CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review, and facility policy review, it was determined the facility failed to have an eff...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review, and facility policy review, it was determined the facility failed to have an effective system in place to ensure one (1) of two (2) sampled residents was provided adequate supervision (Resident #1).
The facility assessed and care planned Resident #1 to be a high risk for elopement and a wanderguard was placed on the resident on 11/22/19. However, on 12/31/19 at approximately 4:00 PM, Resident #1 was able to exit the facility without staff's knowledge. Resident #1 was observed to be across the road from the facility on the sidewalk by a staff member that was leaving work. The resident crossed a busy highway, went into a convenience store, bought a lottery ticket, and walked approximately fifty (50) yards, then crossed back across the busy street. The resident was returned to the facility with no injuries noted.
The facility's failure to have an effective system in place to provide adequate supervision to prevent an elopement, has caused or is likely to cause serious injury, harm, impairment, or death to a resident. Immediate Jeopardy was determined to exist on 12/31/19 and the facility was notified of the Immediate Jeopardy on 01/10/2020.
The facility submitted an Allegation of Compliance (AoC) on 01/14/2020 alleging the Immediate Jeopardy was removed on 01/04/2020, prior to the State Survey Agency entering the building on 01/07/2020, indicating past noncompliance. The State Survey Agency (SSA) determined the facility had corrected the deficiency on 01/04/2020 prior to the SSA entering the building on 01/07/2020; resulting in the determination of Past Jeopardy. However, after supervisory review it was determined the facility was not in substantial compliance on 01/04/2020. Record review and interview revealed the first elopement drill was not held until 01/06/2020 and a Quality Assurance meeting had not been held since 12/31/19 to review the facility's monitoring to ensure compliance was achieved. Therefore, the State Survey Agency determined the Immediate Jeopardy was removed on 01/07/2020. The Scope and Severity was lowered to a D for CFR 483.25 Quality of Care at F689; while the facility develops and implements the Plan of Correction (PoC); and, the facility's Quality Assurance (QA) monitors the effectiveness of the systemic changes.
The findings include:
Review of the facility's policy titled, Accidents and Incidents dated September 2019 revealed the purpose of the Incident and Accident Process is to ensure the facility environment is as free from accident hazards over which the facility has control and that each resident receives adequate supervision and assistive devices to prevent avoidable accidents according to regulatory guidelines. The facility's Administrator will ensure incidents are reported to the appropriate State agency in compliance with the State reporting criteria. Notification of physician and responsible party will be completed with any accident/incident. Incident/Accidents, including elopement, is investigated by the IDT and reported according to regulatory guidelines. Assessments and investigations are done in a systematic manner: Identifying hazards and risks, evaluating and analyzing hazards and risks, implementing interventions to reduce hazards and risks, and monitoring for effectiveness and modifying interventions when necessary. The resident's Care Plan and Certified Nurse Aide Kardex or Care Card is to be updated as interventions are implemented.
Record review revealed the facility admitted Resident #1 on 11/22/19 with a diagnoses of Alzheimer's Dementia.
Review of the Hospital Discharge summary dated [DATE] and faxed to the facility on [DATE], revealed the resident was admitted on [DATE] with diagnoses of Atypical Chest Pain, Gastroesophageal reflux disease, Alzheimers Disease and Dementia. Per family his/her living conditions were poor. He/She lived by self and had a history of wandering out in the middle of the night due to confusion from Dementia. Resident was admitted several days ago for potential placement or assistance at home; however, he/she eloped from hospital. This resulted in police being called and the resident was found at home.
Review of Resident #1's Elopement Evaluation dated 11/22/19 revealed he/she was assessed at a ten (10) which indicated the resident was a high risk for elopement. Further review revealed the resident had a history of wandering prior to admission, ambulated ad lib and was cognitively impaired.
Review of the admission Minimum Data Set (MDS) assessment, dated 11/29/19, revealed the facility assessed Resident #1's cognition was severely impaired with a Brief Interview for Mental Status (BIMS) score of three (3) which indicated the resident was not interviewable. Further review of the assessment in Section E Behavior, revealed the resident was assessed to have wandering behaviors that occurred one (1) of three (3) days. Review of the Activities of Daily Living functional status found the resident was independent with supervisory oversite.
