AUTUMN LAKE HEALTHCARE AT SPA CREEK




Over 2 years since last inspection. Current conditions may differ from available data.
Autumn Lake Healthcare at Spa Creek has received a Trust Grade of F, indicating significant concerns about the facility. Ranked #145 out of 219 in Maryland, this places it in the bottom half of nursing homes in the state, while locally, it ranks #9 out of 13 in Anne Arundel County, with only a few better options available. The facility is showing improvement, reducing issues from 25 in 2023 to 13 in 2025, but it still reported 65 total issues, including one critical incident where a resident received excessive doses of medication, raising serious safety concerns. Staffing is a weakness here, with a 56% turnover rate which is above the Maryland average, and RN coverage is below that of 89% of state facilities, though the facility has no fines on record. While quality measures are rated excellent, there are serious concerns with compliance, including failures to meet professional standards during medication administration, which could jeopardize resident safety.
- Trust Score
- F
- In Maryland
- #145/219
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 56% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Maryland facilities.
- Skilled Nurses ○ Average
- Each resident gets 30 minutes of Registered Nurse (RN) attention daily — about average for Maryland. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 65 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Maryland average (3.0)
Below average - review inspection findings carefully
Near Maryland avg (46%)
Frequent staff changes - ask about care continuity
Part of a multi-facility chain
Ask about local staffing decisions and management
8 points above Maryland average of 48%
The Ugly 65 deficiencies on record
Aug 2025
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
Based on observations, interviews and record reviews it was determined that the facility failed to ensure staff provided services that met professional standards of practice. This was found to be evid...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected most or all residents
Based on observations and interviews it was determined that the facility failed to ensure equipment was operational. This was found to be evident for 1 out of 1 observation for the door alarm operatin...
Read full inspector narrative →
Jun 2025
11 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, it was determined the facility staff failed to treat each resident in a dignified manner by standing over a resident while feeding the resident and speaking t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on reviews of facility reported incidents and interview, it was determined the facility failed to report allegations of abuse to the regulatory agency, the Office of Health Care Quality (OHCQ) w...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on review of complaint, medical record review, and staff interview, it was determined the facility failed to properly perform neuro checks after a fall for residents (Resident #33 and #34). This...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, it was determined that the facility staff failed to provide treatment/services to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of a complaint, record review, and interview, it was determined the facility failed to provide timely medication...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0840
(Tag F0840)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, it was determined that the facility staff failed to obtain outside services for re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined the facility failed to maintain complete and accurate medical records in accordance with accepted professional standards. This was evide...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. On 6/3/25 at 8:40 AM the following environmental observations were made on 3 of the 4 hallways on the second-floor nursing un...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
Based on medical record review and staff interview, it was determined the facility staff failed to ensure Minimum Data Set (MDS) assessments were accurately coded. This was evident for 4 (#26, #18, #2...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and staff interview, it was determined that the facility staff failed to follow infection control practices...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the facility's and vendor's pest control logs, observations and interviews, it was determined that the facili...
Read full inspector narrative →
Feb 2023
25 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview it was determined the facility failed to provide a written notice to a resident, re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 01/05/23 at 7:58 am during the initial walk through of the facility, there were several pieces of paper, two thermometer p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on review of the facility investigation; review of other pertinent documentation and interview with staff it was determined that the facility failed to protect resident #131 from and verbal abus...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0603
(Tag F0603)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews it was determined the facility failed to protect residents from being forced to stay in th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on administrative record review and interviews with facility staff, it was determined the facility failed to report allegations of abuse to the State Licensing Agency. This was found to be evide...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on an administrative record review and interviews with facility staff, it was determined the facility failed to complete a thorough investigation into allegations of abuse. This was found to be ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0638
(Tag F0638)
Could have caused harm · This affected 1 resident
Based on record reviews and staff interviews it was determined that the facility failed to: 1) complete Quarterly Minimum Data Set (MDS) assessments which should have included the resident's participa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. On 1/31/23 at 11:22 am, the surveyor reviewed a complaint (MD00175051) which alleged that the resident was transferred from t...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observations, medical record review, and interviews with facility staff it was determined the facility failed to follow the physician's order for a resident during medication administration o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation and interview it was determined the facility failed to provide oral care in a timely manner to a resident dependent on activities of daily living care (ADL). This was evident in o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observations, interview with family and review of medical records it was determined that the facility staff failed to ensure residents are provided with activities that meet the resident's ne...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews, the facility staff failed to administer medication according to a physician's order and failed to clarify a physician's order prior to administering oxyg...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interviews it was determined the facility failed to monitor a resident's weight who was ident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected 1 resident
Based on record review and interviews it was determined the facility failed to maintain the daily staffing schedule for 18 months. This deficient practice was evident in one of the units observed duri...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide necessary behavioral health services for the diagnosis of a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, a review of the facility's policies and interviews of the facility's staff. it was determined that the facility failed to ensure that the medication refrigerator temperature log...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview it was determined the facility staff failed to monitor the temperature of the refrigerator located in the pantry located on the Unit Lighthouse. This...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, the facility failed to provide an accurate matrix for all current residents. This deficient practice was found during a facility's annual survey.
