CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observations, and interviews, the facility failed to provide supervision to prevent elopement for 2 (Res...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observations, and interviews, the facility failed to provide supervision to prevent elopement for 2 (Resident #38 and Resident #71) of 4 (Resident #38, Resident #70, Resident #71, and Resident #83) sampled residents reviewed for elopement.
This deficient practice resulted in an Immediate Jeopardy situation on 01/08/2023 at 4:40 p.m. when Resident #71, an unsupervised resident identified as an elopement risk, eloped from the facility and was found in the facility's parking lot by staff. The continued failure to provide adequate supervision resulted in the immediate jeopardy continuing on 02/16/2023 at 10:35 p.m. when Resident #38, who was identified as an elopement risk and had severe cognitive impairment, eloped from the facility and was found in the facility's parking lot by a security guard.
S1Administrator was notified of the Immediate Jeopardy on 06/01/2023 at 4:48 p.m.
The Immediate Jeopardy was removed on 06/03/2023 at 1:56 p.m., after it was determined through observations, interviews, and record reviews, the facility implemented an acceptable Plan of Removal, prior to the survey exit, which included:
1. On 06/01/2023 a designated employee was trained by S1Administrator and assigned to provide supervision for Resident #37 and Resident #71 to keep them free of elopement and Resident #37's and Resident #71's Plan of Care was updated by the Minimum Data Set (MDS) Assessment nurse to reflect supervision. Completion: 06/02/2023.
2. On 06/02/2023 an MDS/CCC: Risk of Elopement Wandering Review was completed by facility MDS Assessment nurses on all current residents to identify other residents that may be affected due to being at risk to elope. 10 residents were identified at risk for elopement and were assigned a designated employee trained by S1Administrator to provide visual supervision at all times to keep them free of elopement and their Plans of Care were updated by a MDS Assessment nurse to reflect supervision. Completion: 06/02/2023.
On 06/02/2023 and 06/03/2023 Nursing Administration identified the 10 residents identified as a wandering risk by placing over bed signage of a W. Completion: 06/02/2023
On 06/02/2023 Nursing Administration was educated on completing MDS/CCC: Risk of Elopement Wandering Review with the admission, readmission, quarterly, significant change in condition and annual MDS by a consultant nurse. Completion: 06/02/2023.
On 06/02/2023 the S1Administrator and Nursing Administration were educated on ensuring the 10 residents identified as at risk for elopement had adequate supervision with a designated employee trained by S1Administrator and assigned to provide supervision by consultant nurse.
Completion: 06/02/2023.
Beginning on 06/01/2023 and continuing on 06/02/2023 and 06/03/2023 all onsite staff and onsite contracted agency staff were received in-service training conducted by MDS Assessment Nurses and Nursing Administration in regards to residents at risk for wandering have been identified by a W posted on the wall above their bed and in an Elopement Binder accessible to all staff and contracted agency staff at each nurses station, which contained a document with each residents name and picture and a photo document kept was located at the receptionist desk, also easily accessible by all staff and contracted agency staff. Start Date: 06/01/2023 End Date: 07/01/2023.
Moving forward, staff and contracted agency staff that have not been inn-serviced already, will receive in-service training as they are scheduled to work and also called in for training.
Facility staff and contracted agency staff will not be allowed to work until the training will be completed. 100% compliance will be obtained by 07/01/2023. Start Date: 06/01/2023 End Date: 07/01/2023.
On 06/02/2023 a Patient Wandering system designed to secure facility egresses to prevent residents at risk for eloping from exiting the facility was ordered and will be installed upon delivery. Once the Patient Wandering system is installed and staff are in-serviced on use of the system, the monitoring of residents at risk for elopement by the trained designated employee may be discontinued as advised by Quality Assurance and Process Improvement (QAPI) Committee. Start Date: 06/03/2023 End Date: 07/01/2023;
3. On 06/02/2023 Nursing Administration was educated on completing MDS/CCC: Risk of Elopement Wandering Review with the admission, readmission, quarterly, significant change in condition and annual MDS by consultant nurse. Completion: 06/02/2023.
On 06/02/2023 S1Administrator and Nursing Administration were educated on ensuring residents identified as at risk for elopement had adequate supervision with a trained designated employee assigned to provide supervision by consultant nurse. Completion: 06/02/2023.
Beginning on 06/01/2023 and continuing on 06/02/2023 and 06/03/2023 all onsite staff and onsite contracted agency staff were received in-service training conducted by MDS Assessment Nurses and Nursing Administration in regards to residents at risk for wandering have been identified by a W posted on the wall above their bed and in an Elopement Binder accessible to all staff and contracted agency staff at each nurses station which contains a document with each resident's name and picture and the photo document kept is located at the receptionist desk, also easily accessible by all staff and contracted agency staff. Start Date: 06/01/2023 End Date: 07/01/2023.
Moving forward staff and contracted agency staff that have not been in-serviced already, will receive in-service training as they are scheduled to work and also called in for training.
Facility staff and contracted agency staff will not be allowed to work until the training is completed. 100% compliance will be obtained by 07/01/2023. Start Date: 06/01/2023 End Date: 07/01/2023.
On 06/02/2023 a Patient Wandering system designed to secure facility egresses to prevent identified residents at risk for elopement from exiting the facility was ordered and will be installed upon delivery. Once the Patient Wandering system is installed and staff are in-serviced on use of the system, the monitoring of residents at risk for elopement by trained designated employee may be discontinued as advised by QAPI Committee;
4. S1Administrator, S2Director of Nursing (DON) and/or Designee will conduct 5 random chart audits of residents who have been admitted , readmitted , had quarterly or annual MDS review, or significant change in condition for completion of MDS/CCC: Risk of Elopement Wandering Review.
Administrator and/or Designee will conduct visual audits for the presence of trained designated employee supervising residents identified as at risk for elopement and documentation review audits for all residents identified as at risk for elopement. These audits will occur 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. Begin Date: 06/03/2023 End Date: 07/01/2023 Results of audits including tracking and trends will be reviewed weekly in QAPI meeting, and any identified issues will be addressed with re-education, plan modification and progressive discipline; and,
5. Completion Date: 06/03/2023.
The deficient practice had the likelihood to cause serious harm to the remaining 8 residents identified as elopement risks by the facility.
Findings:
Review of the facility's Wandering Resident Policy and Procedure revealed, in part, it is the policy of the facility to identify residents who walk or wheel about unrestricted and are a threat to leave the facility unattended due to their confusion, the purpose is to ensure the resident's safety utilizing the least restrictive means necessary.
Resident #71
Review of the facility's Incident Report entered on 01/08/2023 at 7:58pm revealed, in part, Resident #71 was found outside the facility's back door near the dumpster. Further review revealed staff on the unit were in another resident's room at the time Resident #71 had gotten outside. Review revealed Resident #71 had pushed the push release paddle, opened the door while in her wheelchair, and exited the facility. Further review revealed the door did not have an alarm.
Review of Resident #71 medical record revealed Resident #71 admitted to the facility initially on 12/03/2020 with a readmission date of 11/04/2021 with a diagnosis of Dementia.
Review of Resident #71's Quarterly Minimum Data Set (MDS) dated [DATE] revealed in part, Resident #71 had a BIMS (Brief Interview Mental Status) score of 5 indicating severe cognitive impairment. Further review revealed, Resident #71 used a wheelchair as her mobility device.
Review of Resident #71 current Comprehensive Care plan revealed, in part, Resident #71 was care planned for being at risk for elopement related to wandering and attempting to leave the facility unsupervised with interventions that included alarms placed on exit doors, observe Resident #71's location every hour daily, and Monitor Resident #71's location every 2 hours on even hours.
Review of Resident #71's current physician orders revealed, in part, an order with a start date of 02/17/2023 that read Resident #71 was an elopement risk and needed to be rounded on every 2 hours on the even hours.
Review of Resident #71's Electronic Medication Administration Record (eMAR) for February 2023 revealed documentation for rounds completed on Resident #71 every 2 hours on even hours that started on 02/17/2023 at 7:00pm. Further review revealed no documentation on 02/17/2023 for the time of 7:00 p.m., on 02/19/2023 for the time of 7:00 p.m, on 02/23/2023 for the time of 7:00 p.m, and on 02/25/2023 for the time of 7:00 a.m.
Review of Resident #71's March 2023 eMAR revealed, in part, an order that stated elopement risk: round on resident every 2 hours on even hours every day and night shift. Further review revealed it was documented from 03/01/2023 through 03/31/2023 on once each shift for the 8:00 a.m-8:00 p.m. shift and once each shift for the 8:00 p.m.-8:00 a.m.
Review of Resident #71's April 2023 eMAR revealed, in part, an order that stated elopement risk: round on resident every 2 hours on even hours every day and night shift. Further review revealed it was documented from 04/01/2023 through 04/30/2023 on once each shift for the 8:00 a.m-8:00 p.m. shift and once each shift for the 8:00 p.m.-8:00 a.m.
Review of Resident #71's May 2023 eMAR revealed, in part, an order that stated elopement risk: round on resident every 2 hours on even hours every day and night shift. Further review revealed it was documented 05/01/2023 through 05/31/2023 on once each shift for the 8:00 a.m-8:00 p.m. shift and once each shift for the 8:00 p.m.-8:00 a.m.
Review of Resident #71's Documentation Survey Report Form for February 2023 revealed documentation for rounds completed on Resident #71 every 2 hours on odd hours that started on 02/17/2023 at 7:00 a.m. that were documented once a shift at 7:00 a.m. and 7:00 p.m. Further review revealed no documentation on 02/17/2023 for the time of 7:00 a.m., on 02/19/2023 for the time of 7:00 p.m, on 02/23/2023 for the time of 7:00 p.m, and on 02/25/2023 for the time of 7:00 a.m.
Review of Resident #71's Documentation Survey Report Form for March 2023 revealed documentation for rounds completed on Resident #71 every 2 hours on odd hours were documented once a shift at 7:00 a.m. and 7:00 p.m. Further review revealed no documentation on 03/03/2023 for the time of 7:00 p.m., on 03/11/2023 for the time of 7:00 p.m., on 03/13/2023 for the time of 7:00 a.m. and 7:00 p.m., and on 03/21/2023 for the time of 7:00 p.m.
Review of Resident #71's Documentation Survey Report Form for April 2023 revealed documentation for rounds completed on Resident #71 every 2 hours on odd hours were documented once a shift at 7:00 a.m. and 7:00 p.m. Further review revealed no documentation on 04/08/2023 for the time of 7:00 p.m. and on 04/28/2023 for the time of 7:00 p.m.
Review of Resident #71's Documentation Survey Report Form for May 2023 revealed documentation for rounds completed on Resident #71 every 2 hours on odd hours were documented once a shift at 7:00 a.m. and 7:00 p.m. Further review revealed no documentation on 05/03/2023 for the time of 7:00 p.m., on 05/12/2023 for the time of 7:00 a.m. and 7:00 p.m., on 05/17/2023 for the time of 7:00 p.m., 05/19/2023 for the time of 7:00 p.m., 05/22/2023 for the time of 7:00 p.m., 05/26/2023 for the time of 7:00 p.m., 05/27/2023 for the time of 7:00 a.m., and on 05/31/2023 for the time of 7:00 p.m.
