CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility reported a census of 96 residents. Based on observation, interview, and record review, the facility failed to preve...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility reported a census of 96 residents. Based on observation, interview, and record review, the facility failed to prevent the neglect of cognitively impaired Resident (R)53, who had mental health disorder diagnoses, anger related to living in the facility, and a history of exit seeking, and the facility staff did not respond to his suicidal ideation statements after his elopement (when a cognitively impaired resident leaves the facility without the knowledge or supervision of staff). On [DATE], R53 eloped from the facility. When staff returned R53 to the facility, they placed a Wander Guard (a bracelet that sets off an alarm when residents wearing one attempt to exit the building without an escort) on R53, and he reported he would never eat again. On [DATE] at 04:00 PM, R53 made statements such as give me a gun so I can shoot myself. At 10:00 PM, the resident reported he was being held against his wishes. On [DATE] at 11:30 AM, R53 reported he would not eat until someone came back to talk about him being dismissed. Staff told R53 it may be a while before someone could get to him as there are others in need of services. On [DATE] at 10:02 AM, staff assessed R53 for exit seeking behaviors and continued 15-minute checks for 24 hours until reassessed. On [DATE], new orders were received to increase Seroquel 50 mg to three times a day. On [DATE] at 03:30 PM, staff found R53 had hung himself in his room with the TV cable on the closet door frame. This deficient practice placed R53 in immediate jeopardy.
Findings included:
- Review of the Electronic Health Record (EHR), documented R53 had diagnoses which included dementia (a progressive mental disorder characterized by failing memory and confusion) and bipolar (major mental illness that caused people to have episodes of severe high and low moods) and conduct disorder (a group of behavioral and emotional problems characterized by a disregard for others).
The [DATE] Annual Minimum Data Set (MDS) documented a Brief Interview for Mental Status (BIMS) score of 12, which indicated moderately impaired cognition. R53's total severity score of 00, indicating no depression. The MDS documented the resident did not have behaviors during the look back period. R53 was independent with all his activities of daily living (ADL).
The [DATE] Behavioral Symptoms Care Area Assessment (CAA) documented R53 had episodes of agitation and anxiety and staff would proceed to care plan with continued monitoring and assistance as needed to avoid complications and minimize risks related to behaviors, with referral to physician and/or psychiatric services as needed.
The [DATE] Quarterly MDS documented R53 had a BIMS score of nine, which indicated moderately impaired cognition. The MDS indicated no depression for the resident. R53 had become very anxious and agitated about why he was at the facility and when/why he could not go home for four to six days in the seven-day look-back period. R53 was independent with all his ADL.
The [DATE] Care Plan documented an intervention, dated [DATE], indicating R53 was not allowed outside of the community, independently. Staff were instructed to provide redirection, diversion, and reorientation if R53 became restless, agitated, or exit seeking. The staff were to consult the physician if R53 was not easily redirected or had continued behaviors. The resident was an elopement risk/wanderer. R53 had an actual elopement from the facility. R53 had depression and anxiety and was on a daily psychotropic medication for management, dated [DATE]. The staff would monitor, record, and report to physician as needed for harm to self, suicidal ideation's, or refusal to eat or take medications.
The [DATE], Elopement Assessment documented R53 was not at risk for elopement, however the assessment documented R53 was cognitively impaired, an exit seeker, diagnosed with dementia, and required a secured unit.
Review of the Progress Note revealed on [DATE] at 06:03 PM, R53 was upset about having to wait to get help to get out of the facility. R53 stated he was going to go, one way or another.
The [DATE] Nurse Practitioner Note documented R53 required long term care placement in a memory care unit due to high elopement risk. Furthermore, R53 was upset to still be living in a nursing facility and had daily aggression.
Review of the Progress Note revealed on [DATE] at 01:42 PM, R53 stated if he did not get dismissed, he would sneak out the back door at night.
The Progress Note on [DATE] revealed the following:
At approximately 07:15 AM, staff could not locate R53.
At approximately 08:30 AM, the staff located R53 approximately two miles away from the facility.
At 09:00 AM, Emergency Medical Services (EMS) transported R53 to the hospital for psychological evaluation and medical clearance after his elopement.
At 03:00 PM, R53 returned to facility from the hospital. The staff placed a Wander Guard bracelet (bracelet that sets off an alarm when residents wearing one attempt to exit the building without an escort) to R53's right wrist and placed R53 on one-hour checks for the following 72 hours.
The Progress Note on [DATE] revealed:
At 01:28 PM, staff found R53 at his window and when asked what he was doing. R53 questioned when am I getting out of here? The Wander Guard bracelet was not on R53's wrist, it was located behind the TV in R53's room. The staff notified Physician Extender TT, who instructed staff to give R53 space to calm down and reapproach the resident in a few hours.
At 02:30 PM, R53 continued to be adamant about leaving the facility and the staff contacted Administrative Nurse D.
At 03:30 PM, Administrative Nurse D instructed staff to send R53 to the hospital for evaluation, per provider order.
At 04:00 PM, staff informed R53 that EMS was on route to transport him to a hospital. R53 continued to make comments such as give me a gun so I can shoot myself. Staff were instructed to keep watch on the agitated resident.
At 04:30 PM, R53 left the facility with EMS.
At 10:00 PM, R53 returned to the facility, aggravated that he was back, and with one-on-one in place at that time.
The Progress Note on [DATE] at 06:39 PM, revealed the staff continued with one-on-one monitoring for R53 and the resident was verbally aggressive toward staff.
The [DATE] Physician Orders included an order for the Electronic WanderGuard bracelet to be applied to R53, staff to validate the functioning every night shift.
The Progress Note on [DATE] revealed:
At 08:05 AM, Physician Extender TT updated on R53's continued aggressive behavior and refusal to take medications. Physician Extender TT recommended an inpatient psychiatric stay.
At 08:25 AM, the facility nurse spoke to the hospital nurse, who suggested to send R53 to the hospital for evaluation.
The Progress Note on [DATE] at 01:36 PM revealed the facility nurse spoke with the nurse at 11:00 AM and was informed R53 would be diverted to another hospital for admission to a Behavioral Health Unit (BHU). At 11:30 AM, EMS transported R53, who left willingly, however he stated, I will murder you if I have a reason too.
The Progress Note on [DATE] at 05:20 PM, revealed R53 returned to facility, accompanied by EMS, with no new orders.
The [DATE] Physician Order required staff to check for the placement of the WanderGuard bracelet on every shift.
The Progress Note on [DATE] at 11:30 AM, revealed R53 refused his lunch meal and stated he would not eat again until someone came back to talk to him about his dismissal. The staff advised R53 that it may be a while before someone could talk to him as there were others in need of services. R53 continued to stand at an exit door to watch staff enter the code to the door.
The Progress Note on [DATE] at 02:37 PM, revealed staff noted a referral sent to a BHU at 11:15 AM due to increased behaviors. The BHU contacted the facility at 12:30 PM and informed them there were no beds available. The staff contacted a second behavioral unit and was informed there were no beds available. Staff sent a referral out to a third BHU at 02:41 PM, however, that unit staff stated the referral was not received and the referral was re-faxed.
The Progress Note on [DATE] at 03:06 AM, revealed R53 continued one-on-one supervision. R53 remained in his room.
The Progress Note on [DATE] at 10:02 AM, revealed the Administrative Nurse F assessed R53 for exit seeking behaviors. R53 was at baseline and staff would complete fifteen-minute checks for 24 hours.
The Progress Note on [DATE] at 10:06 AM, revealed Administrative Nurse F assessed the resident and noted R53 continued at baseline and staff discontinued the fifteen-minute checks.
Physician Extender TT's signed [DATE] Psychiatric Progress Note regarding the visit on [DATE] at 02:30 PM to 02:45 PM, documented R53 appeared disheveled, displayed irritable behavior, and had poor insight and impulse control. R53 remained focused on being released and became demanding and easily agitated. R53's conversation was tangential (different from or not directly connected with the one you are talking about) in nature, which further complicated the conversation and understanding R53's concerns. The staff reported R53's recent elopement and ongoing agitation and aggression. New order to increase on [DATE] at 12:45 PM, for R53's Quetiapine fumarate, 50 mg tablet to three times a day, for continued issues with mood and behavior.
The Progress Note on [DATE] at 12:59 PM, noted R53 continued to ask for dismissal orders.
The EHR lacked Progress Notes between the [DATE] at 12:59 PM and the [DATE] at 03:30 PM Progress Note.
The Progress Note on [DATE] documented:
At 03:30 PM, R53 was in his bed at 06:00 AM, with his eyes closed and breathing.
At 08:00 AM, staff administered R53's medications and R53 asked staff when he was leaving.
At approximately 11:30 AM, staff delivered lunch to R53 in his room. He asked how long he had been at the facility.
At approximately 01:00 PM, R53 brought his lunch dish to the nurse's station.
At approximately 03:30 PM, the staff found R53 hanging from his closet. The staff contacted the facility's management team.
At 03:38 PM, Administrative Nurse D and Administrative Nurse F entered R53's room and found R53 hanging from the television cable on the closet door frame. The staff assisted R53 to the floor and began cardiopulmonary resuscitation (CPR- emergency lifesaving procedure performed when the heart stops beating). The staff called 911 and continued CPR.
At 04:00 PM, EMS arrived and took over CPR. Social Service Designee contacted the guardian.
At 04:05 PM, time of death was announced as EMS/Medical Coroner stopped all compressions per the guardian's request.
Review of the Facility Investigation dated [DATE] revealed through record review and interview of staff, family, and physician services, determined that R53 had a previous history of possible suicide ideation's. It was determined at the time of the event, R53 was not known to be a danger to himself or others and had remained stable per his baseline.
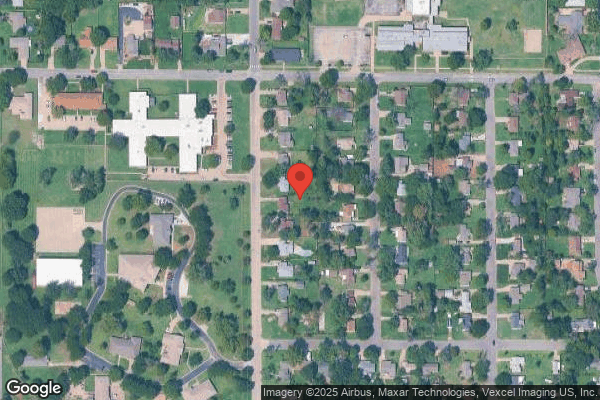
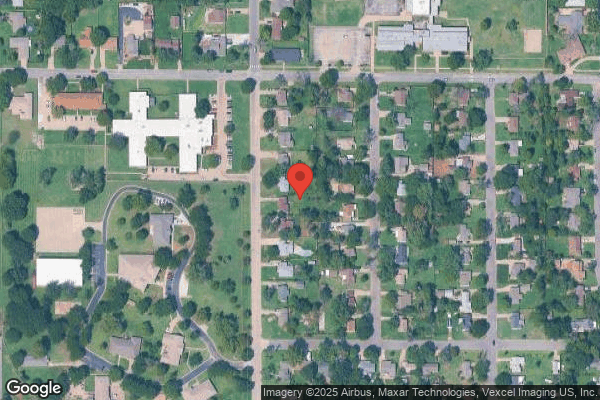
Observation on [DATE] at 11:30 AM, revealed the memory care unit courtyard exit required a code to exit and enter. There was a six-foot wooden fence that surrounded the courtyard and attached to the building. There was a small alcove area that was near the exit door, not completely visible for staff to observe when they looked out the windows to the courtyard.
During an interview on [DATE] at 11:38 AM, CNA Q reported R53 eloped in 2022, and she did not know when R53 had his Wander Guard removed after the elopement in 2022. CNA Q stated she had been educated previously to never let a resident outside by themselves in the courtyard. R53 had exit seeking behaviors as he would state he wanted to leave. CNA Q said the green patio chairs in the courtyard were removed after R53 eloped on [DATE]. She also confirmed she received education after R53 eloped in [DATE] and she received education about abuse, trauma, and suicide in July after the incident.
During an interview on [DATE] at 02:26 PM, CNA MM stated R53 always asked him about being able to leave the facility. CNA MM stated that he received education about elopement, abuse, and trauma after R53 eloped on [DATE]. He also stated that R53 never made verbal comments of hurting himself and he had received training on suicide.
During an interview on [DATE] at 02:26 PM, CNA NN stated R53 always asked about leaving the facility and wanted to live somewhere else. CNA NN stated he received education after R53 eloped, that included elopement, abuse, and trauma. He also stated that R53 never made verbal comments of hurting himself and he had received training on suicide.
On [DATE] at 03:40 PM, Licensed Nurse (LN) I stated she could not locate R53 on [DATE] at approximately 07:15 AM and said CNA P last observed R53 in the courtyard. LN I stated she checked the sign-out book and confirmed R53 had not signed out of the facility. Staff could not locate R53 on the unit and contacted all staff on pager system and announced a Dr. Walker at approximately 07:30 AM. Administrative staff B located the resident at approximately 08:30 AM and brought him back to the facility. LN I confirmed R53 was very agitated about residing at the facility and his behaviors were almost daily. LN I was not sure if R53 had a previous elopement from the facility. LN I stated R53 was antsy and agitated and wanted to get out. She stated that R53 was placed on one-on-one observations 24 hours a day for about two weeks. LN I stated several staff members took turns with R53's one-on-one observation. LN I reviewed Physician Extender TT psychiatric progress note that was received on [DATE], however Physician Extender TT assessed R53 on [DATE]. LN I stated that Physician Extender would write new orders in the facility if needed and that waiting six days for new orders after a visit is not usual. LN I stated R53 was very agitated about being in the facility and never voiced any suicidal ideation's to her. LN I verified R53 had no progress notes charted in the EHR between the [DATE] at 12:59 PM progress note and the [DATE] at 03:30 PM progress note, when R53 was found hung in his room. LN I stated he was still wanting to leave but not as aggressive during that time period or a note would have been written, and stated the nurses' chart by exception. LN I also stated they do not chart notes on psych (antipsychotic- class of medications used to treat major mental conditions which cause a break from reality) medications when changed, unless there was a concern. She stated the nurses would have to chart a lot on the residents, as psych medication changes occur often. LN I stated she had education for elopement, abuse, trauma, and suicidal ideation's signs and symptoms and to report concerns immediately to management.
On [DATE] at 12:02 PM, LN G stated she was not at work the day R53 eloped from facility on [DATE]. She stated that she would not let a resident outside by themselves. LN G revealed that R53 was an exit seeker since the first day he admitted in December of 2022, and was not given a Wander Guard bracelet until after he eloped in December of 2022 shortly after he admitted to the facility. LN G could not recall when staff removed R53's wander guard bracelet. LN G stated that is not normal to receive new orders several days after a resident was seen by a provider. LN G stated that no progress notes were required after a medication change unless there was a concern. LN G stated she last saw R53 on [DATE] and he was his normal self. She confirmed that she received education after both incidents occurred, that included abuse, elopement, trauma, and suicidal ideation's and the facility had an elopement drill.
On [DATE] at 03:00 PM, Administrative Nurse D stated that Physician Extender TT generally did not write orders in the facility when she assessed residents. Administrative Nurse D said Physician Extender TT would email to her all the signed progress notes with orders written on them if she wrote new orders. She stated it would take several days to receive the progress notes and orders back from Physician Extender TT and stated that was not acceptable. Administrative Nurse D confirmed that nurses generally charted when there was a concern.
On [DATE] at 11:49 AM, Administrative Nurse F stated residents from the memory care units were not allowed to go outside in the courtyard or off the units independently. She stated R53 had always been an elopement risk and staff received education on abuse, elopement, suicidal ideation's, and trauma. She stated that the facility tried to assist R53 to get admitted to a behavioral unit a few times and he would just be sent back from the hospital.
On [DATE] at 03:50 PM, phone interview with Physician Extender TT, revealed the progress notes and orders received for R53 on [DATE] from her visit on [DATE] was later than normal. She stated it typically took 48-72 hours to write, sign, and email the progress notes and orders to the Administrative Nurse D. Physician Extender TT verified she would not write orders at the facility during a visit, due to the number of residents she saw there. She stated she was not updated on R53's comment from [DATE] that he would shoot himself if he had a gun. Physician Extender TT stated she received her information from the Administrative Nurse F and the Administrative Nurse D and said the staff on the unit were not the best resource for information needed. She confirmed R53 should have received the order for his medication increase sooner than he did.
The facility Suicide Threats policy dated 02/2021 documented if a resident made a suicidal threat, stay with the resident, and immediately notify the nurse.
The nurse would assess the resident and notify the Director of Nursing or designee and medical provider to establish a plan of care.
The resident's environment would be evaluated, and potentially dangerous items removed.
The interdisciplinary team would review documentations and behaviors and revise the plan of care.
The facility failed to prevent the neglect of cognitively impaired, R53, with known mental illness and anger related to placement in the facility, when staff failed to respond to his suicidal ideation comments after he eloped from the facility on [DATE]. This deficient practice placed R53 in immediate jeopardy, and R53 hung himself with a cable cord from his closet door.
On [DATE] at 09:10 AM, Administrative Staff A and Consultant Staff SS were provided the Immediate Jeopardy (IJ) template and notified the facility failed to prevent the neglect of cognitively impaired, R53, with known mental illness and anger related to placement in the facility, when staff failed to respond to his suicidal ideation comments after he eloped from the facility on [DATE]. This deficient practice placed R53 in immediate jeopardy, and R53 hung himself with a cable cord from his closet door on [DATE].
The facility identified and implemented the following corrective actions, completed on [DATE] after R53's suicide:
1. An Ad Hoc Quality Assurance and Performance Improvement (QAPI) meeting held by interdisciplinary team on [DATE].
2. The Administrator notified the Medical Director on [DATE] at 09:00 AM.
3. The [NAME] President of Clinical Operations re-educated the Administrator and Director of Nursing on community process for recognizing signs and symptoms of suicidal on [DATE].
4. The Corporate Director of Clinical Reimbursement educated the Administrator, Social Service staff, and Director of Nursing regarding the community process of the social service comprehensive assessment and trauma informed care assessment. Education included intended scheduled, psychosocial care planning of
5. Current associates will be re-educated by the community by the Administrator or designee on or before [DATE] or prior to working next scheduled shift on community. Trauma Informed Care process with specific focus on identification of suicidal symptoms and suicidal ideation, required notifications and immediate actions.
6. Social Service comprehensive assessments will be completed upon admission, annually and with significant change. Assessment will be documented in resident medical record.
7. Residents identified with need for trauma preventative services will have a trauma informed assessment
completed upon admission, annually and with identified significant change in condition. Assessments will be
documented in resident medical record. Care plan will be updated as indicated.
8. Routine angle rounds will be completed by assigned interdisciplinary team members routinely and will
include staff members interviews to validate understanding of resident suicide awareness and notification
requirements. Results of the angel rounds will be reported during routine morning stand up meetings. If
discrepancies are identified immediate one on one educations will be completed with associate involved.
9. During weekly risk review meetings, the interdisciplinary team will review the clinical record of newly admitted residents or residents identified change in condition to validate completion of required social service assessments and or trauma informed care evaluations when indicated. The review will be documented in the resident medical record.
10. The Administrator or designee will routinely review sample selected residents for the next 60 days to validate compliance of the following: completion of the social service comprehensive assessment as appropriate, completion of trauma informed care assessment as appropriate, psychosocial care plan present when indicated that include resident specific interventions based upon assessment findings; any noted suicidal ideation as indicated.
11. Monthly review of completed weekly risk review and angle rounds results and trends will be completed by the Administrator or designee and reported to the QAPI committee for the next three months and then re-evaluate to determine if further monitoring is indicated.
Due to the corrective actions the facility completed prior to the onsite visit, the deficient practice was deemed past non-compliance and existed at a J scope and severity.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
The facility reported a census of 96 residents and the facility identified five residents at risk for elopement. Based on observation, interview, and record review the facility failed to provide adequ...
