SANDY RIVER CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Sandy River Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranked #74 out of 77 nursing homes in Maine, it sits in the bottom half of facilities statewide and is the least favorable option in Franklin County. While the facility's trend is improving, having reduced its issues from 18 in 2024 to 3 in 2025, the overall Trust Score remains low at 26 out of 100. Staffing is a relative strength with a rating of 4 out of 5 stars and a turnover rate of 42%, which is below the state average, but the facility has recorded concerning fines of $21,645, higher than 84% of Maine facilities. Specific incidents raise alarms, such as a critical failure to provide appropriate textured meals for a resident with swallowing issues, leading to choking and ultimately the resident's death. Additionally, staff shortages have been reported, with insufficient coverage leading to residents not receiving timely assistance for daily needs. There have also been issues with cleanliness, as multiple areas of the facility were found to be unsanitary, including the presence of flies and dirty floors. Overall, while there are positive aspects like staffing stability, the serious safety concerns and poor inspection outcomes warrant careful consideration.
- Trust Score
- F
- In Maine
- #74/77
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 42% turnover. Near Maine's 48% average. Typical for the industry.
- Penalties ✓ Good
- $21,645 in fines. Lower than most Maine facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 56 minutes of Registered Nurse (RN) attention daily — more than average for Maine. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 45 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (42%)
6 points below Maine average of 48%
Facility shows strength in staffing levels, quality measures, fire safety.
The Bad
Below Maine average (3.0)
Significant quality concerns identified by CMS
Near Maine avg (46%)
Typical for the industry
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 45 deficiencies on record
Sept 2025
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to adequately provide housekeeping and maintenance services necessary ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and review of the facility's Warewashing policy/procedure and the facility's Food Storage pol...
Read full inspector narrative →
Jul 2025
1 deficiency
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0692
(Tag F0692)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on the facility reported incident, record reviews and interviews, the facility failed to provide the appropriate textured ...
Read full inspector narrative →
Aug 2024
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure that the resident's environment was free of accident hazards relating to a desk wall laminate covering for 1 of 3 days of survey. (8/5...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to provide documentation of monitoring of psychotropic medication sid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure appropriate infection control procedures were followed related to hand sanitizing during the medication pass task for 1 of 2 medicatio...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews the facility failed to provide residents/representatives written information concerning th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to adequately provide housekeeping and maintenance services necessary ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interview, the facility failed to ensure that 3 of 3 residents reviewed with a specialized mental he...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident #26 was admitted on [DATE] with diagnoses to include post-traumatic stress disorder, depression, and anxiety.
Review...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure residents' care plans were reviewed and revised by the inte...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews and interviews, the facility failed provide respiratory care consistent with professional ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observations and interviews, the facility failed to ensure that medications were stored properly by having an unlocked, unattended medication cart allowing residents and unauthorized persons ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to offer nourishing snacks to residents who want to eat at non-traditi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations, interviews, the facility's Refrigerated/Frozen Storage policy revision date 6/15/18, the facility's Environment: policy HCSG 028 revised 9/2017, the facility's Warewashing polic...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to maintain a garbage storage area in a sanitary condition to prevent the harborage and feeding of pests for 2 trash collection container for 4 ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on record reviews and interview, the facility failed to ensure that clinical records were complete and contained accurate information for 1 of 1 residents reviewed for activities of daily living...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected multiple residents
Based on review of the quarterly Quality Assurance Performance Improvement/Quality Assurance Assessment (QAPI/QAA) Committee meeting attendance sheets and interview, the facility failed to ensure that...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
Based on record review and interviews, the facility failed to ensure sufficient direct care staff were scheduled and on duty to meet the needs of residents that reside in the facility. This has the po...
Read full inspector narrative →
Apr 2024
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interview, the facility failed to adequately maintain housekeeping and maintenance services necessary ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to properly store, label and date food in the walk-in refrigerator and...
Read full inspector narrative →
Oct 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to provide a resident with care and services (incontinence care/mobility assistance) to promote physical, mental health, and well-being in a ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure that physician's orders were followed for 1 of 2 residents r...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on record reviews and interviews, the facility failed to ensure that clinical records were complete and contained accurate information for 2 of 3 residents reviewed for pressure ulcer care (#1, ...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record reviews and interviews, the facility failed to complete a medication reconciliation to ensure that correct physician orders were implemented for 1 of 2 sampled residents (Resident #1) ...
Read full inspector narrative →
Jul 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to administer physician ordered medications to 1 of 2 sampled residents (Resident #2).
Finding:
On 7/10/23 and 7/11/23, Resident #2's clinic...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to re-evaluate a resident for an elopement risk and removed a physician ordered wander guard bracelet for 1 of 1 residents reviewed that atte...
