CHATEAU LIVING CENTER




Inspected within the last 6 months. Data reflects current conditions.
Chateau Living Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. It ranks #182 out of 264 facilities in Louisiana, placing it in the bottom half of all nursing homes in the state, and #7 out of 12 in Jefferson County, meaning only a few local options are perceived as worse. The facility's situation is worsening, with reported issues increasing from 13 in 2024 to 27 in 2025. Staffing is a major weakness, receiving a 1 out of 5 stars rating and having 49% turnover, which is concerning as staff may not stay long enough to form meaningful relationships with residents. There have been alarming incidents, including a resident who wandered off the premises and suffered a serious head injury, and another resident who sustained second-degree burns from a lighter, showing inadequate supervision and safety measures. Overall, while the facility has some staff, the numerous critical issues and poor ratings suggest a lack of reliable care.
- Trust Score
- F
- In Louisiana
- #182/264
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 49% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $159,972 in fines. Lower than most Louisiana facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 5 minutes of Registered Nurse (RN) attention daily — below average for Louisiana. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 56 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Louisiana average (2.4)
Significant quality concerns identified by CMS
Near Louisiana avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 56 deficiencies on record
Sept 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility failed to provide Activities of Daily Living (ADL) care in a t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to ensure a resident's medication was not available for administration for 1 (Resident #1) of 3 (Resident #1, Resident #2, and Resident #3) ...
Read full inspector narrative →
Jul 2025
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to protect the residents' right to be free from physical abuse by a resident for 1 (Resident #110) of 1 (Resident #110) sampled residents id...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0605
(Tag F0605)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to ensure:1. The skilled nurse documented adequate indication for use of an anti-psychotic (medication used to treat psychosis) medication u...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to ensure a resident's fingernails were maintained for 1 (Resident #174) of 2 (Resident #119, Resident #174) sampled resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record reviews, the facility failed to ensure chemicals in the beauty shop room were secured and not accessible to wandering residents. Findings:Review of the fac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to have evidence a resident's oxygen tubing was changed weekly for 1 (Resident #74) of 2 (Resident #74, Resident #187) reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observations and interviews, the facility failed to ensure food was stored in a sanitary manner. Findings:Observation on 07/21/2025 at 8:45AM revealed an employee's frozen drink was present i...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews the facility failed to ensure resident equipment and rooms were maintained...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
Based on interviews and record reviews, the facility failed to ensure an incident of resident to resident physical abuse was reported to the state agency for 1 (Resident #110) of 1 (Resident #110) sam...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
Based on interviews and record reviews, the facility failed to ensure an incident of resident to resident physical abuse was thoroughly investigated for 1 (Resident #110) of 1 (Resident #110) sampled ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record reviews, the facility failed to:1. Ensure staff used soap and water to perform hand hygiene for a resident on physician ordered contact precautions for Cl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected multiple residents
Based on observations and interviews the facility failed to maintain an effective pest control management program for 7 (Resident #16, Resident #24, Resident #67, Resident #72, Resident #95, Resident ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected multiple residents
Based on observations and interview, the facility failed to post the required nurse staffing information at the beginning of each shift daily for 3 (07/21/2025, 07/22/2025, 07/23/2025) of 3 (07/21/202...
Read full inspector narrative →
Apr 2025
5 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and interviews, the facility failed to provide a privacy cover for a urinary catheter drainage bag for 1 (Resident #R9) of 1 (Resident #R9) residents reviewed for catheters.
Findi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure expired medications were not available for res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record reviews, the facility failed to ensure medications were not left unattended at a resident's bedside for 1 (Resident #2) of 5 (Resident #1, Resident #2, Res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
Based on observations and interviews, the facility failed to serve residents' food at an acceptable temperature as required.
Findings:
In an interview on 04/08/2025 at 8:40AM, Resident #3 indicated th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure a functional call bell was available for 2 (Resident #2, Resident #R6) of 15 (Resident #1, Resident #2, Resident #3, Resident #4, Resi...