Review of Resident #71's nurse's notes revealed a nurses note with a date of 01/08/2023 at 4:40pm which stated Resident #71 was found in the parking lot by a housekeeper. Review revealed Resident #71 stated she was looking for a bathroom. Further review revealed Resident#71's RP was notified at 4:10pm and expressed concerns about a door alarm being placed on the facility exit door.
Review of Resident #71's nurse's notes revealed a nurses note with a date of 01/31/2023 at 9:55pm which stated Resident #71 attempted to wander off of the unit on occasions.
Review of Resident #71's nurses notes revealed a nurse's note with a date of 03/10/2023 at 6:00pm which stated, a dietary worker was walking to the unit and stated your resident was almost out of the building, if I wasn't walking the hallway she would have been gone.
Review of Resident #71's Wandering Risk Assessment completed on 11/01/2023 revealed, in part, Resident #71 was at low risk for wandering. Further review revealed the assessment documented Resident #71 as forgetful with a short attention span, with a diagnosis of vascular dementia, and attempted to exit the building.
Review of Resident #71's Wandering Risk Assessment completed on 01/08/2023 revealed, in part, Resident #71 was at moderate risk for wandering. Further review revealed the assessment documented Resident #71 as disoriented and forgetful with short attention span. Review revealed Resident #71 had a diagnosis of early dementia, had a known history of wandering, wandered in the hallway, and attempted to exit the building
Review of Resident #71's Wandering Risk Assessment completed on 01/31/2023 revealed, in part, Resident #71 was at low risk for wandering. Further review revealed the assessment documented Resident #71 as forgetful with a short attention span, with a diagnosis of vascular dementia, and attempted to exit the building.
Review of Resident #71's Wandering Risk Assessment completed on 03/10/2023 revealed, in part, Resident #71 was at moderate risk for wandering. Review revealed the assessment documented Resident #71 as forgetful with a short attention span. Review revealed Resident #71 had a diagnosis of early dementia, had a known history of wandering, wandered in other rooms, the hallway, and restricted area, and attempted to exit the building. Further review revealed, Resident #71 was being transferred from her current unit to another unit and would receive a room change.
Review of the facility's hourly rounding log for the time period of 03/13/2023 through 04/29/2023 revealed no documentation of hourly rounding for Resident #71 on 03/15/2023,
04/08/2023, and 04/24/2023.
Observation on 05/31/2023 at 11:41 a.m. revealed, Resident #71 sitting in the recliner in Hall V's dayroom. Further observations revealed no staff present on Hall V at this time.
In an interview on 05/30/2023 at 10:51 a.m., S38LPN stated Resident #71 used to wander off the unit frequently. S38LPN stated she had gotten out of the facility a few times.
In an interview on 05/31/2023 at 11:41 a.m., S17CNA stated Resident #71 used her wheelchair to move around throughout the facility without difficulty. S17CNA further stated Resident #71 did not have any restrictions with supervision and she could attend events and move throughout the facility unsupervised.
Observation on 05/31/2023 at 11:50 a.m. revealed, the exit door located on Hall V was disarmed and unlocked.
Observation on 05/31/2023 at 5:13 p.m. revealed Resident #71 sitting in the dining room without staff supervision.
In an interview on 05/31/2023 at 12:15 p.m. S37LPN stated Resident #71 was able to roll herself around in her wheelchair without any difficulty. S37LPN stated Resident #71 was a wander risk and had gotten off of Hall V a few times. S37LPN stated she frequently disappears and staff have to go find her.
Observation on 06/01/2023 at 12:30 p.m. revealed the exit door located on Hall V disarmed and unlocked.
Observation on 06/01/2023 at 2:35 p.m. revealed, a visitor exited the door on Hall V. Further observation revealed the door was disarmed and unlocked.
Observation on 06/01/2023 at 4:14 p.m. revealed Hall U's exterior door with a red locking device that was in the off position.
Resident #38
Review of the facility's Incident Report entered on 02/17/2023 at 1:07 p.m. revealed, in part, a description that stated: Resident #38 eloped from the facility and was found by a security guard in the front of the building on the sidewalk between the front entrance door and the facility parking lot. Further review revealed Resident #38 was placed on 15 minute visual observation. Review of the incident investigation revealed the front doors of the facility had been locked for the night, the side door of the lobby did not lock and opened with a panic bar. It does not have an alarm. It is believed that Resident #38 walked to the lobby and exited the building from the side door. Resident #38 was not able to say how she got out of the facility or where she was going. Resident #38 was found walking on sidewalk between the exit door and the front parking lot approximately 5 feet from the door. No staff inside the building saw Resident #38 exit from the side lobby door. Plans have are being made by the company that will purchase the facility to install a Wander Guard system and video surveillance cameras. The facility is now purchasing AngelSense devices for resident to wear which includes a geofencing feature that will alert staff if resident walks through exit door. This will be in use until the Wander Guard system is installed.
Review of the facility's incident report dated 02/16/2023, revealed while completing medication pass, S42LPN was called to the desk phone through the facility's overhead page and was notified that a security officer was at the entrance door with Resident #38. S42LPN then went to the facility's main entrance to retrieve Resident #38. The security guard notified staff that Resident #38 was found walking in parking lot area near the facility entrance door.
Review of Resident #38 medical record revealed Resident #38 admitted to the facility on [DATE] with a diagnosis of Dementia and anxiety.
Review of Resident #38's current physician orders revealed, in part, an order with a start date of 03/30/2023 that read Resident #38 was an elopement risk and needed to be rounded on every 2 hours on the even hours.
Review of Resident #38's Quarterly Minimum Data Set (MDS) dated [DATE] revealed in part, Resident #38 had a BIMS (Brief Interview Mental Status) score of 5 indicating severe cognitive impairment. Review revealed, Resident #38 used a wheelchair as her mobility device and had no wander/elopement alarm documented.
Review of Resident #38 current Comprehensive Careplan with a date of 02/16/2023, revealed, in part, Resident #38 was care planned for being at risk for elopement related to wandering and attempting to leave the facility unsupervised with interventions that included alarms placed on exit doors, apply stop signs to exit doors, assist resident to and from activities and dining area daily, allow resident to wander on unit and in courtyard under supervision; redirect resident as needed. Further review revealed if Resident #38 had behaviors observed they should be documented in Resident #38's progress notes and Resident #38's Responsible Party and Medical Director should be notified.
Review of Resident #38's Wandering Risk Assessment completed on 11/29/2022 revealed, in part, Resident #38 was at moderate risk for wandering. Review revealed the assessment documented Resident #38 as forgetful with a short attention span and does not understand her surroundings. Further review revealed Resident #38 was independent with mobility, had a diagnosis of early dementia, and had a known history of wandering.
Review of Resident #38's Elopement Risk Assessment, dated 02/16/2023, revealed in part, resident, Resident #38 was cognitively impaired. Review revealed, Resident #38 ambulated independently, wandered aimlessly, and could not be found by staff for 15 minutes. Further review revealed Resident #38 was found in another resident's bathroom.
Review of Resident #38's Wandering Risk Assessment completed on 02/17/2023 at 7:58 a.m. revealed, in part, Resident #38 was at high risk for wandering. Review revealed the assessment documented Resident #38 as disoriented with a short attention span and does not understand her surroundings. Review revealed Resident #38 was independent with mobility, had a diagnosis of early dementia, had a known history of wandering, wandered in the hallway, and had attempted to exit the building
Review of Resident #38's Wandering Risk Assessment completed on 02/17/2023 at 11:04 a.m. revealed, in part, Resident #38 was at moderate risk for wandering. Review revealed the assessment documented Resident #38 as disoriented with a short attention span and does not understand her surroundings. Review revealed Resident #38 was independent with mobility, had a diagnosis of early dementia, had a known history of wandering, wandered in the hallway, and had attempted to exit the building
Review of Resident #38's Wandering Risk Assessment completed on 02/28/2023 at 5:14 a.m. revealed, in part, Resident #38 was at high risk for wandering. Review revealed the assessment documented Resident #38 as disoriented with a short attention span and does not understand her surroundings. Review revealed Resident #38 was independent with mobility, had a diagnosis of early dementia, had a known history of wandering, wandered in the hallway, and had attempted to exit the building
Review of Resident #38's Wandering Risk Assessment completed on 05/31/2023 at 9:04 a.m. revealed, in part, Resident #38 was at moderate risk for wandering. Review revealed the assessment documented Resident #38 as disoriented with a short attention span and does not understand her surroundings. Review revealed Resident #38 was independent with mobility, had a diagnosis of early dementia, had a known history of wandering, wandered in the hallway, and had attempted to exit the building.
Review of Resident #38's February 2023 eMAR revealed, in part, an order that stated elopement risk: round on resident every 2 hours on even hours every day and night shift. Review revealed it was documented from 02/17/2023 through 02/28/2023 once each shift for the 7:00 a.m-7:00 p.m. shift and once each shift for the 7:00 p.m.-7:00 a.m. Further review revealed an additional order that stated observe for exit seeking behavior every hour beginning on 02/17/2023 at 8:00am hourly until 02/20/2023 at 9:00am.
Review of Resident #38's March 2023 eMAR revealed, in part, an order that stated elopement risk: round on resident every 2 hours on even hours every day and night shift. Further review revealed it was documented from 03/01/2023 through 03/31/2023 on once each shift for the 7:00 a.m-7:00 p.m. shift and once each shift for the 7:00 p.m.-7:00 a.m.
Review of Resident #38's April 2023 eMAR revealed, in part, an order that stated elopement risk: round on resident every 2 hours on even hours every day and night shift. Further review revealed it was documented from 04/01/2023 through 04/30/2023 on once each shift for the 7:00 a.m-7:00 p.m. shift and once each shift for the 7:00 p.m.-7:00 a.m.
Review of Resident #38's May 2023 eMAR revealed, in part, an order that stated elopement risk: round on resident every 2 hours on even hours every day and night shift. Further review revealed it was documented 05/01/2023 through 05/31/2023 on once each shift for the 7:00 a.m-7:00 p.m. shift and once each shift for the 7:00 p.m.-7:00 a.m.
Review of Resident #38's Documentation Survey Report Form for February 2023 revealed documentation for rounds completed on Resident #38 every 2 hours on odd hours that started on 02/17/2023 at 7:00 a.m. that were documented once a shift at 7:00 a.m. and 7:00 p.m. Review revealed no documentation on 02/17/2023 for the time of 7:00 a.m. and 7:00 p.m., on 02/24/2023 for the time of 7:00 p.m, on 02/27/2023 for the time of 7:00 a.m, and on 02/28/2023 for the time of 7:00 p.m. Further review revealed on 0/28/2023 at the time of 7:00 p.m. the facility documented the task was not applicable.
Review of Resident #38's Documentation Survey Report Form for March 2023 revealed documentation for rounds completed on Resident #38 every 2 hours on odd hours that were documented once a shift at 7:00 a.m. and 7:00 p.m. Review revealed no documentation on 03/01/2023 for the time of 7:00 p.m., on 03/03/2023 for the time of 7:00 a.m, on 03/06/2023 for the time of 7:00 p.m, on 03/11/2023 for the time of 7:00 p.m., on 03/21/2023 for the time of 7:00 p.m., and on 03/30/2023 for the time of 7:00 p.m. Further review revealed on 03/17/2023 at the time of 7:00 p.m., 03/22/2023 at the time of 7:00 p.m., 03/24/2023 at the time of 7:00 p.m., 03/25/2023 at the time of 7:00 p.m. 03/29/2023 at the time of 7:00 p.m., and 03/31/2023 at the time of 7:00 p.m. the facility documented the task was not applicable.