Read full inspector narrative →
The facility reported a census of 96 residents and the facility identified five residents at risk for elopement. Based on observation, interview, and record review the facility failed to provide adequate supervision to cognitively impaired, independently mobile Resident (R)53, identified as a high risk for elopement. On 06/29/24 at approximately 07:15 AM, staff were unable to locate R53 in the facility. On 06/29/24 at approximately 08:30 AM, staff located R53 approximately two miles away from the facility. R53 walked down busy residential areas with a 35 mile per hour speed limit and would have crossed 20 cross walks and crossed over two river bridges. This deficient practice placed R53 in immediate jeopardy. Furthermore, the facility failed to keep R54 safe, related to fall hazards in R54's room.
Findings included:
- Review of the Electronic Health Record (EHR) documented R53 had diagnoses, which included dementia (a progressive mental disorder characterized by failing memory and confusion), bipolar (major mental illness that caused people to have episodes of severe high and low moods) and conduct disorder (a group of behavioral and emotional problems characterized by a disregard for others). R53 admitted to facility on 12/07/2022.
The 11/20/23 Annual Minimum Data Set (MDS) documented a Brief Interview for Mental Status (BIMS) score of 12, which indicated moderately impaired cognition. R53 had a total mood severity score of 00, indicating no depression and there were no behaviors documented on the assessment. R53 was independent with all his activities of daily living (ADLs).
The 11/20/23 Behavioral Symptoms Care Area Assessment (CAA) documented R53 had episodes of agitation and anxiety. Staff would care plan continued monitoring of the resident and provide assistance as needed to avoid complications and minimize risks related to behaviors, with referral to physician and/or psychiatric services as needed.
The 05/16/24 Quarterly MDS documented a BIMS score of nine, which indicated moderately impaired cognition. No depression noted. R53 was very anxious and agitated about why he was at the facility and when/why he could not go home for four to six days of the seven-day look-back period. R53 was independent with all his ADLs.
The 07/22/24 Care Plan documented an intervention, dated 12/09/22 instructing staff R53 was not allowed outside of the community independently. Staff were instructed to provide redirection, diversion, and reorientation if R53 became restless, agitated, or began exit seeking. Staff would consult the physician if R53 was not easily redirected or had continued behaviors. The resident was an elopement risk/wanderer and on 12/09/22, R53 had an actual elopement from the facility.
The Elopement Assessments revealed the following for R53:
On 12/27/22, 12/09/22, 12/15/22, 03/10/23, 07/10/23, 08/21/23, 11/14/23 and 02/15/24, R53 was identified at risk for elopement.
On 05/13/24 Elopement Assessment, documented R53 was not at risk for elopement, however the assessment documented R53 was cognitively impaired, an exit seeker, diagnosed with dementia, and required a secured unit.
Review of the Progress Notes from 01/01/24 to 06/29/24 revealed the following:
On 04/09/24 at 06:03 PM, R53 was upset about having to wait to get help to get out of the facility. R53 stated he was going to go one way or another.
On 06/22/24 at 01:42 PM, R53 stated if he did not get dismissed, he would sneak out the back door at night.
On 06/29/24 at approximately 07:15 am, staff were unable to locate R53. The facility notified Law Enforcement at approximately 08:00 AM. Staff were able to locate R53 at around 08:30 AM approximately two miles away from the facility.
Review of the Nurse Practitioner Note dated 06/11/24, documented R53 required long term care placement in a memory care unit due to high elopement risk. Furthermore, R53 was upset to be still living in a nursing facility and had daily aggression.
Review of the Facility Investigation, revealed on 06/29/24 at approximately 06:00 AM, Licensed Nurse (LN) J and Certified Nurse Aide (CNA) N provided R53 access to the courtyard to consume a cup of coffee independently. CNA N passed in report to the oncoming CNA O where R53 was. At approximately 06:45 AM, CNA P verified R53 was in the courtyard patio on the bench, with his hands folded, dressed in shirt, pants, and tennis shoes. At approximately 07:15 AM, LN I could not locate R53 and instructed CNA O and CNA P to search the entire Memory Care Unit as R53 was an elopement risk. LN I checked the sign-out book and verified R53 was not signed out. At approximately 07:30 AM, LN I, CNA O, and CNA P confirmed R53 was not in the unit or the courtyard. CNA O located a patio chair placed in the corner of the six-foot-tall fence. LN I initiated the elopement procedure and called a Dr. [NAME] code for (missing resident) over the pager system to alert all staff. All staff assisted with the search of R53 inside and outside of the facility. Staff members drove around the area of the facility, without locating R53. At approximately 07:50 AM, the Police Department was notified of R53 missing from the facility. At approximately 08:25 AM, Administrative Staff B located R53 located approximately two miles from the facility. Administrative Staff B brought R53 back to the facility at approximately 08:45 AM. The physician ordered R53 to a hospital emergency room for a psychological evaluation. Emergency medical staff transported R53 to the hospital at 09:00 AM.
Observation of the area R53 would have presumably walked down was a busy residential area with a 35 miles per hour speed limit and R53 would have crossed 20 cross walks and crossed over two river bridges.
Review of the weather data for the facility area from Weather Underground (www.wunderground.com) on 06/29/24 at approximately 06:45 AM, was daylight and the temperature was 77 degrees Fahrenheit.
On 07/30/24 at 03:40 PM, LN I stated she could not locate R53 on 06/29/24 at approximately 07:15 AM and stated that CNA P last observed R53 in the courtyard. She instructed CNA P and CNA O to complete a thorough check of the unit to locate R53. LN I stated she checked the sign-out book and confirmed R53 had not signed out of the facility. Staff could not locate R53 on the unit and contacted all staff on pager system and announced a Dr. Walker at approximately 07:30 AM. LN I stated she contacted Administrative Nurse F and contacted the Police Department at approximately 08:00 AM as staff had not yet located R53. Some of the staff drove their own vehicles to locate R53. The Police Department arrived at the facility around 08:08 AM and were given a description and picture of R53. Administrative staff B located the resident at approximately 08:30 AM and he was brought back to the facility. LN I confirmed R53 was very agitated about having to reside at the facility and his behaviors were almost daily. LN I was not sure if R53 had a previous elopement from the facility.
On 07/31/24 at 11:38 AM, CNA Q reported R53 had an elopement in 2022, she was unsure when R53 had his Wander Guard (bracelet that sets off an alarm when residents wearing one attempt to exit the building without an escort) removed after the elopement in 2022. CNA Q stated she had been educated previously to never let a resident outside by themselves in the courtyard. R53 had exit seeking behaviors as he would state he wanted to leave. The green patio chairs in the courtyard were removed after R53 eloped on 06/29/24. She also confirmed that she received education after R53 eloped in June 2024.
On 07/31/24 at 02:26 PM, CNA MM stated R53 always asked him about being able to leave the facility. CNA MM stated he received education about elopement, abuse, and trauma after R53 eloped on 06/29/24.
On 07/31/24 at 02:26 PM, CNA NN stated R53 always asked about leaving the facility and wanted to live somewhere else. Stated that he received education after R53 eloped on elopement, abuse, and trauma.
On 07/31/24 at 11:49 AM, Administrative Nurse F stated no residents from the memory care units were allowed to go outside in the courtyard or off of the units independently. She stated R53 had always been an elopement risk and staff received education on abuse, elopement, and trauma.
Observation on 07/31/24 at 11:30 AM, the memory care unit courtyard exit required a code to exit and enter. There was a six-foot wooden fence that surrounded the courtyard and attached to the building. In the courtyard there was a small alcove area that was near the exit door, not completely visible for staff to observe when they looked out the windows to the courtyard.
The facility Elopements policy dated 05/2023 documented it is the policy of the facility that all residents were afforded adequate supervision to provide a safe environment possible. Residents who are at risk for elopement are provide with at least one of the following safety precautions.
1. Door alarms on facility exit
2. A personal safety device that will alert facility when resident has left the building without supervision.
(Wander guard bracelet).
3. Staff supervision.
The facility failed to provide adequate supervision to cognitively impaired, independently mobile R53, identified as a high risk for elopement. On 06/29/24 at approximately 07:15 AM, staff were unable to locate R53 in the facility. R53 was found approximately 45 minutes later, at 08:30 AM, approximately two miles away from the facility. This deficient practice placed R53 in immediate jeopardy.
On 07/31/24 at 09:10 AM, Administrative Staff A and Consultant Staff SS were provided the Immediate Jeopardy (IJ) template for failure to provide R 53, a cognitively impaired resident who had a history of making comments about leaving, was identified as an elopement risk, and had anger issues regarding placement in the facility a safe environment from leaving the facility without staff knowledge.
The immediate jeopardy was determined to first exist on 06/29/24 at 06:00 AM, when staff left R53 unsupervised, outside on a memory care unit and he climbed a fence, left the facility, and was located approximately two miles away.
The facility identified and implemented the following corrective actions, completed on 07/02/24:
1. The Community Interdisciplinary Team completed a review of the community on 07/02/24 with four additional residents identified as being at risk for elopement and placed in wander guard alarms.
2. An Ad Hoc Quality Assurance and Performance Improvement (QAPI) meeting held by interdisciplinary team on 06/29/24.
3. The Administrator notified the Medical Director on 06/29/24.
4. Current clinical associates were re-educated by the Director of Nursing or designee before 07/02/24, or prior to working next scheduled shift on the Community Elopement policy and Community Elopement Evaluation process. Education included identification of at -risk residents, and courtyard oversight requirements.
5. Residents with a new risk for elopement or change in elopement risk will be reviewed by clinical interdisciplinary team during routine clinical huddle to verify elopement risk assessment accuracy, physician notification and preventative interventions in place as indicated. If discrepancies identified, immediate corrective action will be completed, and one on one education completed as indicated.
6. Residents identified with a change in elopement risk or who have had an actual elopement attempt will be reviewed during routine risk meeting by clinical interdisciplinary team. Review will be documented in the resident electronic medical record.
7. Routine elopement drills scheduled per community policy on varying shifts to confirm staff competency.
8. Findings of elopement drills are to be reported to the community Administrator and reviewed at the following morning meeting. If discrepancies are identified immediate correction will be completed and one on one education provided as indicated.
Due to the corrective actions the facility completed prior to the onsite visit, the deficient practice was deemed past non-compliance and existed at a J scope and severity.
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0742
(Tag F0742)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility reported a census of 96 residents. The sample included 20 residents. Based on observation, interview, and record re...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility reported a census of 96 residents. The sample included 20 residents. Based on observation, interview, and record review, the facility failed to ensure the appropriate treatment and services to attain the highest practicable mental and psychosocial well-being of cognitively impaired Resident (R)53, who had a mental health disorder diagnoses, portrayed anger related to living in the facility, a history of exit seeking, and the facility staff did not respond to his suicidal ideation statements after his elopement (when a cognitively impaired resident leaves the facility without the knowledge or supervision of staff). On [DATE], R53 eloped from the facility. When staff returned R53 to the facility they placed a WanderGuard (a bracelet that sets off an alarm when residents wearing one attempt to exit the building without an escort) on R53, and he reported he would never eat again. On [DATE] at 04:00 PM, R53 made statements such as give me a gun so I can shoot myself. At 10:00 PM, the resident reported he was being held against his wishes. On [DATE] at 11:30 AM, R53 reported he would not eat until someone came back to talk about him being discharged from the facility. An unidentified Staff told R53 it may be a while before someone could get to him as there are others in need of services. On [DATE] at 03:30 PM, staff found R53 had hung himself in his room with the TV cable on the closet door frame. This deficient practice placed R53 in immediate jeopardy.
Findings included:
- Review of the Electronic Health Record (EHR), documented R53 had diagnoses which included dementia (a progressive mental disorder characterized by failing memory and confusion) and bipolar (major mental illness that caused people to have episodes of severe high and low moods) and conduct disorder (a group of behavioral and emotional problems characterized by a disregard for others).
The [DATE] Annual Minimum Data Set (MDS) documented a Brief Interview for Mental Status (BIMS) score of 12, which indicated moderately impaired cognition. R53's total mood severity score of 00, indicated no depression. The MDS documented the resident did not have behaviors during the look back period. R53 was independent with all his activities of daily living (ADL).
The [DATE] Behavioral Symptoms Care Area Assessment (CAA) documented R53 had episodes of agitation and anxiety and staff would proceed to care plan with continued monitoring and assistance as needed to avoid complications and minimize risks related to behaviors, with referral to physician and/or psychiatric services as needed.
The [DATE] Quarterly MDS documented R53 had a BIMS score of nine, which indicated moderately impaired cognition. The MDS indicated no depression for the resident. R53 had become very anxious and agitated about why he was at the facility and when/why he could not go home for four to six days in the seven-day look-back period. R53 was independent with all his ADL.
The [DATE] Care Plan documented an intervention, dated [DATE], indicating R53 was not allowed outside of the community, independently. Staff were instructed to provide redirection, diversion, and reorientation if R53 became restless, agitated, or exit seeking. The staff were to consult the physician if R53 was not easily redirected or had continued behaviors. The resident was an elopement risk/wanderer. R53 had an actual elopement from the facility. R53 had depression and anxiety and was on a daily psychotropic (alters mood or thought) medication for management, dated [DATE]. The staff would monitor, record, and report to physician as needed for harm to self, suicidal ideation's, or refusal to eat or take medications.
Review of the Progress Note revealed on [DATE] at 06:03 PM, R53 was upset about having to wait to get help to get out of the facility. R53 stated he was going to go, one way or another.
The [DATE] Nurse Practitioner Note documented R53 required long term care placement in a memory care unit due to high elopement risk. Furthermore, R53 was upset to still be living in a nursing facility and had daily aggression.
Review of the Progress Note revealed on [DATE] at 01:42 PM, R53 stated if he did not get dismissed, he would sneak out the back door at night.
The Progress Note on [DATE] revealed:
At approximately 07:15 AM, staff could not locate R53.
At approximately 08:30 AM, the staff located R53 approximately two miles away from the facility.
At 09:00 AM, Emergency Medical Services (EMS) transported R53 to the hospital for psychological evaluation and medical clearance after his elopement.
At 03:00 PM, R53 returned to facility from the hospital. The staff placed a WanderGuard bracelet to R53's right wrist and placed R53 on one-hour checks for the next 72 hours.
The Progress Note on [DATE] revealed:
At 01:28 PM, staff found R53 at his window and when asked what he was doing R53 questioned when am I getting out of here? The WanderGuard bracelet was not on R53's wrist, it was located behind the TV in R53's room. The staff notified Physician Extender TT, who instructed staff to give R53 space to calm down and reapproach the resident in a few hours.
At 02:30 PM, R53 continued to be adamant about leaving the facility and the staff contacted Administrative Nurse D.
At 03:30 PM, Administrative Nurse D instructed staff to send R53 to the hospital for evaluation, per provider order.
At 04:00 PM, staff informed R53 that EMS was on route to transport him to a hospital. R53 continued to make comments such as give me a gun so I can shoot myself. Staff were instructed to keep watch on the agitated resident.
At 04:30 PM, R53 left the facility with EMS.
At 10:00 PM, R53 returned to facility, aggravated that he was back, and with one-on-one in place at that time.
The Progress Note on [DATE] at 06:39 PM, revealed the staff continued with one-on-one monitoring for R53 and the resident was verbally aggressive toward staff.
The [DATE] Physician Orders included an order for the Electronic WanderGuard bracelet (bracelet that sets off an alarm when residents wearing one attempt to exit the building without an escort) to be applied to R53, staff to validate the functioning every night shift.
The Progress Note on [DATE] revealed:
At 08:05 AM, Physician Extender TT updated on R53's continued aggressive behavior and refusal to take medications. Physician Extender TT recommended an inpatient psychiatric stay.
At 08:25 AM, the facility nurse spoke to the hospital nurse, who suggested to send R53 to the hospital for evaluation.
The Progress Note on [DATE] at 01:36 PM revealed the facility nurse spoke with the nurse at 11:00 AM and was informed R53 would be diverted to another hospital for admission to a Behavioral Health Unit (BHU). At 11:30 AM, EMS transported R53, who left willingly, however he stated, I will murder you if I have a reason too.
The Progress Note on [DATE] at 05:20 PM, revealed R53 returned to facility, accompanied by EMS, with no new orders.
The Progress Note on [DATE] at 11:30 AM, revealed R53 refused his lunch meal and stated he would not eat again until someone came back to talk to him about his dismissal. The staff advised R53 that it may be a while before someone could talk to him as there were others in need of services. R53 continued to stand at an exit door to watch staff enter the code to the door.
The Progress Note on [DATE] at 02:37 PM, revealed staff noted a referral sent to a BHU at 11:15 AM due to increased behaviors. The BHU contacted the facility at 12:30 PM and informed them there were no beds available. The staff contacted a second behavioral unit and was informed there were no beds available. Staff sent a referral out to a third BHU at 02:41 PM, however, that unit staff stated the referral was not received and the referral was re-faxed.
The Progress Note on [DATE] at 03:06 AM, revealed R53 continued one-on-one supervision. R53 remained in his room.
The Progress Note on [DATE] at 10:02 AM, revealed the Administrative Nurse F assessed R53 for exit seeking behaviors. R53 was at baseline and staff would complete fifteen-minute checks for 24 hours.
The Progress Note on [DATE] at 10:06 AM, revealed Administrative Nurse F assessed the resident and noted R53 continued at baseline and staff discontinued the fifteen-minute checks.
Physician Extender TT's signed [DATE] Psychiatric Progress Note regarding the visit on [DATE] at 02:30 PM to 02:45 PM, documented R53 appeared disheveled, displayed irritable behavior, and had poor insight and impulse control. R53 remained focused on being released and became demanding and easily agitated. R53's conversation was tangential (different from or not directly connected with the one you are talking about) in nature, which further complicated the conversation and understanding R53's concerns. The staff reported R53's recent elopement and ongoing agitation and aggression. New order to increase on [DATE] at 12:45 PM, for R53's Quetiapine fumarate, 50 mg tablet to three times a day, for continued issues with mood and behavior.
The Progress Note on [DATE] at 12:59 PM, noted R53 continued to ask for dismissal orders.
The EHR lacked Progress Notes between the [DATE] at 12:59 PM and the [DATE] at 03:30 PM Progress Note.
The Progress Note on [DATE] documented:
At 03:30 PM, R53 was in his bed at 06:00 AM, with his eyes closed and breathing.
At 08:00 AM, staff administered R53's medications and R53 asked staff when he was leaving.
At approximately 11:30 AM, staff delivered lunch to R53 in his room. He asked how long he had been at the facility.
At approximately 01:00 PM, R53 brought his lunch dish to the nurse's station.
At approximately 03:30 PM, the staff found R53 hanging from his closet. The staff contacted the facility's management team.
At 03:38 PM, Administrative Nurse D and Administrative Nurse F entered R53's room and found R53 hanging from the television cable on the closet door frame. The staff assisted R53 to the floor and began cardiopulmonary resuscitation (CPR- emergency lifesaving procedure performed when the heart stops beating). The staff called 911 and continued CPR.
At 04:00 PM, EMS arrived and took over CPR. Social Service Designee contacted the guardian.
At 04:05 PM, time of death was announced as EMS/Medical Coroner stopped all compressions per the guardian's request.
Observation of the area, R53 would have presumably walked down was a residential area with a 35 miles per hour speed limit and R53 would have crossed 20 cross walks and crossed over two river bridges.
Observation on [DATE] at 11:30 AM, revealed the memory care unit courtyard exit required a code to exit and enter. There was a six-foot wooden fence that surrounded the courtyard and attached to the building. There was a small alcove area that was near the exit door, not completely visible for staff to observe when they looked out the windows to the courtyard.
