ST JUDE'S HEALTH & WELLNESS CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
St. Jude's Health & Wellness Center has received a Trust Grade of F, indicating poor performance with significant concerns about care quality. It ranks #246 out of 264 facilities in Louisiana, placing it in the bottom half, and #10 out of 11 in Orleans County, meaning there is only one facility in the area that performs worse. The trend is worsening, with issues increasing from 18 in 2024 to 21 in 2025, and the facility has accumulated $389,001 in fines, which is higher than 98% of Louisiana facilities, suggesting ongoing compliance problems. While staffing is rated average with a 3/5, the turnover rate is concerning at 69%, significantly above the state average of 47%, which may affect the consistency of care. Specific incidents include allowing untrained staff to work independently with residents, which poses a serious risk, and a failure to obtain timely lab services, leading to a hospitalization due to valproic acid toxicity. Overall, families should weigh these significant weaknesses against the average staffing rating when considering this facility for their loved ones.
- Trust Score
- F
- In Louisiana
- #246/264
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 69% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $389,001 in fines. Higher than 60% of Louisiana facilities. Some compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 16 minutes of Registered Nurse (RN) attention daily — below average for Louisiana. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 45 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Louisiana average (2.4)
Significant quality concerns identified by CMS
23pts above Louisiana avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Significant penalties indicating serious issues
21 points above Louisiana average of 48%
The Ugly 45 deficiencies on record
Mar 2025
5 deficiencies
2 IJ (2 affecting multiple)
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Laboratory Services
(Tag F0770)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to obtain laboratory services in a timely manner per physician's ord...
Read full inspector narrative →
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility's administrative staff failed to use its resources efficiently and effectiv...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observations and interviews, the facility failed to ensure
1.) maintenance services placed an outlet cover over a wall socket in a resident's room (Resident #1); and,
2.) housekeeping servi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record reviews, the facility failed to provide incontinence care for 1 (Resident #1) of 3 (Resident #1, Resident #2, and Resident #3) sampled residents investigat...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to ensure staff utilized the correct personal protective equipment (PPE) when providing care to a resident on enhanced barrie...
Read full inspector narrative →
Jan 2025
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to maintain a resident's right to make choices regarding smoking for 1 (Resident #32) of 3 (Resident #26, Resident #32, Resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to ensure a resident's code status documented in the resident's medic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to ensure the Skilled Nursing Facility Advance Beneficiary Notice of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record reviews the facility failed to conduct an accurate comprehensive assessment for 2 (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to provide documentation of a resident's Level II Pre-admission Scree...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on observation, interviews, and record reviews, the facility failed to ensure safe smoking interventions were carried out...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record reviews, the facility failed to ensure a resident's psychotropic medication was not ordered on an as needed basis for greater than 14 days for 1 (Resident #55) of 5 (Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record reviews, the facility failed to ensure a physician was notified laboratory tests were not complete...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility failed to ensure residents received dental services for 2 (Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected 1 resident
Based on observations and interviews, the facility failed to ensure the facility's dumpster was maintained in a sanitary manner.
Findings:
Observation on 01/28/2025 at 10:35AM revealed the facility's ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure the facility assessment included active involvement from dire...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to administer the pneumococcal (a bacterial infection caused by Streptococcus pneumonia bacterial) vaccine for 2 (Resident #43, Resident #81) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure the COVID-19 (an infectious disease caused by the SARS-CoV-2 virus) vaccine was administered for 1 (Resident #81) of 5 (Resident #30...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0563
(Tag F0563)
Could have caused harm · This affected multiple residents
Based on interviews and record review, the facility failed to allow residents unrestricted visitation.
Findings:
Review of the facility's undated visitation policy and procedure, revealed, in part, r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected multiple residents
Based on interview and record reviews, the facility failed to ensure:
1. A resident's dialysis access site was assessed and vital signs were obtained upon the resident's return from dialysis (Resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and observation, the facility failed to ensure:
1. Opened insulin pens were labeled with the date the pen wa...
Read full inspector narrative →
Dec 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record review, facility document review, and facility policy review it was determined that the facility fai...