Review of Resident #38's Documentation Survey Report Form for April 2023 revealed documentation for rounds completed on Resident #38 every 2 hours on odd hours that were documented once a shift at 7:00 a.m. and 7:00 p.m. Review revealed no documentation on 04/07/2023 for the time of 7:00 p.m. and on 04/18/2023 for the time of 7:00 p.m. Further review revealed on 04/03/2023 at the time of 7:00 p.m., 04/04/2023 at the time of 7:00 p.m., 04/13/2023 at the time of 7:00 p.m., 04/17/2023 at the time of 7:00 p.m. 04/19/2023 at the time of 7:00 p.m., 04/22/2023 at the time of 7:00 p.m., 04/23/2023 at the time of 7:00 p.m., 04/27/2023 at the time of 7:00 p.m., and 04/28/2023 at the time of 7:00 p.m. the facility documented the task was not applicable.
Review of Resident #38's Documentation Survey Report Form for May 2023 revealed documentation for rounds completed on Resident #38 every 2 hours on odd hours that were documented once a shift at 7:00 a.m. and 7:00 p.m. Review revealed no documentation on 05/01/2023 for the time of 7:00 p.m., 05/05/2023 for the time of 7:00 p.m., and on 05/24/2023 for the time of 7:00 p.m. Further review revealed on 05/02/2023 at the time of 7:00 p.m., 05/03/2023 at the time of 7:00 p.m., 05/06/2023 at the time of 7:00 p.m., 05/07/2023 at the time of 7:00 p.m., 05/08/2023 at the time of 7:00 p.m., 05/09/2023 at the time of 7:00 a.m., 05/11/2023 at the time of 7:00 p.m., 05/16/2023 at the time of 7:00 p.m., 05/17/2023 at the time of 7:00 p.m., 05/20/2023 at the time of 7:00 p.m., 05/21/2023 at the time of 7:00 p.m., 05/25/2023 at the time of 7:00 p.m., and 05/30/2023 at the time of 7:00 p.m. the facility documented the task was not applicable.
Review of Resident #38's nurse's notes revealed a nurse's note with a date of 02/16/2023 at 10:35 p.m which stated S42LPN was called to the desk phone through the facility's overhead page and was notified that a security officer was at the entrance door with Resident #38. S42LPN then went to the facility's main entrance to retrieve Resident #38. The security guard notified staff that Resident #38 was found walking in parking lot area near the facility entrance door.
Review of Resident #38's nurse's notes revealed a nurse's note with a date of 0/28/2023 at 11:39 p.m. which stated Resident #38 was observed at times wandering in another resident's rooms.
Observation on 05/31/2023 at 11:36 a.m., revealed Resident #38 lying in bed watching television without direct staff supervision.
In an interview on 05/31/2023 11:54 a.m., S39CNA stated Resident #38 was a wanderer and was able to ambulate independently. S39CNA stated Resident #38 has had many incidents of elopement because she is [NAME]. S39CNA further stated Resident #38 would specifically wait for someone to turn around or tend to another resident and then she will attempt to elope.
Observation on 05/31/2023 at 12:46 p.m. revealed Resident #38 ambulating without assistance in the Hall Z day room.
In an interview on 05/31/2023 at 12:47 p.m., S40CNA, stated she was the CNA on Hall Z at this time. S40CNA stated she was not aware of any residents who resided on the unit who were identified as a wanderer. S40CNA further stated this was her second day working at the facility.
In an interview on 05/31/2023 at 2:51 p.m., S35LPN stated Resident #38 is independent and can ambulate without assistive devices. S35LPN stated Resident #38 had a diagnosis of dementia and had wandering behaviors. S35LPN stated Resident #38 did not have a wanderguard in use at this time. S35LPN further stated staff just try to keep an eye out on Resident #38 to prevent her from eloping.
Observation on 05/31/2023 1:12 p.m., revealed the exit door to the parking lot on Hall Y was unlocked. Observation revealed surveyor able to open the door at this time and no alarm sounded. Observation further revealed no signage on the door.
Observation on 06/01/2023 at 7:39 a.m. revealed, Resident #38 sitting in her chair in her room. Observation further revealed no CNA was in direct sight of Resident #38.
In an interview on 06/01/2023 at 7:51 a.m., S25Receptionist stated staff was not always present at facility's front entrance door.
In an interview on 06/01/2023 at 8:15 a.m. S10Clinical Coordinator confirmed Resident #38 had eloped from the facility. S10Clinical Coordinator stated when residents got out of the facility, it was generally out of a door that was present on the unit they resided on. S10Clinical Coordinator stated the wanderguard system could have prevented Resident #38 and Resident #71 from eloping out of the facility.
In an interview on 06/01/2023 at 8:41 a.m. S45CNA stated Resident #38 was an elopement risk. S45CNA stated some of the doors have alarms on them, but there is no wanderguard system in place.
Observation on 06/01/2023 at 8:44 a.m. revealed the door across from the dining room on Hall Y was unlocked, unalarmed, and not supervised. At this time, the surveyor was able to open the door.
In an interview on 06/01/2023 at 8:49 a.m. S44MDSNurse stated following Resident #38's incident of elopement on 02/16/2023, the intervention placed by the facility was for staff to keep an eye on her.
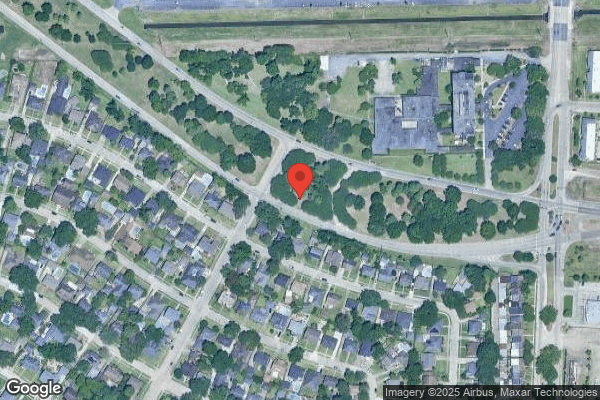
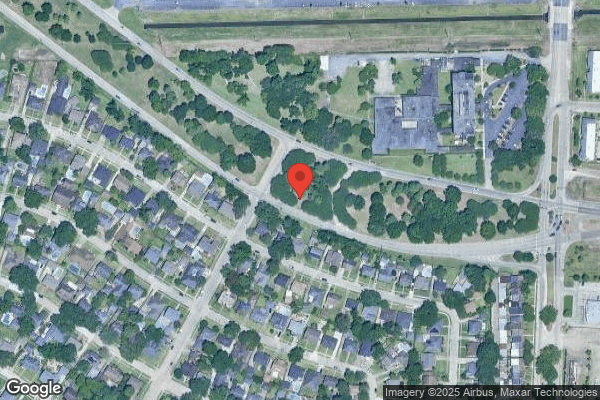
In an interview on 06/01/2023 9:21 a.m. S42LPN stated on 02/16/2023 Resident #38 eloped through the front door of the facility and Resident #38 was found by the school's, next to the facility, security guard. S42LPN stated the incident occurred at night and there wasn't as many staff in the facility. S42LPN stated Resident #38 still had the potential to elope because she can ambulate without assistance.
Observation on 06/01/23 at 9:30 a.m. revealed, the door across from the dining room on Hall Y unlocked. At this time the surveyor was able to open the door and no alarm sounded.
Observation on 06/01/2023 at 9:37 a.m. revealed, the exit door on Hall Z across from Room B had a red alarm attachment with the key hole turned to off. At this time the surveyor pushed the door open and no alarm sounded.
In an interview on 06/01/2023 at 9:40 a.m., S4 LPN stated Resident #38 and Resident #71 had both eloped while she was working at the facility. S4LPN further stated she assumed both residents had eloped off their previous unit out of the back door and the door had no alarm
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected multiple residents
Based on interviews, observation, and record review, the facility failed to ensure it was administered in a manner that enabled it to use its resources effectively and efficiently to have a system in ...
Read full inspector narrative →
Based on interviews, observation, and record review, the facility failed to ensure it was administered in a manner that enabled it to use its resources effectively and efficiently to have a system in place to prevent and control the transmission of COVID-19 infections in the facility and to provide supervision to residents to prevent elopement by:
1.)failing to ensure staff quarantined and tested a resident (Resident #3) upon symptom onset of COVID-19;
2.)failing to ensure staff quarantined a resident ( Resident #27) who tested positive for Covid-19;
3.)failing to ensure staff used personal protective equipment (PPE) with COVID-19 positive residents (Resident #3 and Resident #27);and
4.) failing to provide supervision to keep residents (Resident #38 and Resident #71) free from elopement
This deficient practice resulted in an Immediate Jeopardy situation on 01/08/2023 at 4:40 p.m. when Resident #71, an unsupervised resident identified as an elopement risk, eloped from the facility and was found in the facility's parking lot by staff. The continued failure to provide adequate supervision resulted in the immediate jeopardy continuing on 02/16/2023 at 10:35 p.m. when Resident #38, who was identified as an elopement risk and had severe cognitive impairment, eloped from the facility and was found in the facility's parking lot by a security guard.
This deficient practice resulted in an Immediate Jeopardy situation for Resident #3 on 05/28/2023 at 11:30 a.m., when Resident #3 who displayed symptoms of COVID-19 and was not quarantined or tested by the facility. On 05/31/2023 at 11:46 a.m., Resident #27 tested positive for COVID-19 and was not placed on quarantine until 1:17p.m. On 05/31/2023 at 12:43 p.m. S23Agency Certified Nursing Assistant (CNA) entered Resident #27's, a symptomatic COVID-19 positive resident, room without a gown, gloves, or face shield in place. On 05/31/2023 at 1:02 p.m. S24Housekeeper entered Resident #27's room to deliver a clothing item without a gown, gloves, or face shield in place and then entered the housekeeping closet to stock her housekeeping cart. On 5/31/2023 at 1:33 p.m. S4LPN exited Resident #3's, a symptomatic COVID-19 positive resident, room with a contaminated yellow gown in her hands and entered Hall Y Dayroom. Resident #59 and Resident #74 tested positive for COVID-19 on 06/04/2023. As of 06/06/2023, there were 4 active resident COVID-19 cases in the facility.
S1Administrator was notified of the Immediate Jeopardy on 06/01/2023 at 4:48 p.m.
The Immediate Jeopardy was removed on 06/04/2023 at 4:03 p.m., after it was determined through observations, interviews, and record reviews, the facility implemented an acceptable Plan of Removal, prior to the survey exit, which included:
1. Resident #3 was placed on isolation precautions on 05/30/2023 and Resident #27 was placed on isolation precautions on 5/31/2023. This was completed on 06/01/2023.
Resident # 3 was tested for COVID-19 on 05/30/2023, and placed on isolation precautions. Resident #27 was tested for COVID-19 with a positive result and placed on isolation precautions on 05/31/2023. This was completed on 06/01/2023.