During an interview on [DATE] at 11:38 AM, CNA Q reported R53 eloped in 2022, and she did not know when R53 had his WanderGuard removed after the elopement in 2022. CNA Q stated she had been educated previously to never let a resident outside by themselves in the courtyard. R53 had exit seeking behaviors as he would state he wanted to leave. CNA Q said the green patio chairs in the courtyard were removed after R53 eloped on [DATE]. She also confirmed she received education after R53 eloped in [DATE] and she received education about abuse, trauma, and suicide in July after the incident.
During an interview on [DATE] at 02:26 PM, CNA MM stated R53 always asked him about being able to leave the facility. CNA MM stated that he received education about elopement, abuse, and trauma after R53 eloped on [DATE]. He also stated that R53 never made verbal comments of hurting himself and he had received training on suicide.
During an interview on [DATE] at 02:26 PM, CNA NN stated R53 always asked about leaving the facility and wanted to live somewhere else. CNA NN stated he received education after R53 eloped, that included elopement, abuse, and trauma. He also stated that R53 never made verbal comments of hurting himself and he had received training on suicide.
On [DATE] at 03:40 PM, Licensed Nurse (LN) I stated she could not locate R53 on [DATE] at approximately 07:15 AM and said CNA P last observed R53 in the courtyard. LN I stated she checked the sign-out book and confirmed R53 had not signed out of the facility. Staff could not locate R53 on the unit and contacted all staff on pager system and announced a Dr. Walker at approximately 07:30 AM. Administrative staff B located the resident at approximately 08:30 AM and brought him back to the facility. LN I confirmed R53 was very agitated about residing at the facility and his behaviors were almost daily. LN I was not sure if R53 had a previous elopement from the facility. LN I stated R53 was antsy and agitated and wanted to get out. She stated that R53 was placed on one-on-one observations 24 hours a day for about two weeks. LN I stated several staff members took turns with R53's one-on-one observation. LN I reviewed Physician Extender TT psychiatric progress note that was received on [DATE], however Physician Extender TT assessed R53 on [DATE]. LN I stated that Physician Extender would write new orders in the facility if needed and that waiting six days for new orders after a visit is not usual. LN I stated R53 was very agitated about being in the facility and never voiced any suicidal ideation's to her. LN I verified R53 had no progress notes charted in the EHR between the [DATE] at 12:59 PM progress note and the [DATE] at 03:30 PM progress note, when R53 was found hung in his room. LN I stated he was still wanting to leave but not as aggressive during that time period or a note would have been written, and stated the nurses' chart by exception. LN I also stated they do not chart notes on psych medications when changed, unless there was a concern. She stated the nurses would have to chart a lot on the residents, as psych medication changes occur often. LN I stated she had education for elopement, abuse, trauma, and suicidal ideation's signs and symptoms and to report concerns immediately to management.
On [DATE] at 12:02 PM, LN G stated she was not at work the day R53 eloped from facility on [DATE]. She stated that she would not let a resident outside by themselves. LN G revealed that R53 was an exit seeker since the first day he admitted in December of 2022, and was not given a WanderGuard bracelet until after he eloped in December of 2022 shortly after he admitted to the facility. LN G could not recall when staff removed R53's WanderGuard bracelet. LN G stated that is not normal to receive new orders several days after a resident was seen by a provider. LN G stated that no progress notes were required after a medication change unless there was a concern. LN G stated she last saw R53 on [DATE] and he was his normal self. She confirmed that she received education after both incidents occurred, that included abuse, elopement, trauma, and suicidal ideation's and the facility had an elopement drill.
On [DATE] at 03:00 PM, Administrative Nurse D stated that Physician Extender TT generally did not write orders in the facility when she assessed residents. Administrative Nurse D said Physician Extender TT would email to her all the signed progress notes with orders written on them if she wrote new orders. She stated it would take several days to receive the progress notes and orders back from Physician Extender TT and stated that was not acceptable. Administrative Nurse D confirmed that nurses generally charted when there was a concern.
On [DATE] at 11:49 AM, Administrative Nurse F stated residents from the memory care units were not allowed to go outside in the courtyard or off the units independently. She stated R53 had always been an elopement risk and staff received education on abuse, elopement, suicidal ideation's and trauma. She stated that the facility tried to assist R53 to get admitted to a behavioral unit a few times and he would just be sent back from the hospital.
The facility Suicide Threats policy dated 02/2021 documented if a resident made a suicidal threat, stay with the resident and immediately notify the nurse.
The nurse would assess the resident and notify the Director of Nursing or designee and medical provider to establish a plan of care.
The resident's environment would be evaluated, and potentially dangerous items removed.
The interdisciplinary team would review documentations and behaviors and revise the plan of care.
The facility failed ensure the appropriate treatment and services to attain the highest practicable mental and psychosocial well-being to cognitively impaired, R53, with known mental illness and anger related to placement in the facility, when staff failed to respond to his suicidal ideation comments after he eloped from the facility on [DATE]. This deficient practice placed R53 in immediate jeopardy, and R53 hung himself with a cable cord from his closet door.
On [DATE] at 09:10 AM, Administrative Staff A and Consultant Staff SS were provided the Immediate Jeopardy (IJ) template and notified the facility failed to prevent the neglect of cognitively impaired, R53, with known mental illness and anger related to placement in the facility, when staff failed to respond to his suicidal ideation comments after he eloped from the facility on [DATE]. This deficient practice placed R53 in immediate jeopardy, and R53 hung himself with a cable cord from his closet door on [DATE].
The immediate jeopardy was determined to first exist on [DATE] at 06:00 AM, when staff left R53 unsupervised, outside on a memory care unit and he climbed a fence, left the facility, and was located approximately two miles away.
The facility identified and implemented the following corrective actions, completed on [DATE] after R53's suicide:
1. An Ad Hoc Quality Assurance and Performance Improvement (QAPI) meeting held by interdisciplinary team on [DATE].
2. The Administrator notified the Medical Director on [DATE] at 09:00 AM.
3. The [NAME] President of Clinical Operations re-educated the Administrator and Director of Nursing on community process for recognizing signs and symptoms of suicidal on [DATE].
4. The Corporate Director of Clinical Reimbursement educated the Administrator, Social Service staff, and Director of Nursing regarding the community process of the social service comprehensive assessment and trauma informed care assessment. Education included intended scheduled, psychosocial care planning of
5. Current associates will be re-educated by the community by the Administrator or designee on or before [DATE] or prior to working next scheduled shift on community. Trauma Informed Care process with specific focus on identification of suicidal symptoms and suicidal ideation, required notifications and immediate actions.
6. Social Service comprehensive assessments will be completed upon admission, annually and with significant change. Assessment will be documented in resident medical record.
7. Residents identified with need for trauma preventative services will have a trauma informed assessment
completed upon admission, annually and with identified significant change in condition. Assessments will be
documented in resident medical record. Care plan will be updated as indicated.
8. Routine angle rounds will be completed by assigned interdisciplinary team members routinely and will
include staff members interviews to validate understanding of resident suicide awareness and notification
requirements. Results of the angel rounds will be reported during routine morning stand up meetings. If
discrepancies are identified immediate one on one educations will be completed with associate involved.
9. During weekly risk review meetings, the interdisciplinary team will review the clinical record of newly admitted residents or residents identified change in condition to validate completion of required social service assessments and or trauma informed care evaluations when indicated. The review will be documented in the resident medical record.
10. The Administrator or designee will routinely review sample selected residents for the next 60 days to validate compliance of the following: completion of the social service comprehensive assessment as appropriate, completion of trauma informed care assessment as appropriate, psychosocial care plan present when indicated that include resident specific interventions based upon assessment findings; any noted suicidal ideation as indicated.
11. Monthly review of completed weekly risk review and angle rounds results and trends will be completed by the Administrator or designee and reported to the QAPI committee for the next three months and then re-evaluate to determine if further monitoring is indicated.
12. Residents identified with a change in elopement risk or who have had an actual elopement attempt will be reviewed during routine risk meeting by clinical interdisciplinary team. Review will be documented in the resident electronic medical record.
13. Routine elopement drills scheduled per community policy on varying shifts to confirm staff competency.
14. Findings of elopement drills are to be reported to the community Administrator and reviewed at the following morning meeting. If discrepancies are identified immediate correction will be completed and one on one education provided as indicated.
Due to the corrective actions the facility completed prior to the onsite visit, the deficient practice was deemed past non-compliance and existed at a J scope and severity.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0553
(Tag F0553)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility reported a census of 96 residents, that included 20 residents included in the sample. Based on interview and record...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility reported a census of 96 residents, that included 20 residents included in the sample. Based on interview and record review, the facility failed to include Resident (R)61 in the development and planning of the resident's care plan quarterly, which placed R81 at risk of impaired care and autonomy.
Findings included:
- Resident (R)61's Electronic Medical Record (EMR) documented diagnosis that included acute kidney failure, Human immunodeficiency virus (HIV is a virus that attacks cells that help the body fight infection, making a person more vulnerable to other infections and diseases) and muscle weakness.
The admission Minimum Data Set(MDS) dated [DATE], documented R61 had a Brief Interview for Mental Status (BIMS) score of 15, indicating intact cognition. R61 had verbal behavioral symptoms four to six days, but less than daily during the look-back period. It was somewhat important to have family, or a close friend involved in discussions about his care. He required staff assistance with activities of daily living (ADL). He had occasional incontinence of bladder. He had obvious or likely cavity or broken natural teeth. R61 had moisture associated skin damage (MASD) and used a pressure reducing device for his chair and bed. Section Q of the MDS documented participation in assessment and goal setting checked as resident participation.
The Care Area Assessment (CAA) triggered for Cognitive loss/dementia, ADL Functional/Rehabilitation Potential, Urinary Incontinence and Indwelling Catheter, Psychosocial well-being, Behavioral symptoms, Nutritional Status, Dehydration/Fluid Maintenance, Dental care, and Pressure ulcer(localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction).
The quarterly MDS, dated [DATE], documented R61 had a BIMS of 15, indicating intact cognition.
The quarterly MDS, dated [DATE], documented R61 had a BIMS of 15, indicating intact cognition.
The care plan documented the resident had a potential psychosocial well-being problem and guided staff to provide opportunities for the resident and family to participate in care, dated 12/13/24.
Review of the EMR revealed on 10/18/23 Interdisciplinary care conference notes, revealed the resident and the MDS staff attended the care plan conference. The EMR lacked documentation of any further attendance or invitation to discuss his care plans.
On 07/30/24, R61 reported he had never been given the opportunity to participate in his care plan, and he felt it was important to be in on the care plan.
On 07/31/24 at 03:59 PM, Social services staff X reported staff should give residents the opportunity to go to their care plan. Staff should document in the social service note if the resident attended or did not attend.
On 07/31/24 at 04:16 PM, Administrative Nurse E reported staff should invite R61 to his care plan and verified the facility lacked documentation in his EMR whether he was invited or if he chose to come/refuse his care plan meeting.
On 08/01/24 at 11:36 AM, Administrative Staff A reported it is the expectation of the facility staff to give a notice of the care plan to the resident on the day of the care plan meeting. If a resident would like to participate in the care plan meeting, staff would review and verify information including code status, diet, transfers, and such. The facility had care plan meetings generally every Tuesday.
The facility's undated policy for Care Plan Meeting, documented Federal law provides that, to the extent possible, the resident, the resident's family, or the resident's legal representative should participate in the care plan meeting. It is important to provide plenty of notice and multiple options for their participation (i.e telephone conference, virtual meeting, or in-person). An Interdisciplinary Care Conference Notes Assessment should be completed during the care plan meeting.
The facility failed to include Resident (R)61 in the development and planning of the resident's care plan quarterly, which placed R81 at risk of impaired care and autonomy.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** -Resident (R) 54's Electronic Health Record (EHR) revealed diagnoses that included dementia (progressive mental disorder charact...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** -Resident (R) 54's Electronic Health Record (EHR) revealed diagnoses that included dementia (progressive mental disorder characterized by failing memory, confusion) and muscle weakness.
The 05/28/24 Annual Minimum Data Set (MDS) documented a Brief Interview for Mental Status (BIMS) score of 14, indicating intact cognition. R54 had a total mood severity score of 00, indicating no depression and there were no behaviors documented on the assessment.
The 07/23/24 Quarterly MDS documented a BIMS score of 14. No behaviors. R54 was independent with ADLs, except set-up for shower.
The Care Plan documented R54 wanted take care of his personal belongings dated, 07/06/20.
Review of the Progress Notes from 01/01/24 to 07/30/24 lacked any notes regarding missing personal property.
On 07/30/24 at 09:27 AM, R54 stated his topcoat required new buttons and dry cleaned. He stated that Social Service Staff X assisted with that task. R54 stated his topcoat had been missing for a couple of months and had requested to have it returned. He stated as he threw both of his arms up in the air looking frustrated that he had spoken to Administrative Staff A and Social Service Staff X a few times with no return of his coat.
On 07/31/24 at 12:53 PM, Administrative Staff A stated he was not aware of R54 missing a topcoat. Administrative Staff A stated that R54 was very particular of all his personal items and that R54 had assistance with his dry cleaning of an un-named person.
On 07/31/24 12:55 PM, Social Service Staff X stated that R54 informed her yesterday that his topcoat had been missing since it was taken for dry cleaning.
On 08/01/24 at 02:00 PM, Administrative Staff A revealed that R54's topcoat had been located by Social Service X and brought back the topcoat from the dry cleaners. He stated the buttons were not replaced, but the topcoat was cleaned.
On 08/01/24 at 02:30 PM, Social Service Staff X confirmed she returned R54's topcoat. However, she could not recall when she received R54's coat to have it dry cleaned.
The facility lacked a policy on personal property.
The facility failed to ensure (R)54 received his personal property back in a timely manner. This deficient practice placed the resident at risk for decreased psychosocial well-being.
The facility reported a census of 96 residents. The sample included 20 residents with four residents selected for review related to resident rights to retain and use of their personal possessions. Based on observation, interview , and record review, the facility failed to ensure the resident right to retain and use her personal possessions for Resident (R)63 related to her motorized wheelchair and R 54's missing coat.
Findings included:
- Review of Resident (R)63's Physician Orders, dated 07/09/24 documentation included diagnoses of diabetes (when the body cannot use glucose, not enough insulin made or the body cannot respond to the insulin), cellulitis (skin infection) of left lower limb, chronic obstructive pulmonary disease, (COPD- progressive and irreversible condition characterized by diminished lung capacity and difficulty or discomfort in breathing), anxiety disorder (mental or emotional reaction characterized by apprehension, uncertainty and irrational fear), depressive disorder (a mood disorder that causes a persistent feeling of sadness and loss of interest) and generalized muscle weakness.
The admission Minimum Data Set (MDS) dated [DATE], documentation included a Brief interview for Mental Status, (BIMS) score of 14, indicating cognitively intact. She did not exhibit any behaviors but reported little interest or pleasure in doing things, feeling down, depressed, hopeless, and feeling tired or having little energy. Additionally, the resident stated taking care of her personal belongings, going outside when the weather was good, and participation in her favorite activities were very important. She did not smoke. The resident used a manual wheelchair as a mobility device and noted as independent with wheeling her wheelchair for 150 feet. She received application of ointments (treatment medications) and dressings to manage skin problems to her feet and other than her feet. She received schedule and prn (as needed) pain medication. The resident reported moderated pain and experienced one non-injury fall.
The Functional Abilities (Self-Care and Mobility) Care Area Assessment (CAA) and Psychosocial Wellbeing CAA dated 06/05/24, documentation included respectively the resident required staff assistance with daily care needs, transfers, and mobility for proper completion and safety as needed to avoid complications and minimize risks related to psychosocial wellbeing.
The Care Plan, dated 06/05/24, directed staff the resident had mood problem related to depression
and anxiety. Staff were to monitor/record/report to the physician as needed episode of feelings sadness, loss of pleasure, and interest in activities.
Review of R 63's electronic medical record (EMR), Social Service Progress Note (PN) dated 0/31/24 at 07:24 PM, documentation included Social Service staff X talked to the administrator and asked if R 63 had a motorized scooter in the building. Administrative Staff A referred Social Service Staff X to maintenance to see if the electric chair was located in the building. The maintenance reported to Social Service staff X, that three weeks prior, R 63's previous care facility delivered her electric wheelchair to the current facility and had been stored at the facility. The EMR lacked documentation the resident had been notified of the delivery and/or the location of her wheelchair.
On 07/30/24 at 11:50 AM, Resident (R)63 sat in a manual wheelchair. She had kerlex wraps (type of bandage) on her legs . She was alert, oriented, and identified herself as a resident that smoked. She stated she had to use her manual wheelchair to navigate the hallway to the smoking area at the courtyard off of the 100 hall. The resident reported she had a diagnoses which included diabetes and wounds on her legs, and she could not use her feet to self- propel her wheelchair. She had to use her hands to propel the wheelchair to the smoking area which was a long way from her room (approximately 300 feet away from the resident's room). R 63 reported the facility had designated smoking times and by the time she self-propelled her wheelchair to the designated area, she was exhausted and could not use her full-time smoking. R 63 started crying and stated she had an electric wheelchair she had bought with her own money that had been delivered to the facility and she did not know where it was. She reported the electric wheelchair would help her to be able to attend her favorite activities and be more independent. No one at the facility had let her know the electric wheelchair was at the facility. On inquiry, R 63 reported no one had set up an assessment to determine if she could safely operate the electric wheelchair. However, she knew the facility allowed electric wheelchairs because other residents in the facility used them. She stated she knew the electric wheelchair had been delivered to the facility because she had checked on it.
On 07/31/24 at 11:59 AM, Social Service Staff X stated she was not aware of the resident having an electric wheelchair at the facility and/or needing an electric wheelchair assessment to determine her ability to operate the wheelchair safely. She agreed the residents had a right to retain and use their personal possessions. Social Service Staff X reported she would follow-up with the facility Administrator and or maintenance staff to investigate the resident's electric wheelchair location.
On 07/31/24 at 02:37 PM, Certified Nurse Aide M stated she was not aware the resident had an electric wheelchair at the facility. The resident could self-transfer to her wheelchair, and she would not get as tired with an electric wheelchair.
On 08/05/24 at 03:00 PM, Administrative Staff A confirmed the above findings. Additionally, he reported the resident did not have access to or use of her electric wheelchair while it was in storage.
The facility lacked a policy for Resident Rights, related to the resident's right to retain and use personal property.
The facility failed to ensure the resident right to retain and use her personal possessions related to her motorized wheelchair.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
The facility reported a census of 96 residents with three residents reviewed for Medicare Advance Beneficiary and Medicare Non-Coverage Notices. Based on record review and interview, the facility fail...
Read full inspector narrative →
The facility reported a census of 96 residents with three residents reviewed for Medicare Advance Beneficiary and Medicare Non-Coverage Notices. Based on record review and interview, the facility failed to notify one resident, Resident (R)22, ABN (provides information to beneficiaries so that they can decide if they wish to continue receiving the skilled services that may not be paid for by Medicare and assume financial responsibility before the end of a Medicare covered Party), or a NOMNC (a form given to all Medicare beneficiaries at least two days before the end of a Medicare covered part A stay or when all of Part B therapies are ending), as required.
Findings included:
- On 07/30/24, Administrative staff A provided a list of discharged Medicare A residents with three residents chosen for review. One Resident, (R)22, identified as discharged from Part A services on 03/23/24, lacked a NOMNC or ABN completed when Medicare Part A services were terminated to let the resident know how many days of the 100 days available remained. The skilled nursing facility (SNF) Beneficiary Notification Review form (Form Centers for Medicare/Medicaid services [CMS]-20052) had R22's name on the top. The CMS 20052 form determined if the Medicare Part A Services termination/discharge determined if voluntary, if the facility/provider initiated the discharge from Medicare Part A services when benefit days were not exhausted, or other (and staff could explain). The yes/no boxes were blank to answer if the SNF ABN, Form CMS-10055 provided to the resident. The yes/no boxes were blank to answer if a NOMNC, Form CMS-10123 provided to the resident. The facility lacked a completed CMS-10555 form and lacked a completed CMS 10123-NOMNC form.
