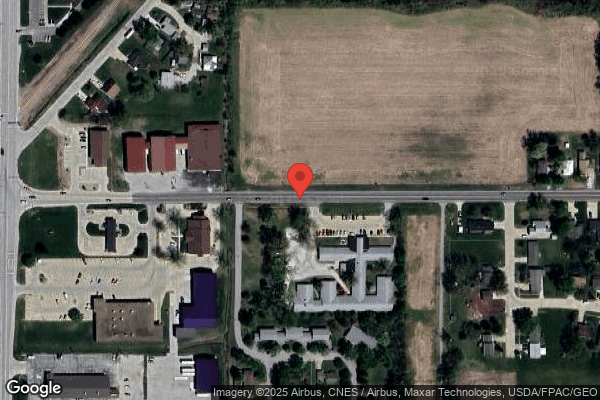
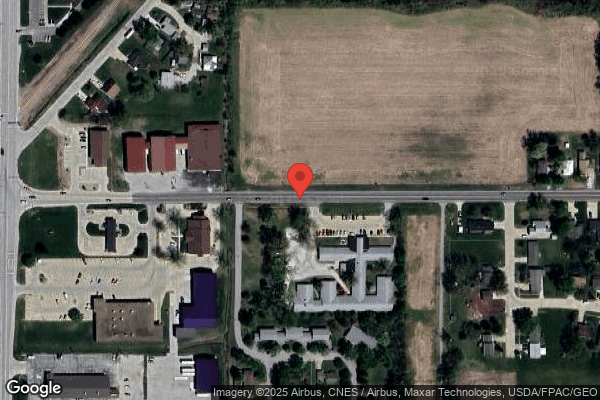
Garden View Care Center



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Garden View Care Center in Shenandoah, Iowa has received a Trust Grade of F, indicating significant concerns about the facility's overall quality and care. It does not rank among the nursing homes in Iowa or Page County, suggesting it is at the bottom of the list with no competitive alternatives nearby. While the facility's trend is improving, having decreased from 30 issues in 2024 to 26 in 2025, the overall situation remains troubling, with 77 issues found during inspections, including critical incidents of physical and verbal abuse involving staff and residents. Staffing turnover is impressively low at 0%, which is a positive sign, but the RN coverage is concerning as it falls below 92% of Iowa facilities. Additionally, the facility has accumulated $167,067 in fines, which is higher than 99% of other nursing homes in the state, indicating serious compliance issues. Families should be aware of the serious issues reflected by the inspector findings, including an incident where a resident was physically and verbally abused by a staff member, which was not reported in a timely manner, exposing residents to ongoing risk. Overall, while there are some staffing strengths, the alarming deficiencies raise significant concerns for potential residents and their families.
- Trust Score
- F
- In Iowa
- #112/223
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ⚠ Watch
- $167,067 in fines. Higher than 76% of Iowa facilities, suggesting repeated compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 24 minutes of Registered Nurse (RN) attention daily — below average for Iowa. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 77 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 77 deficiencies on record
Apr 2025
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on clinical record review, facility policy review and staff interviews the facility failed to provide a bed hold notification upon hospitalization for 1 of 3 residents (Residents #10) reviewed. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on clinical record review, facility policy review, family and staff interviews, the facility failed to provide an opportunity for a comprehensive care plan to be reviewed and revised by an inter...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record, policy review, and interview the facility failed to complete a discharge summary with a recapitulation of the r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, observations, facility policy review and staff interviews,the facility failed to apply a hand s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, Shift Change Controlled Substance Inventory Log review, facility policy review and staff interv...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility policy review and staff interviews, the facility failed to ensure a resident received ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected multiple residents
Based on personnel file review, facility policy review, and staff interviews the facility failed to complete a background check related to abuse and criminal history in a timely manner for one staff m...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of Resident #26's MDS, dated [DATE] for Resident #26 documented a BIMS of 11 indicating moderate cognitive impairment....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected multiple residents
Based on the previous Centers for Medicare and Medicaid Services (CMS) form 2567 review, staff interviews and facility policy review, the facility failed to ensure they provided a comprehensive, effec...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. A review of the Infection Control (IC) program for the facility revealed that the Infection Prevention and Control Program po...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility policy review, and staff interview the facility failed to offer residents a COVID-19 i...
