MAPLE PARK VILLAGE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Maple Park Village has received a Trust Grade of D, indicating below average care with some concerns. It ranks #268 out of 505 nursing homes in Indiana, placing it in the bottom half of facilities in the state, and #12 out of 17 in Hamilton County, meaning only five local options are worse. While the facility is improving, with the number of issues decreasing from 13 in 2023 to 6 in 2024, it still faces significant challenges with a staffing rating of 2 out of 5 stars and a high turnover rate of 59%, above the state average. On the positive side, there have been no fines recorded, and the RN coverage is average, which is crucial for catching problems that might be missed by less experienced staff. However, there are serious incidents to consider, such as a resident falling out of bed due to inadequate safety measures, resulting in a serious injury, and failures in timely medical care for residents with catheter-related complications, which led to severe health issues.
- Trust Score
- D
- In Indiana
- #268/505
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 59% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Indiana facilities.
- Skilled Nurses ○ Average
- Each resident gets 38 minutes of Registered Nurse (RN) attention daily — about average for Indiana. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 38 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near Indiana average (3.1)
Meets federal standards, typical of most facilities
13pts above Indiana avg (46%)
Frequent staff changes - ask about care continuity
Part of a multi-facility chain
Ask about local staffing decisions and management
11 points above Indiana average of 48%
The Ugly 38 deficiencies on record
Oct 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a resident with continuous feeding through a Jejunostomy tube (J-tube) received the ordered amount of nutrient formula ...
Read full inspector narrative →
Oct 2024
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to conduct care plan meetings at least quarterly for 2 of 2 residents reviewed for care plan conferences/meetings. (Resident 5 and 59)
Finding...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure medications were held according to the physician's ordered hold parameters for 2 of 2 residents reviewed for quality of care. (Resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure unlabeled food was not stored in a medication room refrigerator and medications were stored in the original containers ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure staff prepared pureed food in a sanitary manner for 1 of 1 staff member observed to puree food. (Cook 6)
Finding inclu...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a narcotic pain patch was administered at the correct time and new sites were used for the transdermal patch administra...
Read full inspector narrative →
Oct 2023
10 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure the Minimum Data Set (MDS) assessment included the resident had a wanderguard for 1 of 1 resident reviewed for elopemen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a resident with a wanderguard (an alarm bracelet) had a physician's order, daily assessment for placement and a care pl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to identify and implement resident specific preventative nursing measures for a resident with multiple repeat urinary tract infections (UTI) f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to identify significant weight changes, implement timely interventions, and notify the provider and family in a timely manner for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure residents oxygen tubing was dated and replaced for 2 of 3 residents reviewed for respiratory care. (Residents 38 and 76...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure symptom monitoring was in place for the use of an antipsychotic medication prescribed and a gradual dose reduction (GDR) was conside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to label medications with an open date on medications with a shortened expiration date once opened in 1 of 2 medication storage r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a catheter bag was not touching the ground for 1 of 1 resident reviewed for infection control related to catheters. (Re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure residents received non-disposable utensils to eat their meals with for 17 of 17 residents reviewed for dining on the lo...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to give medications within the prescribed time for 6 of 6 residents reviewed for quality of care. (Residents B, C, D, E, F, G)
Findings includ...
Read full inspector narrative →
Sept 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on interview and record review, the facility failed to protect a resident from injury when the resident was left unattended in a bed which was not in the lowest position, and without a fall mat ...
Read full inspector narrative →
Mar 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the prescribed medications ordered by a Physician were acquired from the facility pharmacy in a timely manner for 1 of 3 residents r...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure medications were accurately and completely documented on the Electronic Medication Administration Record (EMAR) for 3 of 3 residents...
Read full inspector narrative →
Dec 2022
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure their skin management program was followed for notification to the physician and the resident representative in a timel...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the Long Term Care Incident Reporting Policy wa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure a plan of care with interventions to prevent a resident from potentially being burnt in the future while receiving hot ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure their skin management program was followed rega...
Read full inspector narrative →
Nov 2022
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure appropriate assistive devices were used to prevent a fall for 1 of 3 residents reviewed for accidents. (Resident C)
Finding includes...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to keep accurate fluid intake records for 1 of 1 resident reviewed for a fluid restriction. (Resident C)
Finding includes:
The record for Resi...
Read full inspector narrative →
Oct 2022
13 deficiencies
2 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Incontinence Care
(Tag F0690)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure a resident received treatment and care in accor...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Respiratory Care
(Tag F0695)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to thoroughly assess and document a resident's change in ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
2. During an observation, on 10/04/22 at 12:20 p.m., CNA 23 was standing to feed Resident 31 her lunch in the 200 hall dining room.