Review of Resident #1's Nursing Notes, dated 11/22/19 at the time of admission, revealed a wander guard was placed due to history of wandering prior to admission.
Review of Resident #1's December 2019 Physician Orders revealed an order for Wanderguard and check placement and function every shift.
Review of the Comprehensive Care Plan for Wandering/Elopement related to exit seeking behaviors, packing of belongings, and wandering behavior, dated 12/09/19, revealed goals that Resident #1 will wander in a safe environment, resident will not wander outside of the facility, resident will be redirected to a safer area, wandering episodes will decrease in ninety (90) days, and the resident will adjust and accept nursing placement. Further review revealed interventions to attempt to determine needs when speaking of leaving, attempt to distract, attempt to have resident complete crossword puzzles as will, distract with programs or general conversation, engage resident in group activities to decrease wandering, involve family/significant other in care planning, notify Medical Doctor of any change in resident's condition, redirect during wandering episode, and staff to be alert for hoarded food/drinks in room, remove as needed and offer snack/drink to replace ones removed. In addition, it was noted on the care plan the resident liked to read the Bible, eat snacks and converse with others and had a Wander guard bracelet.
Review of Resident #1's Nursing Progress Note, dated 12/31/19 at 7:10 PM by Licensed Practical Nurse (LPN) #1 revealed, at approximately 4:00 PM, the resident was noted outside of the facility by a staff member and was returned to the facility. The door alarm sounded with reentrance into facility. The resident was dressed appropriately for outside weather conditions and was placed on one on one watch with staff immediately following entrance to facility. There was no injury noted with visual examination. A full head to toe body audit was completed by signee with no new areas of concern noted at this time. No new bruising, discolorations, edema, open areas, or new areas were noted. Signee called Guardian and left voice mail. The MD was alerted and no new orders were received. Blood pressure was 138/76, Pulse 84, and Respirations 18, even and nonlabored. Temporal temperature was 97.3 and Oxygen saturation was 97% on room air.
Review of the facility's Investigation Report dated, 01/02/2020, revealed based on resident and staff interviews, the resident was observed to be out of the Center, near the Dollar store by a staff member who was leaving the building after completing her shift. The staff member approached the resident and assisted the resident back into the building. The resident stated he/she left the Center to buy him/herself a lottery ticket. The investigation revealed the resident did in fact purchase a lottery ticket from the convenience store across the street from the facility. Upon returning to the facility, the resident was placed on 1:1 supervision. Resident assessment indicated no change in condition and no injuries noted. Further review revealed the facility determine the resident exited the building without staff's knowledge but were unable to determine through which door and how.
According to website timeanddate.com, the temperature on 12/31/19 was 48 degrees Fahrenheit and sunny at 12 noon and 41 degrees Fahrenheit at 6:00 PM.
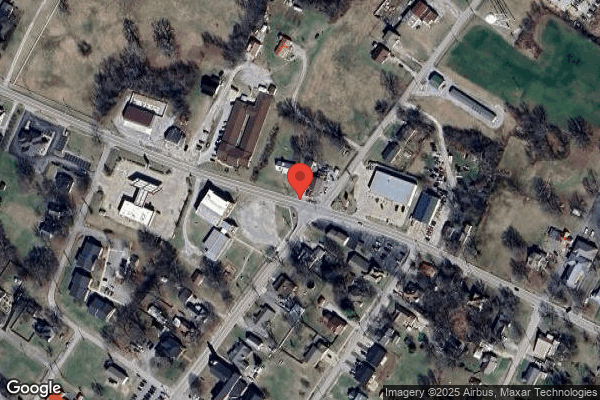
Observation on 01/09/2020 at 1:50 PM by this surveyor and Administrator revealed Resident #1 walked approximately ninety-five (95) yards (verified by Administrator with range finder) to the convenient store, then walked approximately fifty (50) yards to where he/she was first seen by staff. The speed limit for the highway the resident crossed was thirty-five (35) miles per hour (mph). The road is historically busy since it is the main road to and from the county seat.