Read full inspector narrative →
Feb 2025
15 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observations, record review, staff and resident interviews, and policy review the facility failed to update 2 of 7 (Resident #4 and #5) resident's care plans. The facility reported a census o...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, clinical record review, resident and staff interviews, and facility policy review the facility failed to complete treatments as ordered for 1 of 2 residents (Resident #1) with pr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on clinical record review, staff interviews and facility policy review the facility failed to ensure a gait belt was used for 1 of 14 residents (Resident #5) reviewed for falls. The facility rep...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, agency staff schedule, facility schedule, staff interviews and facility assessment the facility...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff interviews, and facility assessment review the facility failed to ensure the appropriate ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on clinical record review, staff interviews, and facility policy review the facility failed to ensure 1 of 4 residents reviewed (Resident #7) was free from unnecessary medications. The facility ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, staff interviews, and facility policy review the facility failed to appropriately store six medications after they were delivered to the facility from the pharmacy. The facility...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on clinical record review, staff interviews and facility policy review the facility failed to ensure Resident #5, #9, and #10's records were complete and accurate. Resident #5's clinical record ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff and resident interviews, and policy review the facility failed to follow physician order'...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on clinical record review, staff interviews and facility policy review the facility failed to complete a full assessment, initiate neuros, and have a licensed nurse assess Resident #5 after she ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on, facility nursing schedule review, facility staffing sheets, management call in logs, facility's Payroll Based Journal (PBJ), staff interviews and facility assessment review the facility fail...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observations and staff interviews the facility failed to ensure the nurse staffing information was posted to include accurate required information and updated daily for residents and visitors...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected multiple residents
Based on observations, staff interviews, clinical record review, and facility assessment review the decisions in administering the facility contributed to deficient practice. The facility reported a c...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected multiple residents
Based on previous CMS-2567 review, staff interview, and facility policy review the facility failed to ensure a comprehensive, effective Quality Assessment and Performance Improvement (QAPI) program. T...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, staff and resident interviews, and facility policy reviews the facility failed to ensure a...
Read full inspector narrative →
Sept 2024
10 deficiencies
4 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, policy, and staff interviews, the facility failed to prevent physical and verbal abuse of R...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Report Alleged Abuse
(Tag F0609)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, policy, and staff interviews, the facility failed to report an allegation of abuse to the I...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Investigate Abuse
(Tag F0610)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility document review, staff interviews and policy review, the facility failed to separate a...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, staff interviews, and policy review the facility failed to protect residents from ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observations, resident interviews, staff interviews and policy review the facility failed to maintain a safe and comfortable environment free of possible hazards by having insufficient linens...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on clinical record review, staff interviews, and policy review the facility failed to develop, implement and follow Comprehensive Care Plans for 3 of 14 residents (#1, #2, #11) reviewed. The fac...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on clinical record review, facility document review, resident interviews, staff interviews, and policy review the facility failed to provide adequate nursing staff to assure residents safety and...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, policy review, and staff interviews the facility failed to provide appropriate inf...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected most or all residents
Based on observation, record review and staff interviews the facility failed to maintain medical records that were systematically organized and failed to safeguard the medical records from loss or des...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on facility record review, staff interviews, and facility policy review the facility failed to demonstrate evidence of sys...
Read full inspector narrative →
Jul 2024
9 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, clinical record review, hospital document review, resident and staff interviews, and facility policy revi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of the Minimum Data Set (MDS) assessment for Resident #6, dated 6/15/24 documented a Brief Interview of Mental ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on clinical record review, resident and staff interviews, and policy review the facility failed to provide ongoing assessment and oversight for residents before and after dialysis for 2 of 2 res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Record review of the MDS assessment for Resident #6, dated 6/15/24 documented a BIMS score of 15/15 indicating normal cogniti...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, clinical record review and policy review the facility failed to offer influenza immunization to 1 of 5...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff interviews, and policy review the facility failed to revise and update the Comprehensive ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, staff interview, and policy review the facility failed to prepare, serve and distribute food by failing to provide hand hygiene and glove use according to professional standards....
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident interviews, staff interviews, facility document review and clinical record review the facility fa...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on staff interviews, facility record review and policy review, the facility failed to provide Registered Nurse (RN) coverage for 8 consecutive hours each day. The facility reported a census of 4...
Read full inspector narrative →
Apr 2024
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on facility investigative file review, staff interviews and policy review the facility failed to report a reportable event in a timely manner for 1 of 3 residents (Resident #6) reviewed for repo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff interview, hospital staff interview and policy review the facility failed to allow a resi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
Based on clinical record review, staff interviews and policy review the facility failed to complete a recapitulation of stay for 2 of 3 residents (Resident #4 & #5) reviewed. The facility reported a c...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on clinical record review, staff interviews and facility policy review the facility failed to complete discharge assessments when 3 of 3 residents (Resident #2, #4, and #4) discharged from the f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff interview, hospital staff interview, and policy review the facility failed to have comple...