During an interview, on 10/04/22 at 12:29 p.m., CNA 23 indicated the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure the IDT (Interdisciplinary Team)determined which medications may be self-administered and failed to ensure a physician'...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure residents had current comprehensive person-centered care plans for enhanced barrier precautions (Residents 67 and 82) a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide assistance with activities of daily living (ADL's), related to shaving and nail care, for 1 of 1 resident reviewed for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to assess, monitor and implement interventions to prevent pressure ulcers from developing for 1 of 1 resident reviewed for pressu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure staff followed fall interventions for 2 of 2 residents reviewed for falls and sustained injuries. (Resident 290 and 293...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure the head of bed (HOB) was properly elevated during an infusion of a Gastrostomy tube (GT) feeding and the syringe and t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure a medication error rate was less than 5%, by ma...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure insulin, an antibiotic tablet, and 2 of 2 medic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide a safe, clean, and comfortable interior environment for 1 of 1 resident room. (Resident 293)
Findings include:
During...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure drinking cups were free of lime build up, to ensure meals served to residents were covered and protected during transpo...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Indiana facilities.
- • Multiple safety concerns identified: 3 harm violation(s). Review inspection reports carefully.
- • 38 deficiencies on record, including 3 serious (caused harm) violations. Ask about corrective actions taken.
- • Grade D (40/100). Below average facility with significant concerns.
- • 59% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is Maple Park Village's CMS Rating?
CMS assigns MAPLE PARK VILLAGE an overall rating of 3 out of 5 stars, which is considered average nationally. Within Indiana, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Maple Park Village Staffed?
CMS rates MAPLE PARK VILLAGE's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 59%, which is 13 percentage points above the Indiana average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at Maple Park Village?
State health inspectors documented 38 deficiencies at MAPLE PARK VILLAGE during 2022 to 2024. These included: 3 that caused actual resident harm and 35 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
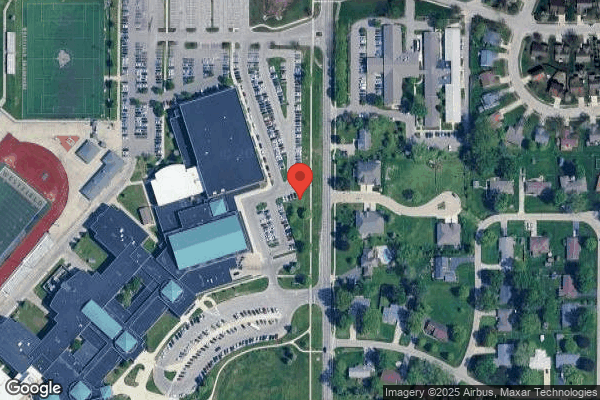
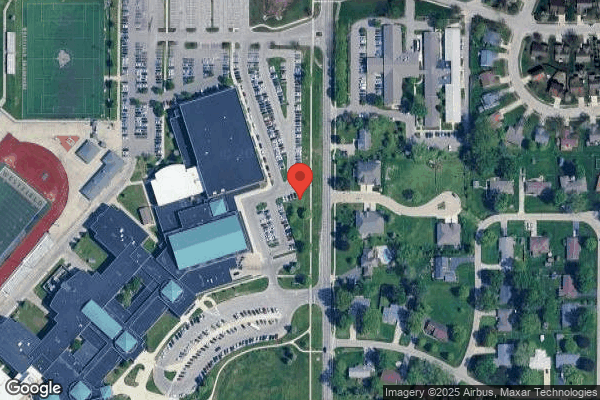
Who Owns and Operates Maple Park Village?
MAPLE PARK VILLAGE is owned by a government entity. Government-operated facilities are typically run by state, county, or municipal agencies. The facility is operated by AMERICAN SENIOR COMMUNITIES, a chain that manages multiple nursing homes. With 106 certified beds and approximately 83 residents (about 78% occupancy), it is a mid-sized facility located in WESTFIELD, Indiana.
How Does Maple Park Village Compare to Other Indiana Nursing Homes?
Compared to the 100 nursing homes in Indiana, MAPLE PARK VILLAGE's overall rating (3 stars) is below the state average of 3.1, staff turnover (59%) is significantly higher than the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Maple Park Village?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is Maple Park Village Safe?
Based on CMS inspection data, MAPLE PARK VILLAGE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Indiana. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Maple Park Village Stick Around?
Staff turnover at MAPLE PARK VILLAGE is high. At 59%, the facility is 13 percentage points above the Indiana average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Maple Park Village Ever Fined?
MAPLE PARK VILLAGE has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Maple Park Village on Any Federal Watch List?
MAPLE PARK VILLAGE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.