Read full inspector narrative →
Nov 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and policy review the facility failed to maintain a sanitary environment for 2 (Resident #1 and Resident #2) of 3 residents reviewed for a sanitary environment.
Find...
Read full inspector narrative →
Jul 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record reviews and interviews, the facility failed to ensure a thorough investigation was completed for an allegation of neglect related to an injury of unknown origin for 1 (Resident #1) of ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record reviews, and interviews the facility failed to ensure a resident's care plan:
1. Was revised to include a decline in a resident's activities of daily living [ADLs] (Resident #1); and,
...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
Based on record reviews, observation, and interviews, the facility failed failed to ensure staff was available at all times to provide care and services to meet the resident's needs by failing to ensu...
Read full inspector narrative →
Apr 2024
2 deficiencies
2 IJ (2 facility-wide)
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0728
(Tag F0728)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews, observations and interviews, the facility failed to ensure staff working as nurse aides met minimum sta...
Read full inspector narrative →
CRITICAL
(L)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Administration
(Tag F0835)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
Based on observations, record reviews, and interviews, the facility failed to be administered in a manner that enabled it to use its resources effectively and efficiently by failing to ensure staff wo...
Read full inspector narrative →
Feb 2024
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to develop policies and procedures to investigate injuries of unknown origin for 1 (Resident #42) of 1 (Resident #42) sampled residents reviewe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to report a bruise with an unknown origin within 2 hours of the bruise having been identified for 1 (Resident #42) of 1 (Resident #42) sampled...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to have evidence that injuries of unknown origin were thoroughly investigated for 1 (Resident #42) of 1 (Resident #42) sampled residents review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure:
1. Louisiana Physician Orders for Scope of Treatment (LaPos...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to obtain the resident's most recent plan of care, certification of terminal illness, and documentation of services provided for 1 (Resident #...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
MDS Data Transmission
(Tag F0640)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure Minimum Data Set (MDS) resident assessments were transmitted and accepted by the Centers for Medicare and Medicaid Services (CMS) wi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure water accessible to residents did not exceed 120 degrees Fahrenheit for 9 (Bathroom A, Bathroom B, Bathroom D, Bathroom E, Bathroom F,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure Certified Nursing Assistants (CNAs) had completed annual competencies as required for 3 (S17CNA, S23CNA, S24CNA) of 5 (S9CNASupervio...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on record reviews and interviews, the facility failed to complete an annual performance review for every certified nurse aide (CNA) at least once every 12 months for 1 (S17CNA) of 5 (S9CNASuperv...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview the facility failed to:
1. Ensure staff performed hand hygiene during dining observation for 3 (Hall W, Hall X, and Hall Z) of 4 (Hall W, Hall X, Hal...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0577
(Tag F0577)
Minor procedural issue · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure all complaint surveys since the last annual survey were available for resident review.
Findings:
In an interview on 02...
Read full inspector narrative →
Jul 2023
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to Protect a resident from physical abuse for 2 Residents (Resident #4...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that a facility-initiated involuntary discharge was performe...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to:
1. Ensure residents had privacy to open packages/mail; and,
2. To deliver packages to residents on the weekend and in a timely manner.
Thi...
Read full inspector narrative →
Mar 2023
2 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, record review, and interviews, the facility failed to ensure:
1.Expired medications were not available for administration to residents for 1 of 2 Med rooms reviewed for medicat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected multiple residents
Based on record review and interview the facility failed to assess and complete Quarterly Minimum Data set in a timely manner on a resident for 7 (#2, #21, #31, #36, #50, #55, and #58) of 13 (#2, #5, ...