On 08/06/24 at 08:57 AM, Administrative Staff B reported she was unable to locate R22's forms. Administrative staff B stated the procedure was for the facility to issue a NOMNC and or ABN three days before discharge.
The facility failed to provide a policy regarding Beneficiary Notice as requested on 0/05/24.
The facility failed to provide R1 forms on ABN, and NOMNC three days before discharge, as required.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
The facility had a census of 96 residents. The sample included 20 residents. Based on observation, interview
and record review, the facility failed to provide consistent activities for two residents....
Read full inspector narrative →
The facility had a census of 96 residents. The sample included 20 residents. Based on observation, interview
and record review, the facility failed to provide consistent activities for two residents. Resident (R)41 and R82 were observed not to have received activities on the Memory Care Unit. This deficient practice placed the residents at risk for complications related to decreased psychosocial wellbeing.
Findings included:
- The 04/14/24 Annual Minimum Data Set (MDS), documented a Brief Interview for Mental Status (BIMS) score of 00, which indicated severely impaired cognition. R41 had a total mood severity score of 00, indicating no depression and there were no behaviors documented. R41 required maximal assistance with activities of daily living, which included toileting, dressing, and bathing. R41 was frequently incontinent of bladder. The resident had no falls. R41 stated it was very important to do her favorite activities in section F activity interview.
The Cognition Loss/Dementia Care Area Assessment (CAA) dated 04/14/24, documented R41 was alert with impaired memory function. Staff to proceed to care plan with continued assistance with daily decisions and tasks to avoid complications and minimize risks.
The 07/14/24 Quarterly Minimum Data Set (MDS), documented a BIMS score of one, which indicated severely impaired cognition. R41 had no depression or behaviors. R41 required maximal assistance with activities of daily living, which included toileting, dressing, and bathing. R41 was frequently incontinent of bladder. The resident had no falls.
The Care Plan dated 04/03/24, lacked any activity preferences.
The Physician's Order documented activities as tolerated unless contraindicated date ordered, 04/01/24.
Review of the Progress Notes from 04/01/24 to 07/30/24 lacked any activity notes for attendance or activity assessment.
On 07/30/24 at 10:58 AM, family member stated that he is not sure if R41 attended activities. He stated when he arrived, she was seated in the lounge and the television was on.
On 07/31/24 at 11:15 AM, Activity Staff Z stated she was responsible for the entire facility activity department. Stated that she has a part time staff member that is scheduled on Thursday and Friday every week. Activity Staff Z revealed a new full time activity employee was recently hired and should start soon. She confirmed that the activities for the Memory Care Units need to be improved and relied on the Certified Nurse Aides (CNA) to provide residents with the activities posted on monthly calendar.
On 07/31/24 at 12:20 PM, R41 was seated in a chair in the main dining room next to her family member eating her dessert.
On 08/01/24 at 09:50 AM, R41 was seated on the couch in lounge and television was on a news channel.
On 08/01/24 at 11:01 AM, R41 was seated on the couch in lounge and television was on a news channel.
On 08/01/24 at 11:01 AM to 01:40 PM, no activities observed on the women's memory care unit.
On 08/01/24 at 11:01 AM, observed no activity noted on unit in lounge. A posted activity calendar in the unit dining room documented 07:30 AM, Breakfast, 11:00 AM, EnerG, 11:30 AM Lunch, 02:00 PM Bingo in the main dining room, and 05:30 PM Dinner.
On 08/01/24 at 11:28 AM, Certified Medication Aide (CMA) R stated he did not provide activities on the monthly calendar, stated that he would hand out coloring supplies to some residents.
On 08/01/24 at 01:01 PM, CNA OO stated that she did not understand the activity named EnerG that was scheduled on the calendar. CNA OO stated she has not observed activities on the memory care unit for a while. She stated the part time activity staff member should be completing the activities. She stated that she will occasionally do some of the residents' fingernails.
On 08/05/24 at 03:00 PM, Administrative Staff A stated that activities were extremely important for all the residents. He stated that a full- time activity staff member had been hired and would be starting soon. Furthermore, that position had been vacant for about three months. Administrative Staff A confirmed that the CNAs should provide activities and confirmed the above findings.
The facility lacked a policy on providing activities.
The facility failed to provide consistent activities. This deficient practice placed the resident at risk
for complications related to decreased psychosocial wellbeing.
- The Electronic Health Records (EHR) documented Resident (R)82 had the following diagnoses that included dementia (progressive mental disorder characterized by failing memory, confusion), muscle weakness and unsteadiness on feet.
The 02/15/24 Annual Minimum Data Set (MDS), documented a Brief Interview for Mental Status (BIMS) score of 01, which indicated severely impaired cognition. R82 had a total mood severity score of 00, indicating no depression and there were no behaviors documented. R82 required moderate assistance with activities of daily living, which included toileting, dressing, transfers, and bathing. R82 was always incontinent of bladder. R82 had two non-injury falls.
The Cognition Loss/Dementia Care Area Assessment (CAA) dated 02/15/24, documented R82 alert with impaired memory function, dementia with poor decision skills and safety awareness. Staff to proceed to care plan with continued monitoring and assistance with decisions and tasks for proper completion and safety and to avoid complications and minimize risks with referral to physician as indicated.
The 05/17/24 Quarterly Minimum Data Set (MDS), documented a BIMS score of one, which indicated severely impaired cognition. R82 had no depression or behaviors. R82 required moderate assistance with activities of daily living, which included toileting, dressing, transfers, and bathing. R82 had no falls.
The Care Plan reviewed on 07/31/24, revealed R82 had activity preferences dated 02/09/23. Staff were provided with R82's preference and documented R82 liked jazz and Christian music, she liked animals, word games, painting, and liked to watch movies that were in Spanish.
The Physician's Order documented activities as tolerated unless contraindicated, date ordered 02/09/23.
Review of the Progress Notes from 04/01/24 to 07/30/24 documented the following:
On 05/13/24 at 05:13 PM, R82 met with activity director for a quarterly review and completed a nail spa activity with R82.
On 07/01/24 at 05:10 PM, R82's family was contacted and obtained R82's activity preferences. Family member stated that R82 enjoyed knitting, painting, and liked to go outside for fresh air.
On 07/31/24 at 11:15 AM, Activity Staff Z stated she was responsible for the entire facility activity department. Stated that she has a part time staff member that is scheduled on Thursday and Friday every week. Activity Staff Z revealed a new full time activity employee was recently hired and should start soon. She confirmed that the activities for the Memory Care Units need to be improved and relied on the Certified Nurse Aides (CNA) to provide residents with the activities posted on monthly calendar.
On 08/01/24 at 09:48 AM, R82 was seated in her wheelchair facing a wall.
On 08/01/24 at 11:01 AM, R82 was seated in her wheelchair facing a wall, R82 had a patio door window on her right side that she would look out at times.
On 08/01/24 at 11:01 AM, observed no activity noted on unit in lounge. A posted activity calendar in the unit dining room documented 07:30 AM, Breakfast, 11:00 AM, EnerG, 11:30 AM Lunch, 02:00 PM Bingo in the main dining room, and 05:30 PM Dinner.
On 08/01/24 at 11:01 AM to 01:40 PM, no activities observed on the women's memory care unit.
On 08/01/24 at 11:28 AM, Certified Medication Aide (CMA) R stated he does not provide activities on the monthly calendar, stated that he would hand out coloring supplies to some residents.
On 08/01/24 at 01:01 PM, CNA OO stated that she did not understand the activity named EnerG that was scheduled on the calendar. CNA OO stated she has not observed activities on the memory care unit for a while. She stated the part time activity staff member should be completing the activities. She stated that she will occasionally do some of the residents' fingernails.
On 08/05/24 at 03:00 PM, Administrative Staff A stated that activities were extremely important for all the residents. He stated that a full time activity staff member had been hired and would be starting soon. Furthermore, that position had been vacant for about three months. Administrative Staff A confirmed that the CNAs should provide activities and confirmed the above findings.
The facility lacked a policy on providing activities.
The facility failed to provide consistent activities. This deficient practice placed the residents at risk
for complications related to decreased psychosocial wellbeing.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility reported a census of 96 residents with 20 residents in the sample, that included one resident reviewed for dialysis...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility reported a census of 96 residents with 20 residents in the sample, that included one resident reviewed for dialysis (procedure where impurities or waste were removed from the blood). Based on observation, interview, and record review, the facility failed to ensure staff obtained vital signs or the dialysis site after Resident (R)81 received dialysis (procedure where impurities or waste were removed from the blood).
Findings include:
- The Physician Orders dated 04/01/24 revealed the following diagnosis for Resident (R) 81 diabetes mellitus (when the body cannot use glucose, not enough insulin made, or the body cannot respond to the insulin) end stage renal disease (a terminal disease because of irreversible damage to vital tissues or organs).
The Significant Change Minimum Data Set (MDS) dated [DATE] revealed a Brief Interview for Mental Status (BIMS) score of 14, indicating intact cognition. Review of the functional abilities and goals indicated R 81 required substantial/maximal assistance impairment of upper and lower extremities. R81 used a wheelchair for mobility.
The Quarterly (MDS) dated [DATE], revealed no changes in memory or abilities.
The Care Plan revised on 08/16/23, revealed R81 required dialysis every Tuesday, Thursday, and Saturday due to end stage renal failure. The Chair time was 05:15 AM. The dialysis access double lumen catheter was in R81's left upper chest. Staff was to ensure the resident's dialysis book was sent with R81 to each session. Staff were to monitor when R81 returned for any new orders, communication, or information sent back with her. Staff were to monitor/document/report to the physician as needed of any signs or symptoms of infection or bleeding to the access site. Staff were to obtain vital signs (blood pressure, pulse, temperature, and respirations) and report significant changes immediately.
Review of the Dialysis Book forms from 08/07/23 to 07/30/24 revealed the facility lacked documentation of post dialysis vital signs, and nurses' signature on 62 occasions.
On 08/05/24 at 08:40 AM, Licensed Nurse (LN) K reported he would document the vitals in the Electronic Medical Record (EMR), but not necessary on the dialysis form.
On 08/05/24 at 11:54 AM, Administrative Nurse D reported staff does not remove the dialysis book out of R18s wheelchair when she returns from dialysis. The nurses are to document on the dialysis forms and document a progress note, if it is not documented it was not done.
The facilities policy Dialysis Communication dated 01/2017 revealed the policy of the facility to communicate openly and effectively with any provider or dialysis for a resident of the facility. A dialysis communication form will be used to send information to and from the facility to the dialysis center and back. Upon return of the residents from the dialysis center, the nurse in charge of the resident will review the communication form and will obtain necessary post dialysis information. The nurse will compete post dialysis information on the dialysis communication form the form will be scanned into the electronic medical record and communicate any significant information (complications or concerns) to the medical practitioner and or representative.
The facility failed to ensure the staff obtained vital signs after R81 returned from dialysis to ensure stability for adverse reactions to the dialysis procedure.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility reported a census of 96 residents, that included 20 residents included in the sample. The sample included six resid...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility reported a census of 96 residents, that included 20 residents included in the sample. The sample included six residents for unnecessary medications. Based on observation, interview, and record review, the facility failed to ensure Resident (R)61's medication was available for administration without missed doses. This deficient practice placed R61 at risk of unnecessary complications from not receiving his medication, as ordered by the physician.
Findings included:
- Resident (R)61's Electronic Medical Record (EMR) documented diagnosis that included Human immunodeficiency virus (HIV is a virus that attacks cells that help the body fight infection, making a person more vulnerable to other infections and diseases).
The admission Minimum Data Set(MDS) dated [DATE], documented R61 had a Brief Interview for Mental Status (BIMS) score of 15, indicating intact cognition.
The care plan, revised on 01/04/24, documented staff were to administer HIV medications as ordered.
The physician's orders included Abacavir Sulfate- lamivudine, 600-300 mg, daily at bedtime, for HIV, ordered 09/26/24.
Efavirenz, 600 milligrams, at bedtime, for antiretroviral, ordered 09/26/24.
Review of the Medication Administration Record (MAR) from 06/01/24 to 07/31/24, revealed marked 5, indicated to see progress notes. However, the progress notes lacked notes related to why the medication was on hold.
Review of the nurse notes on 07/30/24, revealed the resident was out of Efavirenz and Abacavir Sulfate-Lamivudine. Resident wants both medications taken together. Efavirenz was not available as it was on order. Staff told R61 that one of the medications was not available but may be delivered at midnight.
On 07/30/24 at 11:28 AM, R61 reported he doesn't always get his medications as ordered.
On 08/01/24 at 01:13 PM, Administrative Nurse D reported medications should be made available. Staff should check the medications, and if there was only a seven-day supply left, staff should reorder the medication. Staff should not wait until it runs low to be contacting the pharmacy. If the medication was on backorder from the manufacturer, staff should have contacted R61's physician for further guidance. Administrative Nurse D verified staff failed to notify the physician for further guidance when R61 was out of his medication.
The facility's undated policy for Medication availability, documented refills ordered timely through the electronic health records (EHR) or by pulling stickers. Refills should be ordered when a 3-day supply of medication remain. Not all medications are auto received, must check and clear the Waiting to be Received queue in (computer software) Medication administration audit report run every day during clinical meeting, follow up to be done immediately. If medication not available, staff to check emergency drug kit for medication, staff to call the pharmacy if the medication was not in the emergency drug kit, notify the director of nursing, and notify the practitioner.
The facility failed to ensure Resident (R)61's medication was available for administration without missed doses. This deficient practice placed R61 at risk of unnecessary complications from not receiving his medication, as ordered by the physician.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
The facility had a census of 96 residents. The sample included 20 residents. Based on observations, interview and record review, the facility failed to honor a food preference for Resident (R)41. Staf...
Read full inspector narrative →
The facility had a census of 96 residents. The sample included 20 residents. Based on observations, interview and record review, the facility failed to honor a food preference for Resident (R)41. Staff served R 41 pork when documented on her meal ticked as no pork. This deficient practice placed the resident at risk for inadequate care and services.
Findings included:
- The 04/14/24 Annual Minimum Data Set (MDS), documented a Brief Interview for Mental Status (BIMS) score of 00, which indicated severely impaired cognition. R41 had a total mood severity score of 00, indicating no depression and there were no behaviors documented. R41 required staff to set-up her meals.
The Cognition Loss/Dementia Care Area Assessment (CAA) dated 04/14/24, documented R41 alert with impaired memory function. Staff to proceed to care plan with continued assistance with daily decisions and tasks to avoid complications and minimize risks.
The Care Plan dated 07/15/24, documented no pork products or shellfish per R41's preference.
The Physician's Order documented regular diet, no pork or shellfish products, ordered 04/01/24.
Review of the Progress Notes from 04/01/24 to 07/30/24 lacked any documentation for food preferences.
On 07/30/24 at 11:13 AM, R41's family member stated that R41 had a preference to not eat pork products or shellfish. He stated that R41 had received a salami sandwich a couple of days ago and had to remind staff again.
R41's family member stated that her preference for no pork products or shellfish had been discussed when she was admitted in April 24.
On 08/01/24 at 12:20 PM, staff served R41 a bowl of ham and bean soup. R41's family member addressed the concern with Certified Nurse Aide (CNA) OO.
On 08/0124 at 12:21 PM, CNA OO showed the surveyor R41's daily paper meal ticket, which clearly had NO PORK written on the bottom of the ticket. She stated that she wrote that on the meal ticket then delivered the meal tickets to the kitchen.
08/01/24 at 12:26 PM, Dietary Staff CC entered the dining room with a bowl of tomato soup and apologized to R41's family member. Dietary Staff CC stated that R41 would eat sausage at breakfast, and she did not have an issue with that. Dietary Staff CC then asked if R41 had an allergy to pork. R41's family member stated that R41 preferred to not eat pork products or shellfish and had mentioned that concern in the past. Dietary Staff CC stated he remembered the no shellfish, but not the no pork products and apologized once again. Dietary Staff CC confirmed R41 had no pork written on her meal ticket and stated that it was missed. He stated that a new computer system that printed out the meal tickets had an issue to print out the extra comments that staff are used to observing during the meal line prep.
On 08/01/24 at 02:45 PM, Administrative Staff A confirmed the concern above and stated that was unacceptable.
The facility lacked a policy on food preferences.
The facility failed to honor a food preference for Resident (R)41. R41 was served a food item that was recorded as a no pork on her meal ticket. This deficient practice placed the residents at risk for inadequate care and services.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** - The Physician Orders dated 04/01/24 revealed the following diagnoses for Resident (R) 81 had diagnoes that included diabetes m...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** - The Physician Orders dated 04/01/24 revealed the following diagnoses for Resident (R) 81 had diagnoes that included diabetes mellitus (when the body cannot use glucose, not enough insulin made, or the body cannot respond to the insulin) and end stage renal disease (a terminal disease because of irreversible damage to vital tissues or organs).
The Significant Change Minimum Data Set (MDS) dated [DATE] revealed a Brief Interview for Mental Status (BIMS) score of 14, indicating intact cognition. Review of the functional abilities and goals indicated R 81 required substantial/maximal assistance with bathing.
The Quarterly MDS dated 06/12/24 revealed no changes in memory or abilities.
Review of the Care Plan dated 05/07/23 regarding Care/Activities of daily living (ADL) preferences indicated R 81 preferred a shower two times a week as tolerated, revised on 12/02/23. The care plan lacked which days/time R81 preferred to have her bath completed per her choice.
Review of the bathing sheets for May 2024, indicated R81 received a bath/shower three days out of 31 days.
Review of the bathing sheet for June 2024, indicated R81 received a bath/shower five days out of 30 days.
Review of the 30 days look back period for July 2024, revealed a bath/shower R81 received five days out of 31 days.
On 07/31/24 at Interview with Administrative Nurse D confirmed resident's bathing master schedules are by room number and divided between first and second shift. She stated if a resident has a preference their preference for time, type and frequency of bath should be respected.
The facility failed to provide a policy regarding Bathing/ Preferences as requested on 08/05/24
The facility failed to provide R 81 with preference choices for bath days and times of her bathing.
The facility reported a census of 96 residents. The sample of 20 residents included five dependent residents reviewed for choices/preferences related to bathing. Based on observation, interview, and record review, the facility failed to provide choices related to the resident's bathing preferences for four Residents (R)92, 73, 74, 81 related to bathing.
Findings included:
- Review of Resident (R) 92's undated Physician's Orders, documentation included diagnoses of spastic hemiplegia (paralysis of one side of the body) and hemiparesis (muscular weakness of one half of the body) affecting left dominate side, and memory deficit following cerebral infarction ([CVA] stroke - sudden death of brain cells due to lack of oxygen caused by impaired blood flow to the brain by blockage or rupture of an artery to the brain).
The admission Minimum Data Set (MDS) dated [DATE], revealed a Brief Interview for Mental Status (BIMS) score of 14, indicating cognitive intact. R92 did not exhibit behaviors. He reported it was very important to choose the type of bath he preferred. The resident had impairment of his lower extremity on one side of his body and required substantial/maximal assistance of staff with bathing.
The Functional Abilities Self-Care Mobility Care Area Assessment (CAA) dated 06/14/24, documentation included a recent history of CVA with hemiparesis. The resident required assistance with daily cares and mobility. The facility staff would proceed to care plan with continued active participation in rehabilitation services for improvement and staff assistance as needed to avoid complications and minimize risks related to functional abilities.
The Care Plan, dated 08/01/24, directed staff the resident required staff participation with bathing, check nail length, trim, and clean on bath days as necessary. The care plan lacked direction to staff related to the residents bathing schedule and/or preferences.