Read full inspector narrative →
Feb 2024
6 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review, resident and staff interviews, and policy review the facility failed to develop a comprehensive Care Plan for 1 of 6 residents reviewed (Resident #6). The facility reported a c...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observations, record review, staff and resident interviews, and grievance forms review the facility failed to provide bathing opportunities for 3 of 3 residents reviewed (Residents #4, #5, an...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on record review, staff and resident interviews, and facility policy review the facility failed to carry out restorative programs for 2 of 2 residents reviewed (Resident #4 and #5). The facility...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, resident and staff interviews, resident council minutes, and facility assessment, the facility failed to ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on the staff roster, daily schedules, monthly schedule, payroll-based journal (PBJ), facility assessment, and staff interviews, the facility failed to have a Registered Nurse (RN) for eight cons...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observations and staff interview the facility failed to ensure the nurse staffing information was posted to include the required information and in an accessible area for residents and visito...
Read full inspector narrative →
Aug 2023
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility policy review, staff, and resident interviews the facility failed to have a nurse asse...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff interviews, and hospital staff interviews the facility failed to ensure 1 of 3 residents ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff interviews and facility policy review the facility failed to report a reportable event for 1 of 3 ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and staff interviews the facility failed to maintain a safe and sanitary environment. The facility reporte...
Read full inspector narrative →
Apr 2023
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to honor resident dignity and serve residents seated together during dining at the same time for one supplemental resident of si...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of 16 sampled residents (Resident (R) 5) h...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interview, and facility policy review, the facility failed to report an injury of unknown origin to loca...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review, and policy review, the facility failed to revise care plans for two of 16 sampled residents (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to document discharge planning and create a discharge care plan for on...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review, and review of facility policy, for one of sixteen sampled residents (Resident (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide care and services for managing contractures f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, record review, interviews, and review of manufacturer's instructions for use, the facility failed to ensure the proper storage and labeling of insulin in one of two medication ca...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on observations, interviews, review of Resident Council Minutes, and test tray sample, the facility failed to provide food that was palatable and at an appetizing temperature for one of three te...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observation, interview, record review, and review of facility policy, the facility failed to ensure food preferences were honored for one of six residents reviewed for food (Resident (R) 5). ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, record review, and facility policy review, the facility failed to follow appropriate transmis...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
Based on interviews, and review of the job description for the Dietary Manager (DM), the facility failed to have a qualified director of food and nutrition services. This had the potential to affect 4...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure menus were followed for all residents who received food from the facility kitchen. This failure had the potential to a...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, review of the job description for the Dietary Manager (DM), review of the Nutrition Services Manual, and ...
Read full inspector narrative →
Feb 2023
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
Based on record review, staff interviews, and facility policy review, the facility failed to prove a timely assessment and implement additional interventions for 1 of 3 residents (Resident #1) reviewe...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record review, staff interviews, and facility policy review, the facility failed to update 1 of 3 residents' care plans reviewed. After Resident #1 returned from the hospital with new orders ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on record review, staff interviews, and facility policy review the facility failed to transcribe orders for 1 of 3 residents (Resident #1) reviewed. The facility reported a census of 42 resident...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 4 life-threatening violation(s), Special Focus Facility, 3 harm violation(s), $167,067 in fines, Payment denial on record. Review inspection reports carefully.
- • 77 deficiencies on record, including 4 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $167,067 in fines. Extremely high, among the most fined facilities in Iowa. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Garden View Care Center's CMS Rating?
Garden View Care Center does not currently have a CMS star rating on record.
How is Garden View Care Center Staffed?
Detailed staffing data for Garden View Care Center is not available in the current CMS dataset.
What Have Inspectors Found at Garden View Care Center?
State health inspectors documented 77 deficiencies at Garden View Care Center during 2023 to 2025. These included: 4 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 3 that caused actual resident harm, 69 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Garden View Care Center?
Garden View Care Center is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by ARBORETA HEALTHCARE, a chain that manages multiple nursing homes. With 50 certified beds and approximately 39 residents (about 78% occupancy), it is a smaller facility located in Shenandoah, Iowa.
How Does Garden View Care Center Compare to Other Iowa Nursing Homes?
Comparison data for Garden View Care Center relative to other Iowa facilities is limited in the current dataset.
What Should Families Ask When Visiting Garden View Care Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Garden View Care Center Safe?
Based on CMS inspection data, Garden View Care Center has documented safety concerns. Inspectors have issued 4 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 0-star overall rating and ranks #100 of 100 nursing homes in Iowa. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Garden View Care Center Stick Around?
Garden View Care Center has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Garden View Care Center Ever Fined?
Garden View Care Center has been fined $167,067 across 3 penalty actions. This is 4.8x the Iowa average of $34,750. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Garden View Care Center on Any Federal Watch List?
Garden View Care Center is currently on the Special Focus Facility (SFF) watch list. This federal program identifies the roughly 1% of nursing homes nationally with the most serious and persistent quality problems. SFF facilities receive inspections roughly twice as often as typical nursing homes. Factors in this facility's record include 4 Immediate Jeopardy findings and $167,067 in federal fines. Facilities that fail to improve face escalating consequences, potentially including termination from Medicare and Medicaid. Families considering this facility should ask for documentation of recent improvements and what specific changes have been made since the designation.