Interview with the Human Resources employee, on 01/09/2020 at 1:43 PM revealed on 12/31/19 she left work around 3:55 PM. She stated she turned left out of parking lot and noted Resident #1 on the sidewalk across the road past the facility so she pulled into a parking lot of the gym and she then noted the resident had walked back across the road. She stated she also crossed the road and asked the resident to go with her back to the facility, and they both crossed the road again and she got the resident into her car and drove back to the facility. She revealed she text the Activities Director who met her at the door with the Assistant Director of Nursing and LPN #1. She further revealed she was glad she saw the resident and returned him/her back to facility.
Interview with Activities Director on 01/09/2020 at 2:24 PM revealed she received a text from the Human Resources Employee at 4:10 PM and met them at the door. She stated when she opened the door, Resident #1 walked back into the facility, and the resident's wanderguard alarm sounded. She also revealed she had witnessed the resident walking the halls earlier on 12/31/19 prior to the elopement.
Interview (Post Survey) with Certified Nurse Aide (CNA) #5 on 01/15/2020 at 1:10 PM revealed she was caring for Resident #1 on 12/31/19, the day of the elopement. She stated she did not see the resident trying to leave facility but did see him/her going from the lobby back and forth to the room in a calm manner which was calmer than usual for the resident. She revealed the resident usually goes back and forth to call her family at the lobby nurses station. She stated she did not see resident with a coat on that day and the last time she saw him/her, he/she was around his/her doorway at 3:45 PM. She further revealed she did not remember hearing a wander guard alarm sound that day or hear an alarm sound when resident came back to building. She stated when the resident wanders, we redirect him/her with snacks and activities including word search books or puzzles.
Interview with LPN #1 (who was assigned to Resident #1 on 12/31/19), on 01/10/2020 at 10:55 AM revealed she had noted Resident #1 walking up and down the halls on 12/31/19. She stated she did not remember the alarm going off that day around 3:45 PM to 4:00 PM; however, she was at the door when the resident returned and the wanderguard alarm sounded when he/she approached the door.
Interview (Post Survey) with CNA #6 on 01/15/2020 at 1:20 PM revealed she was assigned to Resident #1's hall but not the resident. She stated she saw Resident #1 walking up and down hallway as usual but did not see him/her trying to get out of the facility. She revealed the resident was easily distracted by striking up a conversation with him/her and would sit for a while. She further revealed the resident liked word search books. She stated the last time she saw Resident #1 was at 3:20 PM when she clocked out and the resident was sitting on the couch in the lobby speaking with another resident. She further stated she did not hear any wander guard alarms go off that day.
Interview with CNA #3 (not assigned to hall with resident) on 01/10/2020 at 4:55 PM revealed she worked on 12/31/19 and saw Resident #1 walking up and down the halls on that date. She also revealed she saw the resident at the lobby nurses station talking on the phone. She stated she did not hear the wanderguard alarm sound that date nor did she see the resident leave the building. She further revealed the resident was always visiting with other residents.
Interview with Director of Culinary Services on 01/09/2020 at 3:30 PM revealed Resident #1 likes to visit in her office. She stated she had seen the resident in her coat and he/she told her he/she wanted to go to church outside of facility. She stated she heard the door alarm on 12/31/19 around noon, went to the side door where visitors come in and found Resident #1 trying to open the door. She revealed she directed the resident to back away from the door and then opened the door for visitors. She stated she was aware the resident's wanderguard alarm had not sounded and took the resident immediately to LPN #1 and tested the resident's wanderguard and found it was working; however, when the resident was taken to the outside door, the alarm did not sound. She stated the wanderguard was removed and replaced, and the new wanderguard bracelet was validated to be working properly.
Further review of the resident's plan of care revealed on 12/31/19 an intervention was added that wander guard bracelet replaced. Interview with LPN #1 on 01/10/2020 at 10:55 AM revealed she remembered changing the resident's wanderguard bracelet that date. She stated it was around lunch time but unable to recall exact time.