Read full inspector narrative →
Mar 2025
6 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record reviews, the facility failed to provide good personal hygiene for 1 (Resident #2) o...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observations and interviews, the facility failed to ensure
1. facility's halls were free of strong unpleasant odors for Hall A and Hall B; and,
2. debris and trash were removed from Residen...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure a Certified Nursing Assistant (CNA) notified th...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a resident diagnosed with peripheral vascular ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record reviews, and interviews, the facility failed to ensure Certified Nursing Assistants (CNAs) demonstr...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews facility failed to maintain an infection prevention and control program fo...
Read full inspector narrative →
Jan 2025
2 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
Based on observations, interviews and record reviews, the facility failed to ensure the resident's environment remained free of accident/hazards, identify and eliminate the risk of accident hazards to...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to ensure a Certified Nursing Assistant (CNA) was competent in the facility's procedure for elopement risk residents for 1 (S7CNA) of 21 (S3...
Read full inspector narrative →
Aug 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on record reviews, observation, and interviews the facility failed to ensure a resident was provided privacy during Percutaneous Endoscopic Gastrostomy (PEG) tube (a tube inserted through the sk...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on record reviews, observations, and interviews, the facility failed to ensure staff wore proper protective equipment for Enhanced Barrier Precautions (EBP) during Percutaneous Endoscopic Gastro...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observations and interviews, he facility failed to ensure water from the shower room did not leak into the hallway for 1 (Shower Room A) of 4 (Shower Room A, Shower Room B, Shower Room C, and...
Read full inspector narrative →
Jul 2024
10 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on record reviews, observations, and interviews, the facility failed to assess a resident for self-administration of medications for 2 of 53 sampled observed for self-administration of medicatio...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observations and interviews the facility failed to ensure a resident's wheelchair was in good repair and maintained in a sanitary manner for 1 resident (Resident #77) of 3 Residents (Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, the facility failed to ensure a Level I Pre-admission Screening and Resident Review (PAS...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews the facility failed to ensure site care was provided to a peripherally inserted central c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interviews the facility failed to maintain food on the steam table to at least 135 degrees Fahrenheit (F).
Findings:
Review of Centers for Medicare and Medica...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on record reviews and interview, the facility failed to accurately revise a plan of care that addressed a resident's skin condition for 1 (Resident #62) of 2 (Resident #62 and Resident #29) samp...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, the facility failed to:
1. Ensure the facility's policy was followed by failing to compl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on record reviews, observation, and interviews, the facility failed to ensure discontinued and expired medication was stored properly and was not available for resident use for 1 ( Medication {M...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
MDS Data Transmission
(Tag F0640)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interview, the facility failed to transmit the resident assessment within 14 days of completion for ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Assessment Accuracy
(Tag F0641)
Minor procedural issue · This affected multiple residents
Based on record reviews and interviews, the facility failed to ensure a resident's Minimum Data Set (MDS) assessment reflected the resident's accurate skin condition for 1 (Resident #62) of 2 (Residen...
Read full inspector narrative →
Sept 2023
16 deficiencies
2 IJ (2 affecting multiple)
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews, interviews, and observations, the facility failed to ensure residents who had a history of unsafe use o...
Read full inspector narrative →
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected multiple residents
The facility failed to be administered in a manner that enabled it to use its resources effectively and efficiently by failing to provide the necessary administrative oversight to ensure systems were ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews and interviews, the facility failed to have a written order for the physical restraint for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews, and interviews the facility failed to:
1. Ensure a resident's interventions were updated ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review the facility failed to ensure a resident with a newly developed stage 2 pre...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure proper positioning of a resident receiving a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to maintain communication with a dialysis center for 1 (Resident #49) of 1 (Resident #49) sampled resident investigated for dialysis services...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to:
1. Ensure food was not stored on the freezer floor;
2. Ensure expired beverages were not available for resident consumption;
3. Ensure kitch...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observations and interviews the facility failed to ensure the resident's ice supply was maintained according to infection control practices for 2 (Ice Chest A and Ice Chest B) of 2 (Ice Chest...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
Based on interview, and record review, the facility failed to notify a resident's representative of a change in condition. This deficient practice was identified for 1 (Resident #268) of 5 (Resident #...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0603
(Tag F0603)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure a resident was free from unnecessary isolation ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident with an identified mental health diagnosis was re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected multiple residents
Based on observation, interviews, and record reviews the facility failed to:
1. Ensure a resident's suprapubic catheter (a tube that is passed through the lower abdominal wall directly into the bladde...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview the facility failed to ensure a resident's oxygen tubing and nebulizer tubing was dated and stored properly when not in use for 2 (Resident #20 and R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure a resident's medications were available to be administered a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure a resident's medication administration was documented accura...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 3 life-threatening violation(s), $159,972 in fines. Review inspection reports carefully.