The fin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined the facility failed to maintain medical records according to professional standards. This was evident in one (#66) resident of thirteen m...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observations and interviews it was determined that the facility failed to provide a safe, functional, sanitary, and comfortable environment for residents and staff. This deficient practice ha...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
Based on observation, medical record review and interviews, it was determined that the facility staff failed to promote care for residents in a manner and in an environment that maintained or enhanced...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to accommodate the needs of residents by failing to ensure resident meal trays reflect the resident-completed meal slips, (Residents #6, #14, #1...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and staff interviews it was determined that the facility failed to complete the Comprehensive Minimum Da...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2.
1. On 01-06-23 at 2:00 PM resident # 88 medical record review revealed an MDS assessment with a reference date of 11-14-2022....
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview with facility staff it was determined the facility failed to initiate a care plan f...
Read full inspector narrative →
Nov 2018
21 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0760
(Tag F0760)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on administrative and medical record review and staff interview it was determined the facility failed to ensure residents ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected 1 resident
Based on interviews with residents and staff and a review of resident council meeting minutes it was determined the facility failed to give adequate responses to grievances that were presented by the ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on medical record review, observation and interview it was determined that the facility failed to ensure a chair alarm was only used when there was a physician order for the use of the alarm. Th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews it was determined that the facility failed to have an effective system in place to ensure residents and responsible parties were provided written notifica...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on on medical record review, interview and review of recent facility discharge practices, it was determined that the facility failed to provide residents and or the resident representative (RP) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
3. Review of the medical record for Resident #88 on 10/29/18 at 8:40 AM, revealed diagnoses including admission to the facility post fall with fractures, joint replacement, generalized muscle weakness...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interviews with facility staff it was determined the facility failed to complete a baseline c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Failed to develop and implement a care plan that addressed urinary incontinence based on a comprehensive assessment of the re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined the facility failed to update the care plan that addressed: 1. the risk for fluid volume excess for a resident and 2. the use of a ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and review of medical records it was determined that the facility failed to ensure staff reported when a resident sustained a fall. This was found to be evident for 1 out of 6 resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on review of employee files and interview it was determined that the facility failed to have a system in place to ensure annual evaluations and required dementia training had been completed by t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on administrative and medical record review and staff interview it was determined the facility failed to promptly dispose ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
2. A medical record review was done on 11/1/18 and review of the Medication Regimen Review for Resident # 49 revealed that an irregularity was noted on 10/11/18. A copy of the recommendation was not i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
2. Review of the medical record for Resident #79 on 10/30/18 at 10:00 AM revealed diagnoses including Parkinson's disease and chronic pain syndrome.
Further review of Resident #79's medical record re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation and medical record review it was determined that the facility failed to administer medications and maintain an error rate of less than 5% by following physician orders. This was e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #103 was admitted to the facility for palliative care with diagnoses that included but were not limited to cancer wi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility failed to have an effective system in place to ensure influenza consents were obtained from the appropriate ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on administrative and medical record review and staff interview it was determined the facility failed to: 1. report a subnormal temperature to the physician and monitor the resident (Resident #2...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
Based on medical record review and interview it was determined the facility staff failed to establish and maintain a system for ensuring accuracy in weight measurements for a nutritionally compromised...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected multiple residents
Based on administrative record review and interviews with facility staff it was determined the facility failed to ensure that there was not greater than 14 hours between the residents receiving their ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations and interviews with facility staff it was determined the facility failed to ensure that sanitary conditions were maintained in the kitchen and food was stored properly. This was ...