Interview with the Maintenance Supervisor on 01/09/2020 at 2:39 PM revealed he clocked out on 3:51 PM at the nurses station in the lobby and Resident #1 was on the phone at the nurses station with his/her coat and hat on. He stated the resident liked to move around and talk with people. He revealed the resident's wanderguard had been replaced earlier that day due to it not working at the outer doors and the replacement wanderguard was validated and worked properly. He stated there were wanderguard alarms on each outside egress to the facility, and he checks the doors daily and they have been working correctly. He further revealed on 12/31/19 he actually checked the doors three (3) times due to the resident's wanderguard not working. He revealed in his opinion, the door was probably opened by a visitor and the resident walked out the door. He believed the alarm sounded but no one checked to see if a resident was leaving. He revealed he could not prove that but since the alarms systems were working, that was his conclusion.
Interview with the Assistant Director of Nursing (ADON) on 01/09/2020 at 12:50 PM revealed when Resident #1 returned to the facility, the resident was dressed appropriately for outside with a coat and hat on. The ADON stated when the resident walked back into the building the resident's wanderguard alarmed. She revealed a head to toe assessment was completed with no new injuries identified. She further revealed the resident stated he/she was not aware he/she could not leave the facility and just wanted a lottery ticket. She stated a full facility head count was completed when the resident returned and all residents were accounted for. She also revealed the resident had a history of going to the doors and looking out and also goes into other resident's rooms to visit and talk.
Interview with the Director of Nursing (DON) on 01/10/2020 at 2:10 PM revealed it was not determined what door the resident left from; however, when she interviewed the resident on 12/31/19 at 5:15 PM, the resident stated he/she went out the left upper side door and went to buy a lottery ticket. She stated the resident said, I went out with everyone else. The DON further revealed, if resident went out the front side door, then he/she took the drive to the road, and walked across the road to the convenience store across from facility.
Interview with Resident #1's Guardian, on 01/09/2020 at 12:01 PM revealed the MD orders from the hospital were for the resident to go to a secured facility because of Dementia/Alzheimer's and the resident had wandered off from the hospital. She stated she was under the assumption the facility was secured.
Interview with the Advanced Practice Registered Nurse (APRN) #1 on 01/10/2020 at 10:39 AM revealed she was not aware the resident had eloped from the hospital prior to admission and did not know the history of wandering off from home. She revealed this facility was not a memory care unit which appeared the resident required.
Interview with the DON on 01/09/2020 at 3:47 PM revealed if she had known the resident was an elopement risk prior to the admission, she would have turned down the admission. She stated she was unaware the resident had eloped from the hospital prior to admission and admissions were usually an IDT decision if the resident had a history of elopement on the referral.
Further review of Resident #1's record revealed the facility reassessed the resident's BIMS score on 12/31/19 and assessed Resident #1's cognition as moderately impaired with a BIMS score of nine (9) which indicated the resident was interviewable.
Interview and observation with Resident #1 on 01/09/2020 at 12:15 PM revealed the resident had a sitter at bedside. When asked, the resident revealed he/she did not know they could not leave the facility. The resident revealed he/she liked to buy lottery tickets and would be sad if he/she could not buy them. Further interview with the resident on 01/10/2020 at 10:16 AM revealed he/she would not leave the facility unless someone took him/her. The resident stated they went out the door but did not recall which door or if alarm sounded or not.
**The facility implemented the following actions to correct the deficient practice:
1. A complete head to toe assessment was conducted for Resident #1 including but not limited to a complete set of vital signs. This was completed by LPN #1 on 12/31/19.
2. A new Elopement Risk Assessment was completed on Resident #1 on 12/31/19 and 01/02/2020 by the MDS Coordinator.
3. Resident #1's Wanderguard was checked for function and placement by LPN #1 on 12/31/19.
4. The DON and LPN #1 notified Resident #1's MD and resident representative he/she exited the facility on 12/31/19.
5. Resident #1's Plan of Care and CNA Plan of Care was updated per DON/Licensed Nurse on 12/31/19.
6. The IDT team reviewed Resident #1's entire plan of care to determine if all interventions were in place per the plan of care on 12/31/19.