On 06/01/2023 onsite staff and contracted agency staff were inserviced by S2Directior of Nursing (DON) and S3Assistant Director of Nursing//Infection Preventionist (S3ADON/IP) regarding identification of COVID-19 symptoms, staff responsibilities when symptoms of COVID-19 were observed, and transmission-based precautions including the use of personal protective equipment (PPE) with COVID-19 positive residents in accordance with Centers for Disease Control (CDC) guidelines. Training by S2DON and S3ADON/IP and/or Designee would continue as staff and contracted agency staff on alternate schedules reported to work. Staff and contracted agency staff would not be allowed to work until training was completed. This began on 06/01/2023 and will end on 06/09/2023.
On 06/02/2023 onsite licensed nurses and onsite contracted agency licensed nurses were inserviced by S2DON and S3ADON/IP regarding the need to quarantine residents with symptoms of COVID-19, while determining if a resident was positive for COVID-19, and testing residents upon COVID-19 symptom onset in accordance with CDC guidelines. Training would continue as licensed nursing staff and contracted agency licensed nursing staff on alternate schedules reported to work. Licensed Nursing Staff and contracted agency licensed nursing staff would not be allowed to work until training is completed. This began on 06/02/2023 and will end on 06/09/2023.
On 06/01/2023 designated employees were trained by S1Administrator, and assigned to provide supervision for Resident #37 and Resident #71 to keep them free of elopement, and their Plan of Care was updated by the facility's MDS Assessment nurses to reflect supervision. This was completed on 06/02/2023.
2. All other 86 residents that resided in the facility had the potential to be affected.
On 05/31/2023 S2DON, S3ADON/IP, and Nursing Administration conducted broad based testing of all residents and onsite staff. Resident #27 tested positive for COVID-19 and was placed on isolation precautions on 05/31/2023. Broad based testing was repeated on 06/02/2023 and all tests were negative. Broad based testing conducted by S2DON, S3ADON/IP, and Nursing Administration would continue every 3 days until test results were negative for a two week period. This began on 05/31/2023 and would end once all negative tests were obtained for two weeks.
In order to keep the current resident population free from contracting COVID-19, S2DON and S3ADON/IP were educated on 06/02/2023 regarding Infection Control policies and procedures and Infection Surveillance policies by the consultant nurse. This was completed on 06/02/2023.
On 06/01/2023 onsite staff and contracted agency staff were inserviced by S2DON and S3ADON/IP regarding identification of COVID-19 symptoms, staff responsibilities when symptoms of COVID-19 were observed, and transmission-based precautions including the use of personal protective equipment (PPE) with COVID-19 positive residents in accordance with CDC guidelines. Training by S2DON and S3ADON/IP and/or Designee would continue as staff and contracted agency staff on alternate schedules reported to work. Staff and contracted agency staff would not be allowed to work until training was completed. This began on 06/01/2023 and will end on 06/09/2023.
On 06/02/2023 an MDS/CCC: Risk of Elopement Wandering Review was completed by facility's MDS Assessment nurses on all current residents to identify other residents that may be affected due to being at risk to elope. 10 Residents were identified as being at risk for elopement, and were assigned a designated employee trained by S1Administrator to provide visual supervision at all times to keep them free of elopement, and their Plans of Care were updated by facility's MDS Assessment nurses to reflect supervision. This was completed on 06/02/2023.
On 06/02/2023 and 06/03/2023 Nursing Administration indicated that the 10 residents identified as a wandering risk had signage of a W placed over bed. This was completed on 06/02/2023.
On 06/02/2023 Nursing Administration was educated on completing the MDS/CCC: Risk of Elopement Wandering Review with the admission/readmission, quarterly, a significant change in condition and annual MDS by the consultant nurse. This was completed on 06/02/2023.
On 06/02/2023 the S1Administrator and Nursing Administration were educated on ensuring the 10 residents identified as at risk for elopement had adequate supervision with a designated employee trained by S1Administrator and were assigned to provide supervision by the consultant nurse. This was completed on 06/02/2023.
Beginning on 06/01/2023 and continued on 06/02/2023 and 06/03/2023, all onsite staff and onsite contracted agency staff received inservice training conducted by facility's MDS Assessment Nurses and Nursing Administration in regards to residents at risk for wandering identified by a W posted on the wall above their bed, and in an Elopement Binder, accessible to all staff and contracted agency staff, at each nurses station, which contained a document with each residents name and picture and a photo document located at the receptionist desk, also easily accessible by all staff and contracted agency staff. This began on 06/01/2023 and will end on 07/01/2023.
Moving forward, staff and contracted agency staff that were not inserviced already, would receive inservice training as they were scheduled to work, and were also called in for training. Facility staff and contracted agency staff would not be allowed to work until the training was completed. 100% compliance would be obtained by 06/09/2023. This began on 06/01/2023 and will end on 06/09/2023.
On 06/02/2023 a Patient Wandering system designed to secure facility egresses to prevent residents at risk for eloping from exiting the facility was ordered, and would be installed upon delivery. Once the Patient Wandering system would be installed, and staff were inserviced on use of the system, the monitoring of residents at risk for elopement by trained designated employee would be discontinued as advised by the QAPI Committee. This began on 06/03/2023 and will end on 07/01/2023.
3. On 06/03/2023 S1Administrator was educated regarding job description and responsibilities by President of facility's management company. This was completed on 06/03/2023.
Responsible Employee: S3ADON/IP was responsible for ensuring that Infection Control policies and procedures and Infection Surveillance policies were implemented and that staff were inserviced and monitored for adherence to the policies and procedures to prevent the transmission of COVID-19. S2DON would provide oversight of S3ADON/IP that ensured compliance of the Infection Prevention and Control Program.
On 06/02/2023 S2DON and S3ADON/IP were educated on Infection Control policies and procedures and Infection surveillance policies by the consultant nurse. This was completed on 06/02/2023.
On 06/01/2023 onsite staff and contracted agency staff were inserviced by S2DON and S3ADON/IP regarding identification of COVID-19 symptoms, staff responsibilities when symptoms of COVID-19 were observed, and transmission-based precautions including the use of personal protective equipment (PPE) with COVID-19 positive residents in accordance with CDC guidelines. Training by S2DON and S3ADON/IP and/or Designee would continue as staff and contracted agency staff on alternate schedules reported to work. Staff and contracted agency staff would not be allowed to work until training was completed. This began on 06/01/2023 and will end on 06/09/2023.
On 06/01/2023 licensed nurses onsite and contracted agency licensed nurses were inserviced by S2DON and S3ADON/IP regarding the need to quarantine residents with symptoms of COVID-19, while determining if resident was positive for COVID-19, and testing residents upon COVID-19 symptom onset in accordance with CDC guidelines. Training would continue as licensed staff nursing and contracted agency licensed nurses on alternate schedules reported to work. Licensed Nursing Staff and contracted agency licensed nursing staff would not be allowed to work until training was completed. This began on 06/01/2023 and will end on 06/09/2023.
On 06/01/2023 licensed nurses onsite and contracted agency licensed nurses were inserviced by S2DON and S3ADON/IP regarding the need to quarantine residents with symptoms of COVID-19, while determining if resident was positive for COVID-19, and testing residents upon COVID-19 symptom onset in accordance with CDC guidelines. Training would continue as licensed staff nursing and contracted agency licensed nurses on alternate schedules reported to work. Licensed Nursing Staff and contracted agency licensed nursing staff would not be allowed to work until training was completed. This began on 06/01/2023 and will end on 06/09/2023.
On 06/02/2023 S2DON and S3ADON/IP were educated on Infection Control policies and procedures and Infection surveillance policies by the consultant nurse. This was completed on 06/02/2023.
On 06/02/2023 Nursing Administration was educated on completing the MDS/CCC: Risk of Elopement Wandering Review with the admission/readmission, quarterly, a significant change in condition and annual MDS by the consultant nurse. This was completed on 06/02/2023.
On 06/02/2023 S1Administrator and Nursing Administration were educated on ensuring residents identified as at risk for elopement had adequate supervision with a trained designated employee assigned to provide supervision by the consultant nurse. This was completed on 06/02/2023.
Beginning on 06/01/2023 and continued on 06/02/2023, and 06/03/2023 all onsite staff and onsite contracted agency staff received inservice training conducted by facility's MDS Assessment Nurses and Nursing Administration in regards to residents at risk for wandering identified by a W posted on the wall above their bed, and in an Elopement Binder, accessible to all staff and contracted agency staff, at each nurses station, which contained a document with each residents name and picture and a photo document located at the receptionist desk, also easily accessible by all staff and contracted agency staff. This began on 06/01/2023 and will end on 07/01/2023.
Moving forward, staff and contracted agency staff that were not inserviced already, would receive inservice training as they were scheduled to work, and were also called in for training. Facility staff and contracted agency staff would not be allowed to work until the training was completed. 100% compliance would be obtained by 06/09/2023. This began on 06/01/2023 and will end on 06/09/2023.
On 06/02/2023 a Patient Wandering system designed to secure facility egresses to prevent identified residents at risk for elopement from exiting the facility was ordered and would be installed upon delivery. Once the Patient Wandering system would be installed, and staff were inserviced on use of the system, the monitoring of residents at risk for elopement by trained designated employee would be discontinued as advised by the QAPI Committee.
S2DON and/or Designee would conduct random interview audits of staff from both shifts that ensured knowledge of COVID-19 symptoms 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
S2DON and/or Designee would conduct 10 random visual audits that ensured the proper use of transmission-based precautions, that included the use of personal protective equipment (PPE) with COVID-19 positive residents in accordance with CDC guidelines 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
S2DON would conduct documentation audits of COVID-19 testing 3 times per week for 4 weeks, then 2 times per week for weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
S2DON and/or Designee would conduct 10 random interview audits of staff from both shifts that ensured knowledge of COVID-19 symptoms 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
S1Administrator, S2DON, and/or Designee would conduct 5 random chart audits of residents who have been admitted or readmitted , had quarterly or annual MDS review, or a significant change in condition for completion of the MDS/CCC: Risk of Elopement Wandering Review 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
S2DON and/or Designee would conduct 10 random interview audits of staff from both shifts that ensured knowledge of COVID-19 symptoms 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and ended on 07/29/2023.
S2DON and/or Designee would conduct 10 random visual audits that ensured the proper use of transmission-based precautions, including the use of personal protective equipment (PPE) with COVID-19 positive residents 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
S2DON and/or Designee would conduct 10 random chart audits to review for residents with COVID-19 symptoms being placed in quarantine while determining if resident is positive for COVID-19, and that residents were tested upon COVID-19 symptom onset in accordance with CDC guidelines 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
S1Administrator and/or Designee would conduct visual audits for the presence of trained designated employee supervising residents identified as at risk for elopement and documentation review audits for all residents identified as at risk for elopement. These audits would occur 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/01/2023.
Results of audits including tracking and trends would be reviewed weekly in the QAPI meeting, and any identified issues would be addressed with re-education, plan modification and progressive discipline.
4. S1Administrator would review all audits implemented for this plan of correction for completion and for documentation of re-education, plan modification and progressive discipline as necessary 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the President of facility's management company and/or RDO. This began on 06/03/2023 and will end on 07/29/2023.