Read full inspector narrative →
Oct 2022
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to maintain the dignity of 1 of 6 residents (Resident#27) reviewed for dignity related to urinary collection bags during 1 of 5 days of survey (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility's interdisciplinary team (IDT) failed to determine if it was clinically appropriate for a resident to keep a medication at bedside and self-administe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure that 1 of 3 residents with a specialized mental health diagn...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on observations, record review, and interviews, the facility failed to change oxygen tubing for 1 of 2 sampled residents ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure that the Consultant Licensed Pharmacist reported an identified required gradual dose reduction (GDR) for an antipsychotic medication...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
Based on interviews and observations, the facility failed to ensure that call lights were within reach for residents that are capable of using a call bell for 2 of 5 days of survey (10/24/22, 10/25/22...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility was unable to provide evidence that a Skilled Nursing Facility Advance Beneficiary Notice (SNFABN) Form 10055, which included appeal rights and liabi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, the facility failed to notify the resident and/or the resident's representative in writi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on clinical record reviews, review of the electronic Medication Administration Record (MAR) and interviews, the facility failed to administer a physician ordered medication that was available fo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
2. On 10/27/22, Resident #17's clinical record was reviewed. A physician order was written on 8/15/22 for Lorazepam Tablet 0.5 mg, give 1 tablet by mouth every 8 hours as needed for agitation. The cli...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations and interviews, the facility failed to ensure the kitchen was maintained in a clean and sanitary manner for the floor, the food disposal control box, ceiling vents, ceiling tiles...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected multiple residents
Based on observation, the facility failed to post the current daily nurse staffing information that includes the facility name, day of the month, a breakdown of the number of registered and licensed n...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0868
(Tag F0868)
Minor procedural issue · This affected multiple residents
Based on an interview and review of the facility's Quality Assurance and Performance Improvement (QAPI), the facility failed to present evidence that the required members attended 2 of 4 quarters prov...
Read full inspector narrative →
Jan 2020
5 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on interviews and record reviewss the facility failed to speak to a resident in a dignified manner which upset the resident, causing the resident to yell and argue loudly for 1 of 17 sampled res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record reviews, the facility failed to implement a care plan in the area of falls for 1 of 17 residents sampled whose care plans were reviewed (Resident #20).
Fi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, the facility failed to adequately provide housekeeping and maintenance services necessary ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
2. On 1/28/20 at 7:50 a.m., an interview of Registered Nurse (RN) #2 revealed that he/she was in charge on 11/25/19 and that there had been a verbal altercation between Certified Nursing Assistant (CN...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #41 was admitted to the facility on [DATE] with diagnosis of Dementia, Major Depressive Disorder, Bipolar Disorder a...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 42% turnover. Below Maine's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 1 life-threatening violation(s). Review inspection reports carefully.
- • 45 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $21,645 in fines. Higher than 94% of Maine facilities, suggesting repeated compliance issues.
- • Grade F (26/100). Below average facility with significant concerns.
About This Facility
What is Sandy River Center's CMS Rating?
CMS assigns SANDY RIVER CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Maine, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Sandy River Center Staffed?
CMS rates SANDY RIVER CENTER's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 42%, compared to the Maine average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Sandy River Center?
State health inspectors documented 45 deficiencies at SANDY RIVER CENTER during 2020 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 42 with potential for harm, and 2 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Sandy River Center?
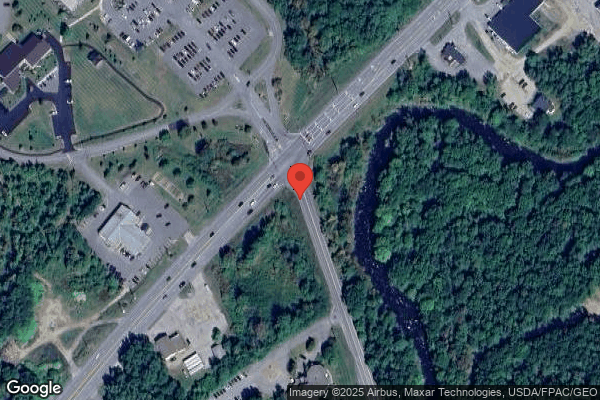
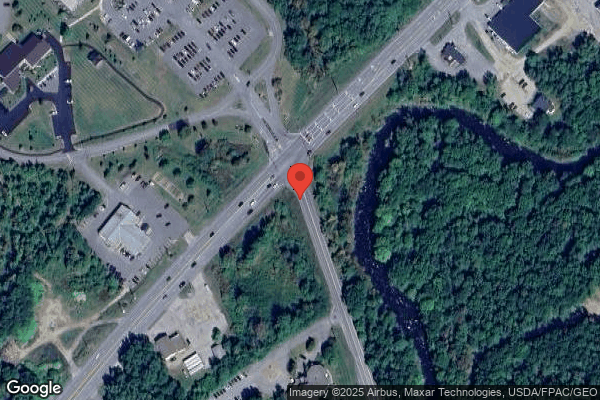
SANDY RIVER CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by GENESIS HEALTHCARE, a chain that manages multiple nursing homes. With 82 certified beds and approximately 71 residents (about 87% occupancy), it is a smaller facility located in FARMINGTON, Maine.
How Does Sandy River Center Compare to Other Maine Nursing Homes?
Compared to the 100 nursing homes in Maine, SANDY RIVER CENTER's overall rating (1 stars) is below the state average of 3.0, staff turnover (42%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Sandy River Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Sandy River Center Safe?
Based on CMS inspection data, SANDY RIVER CENTER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Maine. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Sandy River Center Stick Around?
SANDY RIVER CENTER has a staff turnover rate of 42%, which is about average for Maine nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Sandy River Center Ever Fined?
SANDY RIVER CENTER has been fined $21,645 across 1 penalty action. This is below the Maine average of $33,295. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Sandy River Center on Any Federal Watch List?
SANDY RIVER CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.