7. The DON completed interviews with all staff on duty at the time of the incident related to the whereabouts of Resident #1 and their response to the door alarm on 12/31/19.
8. A timeline was completed from 12/31/19 through 01/03/2020 by the DON and Social Services Director to determine when staff last saw Resident #1 and what he/she was doing at the time.
9. Documented in investigation what resident was wearing, what the temperature and weather conditions were outside and how long resident was outside facility. This was completed by DON, Administrator, Social Services Director, and LPN #1 on 12/31/19.
10. The revised care plan interventions for Resident #1 were communicated to the staff by LPN #1, DON, and Social Services Director on 12/31/19.
11. A complete head count of all current residents was completed by LPN #1 on 12/31/19 with all residents accounted for.
12. New Elopement Risk Assessments were completed for all current residents by the MDS Coordinator on 01/02/2020.
13. All residents with the risk for elopement were audited to determine that the following items were in place for each resident at risk: Wander guard order for placement check and function each shift and signed off appropriately, each resident at risk for elopement has a wander guard in place and not expired, each resident at risk for elopement has behavior monitoring for exit seeking behaviors and person centered non pharmacological interventions, and each resident at risk for elopement has a care plan for exit seeking/elopement risk that is current and reflects the residents' person-centered, non-pharmacological behavior interventions, wander guard, etc. This was completed by the DON, Administrator, Staff Development Coordinator (SDC), LPN #1, and Social Services Director (SSD). This was started on 12/31/19 and completed by 01/03/2020.
14. All Elopement Binders were audited to validate that all current residents at risk have a picture that accurately reflects the residents' current appearance and resident identification information. This was completed on 01/02/2020 by DON and SSD.
15. A Complete assessment of all exit doors to verify doors and door alarms were functioning appropriately was completed on 12/31/19 by the Maintenance Director.
16. The Door and Wanderguard alarm vendor was contacted to have system function verified. The contact was made by the Administrator on 01/01/2020 and system function completed on 01/02/2020 by vendor.
17. All staff was re-educated on the Elopement Process and response to all door alarms by the DON, Administrator, Staff Development Coordinator (SDC) and LPN #1 and education was completed on 01/03/2020.
18. The DON, SSD, SDC, LPN #1 and Administrator completed an elopement drill on each shift to evaluate staff response to the wander guard alarms on 12/31/19.
19. Maintenance completed an assessment of the alarms systems and doors to determine all were functioning as per manufacturer guidelines and audible to staff. This was assessed for completion by the Administrator on 01/02/2020.
20. A certified technician from a vendor checked functioning of exit doors/panels on 01/02/2020 and it was confirmed by the Administrator on 01/02/2020.
21. The DON added signs to exit doors on 12/31/19 to alert visitors/staff upon exiting and entering to not let anyone out without checking with staff.
22. The Administrator and/or Director of Nursing will complete an elopement drill on alternating shifts weekly times four (4) weeks, then monthly times two (2) months, and then at least quarterly moving forward. They will assess the staff response then provide additional education or guidance based on that response. This will be completed by the Administrator, DON and SSD and will be ongoing.
23. A summary of the monthly Elopement drills and door alarm checks will be submitted to the Quality Assurance Committee for further review and recommendations. This will be completed by the Administrator and/or the DON.
24. An Ad Hoc QAPI meeting was held with the Administrator, Director of Nursing, and Medical Director (include others as needed) to review the incident, action plan and findings. This was completed by Administrator, SSD, DON, and the Medical Director on 12/31/19.
25. A monthly QA meeting will be reviewed for current status of Action plan. This will be completed by Administrator, SSD, DON, and the Medical Director on 12/31/19.
**The State Survey Agency validated the corrective action taken by the facility as follows:
1. Review of Resident #1's facility medical record dated 12/31/19 revealed a head to toe assessment with vital signs within normal limits was completed by LPN #1.