President of facility's management company and/or RDO would review S1Administrator's audits for completion and followed up with re-education, plan modification and progressive discipline as necessary. This began on 06/03/2023 and will end on 07/29/2023.
5. This was completed on 06/03/2023.
This deficient practice had the potential to cause serious injury, harm, or death to the remaining 8 residents identified as elopement risks by the facility and the remaining 86 non-positive COVID-19 residents residing in the facility who were at risk for contracting COVID-19.
Findings:
Cross reference F689, F880, and F882.
In an interview on 06/01/2023 at 10:25 a.m., S1Administrator confirmed the facility had two elopements in 2023. S1Adminsitrator stated Resident #38 and Resident #71 eloped out of the facility through the facility exits, but she is unsure of which one. S1Adminstrator stated the facility added alarms to the doors they think the residents utilized to elopement from the facility. S1Adminstrator stated the facility did not have a wanderguard system and not all doors had alarms because alarming all 39 doors was not in the budget. S1Adminstrator stated until the wanderguard was installed, it was the facility's plan to rely on the alarms on the doors to alert staff that residents were attempting to elope. She also stated residents that are an elopement risk still have the possibility of eloping.
In an interview on 06/01/2023 at 11:46 a.m., S2DON stated staff should never enter a COVID-19 positive resident's room without PPE in place and should never exit a COVID-19 positive resident's room with contaminated PPE on their person. S2DON further stated the observations reflected above puts the facility at risk for a facility wide COVID-19 outbreak. S2DON further stated Resident #27 should have been placed on COVID-19 precautions immediately following her positive COVID-19 test.
In an interview on 06/05/2023 at 5:15 p.m., S1Administrator confirmed she did not ensure the facility used its resources to effectively prevent the spread of COVID-19 in the facility. S1Adminsitrator further stated she was not up to date on current COVID-19 guidance and regulations because she was not a nurse. S1Adminsitrator further stated it had been very difficult for her to and keep up with the regulations.
In an interview on 06/06/2023 at 12:15 p.m., S2DON confirmed Resident #3 should have been tested for COVID-19 and placed in quarantine immediately upon the onset of COVID-19 symptoms. S2DON further stated if the facility had acted upon Resident #3's symptoms on 05/28/2023 when they began, the facility could have implemented precautions to prevent Resident #27, Resident #59, and Resident #74 from contracting COVID-19.
In an interview on 06/05/2023 10:47a.m. S36Senior [NAME] President, stated she was unaware of any other interventions implemented for the elopement incidents for Resident #71 on 01/08/2023 and Resident #38 on 02/16/2023. S36Senior [NAME] President stated there was a lack of communication to ensure staff were all aware of the expectations for COVID-19. S26Senior [NAME] President further stated she was responsible for monitoring the administration and nursing administration to ensure they were implementing the correct processes for COVID-19 and elopement and she would perform the audits stated in the above plan of removal until the new company took over the facility.
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Infection Control
(Tag F0880)
Someone could have died · This affected multiple residents
Based on record review, observation, and interview, the facility failed to take steps to prevent the transmission of COVID-19 by:
1.) failing to ensure staff quarantined and tested a resident (Residen...
Read full inspector narrative →
Based on record review, observation, and interview, the facility failed to take steps to prevent the transmission of COVID-19 by:
1.) failing to ensure staff quarantined and tested a resident (Resident #3) upon symptom onset of COVID-19;
2.) failing to ensure staff quarantined a resident ( Resident #27) who tested positive for Covid-19;and
3.) failing to ensure staff used personal protective equipment (PPE) with COVID-19 positive residents (Resident #3 and Resident #27).
This deficient practice resulted in an Immediate Jeopardy situation on 05/28/2023 at 11:30 a.m. when Resident #3 who displayed symptoms of COVID-19 and was not quarantined or tested by the facility. The Immediate Jeopardy situation continued for the following: On 05/31/2023 at 11:46 a.m., when Resident #27 tested positive for COVID-19 and was not placed on quarantine until 1:17p.m. On 05/31/2023 at 12:43 p.m. S23Agency Certified Nursing Assistant (CNA) entered Resident #27's, a symptomatic COVID-19 positive resident's room without a gown, gloves, or face shield in place. On 05/31/2023 at 1:02 p.m. S24Housekeeper entered Resident #27's room to deliver a clothing item without a gown, gloves, or face shield in place and then entered the housekeeping closet to stock her housekeeping cart. On 5/31/2023 at 1:33 p.m. S4LPN exited Resident #3's, a symptomatic COVID-19 positive resident, room with a contaminated yellow gown in her hands and entered Hall Y Dayroom. Resident #59 and Resident #74 tested positive for COVID-19 on 06/04/2023. As of 06/06/2023, there were 4 active resident COVID-19 cases in the facility.
S1Administrator was notified of the Immediate Jeopardy on 06/01/2023 at 4:48 p.m.
The Immediate Jeopardy was removed on 06/04/2023 at 4:03 p.m., after it was determined through observations, interviews, and record reviews, the facility implemented an acceptable Plan of Removal, prior to the survey exit, which included:
1. Resident #3 was placed on isolation precautions on 05/30/2023 and Resident #27 was placed on isolation precautions on 05/31/2023.This was completed on 06/01/2023.
On 06/01/2023, onsite staff and contracted agency staff were inserviced by S2Director of Nursing (DON) and S3Assistant Director Of Nursing (ADON)/Infection Preventionist (IP) regarding identification of COVID-19 symptoms, staff responsibilities when symptoms of COVID-19 are observed, and transmission-based precautions including the use of personal protective equipment (PPE) with COVID-19 positive residents in accordance with Centers for Disease Control and Prevention(CDC) guidelines. The Training by S2DON and S3ADON/IP and/or Designee continued as staff and contracted agency staff on alternate schedules reported to work. Staff and contracted agency staff were not allowed to work until training was completed. This began on 06/01/2023 and will end on 06/09/2023.
On 06/02/2023 licensed nurses onsite and contracted agency licensed nurses were inserviced by S2DON and S3ADON/IP regarding the need to quarantine residents with symptoms of COVID-19 while determining if the resident was positive for COVID-19 and testing residents upon COVID-19 symptom onset in accordance with CDC guidelines. The Training would continue as licensed staff nursing and contracted agency licensed nurses on alternate schedules reported to work. Licensed Nursing Staff contracted agency licensed nursing staff would not be allowed to work until training was completed. This began on 06/02/2023 and will end on 06/09/2023.
2. The other 86 residents who resided in the facility had the potential to be affected.
The initial round of broad based COVID-19 testing was completed on 05/31/2023 to identify any further positive cases of COVID-19 with 1 additional resident who tested positive and was placed on isolation precautions. The second round of broad based testing was completed on 06/02/2023 with no further positive tests. Testing would continue every third day until 2 weeks of negative results are achieved. This began on 05/31/2023 and would end when 2 weeks of negative results was achieved.
On 06/02/2023, S2DON and S3ADON/IP was educated on Infection Control policies and procedures, and Infection Surveillance policies by consultant nurse. This was completed on 06/02/2023.
On 06/01/2023, onsite staff and contracted agency staff were inserviced by S2DON and S3ADON/IP regarding the identification of COVID-19 symptoms, staff responsibilities, when symptoms of COVID-19 are observed, and transmission-based precautions including the use of personal protective equipment (PPE) with COVID-19 positive residents in accordance with CDC guidelines. The training by S2DON and S3ADON/IP and/or Designee continued as staff and contracted agency staff on alternate schedules reported to work. The staff and contracted agency staff would not be allowed to work until training was completed. This began on 06/01/2023 and will end on 06/09/2023.
On 06/01/2023, licensed nurses onsite and contracted agency licensed nurses were inserviced by S2DON and S3ADON/IP regarding the need to quarantine residents with symptoms of COVID-19 while determining if a resident was positive for COVID-19 and testing residents upon COVID-19 symptom onset in accordance with CDC guidelines. The training would continue as licensed staff nursing and contracted agency licensed nurses on alternate schedules reported to work. Licensed Nursing Staff and contracted agency licensed nursing staff would not be allowed to work until training was completed. This began on 06/01/2023 and will end on 06/09/2023.
3. On 06/02/2023, S2DON and S3ADON/IP were educated on Infection Control policies and procedures, and Infection surveillance policies by consultant nurse. This was completed on 06/02/2023.
On 06/01/2023, onsite staff and contracted agency staff were inserviced by S2DON and S3ADON/IP regarding identification of COVID-19 symptoms, staff responsibilities, when symptoms of COVID-19 are observed, and transmission-based precautions including the use of personal protective equipment (PPE) with COVID-19 positive residents in accordance with CDC guidelines. The training by S2DON and S3ADON/IP and/or Designee continued as staff and contracted agency staff on alternate schedules reported to work. Staff and contracted agency staff would not be allowed to work until training was completed. This began on 06/01/2023 and ended on 06/09/2023.
On 06/01/2023, licensed nurse's onsite and contracted agency licensed nurses were inserviced by S2DON and S3ADON/IP regarding the need to quarantine residents with symptoms of COVID-19 while determining if resident is positive for COVID-19 and testing residents upon COVID-19 symptom onset in accordance with CDC guidelines. Training will continue as licensed staff nursing and contracted agency licensed nurses on alternate schedules report to work. Licensed Nursing Staff and contracted agency licensed nursing staff will not be allowed to work until training is complete. This began on 06/01/2023 and ended on 06/09/2023.
4. S2DON and/or Designee will conduct 10 random interview audits of staff from both shifts to ensure knowledge of COVID-19 symptoms 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the Quality Assurance and Performance Improvement (QAPI) Committee. This began on 06/03/2023 and will end on 07/29/2023.
S2DON and/or Designee will conduct 10 random visual audits to ensure the proper use of transmission-based precautions including the use of personal protective equipment (PPE) with COVID-19 positive residents 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
S2DON and/or Designee will conduct 10 random chart audits to review for residents with COVID-19 symptoms who were placed in quarantine while determining if resident is positive for COVID-19, and testing residents upon COVID-19 symptom onset in accordance with CDC guidelines 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
Results of audits including surveillance will be reviewed weekly by QAPI Committee, and any identified issues will be addressed with re-education, plan modification and progressive discipline. This was completed on 06/03/2023.
This deficient practice had the potential to cause serious injury, harm, or death for the remaining 86 non-positive COVID-19 residents residing in the facility who were at risk for contracting COVID-19.
Findings:
1.)
Review of the facility's Coronavirus Disease Testing Residents Policy revealed, in part, any resident, regardless of their vaccination status, with even mild symptoms of COVID-19 would receive a viral test as soon as possible. Review revealed, symptomatic residents, regardless of vaccination status, were placed on transmission-based precautions (TBP) according to CDC guidelines. Review revealed, asymptomatic residents with close contact with someone with SARS-CoV-2(COVID-19) infection, regardless of vaccination status, would have a series of three viral tests for SARS-CoV-2(COVID-19) infection. Review revealed testing would be conducted immediately (but not until 24 hours after the exposure) and, if negative, again 48 hours after the first negative test and, 48 hours after the second negative test. Further review revealed, source control should be worn by all individuals being tested.
Review of Resident #3's Diagnosis List revealed, in part, Resident #3 had a diagnosis of essential hypertension and Type 2 Diabetes Mellitus.