On 07/30/24 at 09:22 AM, upon entering the resident's room, there was a stale musky odor. He laid in the bed. His hair was stringy and oily, and the hair stuck to his head. His overall appearance was unkept. The resident reported he thought his last shower a week ago. He stated he had been a resident for over a month and the facility staff told him he could only have a bath on Mondays. He did not get a bath yesterday (Monday, 07/29/24). Additionally, he reported he had an appointment the next day and did not want to be stinking when he went. The resident stated he would prefer a bath at least two times a week if he could not get one every day. He reported that less than weekly was not acceptable, he did not care what time of day, he just wanted a bath of some type.
Review of the facility's Shower List schedule documentation revealed residents were scheduled based on room numbers. R 92's room number was scheduled for a shower on Mondays and Thursdays during the evening shift.
Review of R 92's electronic medical record (EMR) for the 30 days prior to the resident's interview revealed the resident received a bath on three occasions in the previous 30 days. Bathing documented on 07/11/24, 07/15/24, and 07/25/24. The EMR documentation lacked indication the staff offered the bathing opportunities and if the resident refused.
On 07/31/24 at 11:10 AM, Social Service Staff X reported multiple residents have filed grievances and reported concerns regarding not receiving baths/showers in keeping with their preferences or past routine. She reported she forwarded those concerns to the administrative nurses for address and follow-up.
On 07/31/24 at 02:29 PM, Certified Nurse Aide (CNA) M reported residents should get a minimum of two baths/showers a week and more if they prefer. Residents should have bathing scheduled when they want their bathing done morning or evening, as well as the type of bath/shower they prefer. She reported the resident's preferences and schedule should be in the care plan. Some residents want a bath/shower one or two times a week while others want one every day. The staff should accommodate their preferences. If the residents refuse their bath/shower, staff should let the MDS coordinator know and document in the EMR the refusal. Their bathing should include nail care. CNA M reported when she came in to work this morning, she gave R 92 a bath and dressed him because he requested a bath because he was going to the doctor, and he said he did not get his bath on Monday or Tuesday as he had requested.
On 08/01/24 at 02:53 PM, Licensed Nurse (LN)H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Staff should document refusals in the EMR. Bathing preferences and schedules should be documented in the resident's care plan. Nail care should be provided by staff with bathing and as needed.
On 08/05/24 at 10:37 AM, Administrative Nurse D confirmed the facility's master schedule titled Shower List, was the facility's master schedule assigned day and time of shower based on the resident's room number rather than the resident's preferences. The Shower List schedule was not based on the resident's preferences and choices. She stated if a resident had a preference, their preference for time, type, and frequency of bath should be respected and accommodated. Administrative Nurse D stated the facility staff should obtain resident's preferences on admission and would expect the staff to adjust the resident's schedule accordingly. She confirmed R92's bathing documentation did not reflect his being offered a bathing opportunity at least two times a week or his refusal of any bathing opportunity. She verified his care plan lacked direction to the staff regarding his preferences, for type, frequency, and time of his bathing.
The facility lacked a policy to address the resident's bathing, preferences, and scheduling.
The facility failed to provide choices and accommodate the resident's preferences/choices related to the resident's bathing.
- Review of Resident (R)74's Physician's Orders, dated 07/27/24, documentation included diagnoses of Alzheimer's Disease (disease (progressive mental deterioration characterized by confusion and memory failure), behavioral disturbances, palliative (end of life) care, type 2 diabetes (DM-when the body cannot use glucose, not enough insulin made or the body cannot respond to the insulin), and depression (a mood disorder that causes a persistent feeling of sadness and loss of interest).
The Significant Change in Status Minimum Data Set (MDS) dated [DATE], revealed a Brief Interview for Mental Status (BIMS) score of 03, indicating severe cognitive impairment. The resident exhibited inattention and disorganized thinking continuously. The resident had no rejection of care. No functional impairment in range of motion of upper or lower extremities. He was dependent on staff for activities of daily living (ADL) care (bathing and personal hygiene). The resident received Hospice services. He reported choosing the type of bath preferences as very important.
The Cognitive Loss/Dementia Care Area Assessment (CAA) dated 07/12/24, documented the resident alert with impaired memory function, poor decision skills and safety awareness.
The Care Plan dated 07/12/24, directed staff the resident required limited to extensive assistance of one staff with grooming. Staff should assist with showering twice weekly and as needed. She refused bathing at times. The care plan lacked address of the resident's bathing and personal hygiene schedule, or preferences/choices related to his bathing, and personal hygiene.
On 07/30/24 at 12:44 PM, R 74 laid in bed with long jagged fingernails that extended well over one-half inch beyond the tips of her fingers. There was black substance packed beneath each of his fingernails. He had an unkept appearance with a lingering stale urine odor.
On 07/30/24 at 04:51 PM, R 74 continued to have long jagged fingernails that extended well over one-half inch beyond the tips of her fingers. There was black substance packed beneath each of her fingernails.
Review of the facility's Shower List schedule documentation revealed residents were scheduled based on room numbers. R 74's room number was scheduled for a shower on Wednesdays and Saturdays during the day shift.
Review of R 74's electronic medical record (EMR) for the 30 days prior to the resident's interview revealed the resident received a bath on two occasions in the previous 30 days on 07/08/24 and 07/11/24. The EMR documentation lacked indication the staff had offered the bathing opportunities which she refused. No documentation of nail care or refusals of offered nail care noted.
On 07/31/24 at 02:29 PM, Certified Nurse Aide (CNA) M reported residents should get a minimum of two baths/showers a week and more if they prefer. Residents should have bathing scheduled when they want their bathing done morning or evening, as well as the type of bath/shower they prefer. She reported the resident's preferences and schedule should be in the care plan. Some residents want a bath/shower one or two times a week while others want one every day. The staff should accommodate their preferences. If the residents refuse their bath/shower, staff should let the MDS coordinator know and document in the EMR the refusal. Their bathing should include nail care. Resident's fingernails should be cleaned as needed. If residents are diabetic, their nails should be cut by the nurses, however all direct care staff can clean resident's fingernails when soiled.
On 08/01/24 at 02:53 PM, Licensed Nurse H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Staff should document refusals in the EMR. Bathing preferences and schedules should be documented in the resident's care plan. Nail care should be provided by staff with bathing and as needed. The residents that are diabetic should have their nails trimmed by the nurses.
On 08/05/24 at 10:37 AM, Administrative Nurse D confirmed resident's bathing master schedules are by room number and divided between first and second shift. She stated if a resident has a preference their preference for time, type, and frequency of bath should be respected. Administrative Nurse D stated the facility staff try to obtain resident's preferences on admission and would expect the staff to adjust accordingly. She confirmed R74's bathing documentation did not reflect his being offered a bathing opportunity at least two times a week or his refusal of any bathing opportunity. She verified his are plan lacked direction to the staff regarding his preferences, for type, frequency, and time of his bathing. She confirmed the above findings.
The facility lacked a policy to address the resident's bathing, preferences/choices, and scheduling.
The facility failed to provide choices and accommodate the resident's preferences/choices
related to the resident's bathing.
- Review of Resident (R) 73's Physician's Orders, dated 07/27/24 documentation included diagnoses of diabetes, anxiety disorder, acute kidney failure, transient ischemic attack (TIA- temporary episode of inadequate blood supply to the brain), cerebral infarction (CVA-stroke- sudden death of brain cells due to lack of oxygen caused by impaired blood flow to the brain by blockage or rupture of an artery to the brain), and non-pressure chronic ulcer (type of wound related to diabetic complications) of unspecified foot.
The Annual Minimum Data Set, (MDS) dated [DATE], revealed a Brief Interview for Mental Status (BIMS) score of eight, indicating moderate cognitive impairment. The resident had no functional limitation in range of motion of his upper or lower extremities. He had no behaviors and no rejection of care. He reported feeling down, depressed, or hopeless for two to six days of the look back period. He reported choosing the type of bath he wanted was very important to him. The resident required assistance of the staff with his activities of daily living (ADLs)( personal hygiene and bathing). He was dependent on staff assistance for ADLS and was frequently incontinent of urine and occasionally incontinent of bowel.
The Functional Abilities Self-Care and Mobility Care Area Assessment (CAA) dated 07/28/24 documentation included the resident required staff assistance for proper completion and safety to avoid complications and minimize risks.
The Care Plan dated 05/28/24, directed staff the resident required one staff participation for the resident to bathing, initiated 08/09/23. The care plan failed to direct staff on the type of assistance, type of bath and schedule for bathing the resident. Bathing preferences were not addressed on the resident's care plan.
Review of the facility's Shower List schedule documentation revealed residents were scheduled based on room numbers. R 73's room number was scheduled for a shower on Wednesdays and Saturdays during the day shift.
Review of R 73's electronic medical record (EMR) for the 30 days prior to the resident's interview revealed the resident lacked a bath on two occasions in the 30 days prior to the interview on 7/30/24 (07/08/24 and 07/11/24. The EMR documentation lacked indication the staff offered the bathing opportunities to the resident or that he had refused bathing. No documentation of offered nail care or refusals noted.
On 07/30/24 at 09:58 AM, R 73 laid in the bed. He had a stale musky odor. His hair and beard were long and oily in appearance with his general appearance as notably unkept. The resident's fingernails extended for an inch or more beyond the end of his fingertips with a black substance packed beneath his fingernails. Upon inquiry, he stated he did not move, he stayed in bed 24/7, and the staff knew where he was at and could give him a bath anytime. He reported the facility lacked a hygiene program and he had not had a bath for months. The facility had him on the schedule to receive a shower Tuesday and Saturday, first shift but they do not bath him. He stated he preferred a bed bath at least one time a week but they did not give him one. Additionally, he stated his beard and hair needed trimming, but the beautician did not come to the room to trim resident's hair or beard. He reported he could not get up because the doctor had told him not to put pressure on his feet due to the diabetic ulcer (wound resulting from diabetic complications). R 73 stated he had clippers the staff could use, but no staff would trim his beard or hair in his room. He stated no one had offered to trim or clean his nails which he found to be particularly upsetting because he ate with his hands.
On 07/31/24 at 11:10, Social Service Staff X reported the residents had expressed grievances regarding not receiving their baths and showers. She stated those grievances were forwarded to the Administrative Nursing staff for follow-up. Social Service Staff X reported she did not know how the residents' got their hair and beard trimmed if they did not go to the beauty shop. She stated she did not think the direct care staff provided that care and was not sure if the beautician went to the resident's rooms to trim their hair or bead.
On 07/31/24 at 02:29 PM, Certified Nurse Aide (CNA) M reported residents should get a minimum of two baths/showers a week and more if they prefer. Residents should have bathing scheduled when they want their bathing done morning or evening, as well as the type of bath/shower they prefer. She reported the resident's preferences and schedule should be in the care plan. Some residents want a bath/shower one or two times a week while others want one every day. The staff should accommodate their preferences. If the residents refuse their bath/shower we let the MDS coordinator know and document in the EMR the refusal. Their bathing should include nail care. Resident's fingernails should be cleaned as needed. If residents are diabetic, their nails should be cut by the nurses, however all direct care staff can clean resident's fingernails when soiled. She did not know if the beautician would go to a resident's room and trim their hair or beard.
On 08/01/24 at 02:53 PM, Licensed Nurse H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Staff should document refusals in the EMR. Bathing preferences and schedules should be documented in the resident's care plan. Nail care should be provided by staff with bathing and as needed. The residents that are diabetic should have their nails trimmed by the nurses.
On 08/05/24 at 10:37 AM, Administrative Nurse D confirmed resident's bathing master schedules are by room number and divided between first and second shift. She stated if a resident has a preference their preference for time, type, and frequency of bath should be respected. Administrative Nurse D stated the facility staff try to obtain resident's preferences on admission and would expect the staff to adjust accordingly. She confirmed R74's bathing documentation did not reflect his being offered a bathing opportunity at least two times a week or his refusal of any bathing opportunity. She verified his are plan lacked direction to the staff regarding his preferences, for type, frequency, and time of his bathing. She confirmed the above findings.
The facility lacked a policy to address the inclusion of resident's preferences for bathing, scheduling, grooming and personal hygiene, in the care.
The facility failed to provide choices and accommodate the resident's preferences related to the resident's bathing, grooming and personal hygiene.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
-Resident (R) 54's Electronic Health Record (EHR) revealed diagnoses that included dementia (progressive mental disorder characterized by failing memory, confusion) and muscle weakness.
The 05/28/24 A...
Read full inspector narrative →
-Resident (R) 54's Electronic Health Record (EHR) revealed diagnoses that included dementia (progressive mental disorder characterized by failing memory, confusion) and muscle weakness.
The 05/28/24 Annual Minimum Data Set (MDS) documented a Brief Interview for Mental Status (BIMS) score of 14, indicating intact cognition. R54 had a total mood severity score of 00, indicating no depression and there were no behaviors documented on the assessment.
The 07/23/24 Quarterly MDS documented a BIMS score of 14. No behaviors. R54 was independent with ADLs, except set-up for shower.
The Care Plan documented R54 wanted take care of his personal belongings dated, 07/06/20.
Review of the Progress Notes from 01/01/24 to 07/30/24 lacked any notes regarding missing personal property.
On 07/30/24 at 09:27 AM, R54 stated his topcoat required new buttons and dry cleaned. He stated that Social Service Staff X assisted with that task. R54 stated his topcoat had been missing for a couple of months and had requested to have it returned. He stated as he threw both of his arms up in the air looking frustrated that he had spoken to Administrative Staff A and Social Service Staff X a few times with no return of his coat.
On 07/31/24 at 12:53 PM, Administrative Staff A stated he was not aware of R54 missing a topcoat. Administrative Staff A stated that R54 was very particular of all his personal items and that R54 had assistance with his dry cleaning of an un-named person.
On 07/31/24 12:55 PM, Social Service Staff X stated that R54 informed her yesterday that his topcoat had been missing since it was taken for dry cleaning.
On 08/01/24 at 02:00 PM, Administrative Staff A revealed that R54's topcoat had been located by Social Service X and brought back the topcoat from the dry cleaners. He stated the buttons were not replaced, but the topcoat was cleaned.
On 08/01/24 at 02:30 PM, Social Service Staff X confirmed she returned R54's topcoat. However, she could not recall when she received R54's coat to have it dry cleaned.
The facility lacked a policy on personal property.
The facility failed to ensure (R)54 received his personal property back in a timely manner. This deficient practice placed the resident at risk for decreased psychosocial well-being.
The facility reported a census of 96 residents which included 28 residents that smoked. The facility Identified three designated smoking areas of the facility. Based on observation, interview, and record review, the facility failed to provide a safe, functional, sanitary, and comfortable environment for 28 residents that smoked in three of the three designated smoking areas and the service hallway the residents had travel through to the southeast smoking area that was in need of cleaning and/or repairs.
Findings Included:
- On 07/30/24 at 08:00 AM, on entrance to the facility at the Northeast entrance, noted a stale musty odor prevalent odor throughout the facility during the initial tour.
On 07/30/24 at 10:10 AM, Resident (R)54 and R 26, residents of the men's memory care unit (400 hall), were observed smoking on the courtyard adjacent to the locked unit. This area was a designated smoking area which accommodated four residents on the men's memory care unit that smoked. in the facility. Observations revealed the cigarette ashtray/tower was bent over and cracked. There were approximately 25 cigarette butts discarded on the ground of the covered patio.
On 07/30/24 at 11:30 AM, alert and oriented resident (R)63 identified herself as a resident that smoked. She stated she had to use her wheelchair to navigate the hallway to the smoking area at the courtyard off of 100 hall. She reported she had a diagnosis which included diabetes (when the body cannot use glucose, not enough insulin made or the body cannot respond to the insulin)and wounds on her legs, and she could not use her feet to self- propel her wheelchair to the smoking area, she had to use her hands to propel the wheelchair. She reported it was a long way from her room located on the west end of the facility. R 63 reported the facility had designated smoking times when they could have two cigarettes at each of the smoke breaks. She described the place the resident's smoke as dirty and in need of repair. The resident reported she had to use her hands to roll her wheelchair through the filth on the hallway and she was afraid of her legs getting infected as she got septic (infection of the blood) easily. Additionally, she reported the smoking area was not clean or maintained although the staff proved supervision at each smoke break.
On 07/31/24 at 01:28 PM, during tour of the service hallway at the southeast smoking area with Activity Staff Z, the following concerns were identified:
1. The smell of tobacco smoke was strong and lingered throughout the 100 hall.
2. An area by the vending machines lacked four floor tiles in front of drink machines.
3. There was areas of missing paint and unsealed chair rails that measured approximately 12 feet in length.
4. The ceiling had cracked sheetrock and unfinished sheet rock.
5. Two chair rails that measured approximately two inches by two feet was chipped and exposed raw wood.
6. There were six missing floor tiles and there was garbage on the floor as well as the floor had a black grime build- up throughout the hallway.
On 07/31/24 at 01:32 PM, activity staff Z verified the above findings and reported the smoking area was located off the vending area. Residents come to the area to use the vending machines to obtain snacks and refreshments. She stated there used to be two red containers that sat in the hallway that the facility did not use ,and they have been removed and it appears there were missing tiles under them. She stated she did not know why the garbage was directly on the floor behind where the two red containers were previously. She stated that should have been cleaned up when the containers were moved. Activity staff Z confirmed the identified concerns with the physical environment in the hallway which was used by the residents to access the Southeast courtyard to smoke and reported she was not aware of scheduled repairs the hallway. Multiple residents had to navigate the area to enter the smoking area.
On 07/31/24 at 01:39 PM, Administrative Staff A confirmed the above findings. He reported the facility had been under some renovations which included painting and ceiling repairs, but the hallway had not been completed. There had been two biohazardous containers outside of the biohazardous storage room down the hall that was removed due to lack of use. He verified the hallway needed cleaning and repairs.
On 07/31/24 at 01:45 PM, during a tour of the southeast courtyard/designated smoking area, adjacent to 100 hall with Administrative Staff A, identified the courtyard concrete slab with what appeared to be over 100 plus cigarette butts that covered the concrete where the residents sat to smoke and would self-propel their wheelchair to enter and exit the smoking area. Additionally, the cigarette butt disposal towers were broken and in disrepair. Administrative Staff A confirmed the findings and agreed the staff supervising the smoke breaks should have kept the area clean and the facility failed to provide a safe and comfortable environment for the residents that smoked.
On 08/01/24 at 09:59 AM, revealed the woman's memory care unit (500 Hall) courtyard which accommodated two of the 28 residents that smoked, had approximately 40 cigarette butts on the ground and under a table. This designated smoking area accommodated four of the 28 residents that smoked in the facility. Certified Medication Aide (CMA) O reported that residents on the memory care units were not allowed in the area without staff supervision.
On 08/01/24 at 10:01 AM, Administrative Staff A confirmed the findings noted on the 400 and 500 hall designated smoking area needed to be cleaned and repaired to provide a safe a, sanitary, and comfortable environment for the residents that smoked.
The undated facility policy Smoking,, documentation included all smoking will be done outside the building in the smoking area located outside the service hallway. Smoking times are monitored by staff.
The facility failed to provide a safe, functional, sanitary, and comfortable environment for 28 residents that smoked in three of the three designated smoking areas, in addition to the service hallway to the southeast smoking area needed cleaning and/or repairs.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** - Review of Resident (R) 47's electronic medical record (EMR) revealed a diagnosis of major depressive disorder (MDD- major mood...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** - Review of Resident (R) 47's electronic medical record (EMR) revealed a diagnosis of major depressive disorder (MDD- major mood disorder).
The admission Minimum Data Set (MDS), dated [DATE], documented the staff assessment for cognition revealed severe impairment. The resident received antidepressant medication (medication utilized to treat the symptoms of depression) during the assessment period. The resident did not receive hypnotic medication (a class of psychoactive drugs whose primary function is to induce sleep and to treat insomnia) during the assessment period.