2. Review of Resident #1's medical record revealed an Elopement Risk Assessment completed on 12/31/19 by the MDS Coordinator. The elopement risk evaluation on 12/31/19 revealed a score of twenty (20) which was considered high risk for elopement. The elopement risk evaluation on 01/02/2020 by the MDS Coordinator revealed a score of thirty (30) which revealed a high risk for elopement. However, a revision was completed on that assessment by the MDS Coordinator and a score of fifty (50) was determined.
3. Review of Resident #1's December 2019 Treatment Administration Record revealed the wanderguard was checked for function and placement on 12/31/19 and every shift as ordered.
Observation of Resident #1 on 01/10/2020 at 10:16 AM with one on one staff at bedside found resident laying in bed with Wanderguard Bracelet in place. At 10:55 AM on 01/10/2020, surveyor observed LPN #1 checking the wanderguard for function and the Wanderguard passed testing.
4. Review of Resident #1's Nurse's Notes revealed the resident's guardian and MD was notified on 12/31/19; however, a message was left for the guardian, and the facility did not speak with the guardian until 01/02/2020. This was completed by LPN #1 and the DON.
Interview with LPN #1 on 01/10/2020 at 10:55 AM revealed she had left a message for the guardian and this was verified by phone conversation with the guardian on 01/09/2020 at 12:01 PM.
5. Review of Resident #1's Comprehensive and CNA care plan revealed they were updated on 12/31/19 by the DON and LPN #1.
6. Review of Resident #1's Comprehensive and CNA care plans revealed all interventions were in place per the care plan on 12/31/19. This was reviewed by the IDT team on 12/31/19.
7. Review of the Incident Report for the elopement, revealed all staff on duty at the time of the incident were interviewed about their response to door alarms and the resident's location. This was verified by the staff list for 12/31/19 and written statements of staff found in the incident notebook. These were completed by the Director of Nursing and the Administrator on 12/31/19.
8. Review of the elopement timeline of Resident #1 completed by the DON and Social Services Director, revealed it started on 12/31/19 and was completed on 01/03/2020.
9. Review of documented evidence in the elopement incident notebook compiled by the facility, revealed resident's clothing, temperature, weather conditions and approximate time the resident was outside of facility. This was completed by Director of Nursing, Social Services Director and Administrator on 12/31/19.
10. Review of staff education documentation related to Resident #1's revised care plans and interventions revealed all staff was educated on 12/31/19 by the Social Services Director, DON and LPN #1.
Interviews on 01/10/2020 with LPN #1 at 3:54 PM, RN #1 at 4:35 PM, RN #2 at 4:40 PM, CNA #1 at 4:49 PM, CNA #2 at 4:58 PM, CNA #3 at 4:59 PM, and CNA #4 at 5:04 PM revealed they were educated on Resident #1's care plan revisions.
11. Review of documented evidence in the elopement notebook revealed a complete head count of all residents was conducted on 12/31/19 at 4:30 PM by LPN #1 with all residents accounted for.
Interviews on 01/09/2020 with the DON at 3:47 PM; and on 01/10/2020 with LPN #1 at 3:54 PM, revealed they verified the head count in the facility of all residents on 12/31/19.
12. Record review for ten (10) residents revealed Elopement Risk Assessments were completed before 01/02/2020 by the Social Services Director (SSD).
Interview and review of audit tool with the SSD on 01/10/2020 at 3:38 PM revealed Elopement Risk Assessments were completed.
13. Review of Resident #1 and #2's records revealed there was a Wander guard order for placement check and function each shift and signed off appropriately, a wander guard in place and not expired, had behavior monitoring for exit seeking behaviors and person centered non pharmacological interventions, and had a care plan for exit seeking/elopement risk that is current and reflects the residents' person-centered, non-pharmacological behavior interventions and wanderguard. Resident #1 and #2 were the only residents identified at risk for elopement.
Review of the audit completed by the DON, MDS Coordinator and Social Services Director revealed the audit for the above information was completed on 01/02/2020.
Interviews on 01/10/2020 with the DON at 11:15 AM, SSD at 1:15 PM, and MDS Coordinator at 2:20 PM revealed the audits were completed and the Wander Guard Bracelet had been checked for function and placement each shift.