Review of Resident #3's Minimal Data Set with an Assessment Reference Date of 04/12/2023 revealed, in part, Resident #3's Brief Interview for Mental Status Score was 15, which indicated Resident #3 was cognitively intact.
Review of Resident #3's Careplan, with a revision date of 04/25/2023, revealed, in part, Resident #3 was at risk for COVID-19 related to her comorbidities, and the CDC guidelines should be followed. Further review revealed Resident #3 should be monitored for signs and symptoms of infection and the medical director should be notified if any symptoms occurred. Further review revealed, Resident #3's cough, temperature, and shortness of breath should be evaluated and the medical director should be informed.
Review of Resident #3's nurse's notes, revealed no nursing notes documented from 05/25/2023-05/30/2023 regarding Resident #3 having symptoms of COVID-19.
Review of Resident #3's May 2023 electronic Medication Administration Record (eMAR) revealed, in part, no documented evidence that Resident #3 was assessed for signs and symptoms of COVID-19 on 05/28/2023 and 05/29/2023.
Review of the facility's Covid Testing Log revealed, Resident #3 tested positive for COVID-19 on 05/30/2023, Resident #27 tested positive for COVID-19 on 05/31/2023, Resident #59 tested positive for COVID-19 on 06/04/2023, and Resident #74 tested positive for COVID-19 on 06/04/2023.
Observation on 06/01/2023 at 8:12 a.m., revealed Resident #3 lying on her left side in her bed coughing into a white tissue.
In an interview on 06/01/2023 at 8:15 a.m., Resident #3 stated her symptoms of COVID-19 began on Sunday, 05/28/2023, after she got out of church around 11:30 a.m. Resident #3 further stated she informed S34AgencyLPN she had a sore throat, headache, and body aches. Resident #3 further stated S34Agency LPN told her she had a cold and it would pass in a few days. Resident #3 stated her symptoms continued on Monday, 05/29/2023 and Tuesday, 05/30/2023. Resident #3 stated the facility tested her for COVID-19 on Tuesday, 05/30/2023.
In an interview on 05/31/2023 at 9:20 a.m., S10ClinicalCoordinator stated Resident #3 had symptoms of COVID-19 on Monday, 05/29/2023. S10ClinicalCoordinator further stated Resident #3 complained of a headache, body aches, and weakness on 05/29/2023. S10ClinicalCoordinator further stated she noticed Resident #3 was extremely weak, but she did not notify Resident #3's physician because she assumed S5Licensed Practical Nurse took care of it. S10ClinicalCoordinator further stated Resident #3 now had a loss of appetite and a cough.
In an interview on 05/31/2023 at 2:36 p.m., S3ADON/IP stated COVID-19 testing was currently being completed on all residents in the facility and would not be completed again until 06/03/2023. S3ADON/IP further stated she had not interviewed Resident #3 and she was unaware of when her COVID-19 symptoms began.
In an interview on 06/01/2023 at 3:26 p.m., S34AgencyLPN stated she did not recall if Resident #3 told her she was feeling unwell. S34AgencyLPN further stated she was aware of the signs and symptoms of COVID-19, but she did not know the facility's policy on COVID-19 or the facility's process for a resident with COVID-19 symptoms.
In an interview on 06/01/2023 at 3:30 p.m., S10ClinicalCoordinator stated Resident #3 should have been tested on Sunday, 05/28/2023 upon COVID-19 symptom onset.
In an interview on 06/01/2023 at 5:30 p.m., S15CNA stated she witnessed Resident #3 report to S34AgencyLPN she was not feeling well around 2:00 p.m. on Sunday, 05/30/2023.
In an interview on 06/02/2023 at 11:32 a.m., Resident #3's physician stated it was his expectation that COVID-19 testing was completed upon the identification of symptoms of COVID-19. Resident #3's physician further stated following the identification of a positive COVID-19 result, the resident should be isolated.
In an interview on 06/06/2023 at 12:15 p.m., S2DON confirmed Resident #3 should have been tested for COVID-19 and placed in quarantine immediately upon the onset of COVID-19 symptoms. S2DON further stated if the facility had acted upon Resident #3's symptoms on 05/28/2023 when they began, the facility could have implemented precautions to prevent Resident #27, Resident #59, and Resident #74 from contracting COVID-19.
2.)
Review of the facility's Coronavirus Disease Testing Residents Policy revealed, symptomatic residents, regardless of vaccination status, were placed on transmission-based precautions (TBP) according to CDC guidelines.
Review of Resident #27's nurse's notes dated 05/31/2023 at 3:14 p.m. revealed, in part, Resident #27 tested positive for COVID-19.
In an interview on 05/31/2023 at 12:02 p.m., S10Clinical Coordinator stated Resident #27 tested positive today at 11:46 a.m.
Observation on 05/31/2023 at 12:54 p.m. revealed, Resident #27's door open without PPE or COVID-19 signage present.
Observation on 05/31/2023 at 1:17 p.m. revealed, S10Clinical Coordinator placed PPE and COVID-19 signage on Resident #27's door.
In an interview on 05/31/2023 at 3:46 p.m., S10Clinical Coordinator confirmed she should have placed PPE and COVID-19 isolation signage on Resident #27's door.
In an interview on 05/31/2023 at 3:57 p.m., S3ADON/IP stated PPE and COVID-19 isolation signage should be placed on a COVID-19 positive resident's door immediately and all staff should be made aware.
In an interview on 06/01/2023 at 11:46 a.m., S2DON stated Resident #27 should have been placed on COVID-19 precautions immediately following her positive COVID-19 test.
3.)
Review of the facility's Droplet Precautions policy revealed, in part, gloves, gown, and goggles should be worn when a resident is on droplet precautions.
Review of the facility's Personal Protective Equipment (PPE) policy revealed, in part, PPE provided to the facility's personnel included gowns, gloves, masks, and eye wear.
Review of Resident #3's nurses notes dated 05/30/2023 at 6:03 p.m. revealed, in part, Resident #3 tested positive for COVID-19.
In an interview on 05/31/2023 at 11:00 a.m., S4LPN stated Resident #3 remained symptomatic of COVID-19. S4LPN further stated Resident #3's symptoms included cough, body aches, and weakness.
In an interview on 05/31/2023 at 12:30 p.m., S23Agency CNA stated the only resident positive for COVID-19 was Resident #3.
Observation on 5/31/2023 at 1:33 p.m. revealed, S4LPN exited Resident #3's room with a gown, face shield, gloves, and an N95 mask on and entered Hall Y's Dayroom.
In an interview on 05/31/2023 at 2:13 p.m., S10Clinical Coordinator stated she witnessed S4LPN exit Resident #3's room with a gown, face shield, gloves, and an N95 mask and entered Hall Y's Dayroom. S10Clinical Coordinator stated S4LPN should have removed her gown, gloves, and face shield prior to exiting Resident #3's room. S10Clinical Coordinator further stated S4LPN should have removed her N95 mask, discarded it, and replaced it with a new one and she did not.
Review of Resident #27's nurse's notes dated 05/31/2023 at 3:14 p.m. revealed, in part, Resident #27 tested positive for COVID-19.
In an interview on 05/31/2023 at 12:02 p.m., S10Clinical Coordinator stated Resident #27 was symptomatic. S10Clinical Coordinator further stated Resident #27's symptoms included cough, body aches, and a sore throat.
Observation on 05/31/2023 at 12:43 p.m., revealed, S23Agency Certified Nursing Assistant (CNA) entered Resident #27's resident's room without a gown, gloves, or face shield in place. Further observation revealed S23CNA assisted Resident #27 with her clothing and then exited Resident #27's room and gave a cup of ice to Resident #74.
Observation on 05/31/2023 at 12:54 p.m. revealed, Resident #27's door open without PPE or COVID-19 signage present.
Observation on 05/31/2023 at 1:02 p.m. revealed, S24Housekeeper entered Resident #27's room without a gown, gloves, and a face shield. Observation further revealed S24Housekeeper handed Resident #27 a clothing item and then proceeded to the Hall Y's housekeeping closet to restock her cart.
In an interview on 05/31/2023 at 1:36 p.m., S24Housekeeper confirmed she entered Resident #27's room without a gown, a face shield, and gloves. S24Housekeeper further stated she was unaware that Resident #27 tested positive for COVID-19.
Observation on 05/31/2023 at 1:17 p.m. revealed S10Clinical Coordinator placed PPE and COVID-19 signage on Resident #27's door.
In an interview on 05/31/2023 at 1:36 p.m., S23Agency CNA confirmed she entered Resident #27's room without a gown, a face shield, and gloves. S23Agency CNA further stated she was unaware that Resident #27 tested positive for COVID-19.
In an interview on 05/31/2023 at 3:46 p.m., S10Clinical Coordinator confirmed she should have placed PPE and COVID-19 isolation signage on Resident #27's door and educated staff immediately after Resident #27 tested positive and she did not.
In an interview on 05/31/2023 at 3:57 p.m., S3ADON/IP stated staff should wear a face shield, gown, N95 mask, and gloves prior to entering a COVID-19 isolation room and all PPE should be removed prior to exiting a COVID-19 isolation room. S3ADON/IP further stated PPE and COVID-19 isolation signage should be placed on a COVID-19 positive resident's door immediately and all staff should be made aware.
In an interview on 06/01/2023 at 11:46 a.m., S2DON stated staff should never enter a COVID-19 positive resident's room without PPE in place and should never exit a COVID-19 positive resident's room with contaminated PPE on their person. S2DON further stated the observations reflected above puts the facility at risk for a facility wide COVID-19 outbreak.
CRITICAL
(L)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0882
(Tag F0882)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
Based on observation, interview and record review, the facility failed to ensure the Infection Preventionist established and maintained an effective infection prevention and control program to prevent...
Read full inspector narrative →
Based on observation, interview and record review, the facility failed to ensure the Infection Preventionist established and maintained an effective infection prevention and control program to prevent the transmission of COVID-19 infections in the facility by:
1.)failing to ensure staff quarantined and tested a resident (Resident #3) upon symptom onset of COVID-19;
2.)failing to ensure staff quarantined a resident ( Resident #27) who tested positive for Covid-19;and
3.)failing to ensure staff used personal protective equipment (PPE) with COVID-19 positive residents (Resident #3 and Resident #27).
This deficient practice resulted in an Immediate Jeopardy situation on 05/28/2023 at 11:30 a.m. when Resident #3 who displayed symptoms of COVID-19 and was not quarantined or tested by the facility. The Immediate Jeopardy situation continued for the following: On 05/31/2023 at 11:46 a.m., when Resident #27 tested positive for COVID-19 and was not placed on quarantine until 1:17p.m. On 05/31/2023 at 12:43 p.m. S23Agency Certified Nursing Assistant (CNA) entered Resident #27's, a symptomatic COVID-19 positive resident's room without a gown, gloves, or face shield in place. On 05/31/2023 at 1:02 p.m. S24Housekeeper entered Resident #27's room to deliver a clothing item without a gown, gloves, or face shield in place and then entered the housekeeping closet to stock her housekeeping cart. On 5/31/2023 at 1:33 p.m. S4LPN exited Resident #3's, a symptomatic COVID-19 positive resident, room with a contaminated yellow gown in her hands and entered Hall Y Dayroom. Resident #59 and Resident #74 tested positive for COVID-19 on 06/04/2023. As of 06/06/2023, there were 4 active resident COVID-19 cases in the facility.