The Psychotropic Drug Use Care Area Assessment (CAA), dated 03/05/24, documented the resident received antidepressant medication daily.
The Quarterly MDS, dated 05/28/24, documented the staff assessment for cognition revealed severe impairment. The resident received antidepressant and hypnotic medication during the assessment period.
The care plan, revised 05/29/24, instructed staff the resident received hypnotic medication and not to exceed the recommended dose of the medication.
Review of the resident's EMR revealed the following physician's order:
Trazodone (an antidepressant medication), 50 milligrams (mg), by mouth (po) at bedtime (HS), for insomnia, ordered 02/23/24.
On 08/05/24 at 01:21 PM, Administrative Nurse E confirmed the quarterly MDS, dated [DATE], was inaccurate. The resident had not received hypnotic medication during the assessment period.
The facility utilized the Resident Assessment Instrument (RAI) for accurate completion of the MDS's.
The facility failed to complete an accurate MDS for this resident.
- The Electronic Health Records (EHR) documented Resident (R)41 had the following diagnoses that included dementia (progressive mental disorder characterized by failing memory, confusion), muscle weakness and schizophrenia (mental disorder characterized by gross distortion of reality, disturbances of language and communication and fragmentation of thought).
The 04/14/24 Annual Minimum Data Set (MDS), documented a Brief Interview for Mental Status (BIMS) score of 00, which indicated severely impaired cognition. R41 had a total mood severity score of 00, indicating no depression and there were no behaviors documented. R41 required maximal assistance with activities of daily living, which included toileting, dressing, and bathing. R41 was frequently incontinent of bladder. The resident had no falls.
The Falls Care Area Assessment (CAA) dated 04/14/24, documented R41 was at risk for falls related to impaired cognition and use of medications which may increase risks. Staff to proceed to care plan with continued monitoring and assistance to avoid complications and minimize risk related to falls.
The 07/14/24 Quarterly Minimum Data Set (MDS), documented a BIMS score of one, which indicated severely impaired cognition. R41 had no depression or behaviors. R41 required maximal assistance with activities of daily living, which included toileting, dressing, and bathing. R41 was frequently incontinent of bladder. The resident had no falls.
The Care Plan dated 04/03/24, revealed R41 at risk for falls and staff instructed to provide nonskid socks, call light and personal items were within reach. Staff were instructed to provide reminders to R41 to lock her wheelchair brakes before standing up.
The Physician's Order dated 05/22/24, ordered physical therapy evaluation and treatment due to fall.
Review of the Progress Notes from 04/01/24 to 07/30/24 revealed the following:
On 05/08/24 at 07:30 AM, R41 was found on floor in her room in front of her bed. R41 had a raised bump on the back of her head. R41 was sent to hospital for evaluation and treatment as needed.
On 05/08/24 at 11:15 AM, R41 returned to facility, walked on the unit, smiling.
On 07/30/24 at 11:02 AM, family member revealed R41 had a fall and was sent to hospital over a month ago. Family member stated a fall mat on R41's floor had been placed in her room before she had the fall.
On 07/31/24 at 12:25 PM, Certified Nurse Aide (CNA) OO stated that R41 ambulated with staff assistance or with her family member.
On 07/31/24 at 12:26 PM, R41 ambulated out of dining room by family member holding her hand and giving her verbal directions.
On 08/05/24 at 09:30 AM, Administrative Nurse E confirmed the fall was not captured on the MDS. Her expectation was for all MDS assessments to be accurate. Additionally stated that the facility did not have a policy for MDS completion and used the Resident Assessment Instrument (RAI) manual as a guide.
The facility failed to accurately complete the MDS for R41 related to falls. This practice had the potential to lead to negative psychosocial effects related to safety and uncommunicated needs.
-Resident (R) 54's Electronic Health Record (EHR) revealed diagnoses that included dementia (progressive mental disorder characterized by failing memory, confusion) and muscle weakness.
The 05/28/24 Annual Minimum Data Set (MDS) documented a Brief Interview for Mental Status (BIMS) score of 14, indicating intact cognition. R 54 had a total mood severity score of 00, indicating no depression and there were no behaviors documented on the assessment. R54 was independent with all his activities of daily living (ADLs) except he required a set up for shower. The resident had no falls documented on the MDS.
The 05/28/24 Functional Abilities Care Area Assessment (CAA) documented R54 was active in own care needs. Staff to proceed to care plan with continued monitoring and assistance as needed to avoid complications and minimize risks in functional abilities.
The 07/23/24 Quarterly MDS documented a BIMS score of 14. No behaviors. R54 was independent with ADLs, except set-up for shower. The resident had no falls documented on the MDS.
The 07/31/24 Care Plan documented interventions, dated 05/24/24 staff were to encourage R54 to gather blanket in his hand before walking down the hallway. Staff instructed to not let R54 outside wrapped up in a blanket due to tripping hazard, dated 12/20/22. On 05/28/24, a revision was staff instructed to have R54 wear gripper socks as he will allow. On 06/01/24, social service would provide R54 with appropriate fitted shoes.
The 07/31/24 Physician Orders lacked any order regarding falls or safety.
The Fall Risk Data Collection revealed the following for R54:
On 02/29/24 and 05/24/24, R54 was scored as a low risk for falls.
On 06/01/24 and 07/24/24, R54 was scored as a high risk for falls.
Review of the Progress Notes from 01/01/24 to 07/30/24 revealed the following:
On 05/24/24 at 11:59 AM, R54 had a witnessed fall, R54 tripped on his blanket that he had dragged down the hall.
On 06/01/24 at 10:00 AM, R54 had a witnessed fall, R54 tripped on his blanket, had ill-fitted boots on and had carried several blankets that were dragging on the ground.
On 7/30/24 at 09:40 AM, R54 stated he fell yesterday and hit his right foot. R54 stated he had asked for a band aid, or a wrap from the nurse on duty and told her why. Observed slight swelling and slight redness on the top of R54's right foot. R54 stated the nurse did not even look at his foot. Observed three rolled up blankets on the floor in front of his bed. R54 stated he put them there.
On 07/30 24 at 10:16 AM, Certified Nurse Aide (CNA)RR stated that R54 was independent for all his care.
On 07/31/24 at 11:35 AM, R54 had four blankets scattered on the floor and newspapers located in front of R54's bed. R54 was laying in his bed watching television.
On 08/05/24 at 09:30 AM, Administrative Nurse E confirmed the falls was not captured on the MDS. Her expectation was for all MDS assessments to be accurate. Additionally stated that the facility did not have a policy for MDS completion and used the Resident Assessment Instrument (RAI) manual as a guide.
The facility failed to accurately complete the MDS for R54 related to falls. This practice had the potential to lead to negative psychosocial effects related to safety and uncommunicated needs.
- The Electronic Health Records (EHR) documented Resident (R)82 had the following diagnoses that included dementia (progressive mental disorder characterized by failing memory, confusion), muscle weakness and unsteadiness on feet.
The 02/15/24 Annual Minimum Data Set (MDS), documented a Brief Interview for Mental Status (BIMS) score of 01, which indicated severely impaired cognition. R82 had a total mood severity score of 00, indicating no depression and there were no behaviors documented. R82 required moderate assistance with activities of daily living, which included toileting, dressing, transfers, and bathing. R82 was always incontinent of bladder. R82 had two non-injury falls.
The Falls Care Area Assessment (CAA) dated 02/15/24, lacked any documentation for triggered falls documented on the Annual MDS.
The 05/17/24 Quarterly Minimum Data Set (MDS), documented a BIMS score of one, which indicated severely impaired cognition. R82 had no depression or behaviors. R82 required moderate assistance with activities of daily living, which included toileting, dressing, transfers, and bathing. R82 had no falls.
The Care Plan reviewed on 07/31/24, revealed R82 was at risk for falls and staff was instructed to provide nonskid socks or appropriate footwear when ambulating or self-propelling the wheelchair, dated 02/10/23. The staff was instructed to provide toileting to R82 upon rising, before and after meals, at bedtime, and as needed or requested, dated 01/31/24. Staff instructed to position R82 in the center of the bed for safety, dated 06/10/24.
The Physician's Order dated 07/30/24, lacked any orders about falls.
Review of the Progress Notes from 01/01/24 to 07/30/24 revealed the following:
On 01/31/24 at 03:31 PM, R82 was found on floor in her room and a bruise was noted on her right ear.
On 02/08/24 at 11:57 AM, a Physician visit assessed bruised areas on R82, concurred that the bruised areas were related to a previous fall and R82 received an anticoagulant. (a substance that is used to prevent and treat blood clots in blood vessels and the heart. Also called blood thinner).
On 06/10/24 at 11:30 AM, R82 was found on the floor in her room, seated on the fall mat near her bed.
On 08/05/24 at 09:30 AM, Administrative Nurse E confirmed the fall with injury was not captured on the MDS and the CAA note was not completed. Her expectation was for all MDS assessments to be accurate. Additionally stated that the facility did not have a policy for MDS completion and used the Resident Assessment Instrument (RAI) manual as a guide.
The facility failed to accurately complete the MDS for R82 related to falls. This practice had the potential to lead to negative psychosocial effects related to safety and uncommunicated needs.
The facility reported a census of 96 residents with 20 residents selected for review. Based on observation, interview, and record review, the facility failed to accurately complete the Minimum Data Set (MDS) for five of the sampled residents. Resident (R) 28 and R(47) related inaccurate documentation of medications. R (41), R(54) and R(82) related inaccurate documentation on falls. These deficient practices had the potential to lead to uncommunicated need for care and services to meet each individual resident's needs.
Findings included:
- Review of Resident (R) 28's electronic medical record (EMR), revealed a diagnosis of type II diabetes mellitus (DM- when the body cannot use glucose, not enough insulin made, or the body cannot respond to the insulin).
The Significant Change Minimum Data Set (MDS), dated [DATE], documented the resident had a Brief Interview for Mental Status (BIMS) score of 11, indicating moderate cognitive impairment. He received hypoglycemic medication (a group of drugs used to help reduce the amount of sugar present in the blood) during the assessment period.
The Nutritional Status Care Area Assessment, dated 06/07/24, documented the resident had an elevated body mass index (a measure of body fat based on height and weight).
The Annual MDS, dated 04/01/24, documented the resident had a BIMS score of 15, indicating intact cognition. The resident did not receive hypoglycemic medications during the assessment period.
The resident's care plan, revised 06/13/24, instructed staff the resident had a diagnosis of DM. Staff were to monitor and document any signs or symptoms of hypoglycemia (low blood sugar).
Review of the resident's EMR revealed a lack of a physician's order for any hypoglycemic medication.
On 08/05/24 at 01:16 PM, Administrative Nurse E stated the Significant Change MDS, dated [DATE], was incorrect. The resident did not receive any hypoglycemic medication during the assessment period.
The facility utilized the Resident Assessment Instrument (RAI) in accurate completion of the MDS's.
The facility failed to complete an accurate assessment for this resident.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** -Resident (R) 54's Electronic Health Record (EHR) revealed diagnoses that included dementia (progressive mental disorder charact...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** -Resident (R) 54's Electronic Health Record (EHR) revealed diagnoses that included dementia (progressive mental disorder characterized by failing memory, confusion) and muscle weakness.
The 05/28/24 Annual Minimum Data Set (MDS) documented a Brief Interview for Mental Status (BIMS) score of 14, indicating intact cognition. R 54 had a total mood severity score of 00, indicating no depression and there were no behaviors documented on the assessment. R54 was independent with all his activities of daily living (ADLs) except he required a set up for shower. No falls documented.
The 05/28/24 Functional Abilities Care Area Assessment (CAA) documented R54 was active in own care needs. Staff would proceed to care plan with continued monitoring and assistance as needed to avoid complications and minimize risks in functional abilities.
The 07/23/24 Quarterly MDS documented a BIMS score of 14. No behaviors. Independent with ADLs, except set-up for shower. No falls documented.
The 07/31/24 Care Plan documented interventions, dated 05/24/24, revealed staff were to encourage R54 to gather his blanket in his hand before walking down the hallway. Staff instructed to not let R54 outside wrapped up in a blanket due to tripping hazard, dated 12/20/22. On 05/28/24, revised staff instructed to have R54 wear gripper socks as he will allow. On 06/01/24, social service would provide R54 with appropriate fitted shoes. The care plan lacked any interventions or staff guidance to address the blankets and items R54 places in floor in front of his bed to prevent further falls.
The 07/31/24 Physician Orders lacked any order regarding falls or safety.
The Fall Risk Data Collection revealed the following for R54:
On 02/29/24 and 05/24/24 R54 was scored as a low risk for falls.
On 06/01/24 and 07/24/24 R54 was scored as a high risk for falls.
Review of the Progress Notes from 01/01/24 to 07/30/24 revealed the following:
On 05/24/24 at 11:59 AM, R54 had a witnessed fall, R54 tripped on his blanket that he had dragged down the hall.
On 06/01/24 at 10:00 AM, R54 had a witnessed fall, R54 tripped on his blanket, had ill-fitted boots on and had carried several blankets that were dragging on the ground.
On 7/30/24 at 09:40 AM, R54 stated he fell yesterday and hit his right foot. R54 stated he had asked for a band aid, or a wrap from the nurse on duty and told her why. Observed slight swelling and slight redness on top of R54's right foot. R54 stated the nurse did not even look at his foot. Observed three rolled up blankets on the floor in front of his bed. R54 stated he put them there.
On 07/30 24 at 10:16 AM, Certified Nurse Aide (CNA)RR stated that R54 was independent for all his care. Furthermore, stated that R54 did not like staff moving his personal belongings in his room. Stated that R54 always has items on his floor.
On 07/31/24 at 11:35 AM, R54 had four blankets scattered on the floor and newspapers located in front of R54's bed. R54 was laying in his bed watching television.
On 08/05/24 at 09:03 AM, Administrative Nurse E, stated that all the interdisciplinary team members are responsible to revise care plans.
On 08/05/24 at 09:25 AM, Administrative Nurse D stated that the revisions of care plans are a work in progress and confirmed that care plans are not always revised or updated in a timely manner. She also stated that most of the charge nurses do not know how to update a care plan in EHR.
The facility lacked a policy on care plan revision.
The facility failed to implement care plan interventions for this resident who had falls. This deficient practice placed this resident at risk for preventable falls and injuries.
- The Electronic Health Records (EHR) documented Resident (R)41 had the following diagnoses that included dementia (progressive mental disorder characterized by failing memory, confusion), muscle weakness and schizophrenia (mental disorder characterized by gross distortion of reality, disturbances of language and communication and fragmentation of thought).
The 04/14/24 Annual Minimum Data Set (MDS), documented a Brief Interview for Mental Status (BIMS) score of 00, which indicated severely impaired cognition. R41 had a total mood severity score of 00, indicating no depression and there were no behaviors documented. R41 required maximal assistance with activities of daily living, which included toileting, dressing, and bathing. R41 was frequently incontinent of bladder. The resident had no falls.
The Falls Care Area Assessment (CAA) dated 04/14/24, documented R41 was at risk for falls related to impaired cognition and use of medications which may increase risks. Staff to proceed to care plan with continued monitoring and assistance to avoid complications and minimize risk related to falls.
The 07/14/24 Quarterly Minimum Data Set (MDS), documented a BIMS score of one, which indicated severely impaired cognition. R41 had no depression or behaviors. R41 required maximal assistance with activities of daily living, which included toileting, dressing, and bathing. R41 was frequently incontinent of bladder. The resident had no falls.
The Care Plan dated 04/03/24, revealed R41 at risk for falls and staff instructed to provide nonskid socks, call light and personal items were within reach. Staff were instructed to provide reminders to R41 to lock her wheelchair brakes before standing up.
The Physician's Order dated 05/22/24, ordered physical therapy evaluation and treatment due to fall.
Review of the Progress Notes from 04/01/24 to 07/30/24 revealed the following:
On 05/08/24 at 07:30 AM, R41 was found on floor in her room in front of her bed. R41 had a raised bump on the back of her head. R41 was sent to hospital for evaluation and treatment as needed.
On 05/08/24 at 11:15 AM, R41 returned to facility, walked on the unit, smiling.
On 07/30/24 at 11:02 AM, family member revealed R41 had a fall and was sent to hospital over a month ago. Family member stated a fall mat on R41's floor had been placed in her room before she had the fall.
On 07/31/24 at 12:25 PM, Certified Nurse Aide (CNA) OO stated that R41 ambulated with staff assistance or with her family member.
On 07/31/24 at 12:26 PM, R41 ambulated out of dining room by family member holding her hand and giving her verbal directions.
On 08/05/24 at 09:03 AM, Administrative Nurse E, stated that all the interdisciplinary team members are responsible to revise care plans.
On 08/05/24 at 09:25 AM, Administrative Nurse D stated that the revisions of care plans are a work in progress and confirmed that care plans are not always revised or updated in a timely manner. She also stated that most of the charge nurses do not know how to update a care plan in EHR.
On 08/05/24 at 09:30 AM, Administrative Nurse E confirmed the fall intervention was not on R41's care plan in the
EHR.
The facility lacked a policy on care plan revision.
The facility failed to implement care plan interventions for this resident who had fall. This deficient practice placed this resident at risk for preventable falls and injuries.
- The Physician Orders dated 04/01/24 revealed the following diagnoses for Resident (R) 81 included diabetes mellitus (when the body cannot use glucose, not enough insulin made, or the body cannot respond to the insulin) and end stage renal disease (a terminal disease because of irreversible damage to vital tissues or organs).
The Significant Change Minimum Data Set (MDS) dated [DATE] revealed a Brief Interview for Mental Status (BIMS) score of 14, indicating intact cognition. Review of the functional abilities and goals indicated R 81 required substantial/maximal assistance with bathing.
The Quarterly MDS dated 06/12/24 revealed no changes in memory or abilities.
Review of the Care Plan dated 05/07/23 regarding Care/ADL preferences indicated R 81 preferred a shower two times a week as she tolerated, revised on 12/02/23. The care plan lacked days/time R81 preferred to have her bath days.
On 07/31/24 at 02:29 PM, Certified Nurse Aide (CNA) M reported residents should get a minimum of two baths/showers a week and more if they prefer. Residents should have bathing scheduled when they want their bathing done, morning or evening, as well as the type of bath/shower they prefer. She reported the resident's preferences and schedule should be in the care plan. Some residents want a bath/shower one or two times a week while others want one every day. The staff should accommodate their preferences. If the residents refuse their bath/shower, staff should let the MDS coordinator know and also document in the EMR the refusal.
On 08/01/24 at 02:53 PM, Licensed Nurse H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Staff should document refusals in the EMR. Bathing preferences and schedules should be documented in the resident's care plan.
On 08/05/24 at 10:37 AM, Administrative Nurse D confirmed resident's bathing master schedules are by room number and divided between first and second shift. She stated if a resident had a preference for time, type, and frequency of bath, it should be respected. Administrative Nurse D stated the facility staff try to obtain resident's preferences on admission and would expect the staff to adjust accordingly.
The facility failed to provide a policy regarding ADL Care for Dependent Residents as requested on 08/05/24.
The facility failed to revise R81 care plan regarding preferred bath days and preferred times.
The facility reported a census of 96 residents. The sample of 20 residents included four dependent residents sampled for choices/preferences related to bathing, and two residents reviewed for accident/falls. Based on observation, interview, and record review, the facility failed to review and revise the care plan for four Residents (R)92, R73, R 74, R 81 related to bathing preferences/choices and R 54 and R 41 related to accidents/falls to prevent further falls.
Findings included:
- Review of Resident (R) 92's undated Physician's Orders, documentation included diagnoses of Spastic hemiplegia (paralysis of one side of the body), hemiparesis (muscular weakness of one half of the body) affecting left dominate side, and memory deficit following cerebral infarction (stroke - sudden death of brain cells due to lack of oxygen caused by impaired blood flow to the brain by blockage or rupture of an artery to the brain).