14. Review of the facility's Elopement Binders revealed, they were audited on 01/02/2020 by the DON and Social Services Director to ensure all residents had pictures and identifying information.
Interviews on 01/10/2020 with LPN #1 at 10:55 AM, DON at 11:15 AM, and SSD at 1:15 PM revealed the Elopement Binders had been updated.
Review of the Elopement Binders at each nurse's station, revealed pictures and identifying information of the residents at risk for elopement were in the binder.
15. Review of Exit doors and wanderguard alarms audits revealed they were completed by the Maintenance Director on 12/31/19.
Observation and interview with the Maintenance Director on 01/09/2020 at 11:38 AM revealed the Maintenance Director used the Wanderguard checker to ensure the doors worked properly. The doors locked down and alarm started sounding when he got within four to six feet of the door.
16. Review of Vender assessments dated 01/02/2020 revealed the Manufacturer of Door and Wanderguard alarm vendor came on site and verified the doors were working properly with no concerns.
17. Review of Education In-service records dated 12/31/19 and completed on 01/03/2020 revealed all employees were educated on the Elopement Process and response to door alarms, and following exit seeking interventions on care plans, by administrative staff which included the DON, Administrator and Staff Development Coordinator.
Interviews on 01/09/2020 with Payroll at 1:43 PM, Activities Director 2:24 PM, Maintenance Director at 2:39 PM, ADON at 12:50 PM, Director of Culinary Services at 3:30 PM, and DON at 3:47 PM; and, interviews on 01/10/2020 with LPN #1 at 3:54 PM, RN #1 at 4:35 PM, RN #2 at 4:40 PM, CNA #1 at 4:49 PM, CNA #2 at 4:58 PM, CNA #3 at 4:59 PM, CNA #7 at 5:04 PM, Human Resources Director at 5:24 PM, and Medical Records Director at 5:29 PM revealed the staff was able to verbalize education.
18. Review of the Elopement Incident Notebook revealed Elopement drills were completed on all shifts starting on 12/31/19 through 01/01/2020 by the DON, Social Service Director, Administrator, and Staff Development Coordinator.
Interviews on 01/09/2020 with Payroll at 1:43 PM, Activities Director 2:24 PM, Maintenance Director at 2:39 PM, ADON at 12:50 PM, Director of Culinary Services at 3:30 PM, and DON at 3:47 PM; and, interviews on 01/10/2020 with LPN #1 at 3:54 PM, RN #1 at 4:35 PM, RN #2 at 4:40 PM, CNA #1 at 4:49 PM, CNA #2 at 4:58 PM, CNA #3 at 4:59 PM, CNA #7 at 5:04 PM, Human Resources Director at 5:24 PM, and Medical Records Director at 5:29 PM revealed elopement drills were conducted.
19. Review of the alarm systems audits per the Maintenance Director revealed the audit was conducted on 12/31/19 with no concerns identified. Further review revealed the Administrator had verified the audits had been completed with notation the alarms were in correct working condition. The Administrator verified this with documentation in the elopement notebook.
20. Record review validated the certified technician checked functioning of doors/panels for proper functioning per documented evidence of vendor notation on 01/02/2020.
21. Observation on 01/09/2020 revealed there were signs on all exit doors to alert visitors/staff/vendors at exiting to not allow residents out of doors and to check with staff.
22. Review of the Elopement Drill documentation revealed the first weekly elopement drill was held on 01/06/2020 at 11:00 AM by the Administrator and DON. There were ten (10) staff involved.
23. Interview (Post Survey) with the Administrator on 01/20/2020 at 2:22 PM revealed summaries of the elopement drills would be completed monthly and reviewed by the QA committee.
24. Review of the Ad Hoc QAPI meeting minutes revealed the meeting was held on 12/31/19 with the Administrator, DON, and Medical Director.
Interview with the DON on 01/09/2020 at 3:47 PM revealed she attended the QAPI meeting and the attendees reviewed the information gathered regarding the elopement.
Interview with the Administr[TRUNCATED]