Read full inspector narrative →
Jul 2017
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0166
(Tag F0166)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record and other pertinent documentation and staff interview it was determined the facility faile...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0274
(Tag F0274)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined facility staff failed to conduct a comprehensive assessmen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0315
(Tag F0315)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview it was determined the facility staff failed to conduct a comprehensive assess...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0371
(Tag F0371)
Could have caused harm · This affected 1 resident
Based on observations of the facility's food service operations and staff interviews it was determined that the facility failed to assure proper sanitation of dish and cookware. This was noted in the ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0431
(Tag F0431)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility failed to 1) maintain accurate records of narcotic medication change of shift reconciliation counts and 2) ensur...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0514
(Tag F0514)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview it was determined the facility failed to 1. demonstrate the implementation of...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Maryland facilities.
- • Multiple safety concerns identified: 1 life-threatening violation(s). Review inspection reports carefully.
- • 65 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • Grade F (33/100). Below average facility with significant concerns.
- • 56% turnover. Above average. Higher turnover means staff may not know residents' routines.
About This Facility
What is Autumn Lake Healthcare At Spa Creek's CMS Rating?
CMS assigns AUTUMN LAKE HEALTHCARE AT SPA CREEK an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Autumn Lake Healthcare At Spa Creek Staffed?
CMS rates AUTUMN LAKE HEALTHCARE AT SPA CREEK's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 56%, which is 10 percentage points above the Maryland average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at Autumn Lake Healthcare At Spa Creek?
State health inspectors documented 65 deficiencies at AUTUMN LAKE HEALTHCARE AT SPA CREEK during 2017 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 64 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Autumn Lake Healthcare At Spa Creek?
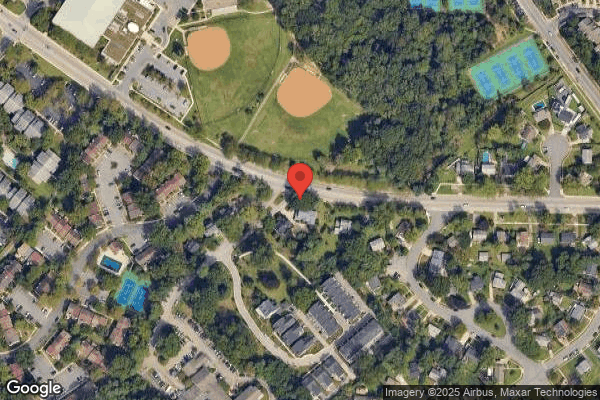
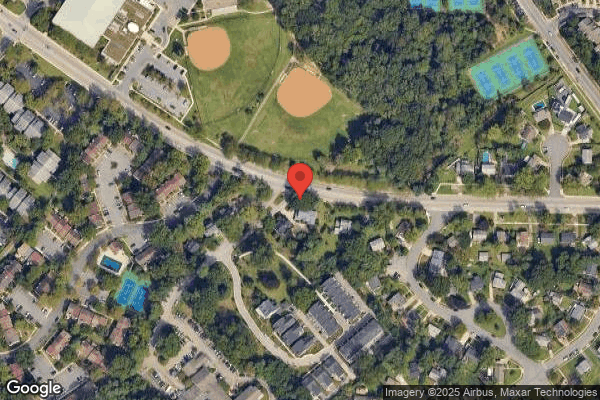
AUTUMN LAKE HEALTHCARE AT SPA CREEK is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by AUTUMN LAKE HEALTHCARE, a chain that manages multiple nursing homes. With 130 certified beds and approximately 116 residents (about 89% occupancy), it is a mid-sized facility located in ANNAPOLIS, Maryland.
How Does Autumn Lake Healthcare At Spa Creek Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, AUTUMN LAKE HEALTHCARE AT SPA CREEK's overall rating (2 stars) is below the state average of 3.0, staff turnover (56%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Autumn Lake Healthcare At Spa Creek?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the facility's high staff turnover rate, and the below-average staffing rating.
Is Autumn Lake Healthcare At Spa Creek Safe?
Based on CMS inspection data, AUTUMN LAKE HEALTHCARE AT SPA CREEK has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Maryland. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Autumn Lake Healthcare At Spa Creek Stick Around?
Staff turnover at AUTUMN LAKE HEALTHCARE AT SPA CREEK is high. At 56%, the facility is 10 percentage points above the Maryland average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Autumn Lake Healthcare At Spa Creek Ever Fined?
AUTUMN LAKE HEALTHCARE AT SPA CREEK has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Autumn Lake Healthcare At Spa Creek on Any Federal Watch List?
AUTUMN LAKE HEALTHCARE AT SPA CREEK is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.