S1Administrator was notified of the Immediate Jeopardy on 06/01/2023 at 4:48 p.m.
The Immediate Jeopardy was removed on 06/04/2023 at 4:03 p.m., after it was determined through observations, interviews, and record reviews, the facility implemented an acceptable Plan of Removal, prior to the survey exit, which included:
1. Resident #3 was placed on isolation precautions on 05/30/2023 and Resident #27 was placed on isolation precautions on 05/31/2023. This was completed on 05/31/2023.
2. The other 86 residents residing in the facility had the potential to be affected.
In order to keep the current resident population free from contracting COVID-19, S2Director of Nursing (DON) and S3Assistant Director of Nursing/Infection Preventionist (ADON/IP) were educated on 06/02/2023 regarding Infection Control policies and procedures and Infection Surveillance policies by the consultant nurse. This was completed on 06/02/2023.
On 05/31/2023 S2DON, S3ADON/IP and Nursing Administration conducted broad based testing of all residents and onsite staff. Resident #27 tested positive for COVID-19 and was placed on isolation precautions on 5/31/2023. Broad based testing was repeated on 06/02/2023 with all tests being negative. Broad based testing conducted by S2DON, S3ADON/IP, and Nursing Administration would continue every 3 days until test results were negative for a two week period. This began on 05/31/2023 and would end once all negative tests were obtained for two weeks.
3. In order to keep the current resident population free from contracting COVID-19, S2DON and S3ADON/IP were educated on 06/02/2023 regarding Infection Control policies and procedures and Infection Surveillance policies by the consultant nurse. This was completed on 06/02/2023.
On 05/31/2023 S2DON, S3ADON/IP, and Nursing Administration conducted broad based testing of all residents and onsite staff. Resident #27 tested positive for COVID-19 and was placed on isolation precautions on 5/31/2023. Broad based testing was repeated on 06/02/2023 with all tests negative. Broad based testing conducted by S2DON, Infection negative for two week period. This began on 05/31/2023 and would end once all negative tests are obtained for two weeks.
Responsible Employee: S3ADON/IP was responsible for ensuring that Infection
Control policies and procedures and Infection Surveillance policies were implemented, and that
staff were inserviced and monitored for adherence to the policies and procedures that prevented the transmission of COVID-19. S2DON would provide oversight of S3ADON/IP to ensure compliance of the Infection Prevention and Control Program.
4. S2DON and/or Designee would conduct 10 random interview audits of staff from both shifts that ensured knowledge of COVTD-19 symptoms 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
S2DON and/or Designee would conduct 10 random visual audits that ensured the proper use of transmission-based precautions including the use of personal protective equipment (PPE) with COVID-19 positive residents in accordance with CDC guidelines 3 times a week for 4 weeks, then 2 times a week for 4 weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
S2DON would conduct documentation audits of broad based testing on 10 random residents 3 times per week for 4 weeks, then 2 times per week for weeks, then as deemed necessary by the QAPI Committee. This began on 06/03/2023 and will end on 07/29/2023.
Results of audits and surveillance would be reviewed weekly by the QAPI Committee, and any identified issues would be addressed with re-education, plan modification and progressive discipline. This was completed on 06/03/2023.
This deficient practice had the potential to cause serious injury, harm, or death for the remaining 86 non-positive COVID-19 residents residing in the facility who were at risk for contracting COVID-19.
Findings:
Cross reference F880.
In an interview on 05/31/2023 at 2:36 p.m., S3ADON/IP stated COVID-19 testing was currently being completed on all residents in the facility and would not be completed again until 06/03/2023.S3ADON/IP further stated she had not interviewed Resident #3 and she was unaware of when her COVID-19 symptoms began.
In an interview on 05/31/2023 at 3:57 p.m., S3ADON/IP stated personal protective equipment(PPE) and COVID-19 isolation signage should be placed on a COVID-19 positive resident's door immediately and all staff should be made aware. S3ADON/IP further stated staff should wear a face shield, gown, N95 mask, and gloves prior to entering a COVID-19 isolation room and all PPE should be removed prior to exiting a COVID-19 isolation room. S3ADON/IP further stated PPE and COVID-19 isolation signage should be placed on a COVID-19 positive resident's door immediately and all staff should be made aware. S3ADON/IP further stated she had not read the updated infection control guidelines issues on 05/11/2023 and she was unaware of any of the new regulations.
In an interview on 06/01/2023 at 11:46 a.m., S2DON stated staff should never enter a COVID-19 positive Resident's room without PPE in place and should never exit a COVID-19 positive residents room with contaminated PPE on their person. S2DON further stated the observations reflected above puts the facility at risk for a facility wide COVID-19 outbreak. S2DON further stated Resident #27 should have been placed on COVID-19 precautions immediately following her positive COVID-19 test.
In an interview on 06/06/2023 at 12:15 p.m., S2DON confirmed Resident #3 should have been tested for COVID-19 and placed in quarantine immediately upon the onset of COVID-19 symptoms. S2DON further stated if the facility had acted upon Resident #3's symptoms on 05/28/2023 when they began, the facility could have implemented precautions to prevent Resident #27, Resident #59, and Resident #74 from contracting COVID-19.
In an interview on 06/02/2023 at 11:25 a.m., S2DON confirmed it was S3ADON/IP's responsibility to educate herself on the new regulations for infection control. S2DON further confirmed the infection control program was S3ADON/IP's responsibility. S2DON further stated the actions stated in the above interviews were S3ADON/IP's responsibility and S3ADON/IP should have ensured the proper infection control practices were implemented.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide privacy for a resident during incontinence care for 1 (Resident #57) of 1(Resident #57) sampled residents observed du...
Read full inspector narrative →
Based on observation, record review, and interview, the facility failed to provide privacy for a resident during incontinence care for 1 (Resident #57) of 1(Resident #57) sampled residents observed during incontinence care in a total investigative sample of 23.
Findings:
Review of Resident #57's Minimum Data Set (MDS) with an Assessment Reference Date (ARD) 03/28/2023 revealed, in part, Resident #57 had a Brief Interview for Mental Status (BIMS) of 5 (0-7 indicated severe impairment). Further review revealed, in part, an indication for an indwelling urinary catheter.
Review of Resident #57's Physician's orders revealed, in part, Foley catheter care every shift- wash with soap and water and dry site every shift related to retention of urine.
Review of Resident #57's care plan revealed, in part, resident requires the use of a Foley catheter related to a diagnosis of urinary retention. Interventions included: Perform pericare every shift and as needed.
Review of the facility's Resident Rights policy statement revealed, in part, residents had to the right to privacy and confidentiality.
Observation on 06/01/2023 at 2:31 p.m. revealed S7 Certified Nursing Assistant (CNA) entered Resident #57's room to provide incontinence and urinary catheter care, and failed to close the window blinds to the outside courtyard which was accessible to residents and staff. Observation further revealed S7CNA opened and removed Resident #57's adult diaper which exposed Resident #57's genital area while the window blinds that look out over the courtyard which was accessible to residents and staff remained opened.
In an interview on 06/01/2023 at 2:45 p.m., S7CNA stated she should have closed the window blinds in Resident #57's room before she performed incontinence and urinary catheter care.
In an interview on 06/05/2023 at 10:51 a.m., S10Clinical Coordinator stated privacy should be maintained during catheter care. S10Clinical Coordinator further stated, S7CNA should have closed the window blinds in Resident #57 room before she provided incontinence and urinary catheter care to Resident #57.
In an interview on 06/05/2023 at 1:40 p.m., S2DON stated S7CNA should have closed Resident #57's window blinds before she provided incontinence and urinary catheter care to Resident #57.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to ensure an allegation of resident to resident physical abuse and an allegation of staff to resident physical and verbal abuse was thoroughl...
Read full inspector narrative →
Based on record review and interviews, the facility failed to ensure an allegation of resident to resident physical abuse and an allegation of staff to resident physical and verbal abuse was thoroughly investigated for 1(Resident #239) of 1 sampled residents reviewed for verbal and physical abuse.
Findings:
Review of the facility's Statewide Incident Management Systems (SIMS) report log, revealed, in part, an allegation of physical abuse regarding Resident #239 was unsubstantiated on 12/21/2023.
Review of Resident #239's Health Standards Incident Report revealed, in part, the allegations of physical and verbal abuse occurred on 12/20/2022 at 12:30 p.m.
Review of the written statement written by S8Licensed Practical Nurse (LPN) revealed, in part, the alleged incident occurred on 12/20/2023 at 6:00 p.m. S8LPN further documented that she did not physically or verbally abuse Resident #239, but that Resident #3 did hit at Resident #239.
Review of the verbal statement given by S6Dietary Aide (DA) and written by S1Administrator revealed, in part, S6DA called S2Director of Nursing (DON) and reported that Resident #239 was hit and yelled at by S8LPN on 12/20/2023 at 12:30 p.m.
In an interview on 06/01/2023 at 4:25 p.m., S1Administrator stated she completed the SIMS reports incorrectly, and she should have indicated that the allegations of physical and verbal abuse were unable to be verified instead of unsubstantiated in regards to the allegation of staff to resident physical and verbal abuse.
In an interview on 06/05/2023 at 2:02 p.m., S2DON stated she was unaware of the difference in timeframe between S8LPN and S6DA's statements. S2DON further stated that this discrepancy in the timeframes of the written statements were not investigated and should have been investigated.
In an interview on 06/05/2023 4:38 p.m., S1Administrator stated she did not do a thorough investigation of the allegation of physical and verbal abuse as it related to S8LPN and Resident #239, and that she was unable to produce any further documentation that the allegations of physical and verbal abuse were investigated further. S1Administrator further stated she did not investigate the discrepancy in regards to the timeframes indicated in S6DA's verbal statement and S8LPN's written statement regarding the allegation of staff to resident physical and verbal abuse. S1Administrator further stated she did not investigate the allegation of resident to resident abuse involving Resident #3 and Resident #239 that was noted in S8LPN's written statement, and that this allegation of resident to resident abuse should have been investigated.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to complete a performance review at least once every 12 months for 3 Certified Nurse Aides (CNA) (S15CNA, S16CNA, and S17CNA) of 8 CNAs (S15CN...
Read full inspector narrative →
Based on record review and interview, the facility failed to complete a performance review at least once every 12 months for 3 Certified Nurse Aides (CNA) (S15CNA, S16CNA, and S17CNA) of 8 CNAs (S15CNA, S16CNA, S17CNA, S18CNA, S19CNA, S20CNA, S21CNA and S22CNAAgency) personnel records reviewed.
Findings:
Review of S15CNA's personnel record revealed, in part, a hire date of 10/18/2021, and no documentation that an annual performance review was completed within the last 12 months.
Review of S16CNA's personnel record revealed, in part, a hire date of 06/10/2019, and no documentation that an annual performance review was completed within the last 12 months.
Review of S17CNA's personnel record revealed, in part, a hire date of 09/21/2021, and no documentation that an annual performance review was completed within the last 12 months.
In an interview on 06/02/2023 at 1:02 p.m., S13Human Resources stated the facility does not have an annual evaluation of S15CNA and S16CNA, and that the facility should have performed annual evaluations of the CNAs.