Read full inspector narrative →
Dec 2022
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to report the final results of the investigation involving an allegation of staff to resident abuse to the State survey agency within 5 working...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 4 life-threatening violation(s), 1 harm violation(s), $389,001 in fines. Review inspection reports carefully.
- • 45 deficiencies on record, including 4 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $389,001 in fines. Extremely high, among the most fined facilities in Louisiana. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is St Jude'S Health & Wellness Center's CMS Rating?
CMS assigns ST JUDE'S HEALTH & WELLNESS CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Louisiana, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is St Jude'S Health & Wellness Center Staffed?
CMS rates ST JUDE'S HEALTH & WELLNESS CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 69%, which is 23 percentage points above the Louisiana average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at St Jude'S Health & Wellness Center?
State health inspectors documented 45 deficiencies at ST JUDE'S HEALTH & WELLNESS CENTER during 2022 to 2025. These included: 4 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 1 that caused actual resident harm, 39 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates St Jude'S Health & Wellness Center?
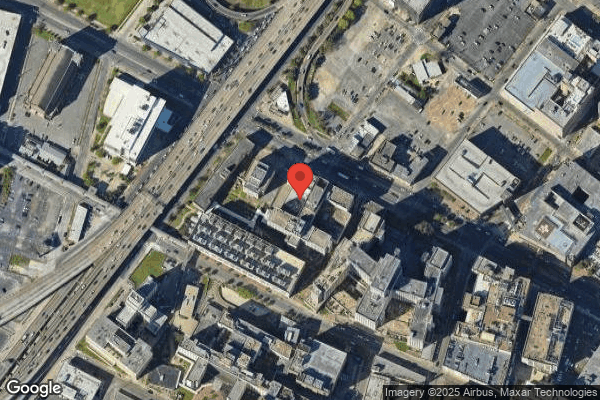
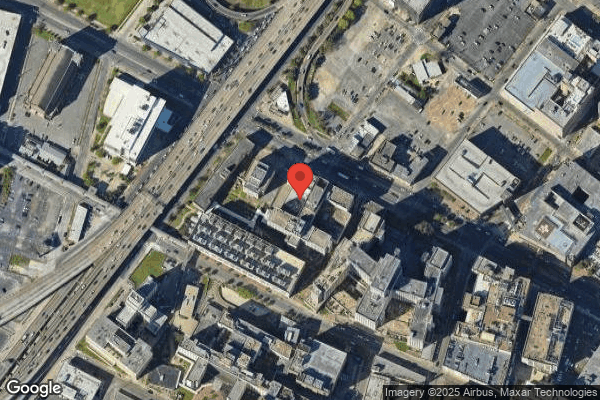
ST JUDE'S HEALTH & WELLNESS CENTER is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 116 certified beds and approximately 80 residents (about 69% occupancy), it is a mid-sized facility located in NEW ORLEANS, Louisiana.
How Does St Jude'S Health & Wellness Center Compare to Other Louisiana Nursing Homes?
Compared to the 100 nursing homes in Louisiana, ST JUDE'S HEALTH & WELLNESS CENTER's overall rating (1 stars) is below the state average of 2.4, staff turnover (69%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting St Jude'S Health & Wellness Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the facility's high staff turnover rate.
Is St Jude'S Health & Wellness Center Safe?
Based on CMS inspection data, ST JUDE'S HEALTH & WELLNESS CENTER has documented safety concerns. Inspectors have issued 4 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Louisiana. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at St Jude'S Health & Wellness Center Stick Around?
Staff turnover at ST JUDE'S HEALTH & WELLNESS CENTER is high. At 69%, the facility is 23 percentage points above the Louisiana average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was St Jude'S Health & Wellness Center Ever Fined?
ST JUDE'S HEALTH & WELLNESS CENTER has been fined $389,001 across 8 penalty actions. This is 10.5x the Louisiana average of $36,969. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is St Jude'S Health & Wellness Center on Any Federal Watch List?
ST JUDE'S HEALTH & WELLNESS CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.