- • 56 deficiencies on record, including 3 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $159,972 in fines. Extremely high, among the most fined facilities in Louisiana. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Chateau Living Center's CMS Rating?
CMS assigns CHATEAU LIVING CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Louisiana, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Chateau Living Center Staffed?
CMS rates CHATEAU LIVING CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 49%, compared to the Louisiana average of 46%.
What Have Inspectors Found at Chateau Living Center?
State health inspectors documented 56 deficiencies at CHATEAU LIVING CENTER during 2023 to 2025. These included: 3 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 50 with potential for harm, and 3 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
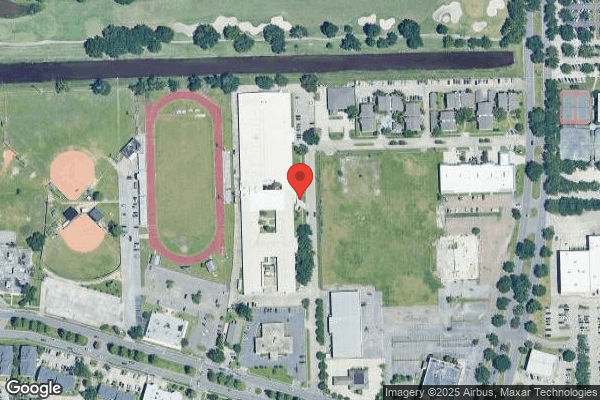
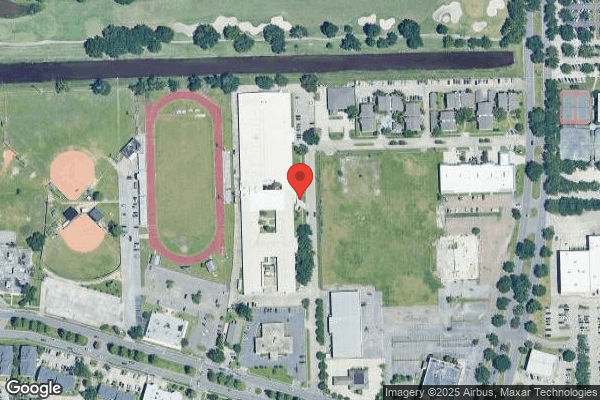
Who Owns and Operates Chateau Living Center?
CHATEAU LIVING CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PLANTATION MANAGEMENT COMPANY, a chain that manages multiple nursing homes. With 215 certified beds and approximately 184 residents (about 86% occupancy), it is a large facility located in KENNER, Louisiana.
How Does Chateau Living Center Compare to Other Louisiana Nursing Homes?
Compared to the 100 nursing homes in Louisiana, CHATEAU LIVING CENTER's overall rating (1 stars) is below the state average of 2.4, staff turnover (49%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Chateau Living Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Chateau Living Center Safe?
Based on CMS inspection data, CHATEAU LIVING CENTER has documented safety concerns. Inspectors have issued 3 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Louisiana. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Chateau Living Center Stick Around?
CHATEAU LIVING CENTER has a staff turnover rate of 49%, which is about average for Louisiana nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Chateau Living Center Ever Fined?
CHATEAU LIVING CENTER has been fined $159,972 across 2 penalty actions. This is 4.6x the Louisiana average of $34,679. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Chateau Living Center on Any Federal Watch List?
CHATEAU LIVING CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.