The admission Minimum Data Set (MDS) dated [DATE], revealed a Brief Interview for Mental Status (BIMS) score of 14, indicating cognitive intact and he did not exhibit behaviors. He reported it was very important to choose the type of bath he preferred. The resident had impairment of his lower extremity on one side of his body and required substantial/maximal assistance of staff with bathing.
The Functional Abilities/Self-Care Mobility Care Area Assessment (CAA) dated 06/14/24, documentation included a recent history of CVA with hemiparesis. He required assistance with daily cares and mobility. Staff were to proceed to care plan with continued active participation in rehabilitation services for improvement and staff assistance as needed to avoid complications and minimize risks related to functional abilities.
The Care Plan, dated 08/01/24, directed staff the resident required staff participation with bathing, check nail length, trim, and clean on bath days as necessary. The care plan lacked direction to staff related to the residents bathing schedule and/or preferences.
On 07/30/24 at 09:22 AM, upon entering the resident's room, there was a stale musky odor. He laid in the bed. His hair was stringy and oily, and his hair stuck to his head. His overall appearance was unkept. The resident reported he thought his last shower was given a week ago. He stated he had been a resident for over a month and the facility staff told him he could only have a bath on Mondays, and he did not get a bath yesterday. Additionally, he reported he had an appointment the next day and did not want to be stinking when he went. The resident stated he would prefer a bath at least two times a week if he could not get one every day. He reported that less than a weekly bath was not acceptable.
Review of the facility's Shower List schedule documentation revealed residents scheduled based on room numbers. R 92's room number scheduled for a shower on Mondays and Thursdays during the evening shift.
Review of R 92's electronic medical record (EMR) for the 30 days prior to the resident's interview revealed the resident received a bath on three occasions in the previous 30 days. He received a bath on 07/11/24, 07/15/24, and 07/25/24. The EMR documentation lacked indication the staff had offered the bathing opportunities.
On 07/31/24 at 11:10 AM, Social Service Staff reported multiple residents have filed grievances and reported concerns regarding not receiving baths/showers and those concerns have been forwarded to the administrative nurses for address and follow-up.
On 07/31/24 at 02:29 PM, Certified Nurse Aide (CNA) M reported residents should get a minimum of two baths/showers a week, and more if they prefer. Residents should have bathing scheduled when they want their bathing done morning or evening, as well as the type of bath/shower they prefer. She reported the resident's preferences and schedule should be in the care plan. Some residents want a bath/shower one or two times a week while others want one every day. The staff should accommodate their preferences. If the residents refuse their bath/shower, staff let the MDS coordinator know and staff should document in the EMR the refusal. Their bathing should include nail care. He reported he had a doctor's appointment and requested a bath, because he didn't get one.
On 08/01/24 at 02:53 PM, Licensed Nurse H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Staff should document refusals in the EMR. Nail care should be provided by staff with bathing and as needed.
On 08/05/24 at 10:37 AM, Administrative Nurse D confirmed resident's bathing master schedules are by room number and divided between first and second shift. She stated if a resident has a preference for time, type, and frequency of bath should be respected. Administrative Nurse D stated the facility staff try to obtain resident's preferences on admission and would expect the staff to make adjustments accordingly. She confirmed R92's bathing documentation did not reflect his being offered a bathing opportunity at least two times a week or his refusal of any bathing opportunity.
The facility lacked a care plan policy to address the resident's bathing, preferences, and scheduling.
The facility failed to review and revise the care plan for the resident related to his bathing preferences /choices regarding frequency, schedule, and type of bath.
- Review of Resident (R) 73's Physician's Orders, dated 07/27/24 documentation included diagnoses of diabetes, anxiety disorder, acute kidney failure, transient ischemic attack (TIA- temporary episode of inadequate blood supply to the brain), cerebral infarction (CVA-stroke- sudden death of brain cells due to lack of oxygen caused by impaired blood flow to the brain by blockage or rupture of an artery to the brain), and non-pressure chronic ulcer (type of wound related to diabetic complications) of unspecified foot.
The Annual Minimum Data Set, (MDS) dated [DATE], revealed a Brief Interview for Mental Status (BIMS) score of eight, indicating moderate cognitive impairment. The resident had no functional limitation in range of motion of his upper or lower extremities. He had no behaviors and no rejection of care. He reported feeling down, depressed, or hopeless for two to six days of the look back period. He reported choosing the type of bath he wanted was very important to him. The resident required assistance of the staff with his activities of daily living (ADLs). He was dependent on staff assistance for ADLS and was frequently incontinent of urine and occasionally incontinent of bowel.
The Functional Abilities Self-Care and Mobility Care Area Assessment (CAA) dated 07/28/24 documentation included the resident required staff assistance for proper completion and safety to avoid complications and minimize risks.
The Care Plan, , dated 05/28/24, directed staff the resident required one staff participation for the resident to bathing, initiated 08/09/23. The care plan failed to direct staff on the type of assistance, type of bath and schedule for bathing the resident. Bathing preferences were not addressed on the resident's care plan. Additionally, the care plan lacked directions to the staff to provide the resident with hygiene and grooming related to his nails, hair, and beard.
Review of the facility's Shower List schedule documentation revealed residents were scheduled based on room numbers. R 73's room number was scheduled for a shower on Wednesdays and Saturdays during the day shift.
Review of R 73's electronic medical record (EMR) for the 30 days prior to the resident's interview revealed the resident lacked a bath on two occasions in the 30 days prior to the interview on 7/30/24, on 07/08/24 and 07/11/24. The EMR documentation lacked indication the staff had offered the bathing opportunities that he had refused. No documentation of nail care or refusals of offered nail care noted.
On 07/30/24 at 09:58 AM, R 73 laid in the bed. He had a stale musky odor. His hair and beard were long and oily in appearance with his general appearance as notably unkept. The resident's fingernails extended for an inch or more beyond the end of his fingertips with a black substance packed beneath his fingernails. Upon inquiry, he stated he did not move, he stayed in bed 24/7, and the staff knew where he was at and could give him a bath anytime. He reported the facility lacked a hygiene program and he had not had a bath for months. The facility had him on the schedule to receive a shower Tuesday and Saturday, first shift but they do not bath him. He stated he preferred a bed bath at least one time a week but they did not give him one. Additionally, he stated his beard and hair needed trimming, but the beautician did not come to the room to trim resident's hair or beard. He reported he could not get up because the doctor had told him not to put pressure on his feet due to the diabetic ulcer (wound resulting from diabetic complications). R 73 stated he had clippers the staff could use, but no staff would trim his beard or hair in his room. He stated no one had offered to trim or clean his nails which he found to be particularly upsetting because he ate with his hands.
On 07/31/24 at 02:29 PM, Certified Nurse Aide (CNA) M reported residents should get a minimum of two baths/showers a week and more if they prefer. Residents should have bathing scheduled when they want their bathing done morning or evening, as well as the type of bath/shower they prefer. She reported the resident's preferences and schedule should be in the care plan. Some residents want a bath/shower one or two times a week while others want one every day. The staff should accommodate their preferences.
On 08/01/24 at 02:53 PM, Licensed Nurse H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Bathing preferences and schedules should be documented in the resident's care plan .
On 08/05/24 at 10:37 AM, Administrative Nurse D confirmed resident's bathing master schedules are by room number and divided between first and second shift. She stated if a resident has a preference their preference for time, type, and frequency of bath should be respected. Administrative Nurse D stated the facility staff try to obtain resident's preferences on admission and would expect the staff to adjust accordingly. She verified his are care plan lacked direction to the staff regarding his preferences, for type, frequency, and time of his bathing. She confirmed the above findings.
The facility lacked a care plan revision policy related to addressing resident's hygiene, grooming, and bathing preferences.
The facility failed to review and revise the care plan for the resident related to his bathing preferences /choices regarding frequency, schedule, and type of bath.
- Review of Resident (R)74's Physician's Orders, dated 07/27/24, documentation included diagnoses of Alzheimer's Disease (disease (progressive mental deterioration characterized by confusion and memory failure), behavioral disturbances, palliative (end of life) care, type 2 diabetes (DM-when the body cannot use glucose, not enough insulin made or the body cannot respond to the insulin), and depression (a mood disorder that causes a persistent feeling of sadness and loss of interest).
The Significant Change in Status Minimum Data Set (MDS) dated [DATE], revealed a Brief Interview for Mental Status (BIMS) score of 03, indicating severe cognitive impairment. The resident exhibited inattention and disorganized thinking continuously. The resident had no rejection of care. No functional impairment in range of motion of upper or lower extremities. He was dependent on staff for activities of daily living (ADL) care (bathing and personal hygiene). The resident received Hospice services. He reported choosing the type of bath preferences as very important.
The Cognitive Loss/Dementia Care Area Assessment (CAA) dated 07/12/24, documented the resident alert with impaired memory function, poor decision skills and safety awareness.
The Care Plan dated 07/12/24, directed staff the resident required limited to extensive assistance of one staff with grooming. Staff should assist with showering twice weekly and as needed. He refused bathing at times. The care plan lacked address of the resident's bathing and personal hygiene schedule, or preferences/choices related to his bathing, and personal hygiene.
On 07/30/24 at 12:44 PM, R 74 laid in bed with long jagged fingernails that extended well over one-half inch beyond the tips of her fingers. There was black substance packed beneath each of his fingernails. He had an unkept appearance with a lingering stale urine odor.
On 07/30/24 at 04:51 PM, R 74 continued to have long jagged fingernails that extended well over one-half inch beyond the tips of her fingers.There was black substance packed beneath each of her fingernails.
Review of the facility's Shower List schedule documentation revealed residents were scheduled based on room numbers. R 74's room number was scheduled for a shower on Wednesdays and Saturdays during the day shift.
Review of R 74's electronic medical record (EMR) for the 30 days prior to the resident's interview revealed the resident received a bath on two occasions in the previous 30 days on 07/08/24 and 07/11/24. The EMR documentation lacked indication the staff had offered the bathing opportunities which she refused. No documentation of nail care or refusals of offered nail care noted.
On 07/31/24 at 02:29 PM, Certified Nurse Aide (CNA) M reported residents should get a minimum of two baths/showers a week and more if they prefer. Residents should have bathing scheduled when they want their bathing done morning or evening, as well as the type of bath/shower they prefer. She reported the resident's preferences and schedule should be in the care plan. Some residents want a bath/shower one or two times a week while others want one every day. The staff should accommodate their preferences.
On 08/01/24 at 02:53 PM, Licensed Nurse H reported bathing preferences and schedules should be documented in the resident's care plan .
On 08/05/24 at 10:37 AM, Administrative Nurse D confirmed resident's bathing master schedules are by room number and divided between first and second shift. She stated if a resident has a preference their preference for time, type, and frequency of bath should be respected. Administrative Nurse D stated the facility staff try to obtain resident's preferences on admission and would expect the staff to adjust accordingly. She confirmed R74's bathing documentation did not reflect his being offered a bathing opportunity at least two times a week or his refusal of any bathing opportunity. She verified his are care plan lacked direction to the staff regarding his preferences, for type, frequency, and time of his bathing.
The facility lacked a care plan policy to address the resident's bathing, preferences, and scheduling.
The facility failed to review and revise the care plan for the resident related to his bathing preferences /choices regarding frequency, schedule, and type of bath.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** - The Electronic Health Records (EHR) documented Resident (R)82 had the following diagnoses that included dementia (progressive ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** - The Electronic Health Records (EHR) documented Resident (R)82 had the following diagnoses that included dementia (progressive mental disorder characterized by failing memory, confusion), muscle weakness and unsteadiness on feet.
The 02/15/24 Annual Minimum Data Set (MDS), documented a Brief Interview for Mental Status (BIMS) score of 01, which indicated severely impaired cognition. R82 had a total mood severity score of 00, indicating no depression and there were no behaviors documented. R82 required moderate assistance with activities of daily living, which included toileting, dressing, transfers, and bathing. R82 was always incontinent of bladder. R82 had two non-injury falls.
The Cognition Loss/ Dementia Care Area Assessment (CAA) dated 02/15/24 documented R82 alert with impaired memory function, dementia with poor decision skills and safety awareness. Staff to proceed to care plan with continued monitoring and assistance with decisions and tasks for proper completion and safety and to avoid complications and minimize risks with referral to physician as indicated.
The 05/17/24 Quarterly Minimum Data Set (MDS), documented a BIMS score of one, which indicated severely impaired cognition. R82 had no depression or behaviors. R82 required moderate assistance with activities of daily living, which included toileting, dressing, transfers, and bathing. R82 had no falls.
The Care Plan reviewed on 07/31/24, documented R82 had a self-care deficit and staff was instructed to provide cueing and assistance with grooming, dated on 02/10/23.
Review of the Progress Notes from 01/01/24 to 07/30/24 lacked documentation regarding grooming.
On 07/30/24 at 12:46 PM, R82 was seated in the dining room with her lunch in front of her. R82 had several long gray and black colored facial hairs on her chin.
On 07/31/24 at 12:22 PM, R82 continued to have several long gray and black colored facial hairs on her chin, approximately half inch in length.
On 08/01/24 at 09:48 AM, R82 continued to have several long gray and black colored facial hairs on her chin, approximately half inch in length.
On 08/01/24 at 09:53 AM, Certified Nurse Aide (CNA) OO stated that R82 could become combative when staff assist with grooming tasks.
On 08/01/24 at 09:50 AM, Certified Medication Aide (CMA) R stated that when a resident received their shower, the facial hair should be removed. He stated that R82 received her scheduled showers on second shift on Monday and Thursday.
On 08/01/24 at 02:53 PM, Licensed Nurse H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Staff should document refusals in the EMR. Nail and facial hair care should be provided by staff with bathing and as needed.
On 08/05/24 at 09:25 AM, Administrative Nurse D confirmed residents should have their facial hair removed if they allowed or wanted staff to remove it.
The facility lacked a policy for ADLs.
The facility failed to ensure Resident (R)82 received care for removal of facial hair. This deficient practice placed the resident at risk for decreased psychosocial well-being.
The Physician Orders dated 04/01/24 revealed the following diagnosis for Resident (R)81 diabetes mellitus (when the body cannot use glucose, not enough insulin made, or the body cannot respond to the insulin) end stage renal disease (a terminal disease because of irreversible damage to vital tissues or organs).
The Significant Change Minimum Data Set (MDS) dated 05/3124 revealed a Brief Interview for Mental Status (BIMS) score of 14 indicating intact cognition. Review of the functional abilities and goals indicated R 81 required substantial/maximal assistance with bathing.
The Quarterly (MDS) dated [DATE] revealed no changes in memory or abilities.
Review of the Care Plan dated 05/07/23 regarding Care/ADL preferences indicated R 81 prefer a shower two times a week as she can tolerated the care plan lacked which days/time R81 prefers to have her bath completed.
Review of the bathing sheets for May 2024 indicated that R81 received a bath/shower three days out of 31 days
Review of the bathing sheet for June 2024 indicated R81 received a bath/shower five days out of 30 days.
Review of the 30 days look back period for July 2024 revealed a bath/shower R81 received five days out of 31 days.
On 08/01/24 at 02:53 PM Licensed Nurse H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Staff should document refusals in the EMR. Bathing preferences and schedules should be documented in the resident's care plan
08/05/24 at 10:37 AM, Administrative Nurse D confirmed resident's bathing master schedules are by room number and divided between first and second shift. She stated if a resident has a preference their preference for time, type and frequency of bath should be respected. Administrative Nurse D stated the facility staff try to obtain resident's [preferences on admission and would expect the staff to adjust accordingly. She verified her care plan lacked direction to the staff regarding her preferences, for type, frequency, and time of her bathing.
The facility failed to provide a policy regarding ADL Care for Dependent Resident as requested on 08/05/24
The facility failed to provide R 81 with preferences for type, frequency and time of her bathing.
The facility reported a census of 96 residents. The sample of 20 residents included five dependent residents sampled for personal hygiene related to bathing, nail care, hair trimming, and facial hair. Based on observation, interview, and record review, the facility failed to ensure necessary services to maintain good personal hygiene for Resident (R)92, 73, 74, 81, and R 82 related to bathing, nail care, hair care and/ or unwanted facial hair.
Findings included:
- Review of Resident (R) 92's undated Physician's Orders, documentation included diagnoses of spastic hemiplegia (paralysis of one side of the body) and hemiparesis (muscular weakness of one half of the body) affecting left dominate side, and memory deficit following cerebral infarction (stroke - sudden death of brain cells due to lack of oxygen caused by impaired blood flow to the brain by blockage or rupture of an artery to the brain).
The admission Minimum Data Set (MDS) dated [DATE], revealed a Brief Interview for Mental Status (BIMS) score of 14, indicating cognitive intact. R92 did not exhibit behaviors. He reported it was very important to choose the type of bath he preferred. The resident had impairment of his lower extremity on one side of his body and required substantial/maximal assistance of staff with bathing.
The Functional Abilities Self-Care Mobility Care Area Assessment (CAA) dated 06/14/24, documentation included a recent history of CVA with hemiparesis. The resident required assistance with daily cares and mobility. The facility staff would proceed to care plan with continued active participation in rehabilitation services for improvement and staff assistance as needed to avoid complications and minimize risks related to functional abilities.
The Care Plan, dated 08/01/24, directed staff the resident required staff participation with bathing, check nail length, trim, and clean on bath days as necessary. The care plan lacked direction to staff related to the residents bathing schedule and/or preferences.
On 07/30/24 at 09:22 AM, upon entering the resident's room, there was a stale musky odor. He laid in the bed. His hair was stringy and oily, and the hair stuck to his head. His overall appearance was unkept. The resident reported he thought his last shower a week ago. He stated he had been a resident for over a month and the facility staff told him he could only have a bath on Mondays. He did not get a bath yesterday (Monday, 07/29/24). Additionally, he reported he had an appointment the next day and did not want to be stinking when he went. The resident stated he would prefer a bath at least two times a week if he could not get one every day, like he did at his previous location. He reported that less than weekly was not acceptable,he did not care time of day, he just wanted a bath of some type.
Review of the facility's Shower List schedule documentation revealed residents were scheduled based on room numbers. R 92's room number was scheduled for a shower on Mondays and Thursdays during the evening shift.
Review of R 92's electronic medical record (EMR) for the 30 days prior to the resident's interview revealed the resident received a bath on three occasions in the previous 30 days. Bathing documented on 07/11/24, 07/15/24, and 07/25/24. The EMR documentation lacked indication the staff offered the bathing opportunities and if the resident refused.
On 07/31/24 at 11:10 AM, Social Service Staff X reported multiple residents have filed grievances and reported concerns regarding not receiving baths/showers and those concerns have been forwarded to the administrative nurses for address and follow-up.
On 07/31/24 at 02:29 PM, Certified Nurse Aide (CNA) M reported residents should get a minimum of two baths/showers a week and more if they prefer. Residents should have bathing scheduled when they want their bathing done morning or evening, as well as the type of bath/shower they prefer. She reported the resident's preferences and schedule should be in the care plan. Some residents want a bath/shower one or two times a week while others want one every day. The staff should accommodate their preferences. If the residents refuse their bath/shower, staff should let the MDS coordinator know and document in the EMR the refusal. Their bathing should include nail care. CNA M reported when shecame in this morning, she gave R 92 a bath and dressed him because he requested a bath because he was going to the doctor, and he said he did not get his bath on Monday or Tuesday. He uses his urinal and is incontinent of bowel, on occasion.
On 08/01/24 at 02:53 PM, Licensed Nurse (LN)H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Staff should document refusals in the EMR. Bathing preferences and schedules should be documented in the resident's care plan. Nail care should be provided by staff with bathing and as needed.