In an interview on 06/02/2023 at 4:13 p.m. S11Clinical Coordinator stated she had not done the annual evaluations for S15CNA and S16CNA.
In an interview on 06/02/2023 5:05 p.m., S10Clinical Coordinator stated that she did not perform S15CNA and S16CNA's annual evaluations.
In an interview on 06/05/2023 at 1:38 p.m., S2DON stated that the annual evaluations for S15CNA, S16CNA, and S17CNA were not performed, and that the annual evaluations should have been performed at least every 12 months.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to provide dementia in-service training for 2 Certified Nursing Assistants (CNA) (S15CNA and S16CNA) of 8 CNAs (S15CNA, S16CNA, S17CNA, S18CN...
Read full inspector narrative →
Based on record review and interviews, the facility failed to provide dementia in-service training for 2 Certified Nursing Assistants (CNA) (S15CNA and S16CNA) of 8 CNAs (S15CNA, S16CNA, S17CNA, S18CNA, S19CNA, S20CNA, S21CNA and S22CNAAgency) reviewed for annual dementia training.
Findings:
Review of the facility's Staff Development Policy revealed, in part, that a required training topic included dementia management.
Review of the facility's Dementia Training Policy revealed, in part, that employees providing direct care to residents will receive four hours of dementia training within 90 days of hire and 1 hour annually thereafter.
Review of S15CNA's personnel record revealed, in part, a hire date of 10/18/2021, and no documentation that dementia training was completed within the last 12 months.
Review of S16CNA's personnel record revealed, in part, a hire date of 06/10/2019, and no documentation that dementia training was completed within the last 12 months.
In an interview on 06/05/2023 at 1:38 p.m., S13Human Resources stated S15CNA and S16CNA did not complete their annual dementia training and that she could not produce any documentation that S15CNA and S16CNA completed their annual dementia training.
In an interview on 06/05/2023 at 1:38 p.m., S2Director of Nursing stated S15CNA and S16CNA did not complete their annual dementia training, and should have completed their dementia training annually.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to have current nurse staffing information posted on a daily basis.
Findings:
In an interview on 05/30/2023 at 9:20 a.m., S25Receptionist stated...
Read full inspector narrative →
Based on observation and interview, the facility failed to have current nurse staffing information posted on a daily basis.
Findings:
In an interview on 05/30/2023 at 9:20 a.m., S25Receptionist stated S11Clinical Coordinator posted the nursing staffing information daily; however, the posted staffing reflects the hours provided on the prior (or previous) day.
Observation on 05/31/2023 at 10:32 a.m. revealed nurse staffing information posted at the front desk for the hours provided on 05/30/2023.
Observation on 05/31/2023 at 2:30 p.m. revealed nurse staffing information posted on Hall A for the hours provided on 05/30/2023.
Observation on 05/31/2023 at 10:30 a.m. revealed nurse staffing information posted at the front desk for the hours provided on 05/29/2023.
Observation on 06/01/2023 at 10:33 a.m. revealed nurse staffing information posted on Hall A for the hours provided on 05/30/2023.
Observation on 06/01/2023 at 10:36 a.m. revealed nurse staffing information posted on Hall B for the hours provided on 05/30/2023.
Observation on 06/02/2023 at 12:05 p.m. revealed nurse staffing information posted on Hall B for the hours provided on 06/01/2023.
Observation on 06/02/2023 at 1:56 p.m. revealed nurse staffing information posted on Hall A for the hours provided on 06/01/2023.
Observation on 06/05/2023 at 9:19 a.m. revealed nurse staffing information posted on Hall B for the hours provided on 06/02/2023 and 06/03/2023.
Observation on 06/05/2023 at 9:20 a.m. revealed nurse staffing information posted on Hall A for the hours provided on 06/02/2023 and 06/03/2023.
In an interview on 06/05/2023 at 1:38 p.m., S11Clinical Coordinator stated the daily posted staffing should reflect the staffing for the current day.
In an interview on 06/05/2023 at 1:38 p.m., S2Director of Nursing stated that the nurse staffing information posted daily should be for the current date and not a previous date.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on record reviews, observations, and interviews, the facility failed to ensure medications were locked and not available for use at a resident's bedside for 1 (Resident #74) of 21 (Resident #6, ...
Read full inspector narrative →
Based on record reviews, observations, and interviews, the facility failed to ensure medications were locked and not available for use at a resident's bedside for 1 (Resident #74) of 21 (Resident #6, Resident #7, Resident #8, Resident #9, Resident #18, Resident #21, Resident #22, Resident #38, Resident #54, Resident #57, Resident #62, Resident #70, Resident #71, Resident #72, Resident #73, Resident #74, Resident #75, Resident #76, Resident #80, Resident #83, and Resident #238) sampled residents observed for medications left at the bedside.
Findings:
Review of the facility's Storage of Medications policy revealed, in part, drugs and biologicals used in the facility are stored in locked compartments and only persons authorized to prepare and administer medications have access to locked medications.
Review of Resident #74's Minimum Data Set with an Assessment Reference Date of 05/03/2023 revealed, in part, Resident #74 was documented to be able to transfer and walk in her room with no physical assistance needed by staff. Further review revealed Resident #74 had a Brief Interview for Mental Status score of 9, which indicated moderate cognitive impairment.
Review of Resident #74's care plan revealed, in part, no documented evidence Resident #74 was care planned to self-administer medications or have medications available for use at the bedside.
Review of Resident #74's May and June 2023 physician's orders revealed, in part, no documented evidence of an order for Resident #74 to have medications available for self-administration at her bedside.
Review of Resident #74's record revealed no documented evidence and the facility did not present any documented evidence Resident #74 was assessed or care planned to have medications available for self-administration.
Observation on 05/30/2023 at 11:24 a.m. revealed Resident #74 had a box of Imodium multi-symptom relief (a medication used to treat diarrhea, bloating, and gas), a bottle of extra strength Tylenol (a medication used to treat pain or fever) and a box of Refresh eye drops (a medication used to lubricate the eyes) located in an unlocked and transparent container near Resident #74's bedside.
In an interview on 05/30/2023 at 11:25 a.m., Resident #74 confirmed she had medications available in her room. Resident #74 stated she was unsure which medications were present because her daughter brought them to her.
Observation on 05/31/2023 at 12:42 p.m. revealed Tylenol, Imodium, Refresh eye drops, and a medication bottle with unidentified tablets visible in Resident #74's unlocked and transparent bedside container.
Observation on 06/01/2023 at 8:06 a.m. revealed Tylenol, Imodium, Refresh eye drops, and Alka-Seltzer (an effervescent antacid and pain reliever) visible in Resident #74's unlocked and transparent bedside container.
Observation on 06/02/2023 at 10:21 a.m. revealed Tylenol, Imodium, Refresh eye drops, and Alka-Seltzer visible in Resident #74's unlocked and transparent bedside container.
In an interview on 06/02/2023 at 10:47 a.m., S5Licensed Practical Nurse stated Resident #74 was not care planned to self-administer medications and Resident #74 should not have medications available for use at her bedside.
In an interview on 06/02/2023 at 10:49 a.m., S10Clinical Coordinator stated Resident #74 was not care planned or assessed to self-administer medications.
Observation on 06/02/2023 at 10:54 a.m. revealed the following medications were removed from Resident #74's unlocked and transparent bedside container by S10Clinical Coordinator:
-Alka-Seltzer effervescent tablets;
-Vitamin B12 5,000 units tablets (a vitamin supplement);
-Triamcinolone Acetonide 0.1% Cream (a steroid cream used to reduce inflammation and allergic reactions);
-2 tubes of Neosporin ointment (an antibiotic ointment used for minor skin infections);
-A tube of antibiotic ointment (an ointment used for minor skin infections);
-A bottle of unidentified tablets;
-A container with 2 unidentified pills;
-Icy Hot Max roller Lidocaine (a topical medication used to treat pain)
-Imodium multi-symptom relief caplets;
-Imodium A-D softgels (a medication used for diarrhea);
-A bottle of 8 unidentified pills with a handwritten label of Tylenol PM (a medication used to treat pain and aid with sleep);
-Max Strength Aspercreme with 4% Lidocaine (a topical medication used for pain);
-2 bottles of Refresh Tears Lubricant eye drops;
-Artificial Tears Lubricant eye drops;
-Orasol Benzocaine 20% (a gel used to numb oral pain);
-Orajel toothache cream (a gel used to numb oral pain);
-Glycerin liquid (a liquid used to moisturize the skin);
-Extra Strength Tylenol 500mg rapid release gels; and,
-2% Miconazole Nitrate (a cream used to treat fungal infections).
In an interview on 06/04/2023 at 3:34 p.m., S2Director of Nursing stated Resident #74 was not assessed or care planned to have medications at the bedside. S2Director of Nursing further stated Resident #74 should not have had medications at the bedside.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected multiple residents
Based on record reviews, observations, and interviews, the facility failed to provide a resident with the correct form of food to meet the residents needs for 1(Resident #7) of 9(Resident #7, Resident...
Read full inspector narrative →
Based on record reviews, observations, and interviews, the facility failed to provide a resident with the correct form of food to meet the residents needs for 1(Resident #7) of 9(Resident #7, Resident #12, Resident #16, Resident #24, Resident #28, Resident #45, Resident #67, Resident #72, and Resident #78) sampled residents reviewed for dining services.
Findings:
Review of the facility's Therapeutic Diet policy revealed, in part, a resident's diet order should match the terminology used by the food and nutrition services department.
Review of Resident #7 Physician Orders revealed an order with a start date of 09/29/2022 that stated Resident #7 was to have a regular diet with regular texture and regular consistency.
Review of Resident #7's dietary status report slip with a date of 12/07/2022 revealed, in part, Resident #7's was to be given finger foods with meals.
Observation on 05/30/2023 at 12:16 p.m., revealed Resident #7 was in the dining room and was served a lunch meal which contained refried beans, creamed corn, mexican rice, and an enchilada with salsa. Further observation revealed, Resident #7's meal ticket read Resident #7 should have finger foods.
Observation on 05/31/2023 at 12:27 p.m., revealed Resident #7 was in the dining room and was served a lunch meal which contained butter beans with rice, stewed spinach, a slice of ham, a cup with fruit pieces, and a piece of corn bread. Observation further revealed Resident #7's meal ticket read Resident #7 should have finger foods.
Observation on 06/01/23 at 5:17 p.m., revealed Resident #7 was in the dining room and was served a lunch meal which contained an egg roll, mixed vegetable rice, boneless chicken with sauce, and chopped pineapple in a bowl. Observation further revealed Resident #7's meal ticket read Resident #7 should have finger foods.
In an interview on 6/02/2023 at 11:09 a.m., S2Director of Nursing (DON) stated Resident #7 was ordered finger foods to allow her to feed herself independently. S2DON further stated Resident #7's diet order was not updated to reflect that finger foods were required and it should have been.
In an interview on 06/02/2023 at 11:10 a.m., S26Dietary Manager stated finger foods are items such as hamburgers, hotdogs, chicken tenders, pizza, broccoli spears, green beans, and chips. S26Dietary Manager stated the food in the above observations was not considered finger foods and Resident #7 should have been served an alternative meal to better meet her needs.