a care plan, a signed consent, and an assessment was obtained prior to the use of side rails for 1...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure pharmaceutical services were obtained and maintained timely ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
2. During observations, on 12/12/24, 12/13/24, and 12/17/24, no enhanced barrier precautions (EBP) sign was noted outside Resident 61's room per the physician's order.
During observations, on 12/18/2...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure compromised controlled substance medications were not stored in the medication cart for 2 of 4 medication carts observe...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure staff were being supervised when a staff member physically kicked a resident in his back for 1 of 3 residents reviewed for abuse. (R...
Read full inspector narrative →
Oct 2023
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure residents were dressed in regular clothing like...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to notify the physician of a blood glucose level greater than the physician's call orders for 1 of 1 resident reviewed for notification. (Resi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to protect the residents' right to be free from verbal abuse for 1 of 1 resident reviewed for abuse. (Resident C)
Finding includes:
During an ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a comprehensive care plan was implemented to address a resident's preferences for 1 of 1 resident reviewed for dignity....
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure there was communication between the hospice company and the facility for care provided by the hospice staff for 1 of 1 resident revi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure a resident's contracted fingers/hands were asse...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide enough staff to prevent low weekend staffing reported in the third quarter to the Pay-Roll Based Journal (PBJ) staffing report and ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
2. The record for Resident J was reviewed on 9/27/23 at 4:19 p.m. Diagnoses included, but were not limited to, Alzheimer's disease, anxiety disorder, cognitive communication deficit, insomnia, anxiety...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a resident who requested dental services had the paperwork completed and was scheduled for the dentist for 1 of 2 resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
2. During an observation, on 9/26/23 at 2:38 p.m., Resident M was lying in bed with the catheter bag on the floor. The Social Service Director (SSD) went into the resident's room, hooked the catheter ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify residents' family representatives prior to staff spending th...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. During an interview, on 9/27/23 at 4:07 p.m., Resident D's family member indicated the BOM gave permission for Unit Manager 1...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure activities were offered daily for 5 of 5 reside...
Read full inspector narrative →
Aug 2022
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to contact the primary responsible party for a resident's fall for 1 of 1 residents reviewed for notification. (Resident G)
Finding includes:
...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to review and implement PASARR (preadmission screening and resident re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to clean and clip a resident's fingernails for 1 of 2 residents for activities of daily living. (Resident 10)
Finding includes:
...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to assess and document the improvement or worsening of a resident's ongoing skin condition for 1 of 3 residents reviewed for non pressure skin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure fall interventions were implemented for 1 of 4...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to review a resident's previous records and assess for side effects of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to identify significant weight loss and potential causes for the significant weight loss for 1 of 3 residents reviewed for nutri...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure physician orders for oxygen were followed for a resident in COVID-19 isolation (Resident J), and to turn on a portable...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
3. Resident 36's record was reviewed, on 08/19/22 02:54 p.m., Diagnoses included, but were not limited to, alzhiemer's disease, subarachnoid hemorrhage, dementia with behavioral disturbance, major dep...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a seizure medication and an effervescent tablet were administered correctly resulting in an 11.54% medication error ra...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure completion of routine vaccinations for 3 of 5 residents reviewed for pneumococcal vaccinations (Resident 18, 33 and 95).
Findings i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure soiled incontinence briefs were placed in trash cans and soiled laundry was removed from the room for 1 of 1 resident ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure licensed and certified staff were in the building and available to provide insulin injections for 5 of 5 residents on the ACU (Alzhe...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most Indiana facilities.
- • 36 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade D (40/100). Below average facility with significant concerns.
About This Facility
What is Brickyard Healthcare -Sycamore Village's CMS Rating?
CMS assigns BRICKYARD HEALTHCARE -SYCAMORE VILLAGE CARE CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Indiana, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Brickyard Healthcare -Sycamore Village Staffed?
CMS rates BRICKYARD HEALTHCARE -SYCAMORE VILLAGE CARE CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 50%, compared to the Indiana average of 46%.
What Have Inspectors Found at Brickyard Healthcare -Sycamore Village?
State health inspectors documented 36 deficiencies at BRICKYARD HEALTHCARE -SYCAMORE VILLAGE CARE CENTER during 2022 to 2024. These included: 36 with potential for harm.
Who Owns and Operates Brickyard Healthcare -Sycamore Village?
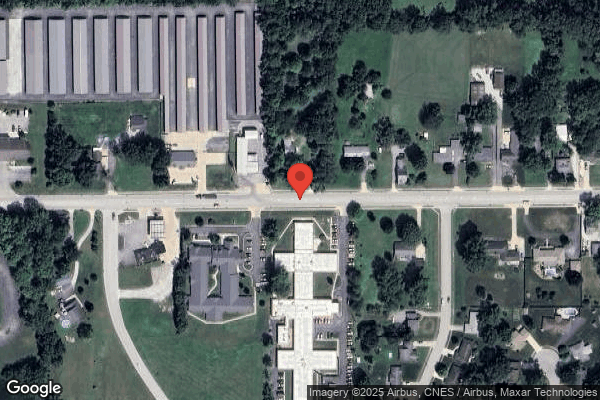
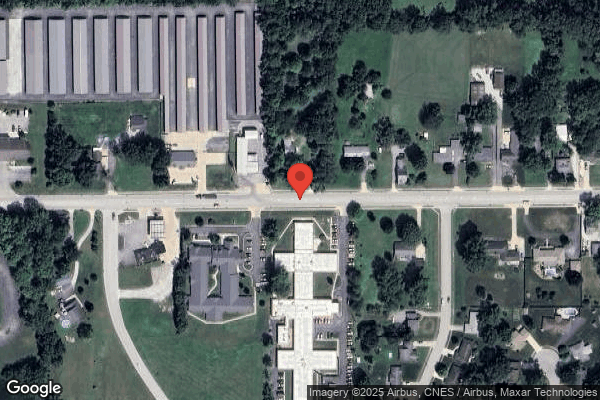
BRICKYARD HEALTHCARE -SYCAMORE VILLAGE CARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by BRICKYARD HEALTHCARE, a chain that manages multiple nursing homes. With 110 certified beds and approximately 105 residents (about 95% occupancy), it is a mid-sized facility located in KOKOMO, Indiana.
How Does Brickyard Healthcare -Sycamore Village Compare to Other Indiana Nursing Homes?
Compared to the 100 nursing homes in Indiana, BRICKYARD HEALTHCARE -SYCAMORE VILLAGE CARE CENTER's overall rating (1 stars) is below the state average of 3.1, staff turnover (50%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Brickyard Healthcare -Sycamore Village?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Brickyard Healthcare -Sycamore Village Safe?
Based on CMS inspection data, BRICKYARD HEALTHCARE -SYCAMORE VILLAGE CARE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Indiana. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Brickyard Healthcare -Sycamore Village Stick Around?
BRICKYARD HEALTHCARE -SYCAMORE VILLAGE CARE CENTER has a staff turnover rate of 50%, which is about average for Indiana nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Brickyard Healthcare -Sycamore Village Ever Fined?
BRICKYARD HEALTHCARE -SYCAMORE VILLAGE CARE CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Brickyard Healthcare -Sycamore Village on Any Federal Watch List?
BRICKYARD HEALTHCARE -SYCAMORE VILLAGE CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.