On 08/05/24 at 10:37 AM, Administrative Nurse D confirmed resident's bathing master schedules are by room number and divided between first and second shift. She stated if a resident has a preference, their preference for time, type, and frequency of bath should be respected. Administrative Nurse D stated the facility staff try to obtain resident's preferences on admission and would expect the staff to make adjustments accordingly. She confirmed R92's bathing documentation did not reflect his being offered a bathing opportunity at least two times a week or his refusal of any bathing opportunity. She verified his care plan lacked direction to the staff regarding his preferences, for type, frequency, and time of his bathing.
The facility lacked a policy to address the resident's bathing, preferences, and scheduling.
The facility failed to ensure necessary services to maintain good personal hygiene related to bathing for this resident.
- Review of Resident (R)74's Physician's Orders, dated 07/27/24, documentation included diagnoses of Alzheimer's Disease (disease (progressive mental deterioration characterized by confusion and memory failure), behavioral disturbances, palliative (end of life) care, type 2 diabetes (DM-when the body cannot use glucose, not enough insulin made or the body cannot respond to the insulin), and depression (a mood disorder that causes a persistent feeling of sadness and loss of interest).
The Significant Change in Status Minimum Data Set (MDS) dated [DATE], revealed a Brief Interview for Mental Status (BIMS) score of 03, indicating severe cognitive impairment. The resident exhibited inattention and disorganized thinking continuously. The resident had no rejection of care. No functional impairment in range of motion of upper or lower extremities. He was dependent on staff for activities of daily living (ADL) care (bathing and personal hygiene). The resident received Hospice services. He reported choosing the type of bath preferences as very important.
The Cognitive Loss/Dementia Care Area Assessment (CAA) dated 07/12/24, documented the resident alert with impaired memory function, poor decision skills, and safety awareness.
The Care Plan dated 07/12/24, directed staff the resident required limited to extensive assistance of one staff with grooming. Staff should assist with showering twice weekly and as needed. She refused bathing at times.
On 07/30/24 at 12:44 PM, R 74 laid in bed with long jagged fingernails that extended well over one-half inch beyond the tips of her fingers. There was black substance packed beneath each of his fingernails. He had an unkept appearance with a lingering stale urine odor.
On 07/30/24 at 04:51 PM, R 74 continued to have long jagged fingernails that extended well over one-half inch beyond the tips of her fingers. There was black substance packed beneath each of her fingernails.
Review of the facility's Shower List schedule documentation revealed residents were scheduled based on room numbers. R 74's room number was scheduled for a shower on Wednesdays and Saturdays during the day shift.
Review of R 74's electronic medical record (EMR) for the 30 days prior to the resident's interview revealed the resident received a bath on two occasions in the previous 30 days on 07/08/24 and 07/11/24. The EMR documentation lacked indication the staff had offered the bathing opportunities which she refused. No documentation of nail care or refusals of offered nail care noted.
On 07/31/24 at 02:29 PM, Certified Nurse Aide (CNA) M reported residents should get a minimum of two baths/showers a week and more if they prefer. Residents should have bathing scheduled when they want their bathing done morning or evening, as well as the type of bath/shower they prefer. She reported the resident's preferences and schedule should be in the care plan. Some residents want a bath/shower one or two times a week while others want one every day. The staff should accommodate their preferences. If the residents refuse their bath/shower, staff should let the MDS coordinator know and document in the EMR the refusal. Their bathing should include nail care. Resident's fingernails should be cleaned as needed. If residents are diabetic, their nails should be cut by the nurses, however all direct care staff can clean resident's fingernails when soiled.
On 08/01/24 at 02:53 PM, Licensed Nurse H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Staff should document refusals in the EMR. Bathing preferences and schedules should be documented in the resident's care plan. Nail care should be provided by staff with bathing and as needed. The residents that are diabetic should have their nails trimmed by the nurses.
On 08/05/24 at 10:37 AM, Administrative Nurse D confirmed resident's bathing master schedules are by room number and divided between first and second shift. She stated if a resident has a preference for time, type, and frequency of bath, it should be respected. Administrative Nurse D stated the facility staff try to obtain resident's preferences on admission and would expect the staff to adjust accordingly. She confirmed R74's bathing documentation did not reflect his being offered a bathing opportunity at least two times a week or his refusal of any bathing opportunity. She verified his are plan lacked direction to the staff regarding his preferences , for type, frequency, and time of his bathing. She confirmed the above findings.
The facility lacked a policy to address the resident's bathing, preferences, and scheduling and the provision of nail care.
The facility failed to ensure necessary services to maintain good personal hygiene related to bathing and nail care for the residents of the facility.
- Review of Resident (R) 73's Physician's Orders, dated 07/27/24 documentation included diagnoses of diabetes, anxiety disorder, acute kidney failure, transient ischemic attack (TIA- temporary episode of inadequate blood supply to the brain), cerebral infarction (CVA-stroke- sudden death of brain cells due to lack of oxygen caused by impaired blood flow to the brain by blockage or rupture of an artery to the brain), and non-pressure chronic ulcer (type of pathological wound) of unspecified foot.
The Annual Minimum Data Set, (MDS) dated [DATE], revealed a Brief Interview for Mental Status (BIMS) score of eight, indicating moderate cognitive impairment. The resident had no functional limitation in range of motion of his upper or lower extremities. He had no behaviors and no rejection of care. He reported feeling down, depressed, or hopeless for two to six days of the look back period. He reported choosing the type of bath he wanted was very important to him. The resident required assistance of the staff with his activities of daily living (ADLs)( personal hygiene and bathing). He was dependent on staff assistance for ADLS and was frequently incontinent of urine and occasionally incontinent of bowel.
The Functional Abilities Self-Care and Mobility Care Area Assessment (CAA) dated 07/28/24 documentation included the resident required staff assistance for proper completion and safety to avoid complications and minimize risks.
The Care Plan, dated 05/28/24, directed staff the resident required one staff participation for the resident to bathing, initiated 08/09/23. The care plan failed to direct staff on the type of assistance, type of bath and schedule for bathing the resident. Bathing preferences were not addressed on the resident's care plan.
Review of the facility's Shower List schedule documentation revealed residents were scheduled based on room numbers. R 73's room number was scheduled for a shower on Wednesdays and Saturdays during the day shift.
Review of R 73's electronic medical record (EMR) for the 30 days prior to the resident's interview revealed the resident lacked a bath on two occasions in the 30 days prior to the interview on 7/30/24, on 07/08/24 and 07/11/24. The EMR documentation lacked indication the staff had offered the bathing opportunities which she refused. No documentation of nail care or refusals of offered nail care noted.
On 07/30/24 at 09:58 AM, R 73 laid in the bed. He had a stale musky odor. His hair and beard were long and oily in appearance with his general appearance as notably unkept. The resident's fingernails extended for an inch or more beyond the end of his fingertips with a black substance packed beneath his fingernails. Upon inquiry, he stated he did not move, he stayed in bed 24/7, and the staff knew where he was at and could give him a bath anytime. He reported the facility lacked a hygiene program and he had not had a bath for months. The facility had him on the schedule to receive a shower Tuesday and Saturday, first shift but they do not bath him. He stated he preferred a bed bath at least one time a week but they did not give him one. Additionally, he stated his beard and hair needed trimming, but the beautician did not come to the room to trim resident's hair or beard. He reported he could not get up because the doctor had told him not to put pressure on his feet due to the diabetic ulcer (wound resulting from diabetic complications). R73 stated he had clippers the staff could use, but no staff would trim his beard or hair in his room. R73 stated no one had offered to trim or clean his nails which he found to be particularly upsetting because he ate with his hands.
On 07/31/24 at 11:10 AM, Social Service Staff X reported the residents had expressed grievances regarding not receiving their baths and showers. She stated those grievances were forwarded to the Administrative Nursing staff for follow-up. Social Service Staff X reported she did not know how the residents' got their hair and beard trimmed if they did not go to the beauty shop. She stated she did not think the direct care staff provided that care and was not sure if the beautician went to the resident's rooms to trim their hair or bead.
On 07/31/24 at 02:29 PM, Certified Nurse Aide (CNA) M reported residents should get a minimum of two baths/showers a week and more if they prefer. Residents should have bathing scheduled when they want their bathing done morning or evening, as well as the type of bath/shower they prefer. She reported the resident's preferences and schedule should be in the care plan. Some residents want a bath/shower one or two times a week while others want one every day. The staff should accommodate their preferences. If the residents refuse their bath/shower we let the MDS coordinator know and document in the EMR the refusal. Their bathing should include nail care. Resident's fingernails should be cleaned as needed. If residents are diabetic, their nails should be cut by the nurses, however all direct care staff can clean resident's fingernails when soiled. She did not know if the beautician would go to a resident's room and trim their hair or beard.
On 08/01/24 at 02:53 PM, Licensed Nurse (LN) H reported the residents have scheduled times for bath/showers. Some residents prefer a bed bath, some refuse. Staff should document refusals in the EMR. Bathing preferences and schedules should be documented in the resident's care plan. Nail care should be provided by staff with bathing and as needed. The residents that are diabetic should have their nails trimmed by the nurses. He reported he could cut R 73's fingernails and anyone could clean them even though the resident was a diabetic.
On 08/05/24 at 10:37 AM, Administrative Nurse D confirmed residents' bathing master schedules are by room number and divided between first and second shift. She stated if a resident has a preference for time, type, and frequency of bath should be respected. Administrative Nurse D stated the facility staff try to obtain resident's preferences on admission and would expect the staff to adjust accordingly. She confirmed R73's bathing documentation did not reflect his being offered a bathing opportunity at least two times a week or his refusal of any bathing opportunity. She verified his care plan lacked direction to the staff regarding his preferences , for type, frequency, and time of his bathing. She confirmed the above findings.
The facility lacked a policy to address the resident's ADL care and personal hygiene to include bathing, preferences, scheduling, nail care, beard and/or hair trimming.
The facility failed to ensure necessary services to maintain good personal hygiene related to bathing and nail care for this resident.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
The facility reported a census of 96 residents. Based on observation, interview, and record review, the facility failed to serve food that is palatable, and at a safe and appetizing temperature for th...
Read full inspector narrative →
The facility reported a census of 96 residents. Based on observation, interview, and record review, the facility failed to serve food that is palatable, and at a safe and appetizing temperature for the residents of the facility.
Findings included:
- On 07/30/24 at 07:45 AM, during entrance tour of the facility, observation revealed open metal carts with 10 plus meal trays being served on each of the five units. The plate lacked insulated covers, nor served in closed insulated food service cart. Staff observed serving and setting up individual trays off the open cart one at a time while the remaining meals trays remained in the hallway on the open carts.
During resident screening, residents shared concerns related to food which included:
1. On 07/30/24 at 09:58 AM, Resident (R)73, reported sometimes is meal is served an hour late and when he got his meal, the temperature of the food is not good. The food that is supposed to be cold is warm, and the hot foods are cold.
2. On 07/30/24 at 12:16 PM, R 68 reported the food is not acceptable. it is rough, the quality of the food, they cannot seem to get anything right. The food is always cold. He stated he did not think he had a warm meal since he had been in the facility.
3. On 07/30/24 at 02:18 PM, R61 reported staff deliver his food to his room, and it is always cold.
On 07/31/24 at 1:10 AM, Social Service Staff X confirmed the residents had expressed multiple complaints about the food temperatures to the direct care staff and during Resident Council. She reported that the facility had COVID in the building and residents ate in their room on the halls. The facility served the residents trays from open carts. Social Service Staff X confirmed the plates lacked covers on the plates to maintain food temperature.
On 07/31/24 at 12:40 PM, Activity Staff Z reported the facility discussed the need for having a Hot Box for tray service for residents that eat in their room. The meals are on the hall awaiting service and the residents have complained about the food temperatures when they get their trays. She reported sometimes staff served the resident's meal served 20 to 30 minutes late.
On 08/01/24 10:12 AM, dietary Staff BB reported the facility did not have enough insulated covers or closed meal cart to maintain temperatures for all the residents that ate in their rooms. The residents' meal selections obtained by the certified nurse aides (CNAs) as they take the orders and bring them to the dietary staff to set up trays. Since COVID we do not have enough insulation covers for every resident that eats in their room.
On 08/01/24 at 12:34 PM, a sample tray was provided from the 300 hall/unit for testing temperatures at point of service. The sample tray included cold items with temperatures outside of the recommended parameters as follows:
1. Potato Salad was 61.4 degrees Fahrenheit (F), verses cold food temperature recommendation of 42 degrees Fahrenheit (F).
2. The egg salad was 58.1 degrees F, verses cold food temperature recommendation of 42 degrees F.
Cold food items were served directly on a heated plate with ham and beans which temped at 141.4 F. Cold item all exceeded acceptable temperature of 42 degrees F to prevent food borne bacteria. Dietary Staff BB confirmed the temperatures were not acceptable.
On 08/01/24 at 12:57 PM, Administrative Staff A confirmed the above findings and confirmed the temperatures exceeded recommendations for point of service of cold foods. Additionally, he stated that the cold foods should not be served directly on the heated plates with the ham and beans, but should be served in separate dishes to maintain acceptable temperature for cold food.
The undated facility policy Cooking and Cooling, lacked address of maintain the temperature of food through point of service.
The facility failed to serve food that is palatable, and at a safe and appetizing temperature for the residents of the facility.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0923
(Tag F0923)
Could have caused harm · This affected multiple residents
The facility reported a census of 96 residents. Based on observation and interview, the facility failed to provide adequate ventilation in the beauty shop. The facility lacked ventilation to the outsi...
Read full inspector narrative →
The facility reported a census of 96 residents. Based on observation and interview, the facility failed to provide adequate ventilation in the beauty shop. The facility lacked ventilation to the outside by means of a window, mechanical vent or the combination of to promote good air circulation, as required.
Findings included:
- On 8/05/24 at 08:00 AM during the initial tour of the facility an assessment of the beauty shop ventilation system revealed the facility lacked an outside ventilation, as required.
On 08/05/24 at 08:15 AM, Interview with Administrative Staff A revealed the beautician did not do any certain treatments like perms or bleaching in the beauty shop, so an exhaust fan is not needed.
The facility failed to provide a policy regarding beauty shop ventilation as requested on 08/05/24.
The facility failed to provide adequate ventilation in the beauty shop to promote good air circulation, as required.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
The facility reported a census of 96 residents. Based on interview and record review, the facility failed to provide direct care staff annual evaluations/performance reviews for five of the five certi...
Read full inspector narrative →
The facility reported a census of 96 residents. Based on interview and record review, the facility failed to provide direct care staff annual evaluations/performance reviews for five of the five certified nursing assistants sampled, to determine strengths and weaknesses in providing resident care.
Findings included:
- Review of five Certified Nursing Assistant (CNA) personnel files revealed the following:
Review of CNA UU, with hire date of 05/29/19, revealed the lack of an annual review.
Review of CNA VV, with hire date of 11/09/21, revealed the lack of an annual review.
Review of CNA S, with hire date of 01/12/22, revealed the lack of an annual review.
Review of CNA PP, with hire date of 11/16/21, revealed the lack of an annual review.
Review of CNA T, with hire date of 12/09/19, revealed the lack of an annual review.
On 08/01/24 at 02:25 PM, Administrative staff B reported employee annual reviews should be completed by the Director of nursing.
On 08/05/24 at 10:36 AM, Administrative Nurse D reported she thought the Administrator was to complete staff annual reviews. She was not aware that staff annual evaluation/reviews were not getting completed.
The facility lacked a policy related to employee annual performance evaluations.
The facility failed to provide direct care staff an annual evaluation to determine strengths and weaknesses.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected most or all residents
The facility reported a census of 96 residents. Based on interview and record review, the facility failed to develop, implement, and maintain an in-service training program to ensure staff completed t...
Read full inspector narrative →
The facility reported a census of 96 residents. Based on interview and record review, the facility failed to develop, implement, and maintain an in-service training program to ensure staff completed the required 12-hour in-service education for five of the five Certified Nurse Assistants (CNA) sampled, who were employed by the facility for at least one year. This deficient practice placed the residents at risk of decreased quality of care.
Findings included:
- Review of five Certified Nursing Assistant (CNA) personnel files and in-service training revealed the following:
Review of CNA UU, with hire date of 05/29/19, lacked 12 hours of in-service education.
Review of CNA VV, with hire date of 11/09/21, lacked 12 hours of in-service education.
Review of CNA S, with hire date of 01/12/22, lacked 12 hours of in-service education.
Review of CNA PP, with hire date of 11/16/21, lacked 12 hours of in-service education.
Review of CNA T, with hire date of 12/09/19, lacked 12 hours of in-service education, as CNA T received 0.5 hour.
On 08/05/24 at 10:36 AM, Administrative Nurse D reported she was aware staff did not have the required 12-hour in-services and it was a work in progress. The director of nurses was starting to monitor the training.
On 08/05/24 at 11:24 AM, Licensed Nurse (LN) staff L reported there was a computer training for some, however LN L reported not all staff have a log in for the computer training. There is an occasional employee meeting to talk about concerns, or the in-service was a piece of paper that would have to be read and signed off.
On 08/05/24 at 11:57 AM, Administrative staff A reported he was aware the computer training was not utilized as it was intended.
The facility lacked a policy related to requirements of 12 in-service hours.
The facility failed to develop, implement, and maintain an in-service training program to ensure staff completed the required 12-hour in-service education for five of the five Certified Nurse Assistants (CNA) sampled, who were employed by the facility for at least one year. This deficient practice placed the residents at risk of decreased quality of care.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0949
(Tag F0949)
Could have caused harm · This affected most or all residents
The facility reported a census of 96 residents. Based on interview and record review, the facility failed to develop, implement, and maintain an effective training program for all staff, which include...
Read full inspector narrative →
The facility reported a census of 96 residents. Based on interview and record review, the facility failed to develop, implement, and maintain an effective training program for all staff, which included, at a minimum, training on behavioral health care and services that was appropriate and effective. This failure placed all 96 residents at risk of not reaching their highest practicable well-being.
Findings included:
- Review of five Certified Nursing Assistant (CNA) personnel files and Course Completion History (computer training) revealed the following:
Review of CNA UU, with hire date of 05/29/19, lacked behavioral training. The Alzheimer's Disease and Related Disorders: Behaviors module not started and was due by 04/30/23. No course listed the module for 2024.
The Behavioral Health module, not started and was due by 01/31/23, and no course listed for the module in 2024.
Review of CNA VV, with hire date of 11/09/21, the Behavioral Health was not started and was due by 01/31/24.
Review of CNA S, with hire date of 01/12/22, lacked behavioral health training. The Alzheimer's Disease and Related Disorders: Behaviors module not started and due by 10/31/22. The Behavioral Health module, due by 01/31/23, was in progress.
Review of CNA PP, with hire date of 11/16/21, lacked behavioral training. The Alzheimer's Disease and Related Disorders: Behaviors module not started and was due by 10/31/22.
The Behavioral Health was not started and was due by 01/31/23.
Review of CNA T, with hire date of 12/09/19, lacked behavioral training. The last Alzheimer's Disease and Related Disorders: Behaviors module completed 10/29/21.
The Managing Behaviors in Long term Care module last completed 10/27/20.
On 08/05/24 at 10:36 AM, Administrative Nurse D reported she was aware staff did not have behavioral training or in-services and it was a work in progress. The director of nurses was starting to monitor the training.
On 08/05/24 at 11:24 AM, Licensed Nurse (LN) staff L reported there was a computer training for some, however LN L reported not all staff have a log in for the computer training. There is an occasional employee meeting to talk about concerns, or the in-service was a piece of paper that would have to be read and signed off. There have been no actual training on how to effectively handle all the residents with behaviors.
On 08/05/24 at 11:57 AM, Administrative staff A reported he was aware the computer training was not utilized as it was intended and the facility lacked educating staff.
The facility lacked a policy related to requirements of behavioral training.
The facility failed to develop, implement, and maintain an effective training program for all staff, which included, at a minimum, training on behavioral health care and services that was appropriate and effective. This failure placed all 96 residents at risk of not reaching their highest practicable well-being.